Abstract
Purpose:
Because diagnosis of Marfan syndrome is difficult during infancy, we used a large cohort of children to describe the evolution of the Marfan syndrome phenotype with age.
Methods:
Two hundred and fifty-nine children carrying an FBN1 gene mutation and fulfilling Ghent criteria were compared with 474 non-Marfan syndrome children.
Results:
Prevalence of skeletal features changed with aging: prevalence of pectus deformity increased from 43% at 0–6 years to 62% at 15–17 years, wrist signs increased from 28 to 67%, and scoliosis increased from 16 to 59%. Hypermobility decreased from 67 to 47% and pes planus decreased from 73 to 65%. Striae increased from 2 to 84%. Prevalence of ectopia lentis remained stable, varying from 66 to 72%, similar to aortic root dilatation (varying from 75 to 80%). Aortic root dilatation remained stable during follow-up in this population receiving β-blocker therapy. When comparing Marfan syndrome children with non-Marfan syndrome children, height appeared to be a simple and discriminant criterion when it was >3.3 SD above the mean. Ectopia lentis and aortic dilatation were both similarly discriminating.
Conclusion:
Ectopia lentis and aortic dilatation are the best-discriminating features, but height remains a simple discriminating variable for general practitioners when >3.3 SD above the mean. Mean aortic dilatation remains stable in infancy when children receive a β-blocker.
Genet Med 2014:16(3):246–250
Similar content being viewed by others
Introduction
Marfan syndrome (MFS; OMIM 154700) is a connective tissue disorder with autosomal dominant inheritance caused mostly by mutations in the protein fibrillin 1 gene (FBN1).1 MFS is characterized by a broad range of clinical manifestations involving the skeletal, ocular, cardiovascular, integumental, pulmonary, and central nervous systems, and shows great phenotypic variability.2,3 Cardiovascular involvement in the form of aortic aneurysm or dissecting aorta is the most serious life-threatening aspect of the syndrome. The succession of classifications (Berlin, Ghent 1, and Ghent 2) illustrates the difficulty in diagnosis.4,5,6,7 Although the phenotype in adults is becoming well documented, data in children are much rarer because of marked phenotypic variability both between and within families, and incomplete phenotype in the young, limiting effectiveness of familial screening in children in the absence of molecular biology. Therefore, child populations examined in earlier reports were possibly biased toward severe phenotypes.
Our objective was to describe the evolution of the Marfan syndrome phenotype with age and compare this phenotype with a population of children consulting for a suspicion of Marfan syndrome.
Materials and Methods
All subjects <18 years of age who came to the French national reference outpatient clinic devoted to Marfan syndrome and related disorders (CNR Marfan) between 1995 and 2010 were considered for this study. Children came to our clinic either because they were referred by a physician for suspicion of Marfan syndrome or because they were relatives of Marfan patients (familial screening is systematic). All patients, or their relatives when they were under the age of 18, signed an informed consent form. Neonatal forms of Marfan syndrome were not included because they have a different prognosis and clinical picture.8
In our center, patients were evaluated by a geneticist, an ophthalmologist, a cardiologist, and a pediatrician. Physical findings included skeletal features used for the diagnosis of Marfan syndrome: scoliosis, pectus deformity, pes planus, arm span/height ratio, and positive thumb-and-wrist sign. Systematic slit-lamp examination, cardiac ultrasonography, and radiological investigations in children older than 6 years of age (radiographs of pelvis, anteroposterior and lateral dorsolumbar spine, chest, and left hand and wrist for evaluation of the bone age) were also performed. In addition to specific Marfan features, pediatricians also checked for height and weight. Bone age was estimated during consultation and compared with the atlas of Greulich and Pyle.9 Aortic root dilatation refers to dilatation at the sinuses of valsalva.
Characteristics of children are reported by age stratum (0–6, 7–9, 10–14, and 15–17 years of age). Follow-up visits (yearly visits between 1995 and 2001 and a visit every 2 years thereafter), including the same workup, were proposed when MFS was diagnosed or could not be ruled out.
FBN1 mutation screening was performed when the family mutation was already recognized (familial screening) or for diagnostic purposes when a child presented at least one major and one minor criteria, in two different systems.3
All children who fulfilled the Ghent 1 criteria at any time during their follow-up4 were included in the “MFS group” if carrying an FBN1 gene mutation. All children evaluated during the same period and in whom MFS could be ruled out, either because they did not carry the familial mutation or because MFS could be definitively ruled out at the age of 18, were included in the “non-MFS group.” Other children (those with undetermined status regarding MFS and those with MFS according to the Ghent criteria—without FBN1 mutation) were excluded from the analysis, but the features observed in MFS according to the Ghent criteria (without FBN1 mutation) are reported.
Statistical analysis
Characteristics of children during the first visit are reported by age stratum. Those characteristics are expressed using frequencies and percentages for categorical variables and using means and SD for continuous variables. Height and weight were compared with the normal value adapted from Sempe.10 Comparisons between MFS and non-MFS children were performed in each stratum of age for categorical variables using χ2 or Fisher’s exact test as appropriate, and for continuous variables using Student’s t-test or Wilcoxon rank-sum test as appropriate. Proband children were compared with nonproband children using the same methodology. The significance level was 5%.
To identify discriminative factors for the diagnosis of MFS in children, potential diagnosis factors were subjected to a decision-tree classification method based on recursive partitioning analysis. Two decision-tree models of the classification and regression tree type were built for each age stratum. Each child could contribute to more than one age stratum but only once in each age stratum (first visit during this stratum). First, the regression trees were built by cross-validation, which is the first pruning method. Subsequently, the complexity parameter of 0.01 was used by default for all regression trees.
A first model was developed including only simple clinical features available to a general practitioner: height, expressed as Z score (SD above the mean), arm span/height ratio, hypermobility (Beighton scale), pectus deformity, thumb sign, wrist sign, angle of the scoliosis (in degrees), and presence of striae. A second model included ectopia lentis, mitral valve prolapse, and aortic diameter in addition.
Statistical analyses were performed using SAS software version 9.2 (SAS Institute, Cary, NC). The classification-and-regression trees were built with the “rpart” package, which implements classification and regression tree modeling using R software v.2.13 (The R Foundation for Statistical Computing).
Results
Population
Between 1995 and 2010, 1,238 children came to the CNR Marfan. Final diagnosis was MFS for 389 children who fulfilled the Ghent criteria for MFS4 (age at first visit was 8.6 ± 4.7 years, and 52.7% were boys). Among these, 259 carried an FBN1 gene mutation (age: 8.6 ± 4.6 years, 51.7% boys) and were included in the present study (MFS group). Age and sex ratios were similar to those of the 130 Marfan children without FBN1 mutation (age: 8.6 ± 4.9 years, 54.6% boys; MFS non-FBN1 group).
MFS could be definitely ruled out in 474 children (11.43 ± 4.68 years, 56.1% boys), whereas diagnosis remained uncertain in 375 children.
Clinical presentation
MFS group. At the first visit, 158/259 (61.0%) children had a family history of MFS. One hundred and three (39.8%) children came for the first visit when they were between 0 and 6 years, 49 (18.9%) between 7 and 9 years, 68 (26.2%) between 10 and 14 years, and 39 (15.1%) between 15 and 17 years of age. One hundred and one (39.0%) were probands.
Two deaths occurred before the age of 18 years, after a mean follow-up of 3.5 ± 3.5 years for all the patients:
-
A 17-year-old boy, who died 2 years after aortic dissection occurred at 15 years (aortic diameter at the sinuses of valsalva: 49 mm at 14 years) and
-
A 4-year-old boy, who died 1 month after surgery (aortic valve–sparing surgery and mitral valvuloplasty).
Including these patients, surgery was performed in 10 children before 18 years of age: seven patients had a replacement of the ascending aorta with valvular surgery at the same time, and three patients had mitral valve surgery alone.
MFS non-FBN1 group
Forty-eight (36.9%) children came for the first visit when they were between 0 and 6 years, 25 (19.2%) between 7 and 9 years, 40 (30.8%) between 10 and 14 years, and 17 (13.1%) between 15 and 17 years of age. In this population, five children had a mutation in the TGFBR2 gene and three had a mutation in the TGFBR1 gene; no mutation was found in the other children.
Non-MFS group
Four hundred and seventy-four children were in the non-MFS group, including 422 children not carrying the familial mutation and 52 children not fulfilling the Ghent criteria at 18 years of age. At first visit, mean age of non-MFS children was higher than that of MFS children (11.4 ± 4.7 vs. 8.6 ± 4.6 years), and distribution of children by age stratum was not similar in the two populations (P < 0.0001). By contrast, the sex ratio (boys:girls) was similar (1.3 vs. 1.1; P = 0.25).
Comparison between MFS and MFS non-FBN1 groups for Marfan features. In the MFS non-FBN1 group, only scoliosis >10° was more frequent (75.8 vs. 33.8%; P < 0.0001) than in the MFS group (see Supplementary Data online).
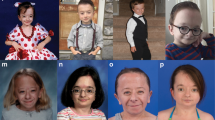
Comparison between MFS and non-MFS groups for Marfan features. Prevalence of Marfan clinical features included in the international nosology (Ghent 1) is presented in Figure 1 for both MFS and non-MFS groups and is detailed by age group in the Supplementary Data online. The evolution of prevalence of skeletal features in MFS children as a function of age stratum is represented in Figure 2 (see Supplementary Data online).
Evolution of the prevalence of different features by age group in the Marfan group. The percentages are provided for each feature and class of age. Comparisons were performed in each stratum of age for categorical variables using Cochrane–Armitage χ2 tests and for continuous variables using Student’s t-test or Wilcoxon rank-sum test as appropriate. NS, nonsignificant. #P < 0.05 and ≥0.0001; ‡P < 0.0001.
MFS children were significantly taller than non-MFS children (P < 0.0001 in all age strata). At the age of 17 years, mean height was 191.2 ± 8.4 cm (+2.9 SD) in MFS boys: 190.5 ± 10.9 cm (2.8 SD) in the MFS non-FBN1 group as compared with 183.6 ± 8.2 cm (+1.7 SD) in non-MFS boys and 178.3 ± 7.6 cm for MFS girls (+2.7 SD); 177.8 ± 7.7 cm (+2.6 SD) in the MFS non-FBN1 group as compared with 169.7 ± 6.6 cm (+1.2 SD) in non-MFS girls. No midparental height was calculated because many parents were in the MFS category, and the predicted height cannot be thus calculated. In the whole MFS group, height >3.3 SD above the mean carried a positive predictive value of 72% for MFS and a negative predictive value of 79%. Arm span/height ratio was higher in the MFS children (P < 0.0001 in all age strata). It increased steadily with aging in the MFS group. Prevalence of pectus deformity, even mild pectus, was more frequent in the MFS group (P < 0.0001 in all age strata). Its prevalence increased with age in the MFS group. Prevalence of thumbs sign (when young children cooperate) increased from 0–6 to 7–9 years, thereafter remaining stable. Wrist sign was more frequent in the MFS group (P < 0.0001 in all age strata). Its prevalence increased between age groups 7–9 and 10–14 years and remained stable thereafter in the MFS group, whereas it continued to increase in the non-MFS group. The severity (in terms of angle) of scoliosis greatly increased with age in MFS children, whereas it remained very low in the non-MFS children. Prevalence of moderate scoliosis (>10°) increased with age in both the MFS and the non-MFS children, earlier in girls than in boys in both populations. Prevalence of scoliosis exceeding 10° was 10 times greater in MFS versus non-MFS children for the 0–6 years age group and nearly three times greater for the 15–17 years age group. Prevalence of hypermobility and pes planus tended to decrease with age, whereas striae appeared toward the age of 10 years. Both these signs were more frequent in the MFS group (P < 0.0001 in all age strata).
Aortic root dilatation (defined as an aortic diameter >2 SD according to Roman)11 was the most frequent feature (present in 80% of the MFS group), and its prevalence remained stable across age strata; defining aortic dilatation as an aortic diameter >3 SD (as suggested in the Ghent 2 criteria)5 decreased its prevalence about 10 points throughout all age classes in both the MFS and the non-MFS groups. When the nomogram published by Gautier was used,12 prevalence of aortic dilatation (aortic diameter >2 SD) was 52.6% in the MFS group and 0.8% in the non-MFS group, also without modification with age.
Similarly, ectopia lentis was present from early infancy, and its prevalence remained stable across age strata.
Comparison between probands and nonprobands in the MFS group. In the various age strata, the percentage of probands was not the same. Probands were less represented in the 0–6 years (35.0%) and 10–14 years (35.3%) groups, whereas they represented >46% in the other age strata. As expected, probands were more severely affected than nonprobands: pectus deformity was more frequent (61.1 vs. 33.3%; P = 0.007) at 0–6 years. Height was greater only in male probands at 10–14 years (4.4 ± 1.2 SD above the mean vs. 3.5 ± 1.7; P = 0.04) and 15–17 years (3.2 ± 1.2 SD above the mean vs. 2.4 ± 1.5; P = 0.02). Similarly, the aortic diameter was significantly greater in probands (4.8 ± 2.7 SD above the mean vs. 3.4 ± 1.7; P < 0.0001); it was also significant by age group. Mitral valve prolapse was more frequent (72.3 vs. 51.7%; P < 0.03) in the 15–17 year age group. Aortic dilatation (defined as an aortic diameter >2 SD according to Roman) was significantly more frequent in probands in the 0–6, 10–14, and 15–17 year classes. Prevalence of ectopia lentis was also greater in probands, particularly in the 0–6 and 15–17 year age groups.
Aortic root diameter within the MFS group. In the MFS group, all patients were treated with β–blockers; mean aortic root diameter increased with age (24.5 ± 4.4 mm between 0 and 6 years, 28.8 ± 3.3 mm between 7 and 9 years, 33.7 ± 5.3 between 10 and 14 years, and 37.6 ± 5.4 between 15 and 17 years of age). However, the importance of dilatation as evaluated by the Z score using the Roman nomogram remained stable (see Supplementary Data online) above the mean normal value.
Discriminating features between MFS and non-MFS children. The features that best discriminated between MFS and non-MFS children in different age classes are shown in the regression trees (see Supplementary Data online). Height was the most discriminating clinical parameter in the simple clinical model, with up to 65% of children correctly classified when height was >3.3 SD above the mean (2.5 SD for 0- to 6-year-old children, 2.3 SD for 7- to 9-year-old ones, 3.2 SD for 10- to 14-year-old ones, and 2.5 SD for 15- to 17-year-old children). In a model including ophthalmological and cardiological evaluations, ectopia lentis and aortic root dilatation (defined as 3 SD above the mean) were both similarly discriminating, with ~90% of children correctly classified.
Discussion
Our work is the largest report to date of the evolution of clinical features in Marfan children carrying a mutation in the FBN1 gene. It is issued from the national reference center in France, a specialized center with extensive use of genetic screening. The population studied was different from those of previous reports, which studied a small number of children (25, 22, 40, and 52 children, respectively)13,14,15,16 with, as eligibility criteria, a former international nosology. A single study included a large number of children (320 patients), but all were probands, thus excluding milder cases.17 We thus think that the population we studied provides a better overview of children affected by MFS. We chose to compare the MFS group with children consulting for suspicion of Marfan in whom MFS could be ruled out with confidence (absence of the familial FBN1 mutation or no features at the age of 18).
Evolution of prevalence of skeletal features was heterogeneous, with the prevalence of some features increasing across age strata, whereas the reverse was true for others. Because the prevalence of skeletal features varies with age, their diagnostic value varies during childhood. Wrist sign, flat feet, and pectus deformity were the signs with the greatest sensitivity after the age of 10, because they have been reported in adults.18 Before 10 years of age, hypermobility and thumb sign were more discriminating. The difference in arm span/height ratio between the MFS and the non-MFS groups is too small to be clinically useful, although statistically significant.
Prevalence of the Ghent criteria was more important in probands than in relatives, especially in terms of cardiovascular and ophthalmological features. Among skeletal features, only pectus deformity and arm span/height ratio were more frequent in probands. It was anticipated that probands would be more severely affected than relatives for two reasons: (i) because children with severe mutations tend to be more seriously affected and easily recognized, and (ii) severely affected patients may not reproduce as much as nonseverely affected patients.17 This may also be related to the fact that children in visible good health are not seeking medical advice, in addition to the fact that specific skeletal features are not well known to general practitioners or pediatricians and thus are not recognized.
Of note, a simple parameter, namely, height, appeared to be discriminant between MFS and non-MFS children. Height >3.3 SD above the mean carried, in our study, a positive predictive value of 72% and a negative predictive value of 79% during childhood. It may be explained partly by statural advance, which has already been reported by others15,19,20 but has never been included in any classification, whereas our study suggests that it has a great diagnostic value. We did not take into account the parents’ height in our study, but parental heights should be taken into account before labeling a child as “tall.” However, an international study including more children would be necessary to definitively define the usefulness of this criterion in screening children suspected of having MFS and to define the relevant difference between observed and predicted height, which may alert the practitioner.
From an ophthalmological perspective, our study allows us to specify that ectopia lentis is an early sign, which was already shown in other studies. In the study by Maumenee et al.,21 dislocation of the lens was observed in 12.5% of MFS children before 3 years of age and in 45% of 4- to 5-year-old children. Faivre et al.17 found ectopia lentis in 57% of MFS children under 10 years.
From the cardiological perspective, our study confirms previous studies, which reported that 80% of the MFS children had an aortic root dilatation using Roman’s nomograms.16,22 But our study specifies that this dilatation appears mostly before 6 years and that mean aortic root diameter remained stable. Stability of the Z score is also observed when Gautier nomograms are used. Mortality, possibly related to aortic dilatation or dissection, was 1.1% up to the age of 18 years, during a relatively short mean follow-up (3.5 years for the entire population), leading to a 0.3% annual mortality. This is low in comparison with that in other studies (range: 2.8–22%).13,16,22 These observations could be partly explained by our practice of proposing β-blockers for all children carrying a mutation in the FBN1 gene even in the absence of aortic root dilatation.22 This opinion is supported by the recent meta-analysis from Gao et al.,23 which concluded that systematic prescription of β-blockers in children with MFS limited dilatation of the aorta.
However, the two most discriminating features allowing diagnosis of MFS were ectopia lentis and aortic dilatation. If Roman nomograms are being used, it is necessary to consider an aortic root diameter limit > 3 SD above the mean because of the high frequency of normal children with an aortic diameter >2 SD above the mean (16%). This is in keeping with the new Ghent nosology giving more importance to ectopia lentis and aortic dilatation and recommending consideration of aortic dilatation when greater than mean + 3 SD in childhood.5
Limitations
This study was a historical cohort. However, the data were entered prospectively, and the register is exhaustive (all patients seen in the Marfan CNR are included in the register). The single-center nature of this study limits the variability of evaluation of the patients and reinforces the value of data obtained during follow-up because the measures are made by a small number of examiners. Otherwise, patients are referred from everywhere in France because this center is the National Reference Center; thus, it allows for a good representation of the children in the register. Inclusion of a population with MFS and an FBN1 mutation may induce a bias toward more severe cases. However, we chose to exclude the children with undetermined status regarding MFS and those with MFS according to the Ghent criteria—without FBN1 mutation in order to have a more homogeneous population. The control group was a mix between relatives and children who did not meet the Ghent criteria by the age of 18 years.
Conclusion
In conclusion, the diagnostic value of skeletal features is highly variable with age, but tall stature appears to be of value for simple screening in the population. Ectopia lentis and aortic root dilatation are the best discriminating features for Marfan diagnosis in childhood. Aortic root dilatation is present early in childhood but remains stable in infancy when children receive a β-blocker.
Disclosure
The authors declare no conflict of interest.
References
Faivre L, Collod-Beroud G, Loeys BL, et al. Contribution of molecular analyses in diagnosing Marfan syndrome and type I fibrillinopathies: an international study of 1009 probands. J Med Genet 2008;45:384–390.
Judge DP, Dietz HC . Marfan’s syndrome. Lancet 2005;366:1965–1976.
Stheneur C, Collod-Beroud G, Faivre L, et al. Identification of the minimal combination of clinical features in probands for efficient mutation detection in the FBN1 gene. Eur J Hum Genet 2009;17:1121–1128.
De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE . Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 1996;62:417–426.
Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet 2010;47:476–485.
Beighton P, de Paepe A, Danks D, et al. International Nosology of Heritable Disorders of Connective Tissue, Berlin, 1986. Am J Med Genet 1988;29:581–594.
Faivre L, Collod-Beroud G, Ades L, et al. The new Ghent criteria for Marfan syndrome: What do they change? Clin Genet 2011;81:433–442.
Stheneur C, Faivre L, Collod-Béroud G, et al. Prognosis factors in probands with an FBN1 mutation diagnosed before the age of 1 year. Pediatr Res 2011;69:265–270.
Greulich W, Idell Pyle S . Radiographic atlas of skeletal development of the hand and wrist. Stanford University Press: Stanford, CA, 1950.
Sempe M, Pedron G, Roy-Pernot M-P . [Auxology method and sequences]. Laboratoire Theraplix: Paris, France, 1979.
Roman MJ, Devereux RB, Kramer-Fox R, O’Loughlin J . Two-dimensional echocardiographic aortic root dimensions in normal children and adults. Am J Cardiol 1989;64:507–512.
Gautier M, Detaint D, Fermanian C, et al. Nomograms for aortic root diameters in children using two-dimensional echocardiography. Am J Cardiol 2010;105:888–894.
Geva T, Hegesh J, Frand M . The clinical course and echocardiographic features of Marfan’s syndrome in childhood. Am J Dis Child 1987;141:1179–1182.
Morse RP, Rockenmacher S, Pyeritz RE, et al. Diagnosis and management of infantile marfan syndrome. Pediatrics 1990;86:888–895.
Lipscomb KJ, Clayton-Smith J, Harris R . Evolving phenotype of Marfan’s syndrome. Arch Dis Child 1997;76:41–46.
van Karnebeek CD, Naeff MS, Mulder BJ, Hennekam RC, Offringa M . Natural history of cardiovascular manifestations in Marfan syndrome. Arch Dis Child 2001;84:129–137.
Faivre L, Masurel-Paulet A, Collod-Béroud G, et al. Clinical and molecular study of 320 children with Marfan syndrome and related type I fibrillinopathies in a series of 1009 probands with pathogenic FBN1 mutations. Pediatrics 2009;123:391–398.
Sponseller PD, Erkula G, Skolasky RL, Venuti KD, Dietz HC 3rd . Improving clinical recognition of Marfan syndrome. J Bone Joint Surg Am 2010;92:1868–1875.
Vetter U, Mayerhofer R, Lang D, von Bernuth G, Ranke MB, Schmaltz AA . The Marfan syndrome–analysis of growth and cardiovascular manifestation. Eur J Pediatr 1990;149:452–456.
Erkula G, Jones KB, Sponseller PD, Dietz HC, Pyeritz RE . Growth and maturation in Marfan syndrome. Am J Med Genet 2002;109:100–115.
Maumenee IH . The eye in the Marfan syndrome. Trans Am Ophthalmol Soc 1981;79:684–733.
Ladouceur M, Fermanian C, Lupoglazoff JM, et al. Effect of beta-blockade on ascending aortic dilatation in children with the Marfan syndrome. Am J Cardiol 2007;99:406–409.
Gao L, Mao Q, Wen D, Zhang L, Zhou X, Hui R . The effect of beta-blocker therapy on progressive aortic dilatation in children and adolescents with Marfan’s syndrome: a meta-analysis. Acta Paediatr 2011;100:e101–e105.
Acknowledgements
This work was supported by grants from the French Ministry of Health (grant Programme Hospitalier de Recherche Clinique 2010 AOM09093) and the Agence Nationale pour la Recherche (ANR 2010 BLAN 1129). We thank Philippe Aegerter, who provided help with statistical analysis. We are grateful to Maria Tchitchinadze for her help with the database.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Data
(PPT 522 kb)
Supplementary Data
(DOC 72 kb)
Supplementary Data
(DOC 78 kb)
Supplementary Data
(DOC 216 kb)
Rights and permissions
About this article
Cite this article
Stheneur, C., Tubach, F., Jouneaux, M. et al. Study of phenotype evolution during childhood in Marfan syndrome to improve clinical recognition. Genet Med 16, 246–250 (2014). https://doi.org/10.1038/gim.2013.123
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2013.123
Keywords
This article is cited by
-
Marfan syndrome in childhood: parents’ perspectives of the impact on daily functioning of children, parents and family; a qualitative study
BMC Pediatrics (2019)
-
Marfan syndrome in adolescence: adolescents’ perspectives on (physical) functioning, disability, contextual factors and support needs
European Journal of Pediatrics (2019)
-
Differences in Cardiovascular Manifestation of Marfan Syndrome Between Children and Adults
Pediatric Cardiology (2019)
-
The importance of genotype-phenotype correlation in the clinical management of Marfan syndrome
Orphanet Journal of Rare Diseases (2018)
-
Skeletal evolution in Marfan syndrome: growth curves from a French national cohort
Pediatric Research (2018)