Abstract
Purpose
Klinefelter syndrome (KS) is associated with lower socioeconomic status and greater morbidity. However, relatively little is known about the quality of life for men with KS, or how KS and other factors combine to determine it.
Methods
A total of 132 men with KS were recruited in clinics, and 313 matched controls were identified by Statistics Denmark. Demographics, socioeconomic status, health problems and behaviors, sexual function, medical follow-up, and mental and physical quality of life (MQoL and PQoL, respectively) were assessed for all participants through surveys.
Results
Men with KS reported significantly lower education attainment levels, income, physical activity, and both PQoL and MQoL, as well as more illness, medication, and sexual dysfunction. KS status was associated directly with lower PQoL, as well as indirectly through reduced income, physical activity, and sexual function, and increased body mass index. KS status and younger age were associated directly with lower MQoL, as well as indirectly through reduced income, physical activity, and partner status (for KS status), or through partner status (for age).
Conclusion
KS status is associated with lower PQoL and MQoL through both direct and indirect paths. These results suggest the need for more comprehensive research and clinical approaches to addressing quality of life for men with KS.
Similar content being viewed by others
Introduction
Klinefelter syndrome (KS), also known as 47,XXY, is the most frequent sex chromosome disorder, with a prevalence of 1 in 660 males.1 Epidemiological studies demonstrate that KS is associated with lower socioeconomic status, including lower levels of education and employment, lower income, and fewer partnerships.2 Men with KS are also at greater risk of psychiatric disorders such as depression, anxiety, attention deficit/hyperactivity disorder, and autism,3, 4, 5 and they are more likely to experience sexual problems.6 Moreover, men with KS experience more morbidity and earlier mortality due to diabetes, cardiovascular disease, infectious diseases, and diseases of the digestive and respiratory system.2, 7, 8 In summary, men diagnosed with KS suffer from a wide variety of both physical and psychological conditions throughout their lives, which may significantly impact their overall quality of life (QoL).
However, relatively little attention has been paid to QoL in men with KS, or the factors that may determine it. In two studies to date, boys and men with KS were found to have a lower QoL than non-KS males in population-based samples.9, 10 KS phenotype severity was also negatively associated with QoL among boys.9 In a third study, KS status was correlated with lower psychosocial well-being, which was associated with lower levels of employment and social support, and greater disease severity.11 While these results are consistent with a link between KS and QoL-related measures, a number of factors limit more definitive conclusions about the associations between KS, QoL, and potential intervening variables. First, KS correlates may differ across studies as a function of population, setting, and timeframe, as well as research design, protocols and measures, indicating the need for a simultaneous assessment of these variables within a single study to enable more direct, valid, and reliable comparisons. Second, in addition to KS, many demographic, physical and psychosocial factors are related to QoL, indicating the need to distinguish between these overlapping influences. Finally, many of these QoL predictors—including KS—are also related to each other, indicating the need to identify significant and independent relationships in the path (if there is one) between KS and QoL.
To address these issues, in this study, we assessed demographic factors, socioeconomic status, health outcomes, and QoL among 132 men with KS and 313 matched controls. In addition to descriptive and bivariate analyses, structural equation modeling (SEM) was used to identify independent predictors of physical and mental QoL (PQoL and MQoL, respectively)—both within and between men with KS and controls—and to determine how these factors combine to predict both QoL outcomes. Finally, path analyses were conducted to identify direct and indirect links between KS status, QoL, and the other study variables.
Materials and methods
Procedure
Men with KS were identified from endocrine, genetics, and fertility clinics throughout Denmark. Surveys were sent to 225 adult males with karyotypically verified KS. For each of the men with KS, Statistics Denmark identified five non-KS control men who were matched on age, zip code and education level from the general population. Three weeks after the first survey was sent, a reminder was sent to the nonresponders. Requirements for inclusion were a response time of less than 4 months and a minimum of 80% of questions answered. Of the 132 men with KS included in the study, 104 (79%) responded after the first contact, whereas 28 (21%) responded after the reminder. Of the 313 controls in this study, 237 (76%) responded after the first contact, and 28 (24%) responded after the reminder. The study was approved by the Danish Data Protection Agency and registered at ClinicalTrials.gov (NCT01690013).
KS participants
Among the participants with KS, 124 men had the 47,XXY karyotype and 7 had 46,XY and 47,XXY; for 1 man there was no information regarding mosaicism. The age at KS diagnosis ranged from prenatal to 52 years, with a mean of 26.5 years. Ninety-five (72%) of the participants with KS reported currently receiving testosterone treatment, and seven (5%) reported having received treatment in the past. The age at testosterone treatment initiation ranged from 10 to 55 years, and the duration of treatment ranged from less than one year to more than 40 years.
Measures
Demographics
In addition to age, demographic measures included height and weight, from which body mass indices (BMIs) were calculated. Participants also indicated when they had left their parents’ home, whether they lived alone (rather than with a partner), and whether they had fathered any children.
Socioeconomic status
Participants indicated their level of education (primary school, high school, some college, completed college, or vocational training), employment status (employed, unemployed, or retired), hours worked per week, as well as when they worked (i.e., during the day or night), and income.
Health behaviors
Participants’ health-related behaviors included alcohol use (number of drinks per week), cigarette smoking (daily, sometimes, former smoker, or never smoked), physical activity (physically active or not), and daily medicine intake (yes or no).
Psychological strain
For each of 15 important stages of life (e.g., starting school, or working in a job),12 participants indicated the level of strain they experienced (none, some, high, or not relevant) during that period.
Health problems
Participants also indicated whether they currently suffered from any of 26 of the most significant health problems among KS males (e.g., hypogonadism, gynecomastia, diabetes, and so on).
Medical follow-up
Participants with KS indicated whether they had received any medical follow-up for their KS-related health problems. Those who did also indicated whether their follow-up care came from a general practitioner, fertility clinic, endocrinologist, or other doctor. Participants with KS also used a five-point Likert scale from 1 (“not at all”) to 5 (“very much”) to indicate how satisfied they were with their follow-up care.
Sexual function
Sexual function was assessed using the International Index of Erectile Function Questionnaire (IIEF-15),13 which assesses male erectile and sexual function over the past 4 weeks. The IIEF-15 comprises five domains, including “erectile function” (six items), “orgasmic function” (two items), “sexual desire” (two items), “intercourse satisfaction” (three items) and “overall satisfaction” (two items). Each item was rated on a Likert scale from 1 (“very poor”) to 5 (“very good”), and an overall sexual function score was computed for each participant by summing their responses to all six items. Cronbach’s alphas for these subscales ranged from 0.86 to 0.96.
QoL
To maximize the content validity of this study’s primary outcome, QoL was assessed using two of the most prominent and well-validated QoL instruments: the brief version of the World Health Organization’s Quality of Life Assessment (WHOQOL-BREF) and the RAND Corporation’s Short Form Health Survey (SF-36).14
The WHOQOL-BREF is a 26-item assessment of individuals’ perceived QoL during the preceding 2 weeks.15 Twenty-four of these items are divided across four domains: “physical health” (seven items), “psychological health” (six items), “social relationships” (three items), and “environmental health” (eight items). The final two domains—general health and overall QoL—are composed of one item each. Each item was rated on a Likert scale from 1 (“very poor”) to 5 (“very good”), and Cronbach’s alphas for the multi-item subscales ranged from 0.62 to 0.84.
The SF-36 comprises eight domains: “physical functioning” (ten items), “role physical” (four items), “bodily pain” (two items), “general health” (five items), “vitality” (four items), “social functioning” (two items), “role emotional” (three items), and “mental health” (five items). Two standardized summary scores—the physical component summary and the mental component summary—were calculated based on the subscales. The physical component summary score was calculated using the four subscales in the physical domain (physical functioning, role physical, bodily pain, and general health), and the mental component summary score was calculated from the four subscales in the mental domain (mental health, vitality, social functioning, and role emotional). Response scales ranged from “yes/no” to six-point Likert scales, and Cronbach’s alphas for the subscales ranged from 0.73 to 0.92. Additional details regarding the measures for this study can be found in the Supplementary Methods online.
Analyses
After initial descriptive statistics and bivariate correlations (Supplementary Table S5) were computed, three levels of analyses were conducted on the study data. First, separate group comparisons were conducted between KS participants and controls for each of the study variables. Men with KS receiving testosterone therapy were also compared with those who were not. Second, SEM was conducted, from which two latent QoL variables emerged—PQoL and MQoL—and significant bivariate predictors of PQoL and MQoL were included in respective SEM models to identify independent, significant predictors of each QoL measure. These two SEM models were conducted separately for both KS and control participants. In the third set of analyses, data from KS and control participants were combined to conduct separate path analyses for PQoL and MQoL, again using their respective bivariate predictors. Path analysis identifies significant links between each pair of variables in a model, controlling for the influence of all other model factors, thus illuminating both direct and indirect “paths” between independent measures, outcomes, and any mediating variables.
A comparative fit index was used to evaluate goodness of fit for these statistical models. Missing data were imputed with maximum likelihood estimates. Continuous measures were tested for normality, and non-normal data were analyzed using the Mann–Whitney U test (as opposed to the Student’s t-test), while categorical data were analyzed using Pearson’s chi-squared test. Given the exploratory nature of this research and the primary concern about type II error, we did not include any adjustment for multiple comparisons. Data entry was done in duplicate using epiDATA version 3.1 (EpiData Association; Odense, Denmark), and statistical analyses were conducted using SPSS and SPSS AMOS version 21.0 (SPSS; Chicago, IL).
Results
KS versus controls
In summary, we found statistically significant differences between KS and controls regarding height, weight, smoking habits, partner status, parenthood, age when leaving parents’ home, educational level, employment status, working hours per week, working shifts, illness-related absences from work, income, and daily medicine intake (Table 1), as well as psychological strain (Supplementary Figure S1) and health problems (Supplementary Table S2). No significant differences were found between KS and controls in age, BMI, or weekly alcohol consumption.
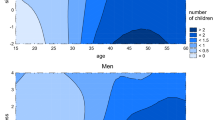
Significantly fewer men with KS than controls reported engaging in physical activity or liking it during childhood or adolescence, either in or out of school. Among participants reporting no physical activity, men with KS were more likely to indicate that it was due to a lack of motivation or companionship, feeling clumsy or fatigued, or their body simply not working (Supplementary Table S1). Regarding sexual function, significantly more men with KS than controls reported being homosexual or bisexual, feeling less self-confidence as a man and a sex partner, experiencing later sexual debut, orgasmic problems, and lower intercourse satisfaction, as well as having more testicular pain, erectile dysfunction, and delayed ejaculation (Table 2). Among men with KS followed up by general practitioners, 36.4% were dissatisfied with their clinical care, compared with 12.4% of those followed up by endocrinologists, and 45% of those not receiving any medical follow-up (Supplementary Figure S2). Finally, KS men reported significantly lower PQoL and MQoL than controls (Figure 1 and Supplementary Table S3). However, there were no differences in either PQoL or MQoL between men with KS receiving testosterone therapy and men with KS who were not (Supplementary Table S4).
Structural equation models
PQoL
Among men with KS, greater PQoL was significantly—and independently—associated with greater employment, higher income, more physical activity, and less daily medication, but not testosterone therapy. Together, these predictors accounted for 37% of the variance in KS participants’ overall PQoL (Figure 2a). Among controls, significant and independent predictors of greater PQoL included more employment, higher income, and more physical activity, as well as lower BMI and less daily medication. These predictors combined to explain 34% of control participants’ PQoL (Figure 2b).
Structural equation models for quality of life in men with Klinefelter syndrome (a,b) and in controls (c,d). Physical quality of life (PQoL; a,c) and mental quality of life (MQoL; b,d) are latent variables, and the single-headed arrows from the latent variables point to their respective indicators. The single-headed arrows from the rectangular boxes (observed variables) to the latent variables represent the impact of each observed variable on the latent variable. Circles E1, E2, and E3 represent errors. The overall goodness-of-fit parameters are displayed below each model. The dashed arrows represent non-significant associations. The numbers beside each association are estimates of standardized regression coefficients. BMI, body mass index; CFI, comparative fit index. *P < 0.05, **P < 0.01.
MQoL
Among men with KS, only higher income and living with a partner were significant independent predictors of (greater) MQoL, accounting for 23% of the variance (Figure 2c). As with PQoL, testosterone treatment did not significantly predict KS participants’ MQoL. Among controls, greater MQoL was significantly and independently predicted by older age, more employment, living with a partner, and less daily medication, which combined to explain 15% of control participants’ MQoL (Figure 2d).
Path analytic models
PQoL
In addition to its direct (negative) association with PQoL, having KS was also linked to lower PQoL indirectly through lower income and higher BMI (Figure 3a). KS status had similarly negative direct and indirect links (again through income and BMI) to physical activity, which was itself associated positively with PQoL—both directly and indirectly—through sexual function, which also mediated a separate link between income and PQoL.
MQoL
As shown in Figure 3b, there were two empirical paths to participants’ MQoL. The first path began with KS status, which was linked directly (and negatively) to MQoL, and indirectly through living alone—which was negatively associated with MQoL and positively associated with income—and lower income, which was positively related to MQoL. Both KS status and income were linked indirectly to MQoL through their associations with physical activity, which was associated with greater MQoL. A second, simpler path to MQoL began with age, which was related directly (and positively) to MQoL, and indirectly through its positive link to living with a partner. A third path comprised significant effects of KS status and older age on higher levels of daily medication.
Discussion
In this study, having KS was strongly and consistently associated with poorer QoL and other related factors, both in bivariate and multivariate analyses. In addition to the previous research on KS correlates cited earlier, these results are consistent with the limited research on the link between KS and QoL, including the inverse association found between QoL and phenotype severity among boys and men with KS,9, 11 and the finding that over three-quarters of KS men felt that KS had had a severely negative impact on their life.16 These results also mirror the lower QoL observed among patients with chronic diseases such as diabetes and heart disease17, 18 (which are also associated with KS), suggesting that lower QoL among KS males may be due, at least in part, to comorbidity.5, 7, 19
Also concordant with previous research, employment and income were negatively associated with KS status, and positively linked with QoL (and each other), both within and between the KS and control groups. This suggests that while employment and income are relevant to the QoL of KS and non-KS populations alike, they are particularly important—but less available in the sense that more KS are unemployed and are less skilled—to those with KS, as was found in previous studies of QoL among other patients17, 18, 20, 21 and healthy people.22 Many of the challenges and limitations that accompany KS may also limit one’s ability to find or maintain employment, as suggested by our finding that KS men were significantly more likely than controls to be unemployed or absent from work due to illness (although the latter may be due in part to KS men working nightshifts, which can also have negative health effects23). It is also worth noting that employment and income had independent effects on QoL, illustrating the importance of both financial and nonmaterial aspects of employment for physical and psychological well-being.
Physical activity was significantly lower among KS men and positively linked to QoL, particularly for PQoL (which is to be expected), and particularly among matched controls, which may reflect the impact of greater physical activity on PQoL and/or vice versa. These results are consistent with previous studies among other patient groups,17, 24 and in the general population.25 Similarly, BMI was significantly higher among KS participants, and negatively associated with PQoL, but only among controls. Consistent with previous research in the general population,25 this finding may reflect lower PQoL variability, or the smaller sample of KS men in this research.
Although unrelated to PQoL, living with a partner was consistently associated with higher MQoL, especially among KS participants, suggesting that men with KS may have a greater need for social support, which is concordant with previous associations between KS status and poorer social skills,26 and previous links between social support and mental health among men with KS11 and other patient groups.17, 18 In addition, the current path analyses indicate that living with a partner partially explains the lower MQoL associated with KS and the higher MQoL as both KS and non-KS men grow older.
While overall sexual dysfunction was only marginally associated with KS status in this research, men with KS reported significantly more erectile dysfunction, decreased orgasmic function and lower intercourse satisfaction, as well as delayed ejaculation and testicular pain. These findings are largely inconsistent with the majority of previous studies on the link between KS and sexual dysfunction, which have not found significant differences.6, 27, 28 However, the external validity of these studies may be limited, given the relatively narrow scope of recruitment, as participants were recruited through men seeking medical treatment for infertility or sexual dysfunction,6, 27, 28 while this research included matched controls from the general population. Consistent with previous research,6, 29 we found no significant differences in the number of sexual partners or intercourse frequency between men with KS and controls, indicating that despite some problems, men with KS maintain active sex lives. In addition, sexual function partially mediated the effects of both income and physical activity on participants’ overall PQoL. We found no QoL differences between KS men who had received testosterone therapy and those who had not. While these findings mirror other null results,6, 27 testosterone treatment has been found to improve sexual motivation and mood in both men with KS30 and other hypogonadal men.31, 32 These discrepancies may reflect differences in the frequency and/or dosage of the testosterone therapies, or the sexual dysfunction of KS men may have other causes unrelated to testosterone level, such as dyslipidemia, diabetes, hypertension, metabolic syndrome, and obesity, which are also associated with erectile dysfunction33 and infertility.34 Further studies correlating sexual function with serum levels of sex hormones and the prevalence of diabetes may elucidate answers to these questions.
Surprising and somewhat alarming, over one-third (38%) of KS men in this study reported receiving no medical follow-up by a specialist, which made these patients significantly less satisfied than those who were seen by a specialist. This may have been due to general practitioners restricting their focus to testosterone supplementation, while endocrinologists may also address other aspects of KS, including comorbidity, sexual function, psychosocial aspects, and QoL. These results are consistent with those of Turriff et al.,35 who found that a primary complaint of KS patients was health-care providers who lacked knowledge about their condition. This suggests that the treatment of men with KS may be improved by addressing KS-related problems identified in this and other research.
Strength and limitations
This research is the most comprehensive study of QoL among men with KS to date, and the first to empirically and simultaneously examine the ability of demographic, anthropometric, socioeconomic, medical, and behavioral factors to predict the PQoL and MQoL of KS men and matched controls. In so doing, this research controlled for different research settings, designs and measures in previous bivariate studies of KS and QoL-related outcomes, while also identifying independent significant predictors of both PQoL and MQoL. Using path analysis, this study also identified direct and indirect empirical pathways between KS, QoL, and their respective mediators. In turn, these results provide not only guidance for future research, but also potential targets for intervention (i.e., mediators) to mitigate the deleterious effects of KS.
The limitations of this study include the cross-sectional and observational nature of the research design, which precludes causal inferences about the relationships identified in these analyses. Of course, the same is true for any research in which predictors—including KS status and most other factors in this study—cannot be randomly assigned. However, given the nature of the analyses and some of the measures in this study, we can make certain conclusions about the directionality of many of the observed links. First, we know that neither KS nor age were caused by any other factors being considered. In addition, physical, social, and socioeconomic characteristics tend to be stable over time and established early in life, suggesting that they likely precede current measures of behavior and psychological states. Finally, these analyses controlled for a wide variety of potential confounds, identifying a number of factors that did not explain the current findings. Nonetheless, more definitive conclusions about the directional and causal links would require future longitudinal and experimental studies, which would be valuable extensions of this research.
The current results may also be limited in their generalizability; although the recruitment of men with KS was conducted in many relevant clinics across Denmark, the selection of these clinics was not random, and the final response rates for KS men and matched controls were 59% and 28%, respectively. Although these response rates are comparable to similar survey studies,36 and the socioeconomic status and health problems of respondents with KS in this research were similar to the broader Danish KS population,2, 7, 37 we found a higher prevalence of fatherhood and a lower prevalence of retirement, suggesting that the KS responders in this study may have had a more favorable socioeconomic profile than the broader KS population in Denmark.
This research was based largely on participant self-reports, which are subject to potential biases, especially for measures with positive or negative social connotations. Although this should not impact linear relationships—assuming the biases are consistent across participants—they may influence the descriptive results, and may introduce confounding effects into bivariate and multivariate analyses (but only if they are associated with both linked variables). One way to assess and control for these effects in future research would be to include a social desirability measure,38 which could control for people’s desire to be viewed in a positive light.
Although comprehensive, the current structural equation models explained between 15 and 37% of the variance in participants’ QoL. While significant, and similar to QoL studies in other patient populations,17, 39 these results indicate that the majority of QoL among KS men and controls was determined by factors not considered in these analyses. These additional determinants may come from different sources (e.g., personality, experience, or physical setting), and they illustrate the importance of continued research in this area.
In conclusion, the results of this research illustrate the multifaceted nature of QoL and its predictors—including KS—and the importance of identifying these relationships for better understanding and more effective treatment of KS-related problems. These findings also argue for additional research and broader knowledge about how genetic, socioeconomic, medical, psychological, and behavioral factors impact individuals’ QoL, and vice versa. In so doing, this research and similar future studies may help to improve the physical and psychological well-being of KS men and others, as well as the conditions that may combine to determine these important health outcomes. The current results are consistent with previous suggestions that men with KS would benefit from multidisciplinary clinical care,40 which we also strongly support.
References
Bojesen A, Juul S, Gravholt CH . Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab 2003;88:622–626.
Bojesen A, Stochholm K, Juul S, Gravholt CH . Socioeconomic trajectories affect mortality in Klinefelter syndrome. J Clin Endocrinol Metab 2011;96:2098–2104.
Bruining H, Swaab H, Kas M, van EH . Psychiatric characteristics in a self-selected sample of boys with Klinefelter syndrome. Pediatrics 2009;123:e865–e870.
Skakkebæk A, Gravholt CH, Rasmussen PM et al. Neuroanatomical correlates of Klinefelter syndrome studied in relation to the neuropsychological profile. Neuroimage Clin 2013;4:1–9.
Van Rijn S, Swaab H, Aleman A, Kahn RS . Social behavior and autism traits in a sex chromosomal disorder: Klinefelter (47XXY) syndrome. J Autism Dev Disord 2008;38:1634–1641.
Corona G, Petrone L, Paggi F et al. Sexual dysfunction in subjects with Klinefelter’s syndrome. Int J Androl 2010;33:574–580.
Bojesen A, Juul S, Birkebaek NH, Gravholt CH . Morbidity in Klinefelter syndrome: a Danish register study based on hospital discharge diagnoses. J Clin Endocrinol Metab 2006;91:1254–1260.
Swerdlow AJ, Higgins CD, Schoemaker MJ, Wright AF, Jacobs PA . Mortality in patients with Klinefelter syndrome in Britain: a cohort study. J Clin Endocrinol Metab 2005;90:6516–6522.
Close S, Fennoy I, Smaldone A, Reame N . Phenotype and adverse quality of life in boys with Klinefelter syndrome. J Pediatr 2015;167:650–657.
De RW, de HA, Drent ML . Quality of life is reduced in patients with Klinefelter syndrome on androgen replacement therapy. Eur J Endocrinol 2009;160:465–468.
Herlihy AS, McLachlan RI, Gillam L, Cock ML, Collins V, Halliday JL . The psychosocial impact of Klinefelter syndrome and factors influencing quality of life. Genet Med 2011;13:632–642.
Naess EE, Bahr D, Gravholt CH . Health status in women with Turner syndrome: a questionnaire study on health status, education, work participation and aspects of sexual functioning. Clin Endocrinol 2010;72:678–684.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A . The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997;49:822–830.
Bjørner JB, Damsgaard MT, Watt T et al. Danish SF-36 manual—a health status questionnaire. LIF Lægemiddelindustriforeningen: : Copenhagen, Denmark, 1997.
The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med 1998;28:551–558.
Turriff A, Levy HP, Biesecker B . Factors associated with adaptation to Klinefelter syndrome: the experience of adolescents and adults. Patient Educ Couns 2015;98:90–95.
Imayama I, Plotnikoff RC, Courneya KS, Johnson JA . Determinants of quality of life in adults with type 1 and type 2 diabetes. Health Qual Life Outcomes 2011;9:115.
Verma AK, Schulte PJ, Bittner V et al. Socioeconomic and partner status in chronic heart failure: relationship to exercise capacity, quality of life, and clinical outcomes. Am Heart J 2017;183:54–61.
Turriff A, Levy HP, Biesecker B . Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genet Med 2011;13:966–972.
Blake C, Codd MB, Cassidy A, O’Meara YM . Physical function, employment and quality of life in end-stage renal disease. J Nephrol 2000;13:142–149.
O’Neill J, Hibbard MR, Brown M et al. The effect of employment on quality of life and community integration after traumatic brain injury. J Head Trauma Rehabil 1998;13:68–79.
Michelson H, Bolund C, Nilsson B, Brandberg Y . Health-related quality of life measured by the EORTC QLQ-C30—reference values from a large sample of Swedish population. Acta Oncol 2000;39:477–484.
Ramin C, Devore EE, Wang W, Pierre-Paul J, Wegrzyn LR, Schernhammer ES . Night shift work at specific age ranges and chronic disease risk factors. Occup Environ Med 2015;72:100–107.
Lloyd CE, Orchard TJ . Physical and psychological well-being in adults with type 1 diabetes. Diabetes Res Clin Pract 1999;44:9–19.
Herman KM, Hopman WM, Vandenkerkhof EG, Rosenberg MW . Physical activity, body mass index, and health-related quality of life in Canadian adults. Med Sci Sports Exerc 2012;44:625–636.
Skakkebæk A, Moore PJ, Pedersen AD et al. The role of genes, intelligence, personality and social engaement in cognitive performance in Klinefelter syndrome. Brain Behav 2017;7:e00645.
Yoshida A, Miura K, Nagao K, Hara H, Ishii N, Shirai M . Sexual function and clinical features of patients with Klinefelter’s syndrome with the chief complaint of male infertility. Int J Androl 1997;20:80–85.
El BH, Majzoub A, Al SS, Alnawasra H, Dabbous Z, Arafa M . Sexual dysfunction in Klinefelter’s syndrome patients. Andrologia; e-pub ahead of print 23 September 2016.
Raboch J, Pietrucha S, Raboch J . Serum testosterone levels and coital activity in men with somatosexual disorders. Neuro Endocrinol Lett 2003;24:321–324.
Wu FC, Bancroft J, Davidson DW, Nicol K . The behavioural effects of testosterone undecanoate in adult men with Klinefelter’s syndrome: a controlled study. Clin Endocrinol 1982;16:489–497.
Wang C, Swerdloff RS, Iranmanesh A et al. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab 2000;85:2839–2853.
Skakkebæk NE, Bancroft J, Davidson DW, Warner P . Androgen replacement with oral testosterone undecanoate in hypogonadal men: a double blind controlled study. Clin Endocrinol 1981;14:49–61.
Rosen RC, Fisher WA, Eardley I, Niederberger C, Nadel A, Sand M . The multinational men’s attitudes to life events and sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin 2004;20:607–617.
Kasturi SS, Tannir J, Brannigan RE . The metabolic syndrome and male infertility. J Androl 2008;29:251–259.
Turriff A, Macnamara E, Levy HP, Biesecker B . The impact of living with Klinefelter syndrome: a qualitative exploration of adolescents and adults. J Genet Couns; e-pub ahead of print 10 November 2016.
Asch DA, Jedrziewski MK, Christakis NA . Response rates to mail surveys published in medical journals. J Clin Epidemiol 1997;50:1129–1136.
Stochholm K, Juul S, Gravholt CH . Socio-economic factors affect mortality in 47,XYY syndrome—a comparison with the background population and Klinefelter syndrome. Am J Med Genet A 2012;158A:2421–2429.
Crowne DP, Marlowe D . A new scale of social desirability independent of psychopathology. J Consult Psychol 1960;24:349–354.
Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L . Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care 1997;20:562–567.
Nieschlag E, Ferlin A, Gravholt CH et al. The Klinefelter syndrome: current management and research challenges. Andrology 2016;4:545–549.
Acknowledgements
We thank I.L. Skakkebæk for assistance with data entry. This study was supported by grants from the Lundbeck Foundation, Augustinus Foundation, Aase and Einar Danielsen Foundation, Novo Nordisk Foundation (NNF13OC0003234 and NNF15OC0016474), “Fonden til lægevidenskabens fremme,” Hede Nielsen Family Foundation, and Health Research Foundation of Region Midtjylland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary material is linked to the online version of the paper at
Rights and permissions
About this article
Cite this article
Skakkebæk, A., Moore, P., Chang, S. et al. Quality of life in men with Klinefelter syndrome: the impact of genotype, health, socioeconomics, and sexual function. Genet Med 20, 214–222 (2018). https://doi.org/10.1038/gim.2017.110
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.110