Abstract
Purpose:
Familial pancreatic cancer kindreds contain at least two affected first-degree relatives. Comprehensive data are needed to assist clinical risk assessment and genetic testing.
Methods:
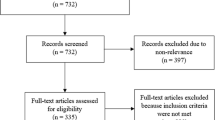
Germ-line DNA samples from 727 unrelated probands with positive family history (521 met criteria for familial pancreatic cancer) were tested in compliance with the Clinical Laboratory Improvement Amendments for mutations in BRCA1 and BRCA2 (including analysis of deletions and rearrangements), PALB2, and CDKN2A. We compared prevalence of deleterious mutations between familial pancreatic cancer probands and nonfamilial pancreatic cancer probands (kindreds containing at least two affected biological relatives, but not first-degree relatives). We also examined the impact of family history on breast and ovarian cancers and melanoma.
Results:
Prevalence of deleterious mutations (excluding variants of unknown significance) among familial pancreatic cancer probands was: BRCA1, 1.2%; BRCA2, 3.7%; PALB2, 0.6%; and CDKN2A, 2.5%. Four novel deleterious mutations were detected. Familial pancreatic cancer probands carry more mutations in the four genes (8.0%) than nonfamilial pancreatic cancer probands (3.5%) (odds ratio: 2.40; 95% confidence interval: 1.06−5.44; P = 0.03). The probability of testing positive for deleterious mutations in any of the four genes ranges up to 10.4%, depending on family history of cancers. BRCA2 and CDKN2A account for the majority of mutations in familial pancreatic cancer.
Conclusion:
Genetic testing of multiple relevant genes in probands with a positive family history is warranted, particularly for familial pancreatic cancer.
Genet Med 17 7, 569–577.
Similar content being viewed by others
Introduction
Pancreatic adenocarcinoma is currently the fourth leading cause of cancer death in the United States,1 and it is anticipated to be the second leading cause by the year 2020.2 Despite medical advances, overall 5-year survival rates have not significantly changed, with the vast majority of diagnoses made at advanced stages of disease.1 The relatively lower incidence of pancreatic cancer compared with other malignancies makes it challenging to conduct the large-scale studies that are needed to determine appropriate early screening measures.3 It is critical to identify populations at high risk, who may potentially benefit from earlier detection with concomitant implications for intervention or therapy.4
Family history studies suggest that ~5–10% of pancreatic adenocarcinoma cases have a strong hereditary basis, and familial pancreatic cancer (FPC) is thought to be genetically heterogeneous. FPC, defined as involving kindred with at least two affected first-degree relatives (FDR), describes an established entity of inherited pancreatic cancer.5 Our knowledge of the genetic basis of FPC largely arises from observed increased pancreatic cancer risk in those with hereditary malignant syndromes. A number of candidate susceptibility genes have been proposed to date, and four genes, BRCA1, BRCA2, PALB2, and CKDN2A, appear to account for the majority of known genetic causes of FPC.5
Individuals carrying germ-line mutations in BRCA1 and BRCA2 demonstrate increased risk for development of other malignancies, including pancreatic cancer.6,7,8 Although germ-line mutations in BRCA1 and BRCA2 are associated with hereditary ovarian and breast cancer syndrome, this increased risk of pancreatic malignancy can also manifest in families who do not meet criteria for hereditary ovarian and breast cancers.9,10 In the initial studies by the Breast Cancer Linkage Consortium, the relative risk of development of pancreatic cancer was increased by a mean of 2.26-fold for BRCA1 6 and 3.5-fold for BRCA27 carriers. However, risk ascertainment was performed for families with hereditary breast cancer rather than for families with pancreatic cancer, thus likely underestimating the actual risk for pancreatic cancer in BRCA1 and BRCA2 mutation carriers. Although initial investigations cite the presence of pancreatic cancer in hereditary ovarian and breast cancer families with deleterious BRCA1 mutations,8,11,12 no germ-line BRCA1 mutations were identified in a series of pancreatic cancer families.13 Thus, available evidence indicates that when individuals are ascertained through FPC kindreds, the risk of pancreatic cancer in BRCA1 mutation carriers is less than it is for BRCA2 mutation carriers. Murphy et al.14 reported 17% prevalence of BRCA2 mutations among affected individuals from 26 European FPC kindreds with three or more affected family members with pancreatic cancer. Subsequent studies of individuals with pancreatic cancer from families meeting FPC criteria (two or more affected FDR) estimated BRCA2 prevalence ranging between 6 and 10%.15 Furthermore, the ethnic variation of the population influences mutation prevalence rates of BRCA1 and BRCA2 and should be recognized when interpreting the literature. For example, among Ashkenazi Jews, similar mutation prevalence was observed for both BRCA1 and BRCA2.16,17 The role of BRCA1 and BRCA2 mutations in larger samples of FPC kindreds remains to be elucidated. Determination of BRCA mutation status has potential therapeutic implications, because those carrying such mutations have been shown to benefit from therapies that inhibit poly(ADP ribose)polymerase (PARP inhibitors).18,19
PALB2, a co-localizer and partner gene to BRCA2, is also proposed to be involved in FPC. PALB2 was originally identified as a novel protein that complexes with BRCA2, leading to its stability and facilitating DNA repair.20 Bi-allelic germ-line mutations in PALB2 lead to the development of Fanconi anemia,21 whereas mono-allelic mutations increase breast cancer susceptibility. While searching for candidate pancreatic cancer susceptibility genes, Jones et al.22 discovered an inherited deleterious PALB2 mutation coupled with a second inactivating hit in a patient with pancreatic cancer. Further PALB2 sequencing in a cohort of 96 FPC patients showed that 3–4% carried deleterious mutations. With the exception of one European study,23 subsequent studies have reported a lower prevalence of PALB2 mutations in FPC.24,25 Studies with large sample sizes and unbiased selection criteria are needed to provide a more complete understanding of the role of BRCA1, BRCA2, and PALB2 in pancreatic cancer susceptibility.
The CDKN2A gene located on chromosome 9p21 encodes the p16 protein, an important cell-cycle regulator that inhibits cyclins, thus preventing premature transition from G1 to the S phase and serving as an important tumor suppressor. Germ-line mutations in CDKN2A are responsible for early-onset melanomas often associated with the development of familial atypical multiple mole melanoma (FAMMM) syndrome. Increased risk for pancreatic cancer development was observed in cases of CDKN2A-associated familial melanoma.26 Examining CDKN2A in German FPC patients, Bartsch et al.27 found that mutations were rare, unless patients had concurrent melanoma. Studies performed in other regions of Europe ultimately demonstrated the occurrence of CDKN2A mutations in FPC kindreds without melanoma, with prevalence ranging from 20 to 30%.28 However, such elevated rates were probably influenced by specific founder mutations; one study also included patients of other familial cancer syndromes. In a large study in the United States of CDKN2A germ-line mutations among 1,537 unselected, mostly sporadic pancreatic cancer cases, McWilliams et al.29 found a much lower overall prevalence of CDKN2A mutations (0.6%), with higher rates in the subset of cases with affected FDR; the limited family history data in this study left open the question of germ-line CDKN2A mutations in patients with FPC, particularly families without evidence of FAMMM.
To better inform genetic counseling of patients and families through more precise prevalence estimates, we comprehensively analyzed BRCA1, BRCA2, PALB2, and CDKN2A in a large cohort of FPC kindreds ascertained via the multicenter Pancreatic Cancer Genetic Epidemiology (PACGENE) Consortium.
Materials and Methods
Subjects
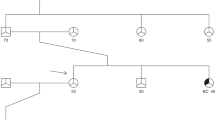
Institutional review board approval was obtained at all participating sites, and written consent was obtained from all probands to be included in the study. PACGENE Consortium sites had assembled 2,853 unrelated kindreds containing at least two family members affected with pancreatic cancer from which subjects for this study sample were drawn (i.e., not all probands had available biospecimens). Ascertainment and recruitment methods were previously described.30 Probands were biopsy proven or clinically documented to have a diagnosis of pancreatic adenocarcinoma. We identified 727 unrelated kindreds that contained at least two biologically related family members affected with pancreatic cancer and from which a proband DNA sample was available. PACGENE sites include Mayo Clinic (Rochester, MN; n = 341), Johns Hopkins University (Baltimore, MD; n = 107), Barbara Ann Karmanos Cancer Institute (Detroit, MI; n = 45), University of Toronto (Ontario, Canada; n = 131), and Dana-Farber Cancer Institute (Boston, MA; n = 58). Data of subjects from kindreds similar to the PACGENE sites were contributed by the University of Texas MD Anderson Cancer Center (Houston, TX; n = 38) and University of Utah (Salt Lake City, UT; n = 7). In general, probands were not selected for hereditary cancer syndrome patterns or whether genetic mutation status in one of the four tested genes may have been previously known. Some potential probands with known mutations in one of the genes being tested may have been excluded by some sites, but this was not systematic. DNA was extracted at each contributing site from peripheral blood or buccal cell samples. Baseline demographics and family history information were available and were typically self-reported.
Of the 727 kindreds in this study, a subset of 521 met criteria for FPC (having two FDR with pancreatic cancer), and the remaining 206 were familial non-FPC cases (these kindreds contained at least two affected biologic relatives, but no FDR). A small proportion (1.2%) of the total sample also had a personal history of melanoma; among females, personal history of breast and ovarian cancers occurred in 6.4 and 0.6%, respectively. All subjects were assigned a unique identifier, and all samples were de-identified during analysis by Myriad Genetic Laboratories.
Mutation analysis
Re-sequencing analysis for germ-line mutations in BRCA1, BRCA2, PALB2, and CDKN2A and large rearrangement analysis of BRCA1 and BRCA2 were conducted by Myriad Genetic Laboratories. Full-sequence DNA analysis of these four genes and breakpoint analysis for five large genomic rearrangements in BRCA1 (exon13del3835bp, exon13ins6kb, exon14-20del26kb, exon22del510bp, and exon8-9del7.1kb) were performed using previously described methods.31,32 All testing adhered to Clinical Laboratory Improvement Amendments requirements.
Briefly, for each of the four genes, full-gene sequencing was performed in both forward and reverse directions. The noncoding intronic regions of each gene that are analyzed do not extend more than 20 base pairs proximal to the 5′ end and 10 base pairs distal to the 3′ end of each exon. Aliquots of subjects’ DNA were each subjected to polymerase chain reaction (PCR) amplification to generate exon-specific amplicons that can be directly sequenced. The amplified products are each sequenced in forward and reverse directions using fluorescent dye-labeled sequencing primers. Electropherogram tracings of each amplicon are analyzed by a proprietary computer-based review system followed by visual inspection and confirmation of all clinically significant variants. Genetic variants are detected by comparison with a consensus wild-type sequence constructed for each gene. All potential clinically significant variants are independently confirmed by repeated PCR amplification of the indicated gene region(s) and sequence determination as noted above. In addition, large-rearrangement analysis of BRCA1 and BRCA2 was performed for each sample using the BRACAnalysis Rearrangement Test (BART), a quantitative multiplex end-point PCR assay that detects all large deletions and duplications across the coding regions and promoters of BRCA1 and BRCA2 using a quantitative end-point multiplex PCR assay. BART uses a set of 12 reactions comprising 11 multiplex PCR reactions containing 9–14 amplicons per multiplex and one contamination detection reaction. These amplicons cover coding exons, promoters, and flanking regions for BRCA1 and BRCA2.33
Deleterious (including suspected deleterious) mutations, variants of uncertain significance (VUS), and single-nucleotide polymorphisms in the four genes were detected and distinguished for the data analysis. Deleterious (including suspected deleterious) mutations, VUS, and single-nucleotide polymorphisms were defined as those established in the current published literature as well as that previously catalogued in Myriad’s established genetic mutation database for these genes. Novel, previously unreported mutations discovered in this study were defined as those not present in the Myriad gene mutation database. All variants were classified in accordance with the recommendations of the American College of Medical Genetics and Genomics for standards in the interpretation and reporting of sequence variations.34
Data analysis
Prevalence of deleterious mutations and of VUS for the four genes studied was compared between individuals of FPC and familial non-FPC kindreds. We focused on the subanalysis of the probands who had complete results on all four genes to gain better insight for genetic counseling for BRCA1, BRCA2, PALB2, and CDKN2A. Descriptive statistics and mutation rates were calculated. Comparisons of the mutation prevalence between groups were measured using either chi-square or Fisher’s exact tests, depending on sample sizes. All statistical analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC).
Results
Baseline demographic characteristics of the 727 probands included in this study are shown in Table 1 . Among these, 521 met criteria for FPC and the remaining 206 were classified as familial non-FPC. A slight majority of probands were males (50.9%), and median age of diagnosis was 65 years (range: 20–95 years). The sample was largely white/Caucasian (87.3%), and 43 (8.0%) were of Ashkenazi Jewish descent among the 538 who self-reported this information. A majority of kindreds (70.4%) contained two affected family members with pancreatic cancer, 19.3% reported three affected individuals, and 10.3% contained four or more affected individuals.
Table 2 summarizes the deleterious mutations, VUS, and single-nucleotide polymorphisms in the four genes for this sample, highlighting those that were not previously established in the current literature. The four novel deleterious mutations detected were: BRCA2 6224insT; PALB2 E837X (2509G>T); PALB2 W1038X (3113G>A); and CDKN2A 286delG. Novel VUS detected were: BRCA1 H1860Q (5699C>A); BRCA2 S538N (1841G>A), T1586I (4985C>T), and dup exon 1; PALB2 E1018D (3054G>T), E892K (2674G>A), I887S (2660T>G), P1009S (3025C>T), P65L (194C>T), P806L (2417C>T), S578G (1732A>G), Y334D (1000T>G); and CDKN2A G101R (301G>A), L65P (194T>C), and T18P (52A>C). These novel VUS, particularly in PALB2, have been classified as incidental findings and are not likely related to the pathogenesis of FPC at this time.35
Table 3 summarizes germ-line mutation prevalence in the subset of 716 probands who had results for all four genes tested (all results in the full sample and by gene are provided in Supplementary Table S1 online). Results in Table 3 are stratified by deleterious mutations and VUS among probands from FPC kindreds and probands from kindreds that did not strictly meet the FPC criterion of containing at least two affected FDR (familial non-FPC). Gene for gene, probands from FPC kindreds carry more deleterious mutations than those from familial non-FPC kindreds. The probability that a proband carried a deleterious mutation in any of these genes was 8.0 and 3.5% in FPC versus familial non-FPC probands, respectively (odds ratio: 2.40; 95% confidence interval: 1.06−5.44; P = 0.03). The aggregate prevalence is 48/716 (6.7%) for all cases with any positive family history. Overall, deleterious mutations in BRCA2 and CDKN2A were more prevalent compared with either BRCA1 or PALB2.
The vast majority of probands who did test positive for a mutation carried a mutation in only one of the four genes. Only two individuals whose only personal cancer history was that of pancreatic cancer had multiple mutations: one proband carried two novel mutations in PALB2: E837X (2509G>T) (classified as deleterious) and P806L (2417C>T) (classified as VUS); another proband from a familial non-FPC kindred carried a mutation in both BRCA1 (187delAG) and BRCA2 (6174delT). Conversely, two probands who had malignancies in addition to pancreatic cancer tested positive for one mutation each: one proband had breast and ovarian cancers in addition to pancreatic cancer and was found to carry 816delGT in BRCA1; another proband had breast cancer and melanoma in addition to pancreatic cancer and was found to carry V932M (2794G>A) in PALB2. The number of individuals affected with pancreatic cancer in a kindred did not correlate with the prevalence of deleterious mutations in FPC kindreds (analysis of variance P = 0.97; Supplementary Table S2 online).
Table 4 displays germ-line mutation prevalence in the subset of 716 probands who had results for all four genes tested, stratified by deleterious mutations and VUS and by whether they also had family history of breast cancer, ovarian cancer, or melanoma. As expected, probands with a family history of breast cancer were more likely to test positive for deleterious mutations in BRCA1 (1.9%) or BRCA2 (4.2%), probands with a family history of ovarian cancer were more likely to test positive for deleterious mutations in BRCA1 (5.2%) and BRCA2 (5.2%), and probands with a family history of melanoma were more likely to test positive for deleterious mutations in CDKN2A (7.8%). Overall, the probability that a proband with a family history of any of these three cancers would test positive for a deleterious mutation in any of the four genes is 8.7%. Similar results for probands when family history is restricted to FDR are shown in Supplementary Table S3 online; those data show that a proband with a family history in an FDR of any of these three cancers has an overall 9.5% probability of testing positive for a deleterious mutation in any of the four genes. To facilitate genetic counseling, we have aggregated a summary of our data showing the distributions of the probabilities of deleterious mutations by various cancer family histories in Figure 1 . As can be seen, BRCA2 and CDKN2A constitute the majority of deleterious mutations across cancer family histories. Probands with pancreatic cancer who have a family member with ovarian cancer have a 10.4% probability of testing positive for a deleterious mutation in BRCA1 or BRCA2. Probands with melanoma in their family history have a 10.4% probability of testing positive for CDKN2A or BRCA2 mutations. Interestingly, 7 of the 14 (50%) patients who carried CDKN2A mutations did not have a personal or family history of melanoma. Of the six BRCA1 mutation carriers, one (16.7%) had no personal or family history of breast cancer, and two (33.3%) had no personal or family history of ovarian cancer. Similarly, the numbers among the 25 BRCA2 mutation carriers were 14 (56%) and 21 (84%), respectively. For PALB2, one of four (25%) and none of the mutation carriers had a personal or family history of breast or ovarian cancer, respectively.
Probability (%) that probands affected with pancreatic cancer (PC) will test positive for a deleterious mutation in BRCA1, BRCA2, PALB2 , or CDKN2A , if from kindreds with various cancer family histories. Number with PC includes proband. Sizes of sample subsets from which probabilities were estimated are shown in parentheses. FDR, first-degree relatives.
We also examined age-at-onset differences by mutation carrier status among 710 probands who had all four gene tests and available age data. Forty-five carried deleterious mutations and were younger than the others (P = 0.03); median ages were 60 (range: 42–93) and 65 (20–95) years, respectively.
Discussion
In this large study, we provided a comprehensive analysis of germ-line mutations occurring in the four genes BRCA1, BRCA2, PALB2, and CDKN2A among FPC probands. With the exception of one FPC proband and one familial non-FPC proband, the vast majority of tested individuals carry only one germ-line mutation in these four genes. We found that 8% of probands who have an FDR with pancreatic cancer (and therefore meet the definition of FPC) harbor a deleterious mutation in one of these four genes and that even probands who have a biological relative other than an FDR with pancreatic cancer may carry a deleterious mutation, although with significantly less probability. We demonstrated that these genes together account for a total of ~5–10% of deleterious mutations in FPC. Overall, any proband with a positive family history of pancreatic cancer has a 6.7% probability of carrying a deleterious mutation in one of the genes. Mutations in BRCA2 and CDKN2A were detected more often than those in BRCA1 and PALB2, consistent with the published literature. We also found a younger age of onset among probands who carried a mutation in one of the four genes. Our study confirms and highlights the genetic heterogeneity of FPC. Thus, when genetic testing of probands is considered, multiple genes will need to be evaluated.
When family history of breast cancer, ovarian cancer, or melanoma is considered, there are varying ranges of probabilities; it is of interest that a proband with a family history of pancreatic cancer and any of the three other cancers has an 8.7% probability of carrying a mutation. Because FPC probands are increasingly referred for genetic risk assessment, we aggregated in Figure 1 selected family history scenarios from our data that will help inform the probability of genetic test outcomes.
With respect to genetic testing of probands, our data can inform the strategy to identify particular FPC individuals as candidates for genetic testing and whose families could potentially benefit from genetic risk assessment. We found that, gene for gene, significantly more deleterious mutations were found in FPC kindreds than in familial non-FPC kindreds. As such, the yield of identifying a mutation would be greatest among those whose kindreds meet the criteria for FPC. Interestingly, the number of family members affected with pancreatic cancer in a kindred did not correlate with the probability of detecting deleterious mutations (Supplementary Table S2 online). We could not confidently explore this relationship in the familial non-FPC cases because of the smaller number of mutations detected.
Previous studies have emphasized the importance of family history in pancreatic cancer risk12,36 and increased incidence of early pancreatic lesions detected via early screening measures.37 Although our findings could lend promise toward use of genetic testing in early pancreatic cancer screening,38 many questions remain regarding how to appropriately translate this into the clinical setting for genetically high-risk individuals.3
In addition to informing genetic counseling, this report provides perhaps the most comprehensive mutation analysis of PALB2 and CDKN2A in the familial setting. We utilized conventional methods and available databases from Myriad Genetic Laboratories as well as the research community at large to determine the classification of deleterious mutations, VUS, and single-nucleotide polymorphisms. We identified four novel deleterious mutations and 15 VUS among these four genes. It is of interest that half of the novel VUS were seen in PALB2, and that three-fourths of all VUS detected were seen in CDKN2A and PALB2. It may be that our classification criteria are more conservative, as there is limited knowledge of PALB2 mutations and pancreatic cancer because it is the least characterized of the four genes. Similarly, the experience of CDKN2A has been focused on probands with melanoma ascertained through FAMMM or familial melanoma kindreds. As can be expected, studies of familial melanoma contributed to the classification of deleterious mutations in CDKN2A; our study focused on CDKN2A mutations ascertained through FPC. It is worth noting that half of the probands who carried CDKN2A deleterious mutations did not have a personal or family history of melanoma. Our data also provide a contrast to what is seen among sporadic patients with pancreatic cancer: among FPC probands, the prevalence of deleterious mutations is nearly fivefold higher (2.5 vs. 0.6%).29 The relatively large numbers of mutations and VUS detected in both genes warrant further research to determine whether the VUS should be reclassified as deleterious mutations. However, in our study, we noted no significant difference of BRCA2 mutation prevalence between probands from FPC versus familial non-FPC kindreds. BRCA2 germ-line mutations have also been detected in sporadic pancreatic cancers for which family pedigrees were not suggestive of an inherited predisposition.39 Taken together, varying penetrance may potentially explain the noted increased prevalence of deleterious CDKN2A mutations. Until further studies clarify these aspects, recognition of our limited knowledge of PALB2 and CDKN2A is important when counseling families presenting with FPC, who may harbor mutations in these two genes and for which the significance has yet to be elucidated.
We ascertained probands for this study through their diagnosis of pancreatic cancer and family history of pancreatic cancer. Analysis of family histories could qualify some of the families to meet criteria for hereditary and ovarian breast cancer and FAMMM, but a number of probands who tested positive for the mutations in genes associated with these cancer syndromes would not be considered as having these syndromes by cancer family history. This finding provides an opportunity to broaden the scope of these classic syndromes and for further characterization of the spectrum of cancer risk and penetrance estimates or, alternatively, to redefine pleiotropic manifestations of the genes.
The large number of probands with a family history of pancreatic cancer from multiple sites is a significant strength in estimating the prevalence of mutations in these four genes. Other strengths include the detailed information regarding personal and family history of breast and ovarian cancers and melanoma. The DNA samples were all tested under Clinical Laboratory Improvement Amendments standard conditions at the Myriad Genetics laboratory, which assured consistent quality of processing protocols, clear criteria for mutation and variant assessments, and utilization of several mutation databases.
There are also several limitations. First, although BART was used, not all deletions and duplications were comprehensively tested for in BRCA1 and BRCA2. Also, duplications and deletions were not tested for in PALB2 and CDKN2A. Second, a number of probands had missing demographic information regarding Ashkenazi Jewish heritage, potentially important for further stratifying risk of pancreatic cancer development in this ethnic group. We did not have the data to adequately interrogate cancer risk in BRCA1 or BRCA2 mutation carriers of Ashkenazi Jewish heritage. Third, we did not test for mutations in mismatch repair genes associated with Lynch syndrome. Although mutations in these genes confer increased risk for pancreatic cancer, the risk is more moderate compared with the four genes we did report.5 Fourth, some of the sites may have excluded potential probands with already-known gene mutations. The estimated prevalence we present here is therefore an underestimate. At this time, we cannot firmly fix the degree of underestimation because the exclusions were not systematic. Future studies should identify other subject characteristics or risk factors that may assist in selecting appropriate affected individuals for genetic testing with the ultimate hope that this will enhance ongoing efforts toward an effective clinical strategy for screening high-risk individuals for pancreatic cancer.40
In this comprehensive study of germ-line mutations in BRCA1, BRCA2, PALB2, and CDKN2A in a sample of probands with FPC, we have confirmed genetic heterogeneity and that a greater proportion of mutations occur in BRCA2 and CDKN2A. Our data suggest there is a role for genetic testing in high-risk FPC families, especially those containing at least two FDRs, supporting proposals made in previous pancreatic cancer screening guidelines.3 Further studies will elucidate the functional relevance of FPC genes as well as their potential interplay with complex intracellular pathways in the pathogenesis of pancreatic cancer.
Disclosure
R.H.H., M.G.G., and A.P.K. receive royalty payments from Myriad Genetics for the PALB2 invention under an agreement through Johns Hopkins University. L.A.C.-A. collaborated with Myriad on gene discovery and receives royalties for BRCA1, BRCA2, and CDKN2A clinical testing under an agreement with the University of Utah. The other authors declare no conflict of interest.
References
Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics, 1975–2011. National Cancer Institute: Bethesda, MD, 2014. http://seer.cancer.gov/csr/1975_2011/. Accessed April 2014.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM . Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913–2921.
Canto MI, Harinck F, Hruban RH, et al.; International Cancer of Pancreas Screening (CAPS) Consortium. International Cancer of the Pancreas Screening (CAPS) Consortium summit on the management of patients with increased risk for familial pancreatic cancer. Gut 2013;62:339–347.
Klein AP . Identifying people at a high risk of developing pancreatic cancer. Nat Rev Cancer 2013;13:66–74.
Klein AP . Genetic susceptibility to pancreatic cancer. Mol Carcinog 2012;51:14–24.
Thompson D, Easton DF ; Breast Cancer Linkage Consortium. Cancer Incidence in BRCA1 mutation carriers. J Natl Cancer Inst 2002;94:1358–1365.
Breast Cancer Linkage Consortium. Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 1999;91:1310–1316.
Lynch HT, Deters CA, Snyder CL, et al. BRCA1 and pancreatic cancer: pedigree findings and their causal relationships. Cancer Genet Cytogenet 2005;158:119–125.
Iqbal J, Ragone A, Lubinski J, et al.; Hereditary Breast Cancer Study Group. The incidence of pancreatic cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer 2012;107:2005–2009.
Lucas AL, Frado LE, Hwang C, et al. BRCA1 and BRCA2 germline mutations are frequently demonstrated in both high-risk pancreatic cancer screening and pancreatic cancer cohorts. Cancer 2014;120:1960–1967.
Al-Sukhni W, Rothenmund H, Borgida AE, et al. Germline BRCA1 mutations predispose to pancreatic adenocarcinoma. Hum Genet 2008;124:271–278.
Lal G, Liu G, Schmocker B, et al. Inherited predisposition to pancreatic adenocarcinoma: role of family history and germ-line p16, BRCA1, and BRCA2 mutations. Cancer Res 2000;60:409–416.
Axilbund JE, Argani P, Kamiyama M, et al. Absence of germline BRCA1 mutations in familial pancreatic cancer patients. Cancer Biol Ther 2009;8:131–135.
Murphy KM, Brune KA, Griffin C, et al. Evaluation of candidate genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial pancreatic cancer: deleterious BRCA2 mutations in 17%. Cancer Res 2002;62:3789–3793.
Couch FJ, Johnson MR, Rabe KG, et al. The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiol Biomarkers Prev 2007;16:342–346.
Stadler ZK, Salo-Mullen E, Patil SM, et al. Prevalence of BRCA1 and BRCA2 mutations in Ashkenazi Jewish families with breast and pancreatic cancer. Cancer 2012;118:493–499.
Lucas AL, Shakya R, Lipsyc MD, et al. High prevalence of BRCA1 and BRCA2 germline mutations with loss of heterozygosity in a series of resected pancreatic adenocarcinoma and other neoplastic lesions. Clin Cancer Res 2013;19:3396–3403.
Drew Y, Mulligan EA, Vong WT, et al. Therapeutic potential of poly(ADP-ribose) polymerase inhibitor AG014699 in human cancers with mutated or methylated BRCA1 or BRCA2. J Natl Cancer Inst 2011;103:334–346.
Lowery MA, Kelsen DP, Stadler ZK, et al. An emerging entity: pancreatic adenocarcinoma associated with a known BRCA mutation: clinical descriptors, treatment implications, and future directions. Oncologist 2011;16:1397–1402.
Xia B, Sheng Q, Nakanishi K, et al. Control of BRCA2 cellular and clinical functions by a nuclear partner, PALB2. Mol Cell 2006;22:719–729.
Xia B, Dorsman JC, Ameziane N, et al. Fanconi anemia is associated with a defect in the BRCA2 partner PALB2. Nat Genet 2007;39:159–161.
Jones S, Hruban RH, Kamiyama M, et al. Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science 2009;324:217.
Slater EP, Langer P, Niemczyk E, et al. PALB2 mutations in European familial pancreatic cancer families. Clin Genet 2010;78:490–494.
Harinck F, Kluijt I, van Mil SE, et al. Routine testing for PALB2 mutations in familial pancreatic cancer families and breast cancer families with pancreatic cancer is not indicated. Eur J Hum Genet 2012;20:577–579.
Grant RC, Al-Sukhni W, Borgida AE, et al. Exome sequencing identifies nonsegregating nonsense ATM and PALB2 variants in familial pancreatic cancer. Hum Genomics 2013;7:11.
Goldstein AM, Fraser MC, Struewing JP, et al. Increased risk of pancreatic cancer in melanoma-prone kindreds with p16INK4 mutations. N Engl J Med 1995;333:970–974.
Bartsch DK, Sina-Frey M, Lang S, et al. CDKN2A germline mutations in familial pancreatic cancer. Ann Surg 2002;236:730–737.
Harinck F, Kluijt I, van der Stoep N, et al. Indication for CDKN2A-mutation analysis in familial pancreatic cancer families without melanomas. J Med Genet 2012;49:362–365.
McWilliams RR, Wieben ED, Rabe KG, et al. Prevalence of CDKN2A mutations in pancreatic cancer patients: implications for genetic counseling. Eur J Hum Genet 2011;19:472–478.
Petersen GM, de Andrade M, Goggins M, et al. Pancreatic cancer genetic epidemiology consortium. Cancer Epidemiol Biomarkers Prev 2006;15:704–710.
Frank TS, Deffenbaugh AM, Reid JE, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 2002;20:1480–1490.
Hendrickson BC, Judkins T, Ward BD, et al. Prevalence of five previously reported and recurrent BRCA1 genetic rearrangement mutations in 20,000 patients from hereditary breast/ovarian cancer families. Genes Chromosomes Cancer 2005;43:309–313.
Judkins T, Rosenthal E, Arnell C, et al. Clinical significance of large rearrangements in BRCA1 and BRCA2. Cancer 2012;118:5210–5216.
Richards CS, Bale S, Bellissimo DB, et al. ACMG recommendations for standards for interpretation and reporting of sequence variations: revisions 2007. Genet Med 2008;10:294–300.
McWilliams RR, Bamlet WR, de Andrade M, et al. Polymorphic variants in hereditary pancreatic cancer genes are not associated with pancreatic cancer risk. Cancer Epidemiol Biomarkers Prev 2009;18:2549–2552.
Klein AP, Brune KA, Petersen GM, et al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res 2004;64:2634–2638.
Langer P, Kann PH, Fendrich V, et al. Five years of prospective screening of high-risk individuals from families with familial pancreatic cancer. Gut 2009;58:1410–1418.
Verna EC, Hwang C, Stevens PD, et al. Pancreatic cancer screening in a prospective cohort of high-risk patients: a comprehensive strategy of imaging and genetics. Clin Cancer Res 2010;16:5028–5037.
Goggins M, Schutte M, Lu J, et al. Germline BRCA2 gene mutations in patients with apparently sporadic pancreatic carcinomas. Cancer Res 1996;56:5360–5364.
Lennon AM, Wolfgang CL, Canto MI, et al. The early detection of pancreatic cancer: what will it take to diagnose and treat curable pancreatic neoplasia? Cancer Res 2014;74:3381–3389.
Acknowledgements
The authors thank the probands and their families. They also thank study assistants Ryan Wuertz, Bridget Eversman, Sarah Amundson, Megan Reichmann, Denesia Parris, Chinedu Ukaegbu, Chelsea Michael, and Diane Echavarria, for their contributions to the study. The Pancreatic Cancer Genetic Epidemiology (PACGENE) Consortium is funded by National Cancer Institute (NCI) grant R01 CA97075. Other funding support for this study includes National Institutes of Health NCI SPORE grants P50 CA102701 and P50 CA62924, Susan Wojcicki, Dennis Troper, grant K24113433, the Sol Goldman Pancreatic Cancer Research Center (grants N01-PC35145 and P30 CA22453), the Karp Family H.H. & M. Metals, Inc. Fund, the Sheikh Ahmed Center for Pancreatic Cancer Research, and the American Association for Cancer Research Innovation (grant 11-60-25-CANN, awarded to L.A.C.-A.). This work was presented at the American Society of Human Genetics annual meeting, Boston, MA, 24 October 2013.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Tables
(DOC 72 kb)
Rights and permissions
About this article
Cite this article
Zhen, D., Rabe, K., Gallinger, S. et al. BRCA1, BRCA2, PALB2, and CDKN2A mutations in familial pancreatic cancer: a PACGENE study. Genet Med 17, 569–577 (2015). https://doi.org/10.1038/gim.2014.153
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2014.153
Keywords
This article is cited by
-
Genetic and other risk factors for pancreatic ductal adenocarcinoma (PDAC)
Familial Cancer (2024)
-
Das familiäre Pankreaskarzinomsyndrom
Die Chirurgie (2023)
-
Significance of prostate/pancreatic/skin cancer family history for detecting BRCA2 pathogenic variant careers among patients with breast cancer
Breast Cancer (2022)
-
Familial pancreatic cancer: who should be considered for genetic testing?
Irish Journal of Medical Science (1971 -) (2022)
-
Pancreatic mixed acinar–neuroendocrine carcinoma in a patient with a germline BRCA2 mutation: a case report
Clinical Journal of Gastroenterology (2022)