Abstract
Purpose:
“Jaffe–Campanacci syndrome” describes the complex of multiple nonossifying fibromas of the long bones, mandibular giant cell lesions, and café-au-lait macules in individuals without neurofibromas. We sought to determine whether Jaffe–Campanacci syndrome is a distinct genetic entity or a variant of neurofibromatosis type 1.
Methods:
We performed germline NF1, SPRED1, and GNAS1 (exon 8) mutation testing on patients with Jaffe–Campanacci syndrome or Jaffe–Campanacci syndrome–related features. We also performed somatic NF1 mutation testing on nonossifying fibromas and giant cell lesions.
Results:
Pathogenic germline NF1 mutations were identified in 13 of 14 patients with multiple café-au-lait macules and multiple nonossifying fibromas or giant cell lesions (“classical” Jaffe–Campanacci syndrome); all 13 also fulfilled the National Institutes of Health diagnostic criteria for neurofibromatosis type 1. Somatic NF1 mutations were detected in two giant cell lesions but not in two nonossifying fibromas. No SPRED1 or GNAS1 (exon 8) mutations were detected in the seven NF1-negative patients with Jaffe–Campanacci syndrome, nonossifying fibromas, or giant cell lesions.
Conclusion:
In this study, the majority of patients with café-au-lait macules and nonossifying fibromas or giant cell lesions harbored a pathogenic germline NF1 mutation, suggesting that many Jaffe–Campanacci syndrome cases may actually have neurofibromatosis type 1. We provide the first proof of specific somatic second-hit mutations affecting NF1 in two giant cell lesions from two unrelated patients, establishing these as neurofibromatosis type 1–associated tumors.
Genet Med 16 6, 448–459.
Similar content being viewed by others
Introduction
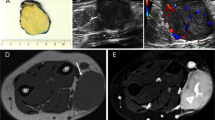
The term “Jaffe–Campanacci syndrome” (JCS) was coined in 1982 to describe the complex of multiple nonossifying fibromas (NOFs) of the long bones, giant cell granulomas of the jaw, and café-au-lait macules (CALMs) in individuals without neurofibromas; additional variable features included intellectual disability, precocious puberty, congenital blindness, and kyphoscoliosis.1,2,3 The possibility that JCS is a form of neurofibromatosis type 1 (NF1), an autosomal-dominant disorder with CALMs and deregulated tissue growth, has been suggested4 but never resolved. Nonossifying fibromas are common benign bone lesions typically observed in the second decade of life and are predominantly found in the lower extremities. Most are asymptomatic and regress spontaneously. Giant cell granulomas of the jaw are benign bone lesions observed in the second and third decade of life and are predominantly located in the mandible. They are not inflammatory in nature and are more appropriately termed aggressive (or nonaggressive) “giant cell lesions” based on established clinical and radiographic criteria.5,6 The lesions are most commonly solitary but may be multiple.7 Only 18 cases of JCS have been published in the English literature, including four cases in which an initial diagnosis of NF1 was overturned in favor of JCS (see Supplementary Table S1 online). Multiple bilateral NOFs of the long bones are a consistent feature in JCS, whereas CALMs have been present in most, but not all, reported individuals. Relatively few jaw lesions have been identified. Extraskeletal abnormalities, when present, are not consistent. Reports of JCS have appeared primarily in the orthopedic, radiology, and pathology literature. In most reports of JCS, a diagnosis of NF1 has been considered but was usually dismissed because of the absence of neurofibromas, a hallmark of NF1. However, 16 out of 18 individuals reported with JCS were younger than 18 years of age, and hence, they may not yet have developed neurofibromas (see Supplementary Table S1 online), which typically appear in early adolescence. It is not uncommon to see adolescents and young adults harboring a known germline NF1 mutation without any neurofibromas.8 There has even been one specific in-frame deletion found (c.2970_2972delAAT) that is associated with a milder phenotype lacking dermal neurofibromas.9 Many of the JCS accounts lack documentation of slit-lamp (Lisch nodules) and skin (café-au-lait macules, freckling) examinations, evaluation of family history, or consideration of the consensus criteria for the diagnosis of NF1, even for reports published after 1988 when the National Institutes of Health (NIH) criteria were established.10 To date, no consensus criteria exist to diagnose JCS, and NF1 genetic testing was pursued in only one4 of the previously published case reports. All cases were sporadic.
There are many accounts in the English literature that describe an association between NF1 and multiple NOFs, the first dating to 1948 (see Supplementary Table S2 online). To our knowledge, only one study has reported a germline mutation in NF1 in patients with NOFs.4 In the English literature, there are eight case reports in seven publications of NF1 patients with either solitary or multifocal giant cell lesions of the jaw (see Supplementary Table S3 online); in many of these reports, no imaging of the long bones was performed or reported (see Supplementary Table S3 online). Three of these studies found an NF1 mutation in blood and/or in the giant cell lesion or in the giant cell lesion–like lesion: (i) a case study of an 11-year-old girl carrying the NF1 splice mutation c.4268A>G with a giant cell lesion of the nasal bridge (but no evidence of biallelic inactivation of NF1 in the lesion, although only exon 24 of the NF1 gene was sequenced)11; (ii) a case study of a 10-year-old boy with cherubism secondary to multiple mandibular cysts with osteoclast-like giant cells and a splice mutation (IVS37+1G>A, exon 37) in NF1 in DNA from peripheral blood lymphocytes (jaw lesion DNA not sequenced),12 and (iii) a case study of a 7-year-old girl with NF1 and a recurrent giant cell lesion of her right mandible that demonstrated loss of heterozygosity for NF1 in the lesion.13 This latter case was the first with evidence of biallelic inactivation of NF1 in a giant cell lesion. Finally, there are three case reports of individuals diagnosed with NF1 (but who lack NF1 genetic testing) with both long bone and jaw lesions (see Supplementary Table S4 online).
Both Jaffe and Campanacci considered the likelihood that JCS is a form of neurofibromatosis.2,3 Solitary NOFs are common, and the incidence of multiple NOFs may be underestimated,14 raising the possibility of a simple coincidental presence of NOF in NF1 patients. Colby and Saul (2003)4 reported a case series of four individuals meeting consensus criteria for the diagnosis of NF110 who could, however, equally legitimately have been diagnosed with JCS. A partial deletion, not further specified, of NF1 was identified in one subject (patient CS4); the other three subjects had not undergone genetic testing at the time of the paper’s publication.4 To clarify the relationship of NOF, giant cell lesions, and JCS with NF1, we performed an extensive literature review, pursued further NF1 mutation analysis in previously published cases,4 reviewed all patients with solitary or multiple NOFs and/or giant cell lesions referred to the Center for Human Genetics at University Hospitals Leuven, and reviewed all patients referred for comprehensive NF1 testing to the Medical Genomics Laboratory at the University of Alabama Birmingham (UAB), due to the presence of at least one NOF and/or a suspected diagnosis of JCS. Given some similarities in pigment and bony abnormalities in NF1 and McCune–Albright syndrome, in individuals with negative NF1 mutation testing with JCS and/or NOF, we also performed sequencing of exon 8 of GNAS.15 Since Legius syndrome is only recently described and prominently features pigment abnormalities, we also performed SPRED1 sequencing.16
Materials and Methods
NF1 mutation analysis in patients described by Colby and Saul
For patients 1–3, comprehensive cDNA-based sequencing of NF1 was performed as previously described.17
Cell culture of NOFs and giant cell lesions and NF1 mutation detection
Surgically excised NOFs or giant cell lesions were digested at 37 °C overnight with collagenase (160 U/ml) and dispase (0.8 U/ml). Cells were grown to confluency in Dulbecco’s Modified Eagle Medium (Gibco, catalog no. 11995-065): Nutrient Mixture F-12 (Gibco, catalog no. 11765-054) + 10% fetal bovine serum (Atlanta Biologicals, catalog no. S11150) + penicillin + streptomycin (Gibco, catalog no. 15070-063) and harvested. NF1 mutation detection was performed essentially as previously reported.17
Retrospective review of patient samples with suspected JCS and/or NOF referred for NF1 testing to UAB Medical Genomics Laboratory
A phenotypic checklist (http://www.genetics.uab.edu/medgenomics), completed by the referring physician, accompanies each sample referred for comprehensive clinical NF1 testing to the UAB Medical Genomics Laboratory. Search for genotype–phenotype correlations using a Microsoft Access database containing deidentified phenotypic and mutation data was performed using JCS-related descriptors, including “nonossifying fibroma” (solitary or multiple), “giant cell granuloma” of the mandible (solitary or multiple), and the label “Jaffe–Campanacci syndrome.” Referring physicians were recontacted to confirm the accuracy of the previously submitted information as well as to obtain updated phenotypic information about the tested individuals, if available since the time genetic testing was performed. All NF1 mutation–negative patients (except for KUL-22) with JCS and/or NOF also underwent comprehensive SPRED1 genetic testing, as previously described.8,18 In addition, direct sequencing of GNAS1 exon 8 was performed after amplification using two pairs of primers: 8-1f: 5′-ggactctgagccctctttcc-3′, 8-1r: 5′-ggactggggtgaatgtcaag-3′ and 8-2f: 5′-gagcgatcaggtgtgcaaaa-3′, 8-2r: 5′-cagagggactggggtgaatg-3′. In addition, clinical and genetic data on five individuals diagnosed with JCS at the Center for Human Genetics from the University Hospitals Leuven (KUL) was reviewed and included. Descriptions of patients UAB/NIH-919 and KUL-1420 have been previously reported. This work was performed under the auspices of the institutional review boards of the respective participating institutions.
Results
NF1 mutation analysis in patients described by Colby and Saul
An NF1 mutation was found in each of the four individuals reported by Colby and Saul4 ( Table 1 ): a minor lesion mutation in patients CS1–CS3 and a deletion in patient CS4. The deletion in patient CS4 spanned 1.4 Mb indicative of a type 1 microdeletion.21
Thirteen of fourteen individuals with “classical” (multiple CALMs and multiple NOFs or giant cell lesions) JCS harbored pathogenic mutations in NF1
Table 1 lists, in addition to the four patients described by Colby and Saul4 (2003), 10 individuals with suspected JCS referred to UAB or KUL. Only individual UAB-19 did not harbor a mutation in NF1. If the definition of JCS is restricted to include patients with CALMs and NOFs or giant cell lesions and no neurofibromas (CS1, CS2, and UAB-19), as defined in the original reports,1,2 two of the three patients (CS1 and CS2) harbor a pathogenic mutation in NF1. We were not able to evaluate UAB-19 for NF1 mosaicism, which seems a likely diagnosis.
A second group of patients (UAB-12, KUL-14, and KUL-15 in Table 2 ) who did not have classical JCS but had CALMs and a single NOF of a long bone or a giant cell lesion of the jaw also met diagnostic criteria for NF1. In this group, all three (100%) had a pathogenic mutation in NF1. In summary, all patients (16/16) who met NF1 diagnostic criteria also harbored a pathogenic mutation in NF1. Five of the 16 patients (31%) with an NF1 mutation and at least one NOF or giant cell lesion had a history of pathologic fracture, in some cases requiring multiple orthopedic procedures. In the group with an NF1 mutation, we observed a male:female ratio of 11:5 with an age range of 2 months to 43 years at the time of NF1 genetic testing. Seven of the 16 individuals (42.7%) carried truncating NF1 mutations, five had splicing mutations (31.2%), two had a multiexon NF1 deletion (12.5%), one a total NF1 gene deletion (6.6%), and one (6.6%) a missense NF1 mutation. The distribution of mutations spanned the length of the NF1 gene.
Table 2 lists the nine individuals with NOFs of the long bones or giant cell lesions of the jaws. As noted above, three (UAB-12, KUL-14, and KUL-15) harbored pathogenic mutations in NF1. The remainder had one or two NOFs (patients UAB-16, UAB-17, UAB-18, and KUL-22), a single giant cell lesion and one NOF (patient UAB-21) or multiple lytic lesions but no CALMs (patient UAB-20). Of the six patients ( Table 2 ) without an NF1 mutation, we observed a male:female ratio of 2:4 with an age range of 9–15 years at last follow-up. Two of the six patients (33%) had a history of a pathological fracture. Short clinical descriptions of these six individuals are provided in the Supplementary Data online.
Cell culture of NOFs and giant cell lesions and NF1 mutation detection
Somatic NF1 mutations were detected in two giant cell lesions (patients KUL-14 and KUL-15; Table 1 ) but not in two NOFs (patient KUL-13; Table 1 and patient KUL-22; Table 2 ). However, it is possible that none of the NF1 two-hit cells in the NOFs enriched in tissue culture and were therefore undetectable.
Discussion
JCS is a controversial entity4 that features CALMs, NOFs, and/or giant cell lesions and a significant overlap with the NF1 phenotype. The majority of patients with a JCS diagnosis have been published in the orthopedic, radiography, or pathology literature (see Supplementary Table S1 online). NF1 genetic testing has been reported in only one case of JCS.4
We found germline NF1 mutations in 13 of 14 patients with multiple NOFs and multiple CALMs, a group that could be considered to have “classical” JCS ( Table 1 ). If the diagnosis of JCS is further constricted to include only those with multiple CALMs, multiple NOFs, and an absence of neurofibromas, as has been advocated,1,2 two of the three (patients 1 and 2) harbored pathogenic NF1 mutations. The third individual (UAB-19) may be mosaic for NF1, although this was not tested. A second group of three (patients UAB-12, KUL-14, and KUL-15) with a single NOF of a long bone or a giant cell lesion of the jaw met NF1 diagnostic criteria but were not considered to have “classical” JCS; all three patients had NF1 pathogenic mutations. The finding of multiple, bilateral NOFs in an individual with a germline NF1 mutation suggests that the NOFs arise secondary to biallelic inactivation of NF1, as predicted by the Knudson hypothesis, and as previously demonstrated in a number of NF1-related tumors and CALMs.22 However, we did not find such a somatic NF1 mutation in an NOF from patient 13, who harbored a germline NF1 mutation. The detection rate of somatic NF1 mutations in NF1-associated neurofibromas is high (~84%)23; however, the detection rate of somatic NF1 mutations in rarer NF1-associated tumors is unknown, but might be lower depending on the fraction of cells carrying a second hit in the NOF.22 As only one NOF was analyzed, no firm conclusions can be made at this point. However, we identified germline and somatic truncating NF1 mutations in both giant cell lesions from patients KUL-14 and KUL-15, establishing definitive genetic proof that these are NF1-associated tumors. This observation extends the previous finding of NF1 loss of heterozygosity in a mandibular giant cell lesion in a female NF1 patient by Friedrich et al.13
The 16 patients with at least one NOF or giant cell lesion and who met NF1 diagnostic criteria harbored a pathogenic NF1 mutation. These were distributed along the entire NF1 gene: no mutational hotspots were identified.24 Five nonsense, five splice-site, two multiexon deletions, two frameshift, one type 1 NF1 gene microdeletion, and one missense mutation were detected. All variants except the but the missense mutation are expected to result in haploinsufficiency or absence of NF1 and/or flanking gene products. One splice-site mutation (patient UAB-12) was the result of a de novo, novel AluSb1 insertion, as recently described,25 and would normally escape detection using exon-by-exon gDNA-based sequencing. There are only two well-documented examples of NF1 genotype/phenotype correlation: a three base-pair deletion of one amino acid (c.2970_2972delAAT in exon 17) that is associated with an absence of neurofibromas9 and the microdeletions of the NF1 gene (and a variable number of flanking genes) which are consistently associated with a more severe phenotype, including increased neurofibroma burden, learning disabilities, facial dysmorphism, and possible increased risk of malignant peripheral nerve sheath tumors.26,27 Given the wide spectrum of NF1 mutation type observed in this study, there was no obvious genotype–phenotype correlation, although the total number of patients is small.
The six patients without NF1, SPRED1, or exon 8 of GNAS1 mutations detected in the blood are a heterogeneous group and did not meet NF1 diagnostic criteria ( Table 2 ). Patients UAB-16, UAB-17, UAB-18, UAB-21, and KUL-22 have two or fewer NOFs and/or giant cell lesions and fewer than six CALMs. Since a single NOF is common in the general population,28 as is a single CALM,29 it is plausible that some of the patients may have a coincidental cluster of minor abnormalities. Patient UAB-17 had fibular dysplasia, a rare but well-characterized abnormality.30 The familial multiple CALMs without other features of NF1 in patient 16 is unexplained, despite mutation testing of NF1 and SPRED1.16 Patients UAB-19 and UAB-20 feature a more severe phenotype with multiple lytic lesions or NOFs in one or more legs; however, only UAB-19 can be considered as “true” JCS given her multiple CALM. She may be mosaic for an NF1 mutation. In patient UAB-20, it is unlikely that the bony lesions arose from NF1 mosaicism because no NF1 mutations were detected in cells cultured from the resected NOF of the left femur. Given the presence of so many aggressive lesions, an underlying genetic factor is presumed but unidentified. Multiple lytic foci of the mandible and femur in patients with a diagnosis of JCS have been reported previously (see Supplementary Table S1 online), but no mutational data were available from these patients.
The high percentage of pathologic fractures in our cohort (patients CS1, CS2, KUL-5, UAB/NIH-9, and KUL-13) almost certainly reflects an ascertainment bias for bone cysts among the NF1 patients, and systematic screening in NF1 patients for presence of NOFs has been suggested.4 Such screening needs to be balanced with the risk of radiation exposure in the pediatric (increased risk of leukemia)31 and NF1 populations (possible increased risk of malignant peripheral nerve sheath tumor).32 However, it seems reasonable to have a lower threshold to image sites of persistent bony pain in individuals with NF1.
The JCS diagnosis requires an absence of neurofibromas and the presence multiple CALMs, the latter a classical hallmark of NF1. This is especially problematic in children because neurofibromas typically do not appear until adolescence, or later. In many of the reports describing JCS, insufficient or inadequate phenotypic data were provided, hampering evaluation of the appropriateness of the diagnosis. In addition, there is no feature unique to JCS that must be present to distinguish it from other syndromes, including NF1. Axillary freckling, a specific finding in NF1, has also been reported in some patients with JCS.1,19 Since accurate diagnosis is essential to ensure appropriate medical management and genetic counseling, we recommend the clinical algorithm outlined in Figure 1 to be followed for patients presenting with multiple NOFs and/or giant cell lesions. The algorithm is derived from our data, which supports the hypothesis that JCS is frequently a manifestation of NF1.4 It also incorporates the hypothesis that a fraction of NF1 mutation–negative patients with multiple NOFs may be mosaic for an NF1 mutation. Formal consideration of a diagnosis of NF1 (and genetic testing, as needed) should prevent the “re-diagnosis” of JCS (from NF1) and its attendant confusion and avoid potentially missed screening opportunities (e.g., for optic pathway glioma in children). We recommend that the term “Jaffe–Campanacci syndrome” only be used for the likely small percentage of patients with multiple CALMs, multiple NOFs, and/or giant cell lesions who also lack a germline NF1 mutation or who lack evidence of an other recognized, usually distinct and rare disorder associated with NOFs and giant cell lesions ( Table 3 ). In these individuals, testing of melanocytes from multiple biopsies from CALMs for first and second hits in NF1, if available, is needed to exclude a diagnosis of mosaic NF1.33,34 It has been recognized recently that cherubism-associated giant cell lesions (and thus mutations in SH3BP2) result in loss of tankyrase-mediated destruction of adapter protein 3BP2 and thus stabilization and hyperactivation of SRC, SYK, and VAV pathways.35 The association of giant cell lesions with mutations in NF1 and PTPN11 ( Table 3 ), both members of the RAS signaling pathway, may provide additional insights to the pathogenesis of these tumors.
Proposed algorithm to evaluate patients with multiple nonossifying fibromas (NOFs) and/or giant cell lesions and café-au-lait macules (CALMs). The appearance of diagnostic features of neurofibromatosis type 1 (NF1) are time dependent, and thus a child who does not meet diagnostic criteria should be periodically re-evaluated. JCS, Jaffe–Campanacci syndrome; NIH, National Institutes of Health.
In conclusion, the majority of patients with CALMs and NOFs or giant cell lesions harbored a pathogenic germline NF1 mutation, suggesting that many JCS cases may actually have NF1. In addition, we provide the first proof of specific somatic second-hit mutations affecting NF1 in two giant cell lesions from two unrelated patients, establishing that these are NF1-associated tumors. The diagnosis of the JCS may apply to a small number of patients with multiple CALMs, multiple NOFs, and/or giant cell lesions who have undergone meticulous clinical evaluation to exclude other rare disorders associated with NOFs and giant cell lesions. In addition, comprehensive molecular analysis to exclude a germline NF1 mutation and, when possible, testing to exclude mosaic NF1 should be performed.
Disclosure
The authors declare no conflict of interest.
References
Mirra JM, Gold RH, Rand F . Disseminated nonossifying fibromas in association with café-au-lait spots (Jaffe-Campanacci syndrome). Clin Orthop Relat Res 1982;168:192–205.
Campanacci M, Laus M, Boriani S . Multiple non-ossifying fibromata with extraskeletal anomalies: a new syndrome? J Bone Joint Surg Br 1983;65:627–632.
Jaffe H . Tumors and Tumorous Conditions of the Bones and Joints. Lea and Febiger: Philadelphia, PA, 1958.
Colby RS, Saul RA . Is Jaffe-Campanacci syndrome just a manifestation of neurofibromatosis type 1? Am J Med Genet A 2003;123A:60–63.
Chuong R, Kaban LB, Kozakewich H, Perez-Atayde A . Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofac Surg 1986;44:708–713.
Ficarra G, Kaban LB, Hansen LS . Central giant cell lesions of the mandible and maxilla: a clinicopathologic and cytometric study. Oral Surg Oral Med Oral Pathol 1987;64:44–49.
de Lange J, van den Akker HP, van den Berg H . Central giant cell granuloma of the jaw: a review of the literature with emphasis on therapy options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:603–615.
Messiaen L, Yao S, Brems H, et al. Clinical and mutational spectrum of neurofibromatosis type 1-like syndrome. JAMA 2009;302:2111–2118.
Upadhyaya M, Huson SM, Davies M, et al. An absence of cutaneous neurofibromas associated with a 3-bp inframe deletion in exon 17 of the NF1 gene (c.2970-2972 delAAT): evidence of a clinically significant NF1 genotype-phenotype correlation. Am J Hum Genet 2007;80:140–151.
Neurofibromatosis. Conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol 1988;45:575–578.
Krammer U, Wimmer K, Wiesbauer P, et al. Neurofibromatosis 1: a novel NF1 mutation in an 11-year-old girl with a giant cell granuloma. J Child Neurol 2003;18:371–373.
van Capelle CI, Hogeman PH, van der Sijs-Bos CJ, et al. Neurofibromatosis presenting with a cherubism phenotype. Eur J Pediatr 2007;166:905–909.
Friedrich RE, Mautner VF, Scheuer HA . Loss of heterozygosity in tumor cells of a recurrent mandibular giant cell granuloma in neurofibromatosis type 1. Anticancer Res 2007;27(4A):2079–2083.
Moser RP Jr, Sweet DE, Haseman DB, Madewell JE . Multiple skeletal fibroxanthomas: radiologic-pathologic correlation of 72 cases. Skeletal Radiol 1987;16:353–359.
Weinstein LS, Shenker A, Gejman PV, Merino MJ, Friedman E, Spiegel AM . Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N Engl J Med 1991;325:1688–1695.
Brems H, Chmara M, Sahbatou M, et al. Germline loss-of-function mutations in SPRED1 cause a neurofibromatosis 1-like phenotype. Nat Genet 2007;39:1120–1126.
Messiaen LM, Callens T, Mortier G, et al. Exhaustive mutation analysis of the NF1 gene allows identification of 95% of mutations and reveals a high frequency of unusual splicing defects. Hum Mutat 2000;15:541–555.
Spencer E, Davis J, Mikhail F, et al. Identification of SPRED1 deletions using RT-PCR, multiplex ligation-dependent probe amplification and quantitative PCR. Am J Med Genet A 2011;155A:1352–1359.
Hau MA, Fox EJ, Cates JM, Brigman BE, Mankin HJ . Jaffe-Campanacci syndrome. A case report and review of the literature. J Bone Joint Surg Am 2002;84-A:634–638.
Legius E, Wu R, Eyssen M, Marynen P, Fryns JP, Cassiman JJ . Encephalocraniocutaneous lipomatosis with a mutation in the NF1 gene. J Med Genet 1995;32:316–319.
Kehrer-Sawatzki H . Structure of the NF1 gene region and mechanisms underlying gross NF1 deletions. In: Kaufmann D (ed). Neurofibromatoses, vol. 16. Karger: Basel, 2008:89–102.
De Raedt T, Maertens O, Serra E, Legius E . Somatic NF1 mutations in tumors and other tissues. In: Kaufmann D (ed). Neurofibromatoses, vol 16. Karger: Basel, 2008:143–153.
Maertens O, Brems H, Vandesompele J, et al. Comprehensive NF1 screening on cultured Schwann cells from neurofibromas. Hum Mutat 2006;27:1030–1040.
Messiaen LM, Wimmer K . NF1 mutational spectrum. In: Kaufmann D (ed). Neurofibromatoses. Karger: Basel, 2008:63–77.
Wimmer K, Callens T, Wernstedt A, Messiaen L . The NF1 gene contains hotspots for L1 endonuclease-dependent de novo insertion. PLoS Genet 2011;7:e1002371.
Tonsgard JH, Yelavarthi KK, Cushner S, Short MP, Lindgren V . Do NF1 gene deletions result in a characteristic phenotype? Am J Med Genet 1997;73:80–86.
De Raedt T, Brems H, Wolkenstein P, et al. Elevated risk for MPNST in NF1 microdeletion patients. Am J Hum Genet 2003;72:1288–1292.
Betsy M, Kupersmith LM, Springfield DS . Metaphyseal fibrous defects. J Am Acad Orthop Surg 2004;12:89–95.
Shah KN . The diagnostic and clinical significance of café-au-lait macules. Pediatr Clin North Am 2010;57:1131–1153.
Birch JG, Lincoln TL, Mack PW, Birch CM . Congenital fibular deficiency: a review of thirty years’ experience at one institution and a proposed classification system based on clinical deformity. J Bone Joint Surg Am 2011;93:1144–1151.
Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012;380:499–505.
Zadeh G, Buckle C, Shannon P, Massicotte EM, Wong S, Guha A . Radiation induced peripheral nerve tumors: case series and review of the literature. J Neurooncol 2007;83:205–212.
Maertens O, De Schepper S, Vandesompele J, et al. Molecular dissection of isolated disease features in mosaic neurofibromatosis type 1. Am J Hum Genet 2007;81:243–251.
De Schepper S, Maertens O, Callens T, Naeyaert JM, Lambert J, Messiaen L . Somatic mutation analysis in NF1 café au lait spots reveals two NF1 hits in the melanocytes. J Invest Dermatol 2008;128:1050–1053.
Levaot N, Voytyuk O, Dimitriou I, et al. Loss of Tankyrase-mediated destruction of 3BP2 is the underlying pathogenic mechanism of cherubism. Cell 2011;147:1324–1339.
Wolvius EB, de Lange J, Smeets EE, van der Wal KG, van den Akker HP . Noonan-like/multiple giant cell lesion syndrome: report of a case and review of the literature. J Oral Maxillofac Surg 2006;64:1289–1292.
Ueki Y, Tiziani V, Santanna C, et al. Mutations in the gene encoding c-Abl-binding protein SH3BP2 cause cherubism. Nat Genet 2001;28:125–126.
Ardinger HH, Horii KA, Begleiter ML . Expanding the phenotype of oculoectodermal syndrome: possible relationship to encephalocraniocutaneous lipomatosis. Am J Med Genet A 2007;143A:2959–2962.
Moog U . Encephalocraniocutaneous lipomatosis. J Med Genet 2009;46:721–729.
Pina-Neto JM, Moreno AF, Silva LR, et al. Cherubism, gingival fibromatosis, epilepsy, and mental deficiency (Ramon syndrome) with juvenile rheumatoid arthritis. Am J Med Genet 1986;25:433–441.
Groesser L, Herschberger E, Ruetten A, et al. Postzygotic HRAS and KRAS mutations cause nevus sebaceous and Schimmelpenning syndrome. Nat Genet 2012;44:783–787.
Orhan E, Erol S, Deren O, Sevin A, Ekici O, Erdogan B . Idiopathic bilateral central giant cell reparative granuloma of jaws: a case report and literature review. Int J Pediatr Otorhinolaryngol 2010;74:547–552.
Hennekam R, Allanson J, Krantz I, et al. Syndromes of the Head and Neck, 5th edn. Oxford University Press: New York, 2010:564.
Acknowledgements
This work was supported by internal funds from the Medical Genomics Laboratory at the University of Alabama Birmingham, the Hayward Foundation (MRW laboratory), the Division of Intramural Research of the National Human Genome Research Institute (NHGRI), the Division of Cancer Epidemiology and Genetics of the National Cancer Institute’s Intramural Research Program, and in part with federal funds from the National Cancer Institute, National Institutes of Health. H.B. is a postdoctoral researcher of the Research Foundation Flanders (FWO) at the KULeuven. The authors thank Kathleen Freson (Molecular and Vascular Biology, KULeuven) for GNAS1 mutation analysis. E.L. is supported by the Clinical Research Foundation of the University Hospitals Leuven and by a grant from the FWO-Vlaanderen (G057806N).
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Author information
Authors and Affiliations
Corresponding authors
Supplementary information
Supplementary Table S1
(XLS 56 kb)
Supplementary Table S2
(XLS 59 kb)
Supplementary Table S3
(XLS 53 kb)
Supplementary Table S4
(XLS 50 kb)
Supplementary Data
(DOC 38 kb)
Rights and permissions
About this article
Cite this article
Stewart, D., Brems, H., Gomes, A. et al. Jaffe–Campanacci syndrome, revisited: detailed clinical and molecular analyses determine whether patients have neurofibromatosis type 1, coincidental manifestations, or a distinct disorder. Genet Med 16, 448–459 (2014). https://doi.org/10.1038/gim.2013.163
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2013.163
Keywords
This article is cited by
-
Novel, heterozygous, de novo pathogenic variant (c.4963delA: p.Thr1656Glnfs*42) of the NF1 gene in a Chinese family with neurofibromatosis type 1
BMC Medical Genomics (2023)
-
Novel, heterozygous, pathogenic variant (c.4272delA: p.I1426Ffs*2) for the NF1 gene in a large Chinese family with neurofibromatosis type 1
Molecular Biology Reports (2023)
-
Update of pediatric bone tumors: osteogenic tumors and osteoclastic giant cell-rich tumors
Skeletal Radiology (2023)
-
Jaffe-Campanacci syndrome or neurofibromatosis type 1: a case report of phenotypic overlap with detection of NF1 gene mutation in non-ossifying fibroma
Italian Journal of Pediatrics (2020)
-
Intracranial arterial dolichoectasia and skull damage in a girl with Jaffe-Campanacci syndrome: a case report
Child's Nervous System (2019)