Abstract
Abstract: Hereditary breast and ovarian cancer due to mutations in the BRCA1 and BRCA2 genes is the most common cause of hereditary forms of both breast and ovarian cancer. The overall prevalence of BRCA1/2 mutations is estimated to be from 1 in 400 to 1 in 800 with a higher prevalence in the Ashkenazi Jewish population (1 in 40). Estimates of penetrance (cancer risk) vary considerably depending on the context in which they were derived and have been shown to vary within families with the same BRCA1/2 mutation. This suggests there is no exact risk estimate that can be applied to all individuals with a BRCA1/2 mutation. The likelihood of harboring a BRCA1 or BRCA2 mutation is dependent on one's personal and/or family history of cancer and can be estimated using various mutation probability models. For those individuals who have a BRCA1 or BRCA2 mutation, several screening and primary prevention options have been suggested, including prophylactic surgery and chemoprevention. Once a BRCA1 or BRCA2 mutation has been identified in a family, testing of at-risk relatives can identify those family members who also have the familial mutation and thus need increased surveillance and early intervention when a cancer is diagnosed.
Similar content being viewed by others
NATURAL HISTORY AND GENETICS
Disease characteristics
Germline mutations in breast cancer 1 gene (BRCA1) and breast cancer 2 gene (BRCA2) predispose to breast and ovarian cancer as well as other cancers. The risk of developing cancer (penetrance) that is associated with a BRCA1 or BRCA2 mutation appears variable within families and has been derived from a variety of sources, including families with multiple-affected individuals, families with few affected individuals, and population-based studies.1,2 Prognosis for breast and ovarian cancer depends on the stage at which the cancer is diagnosed, but studies on survival have been conflicting for individuals with BRCA1 and BRCA2 mutations when compared with patients who are not mutation carriers.3–19
Prevalence
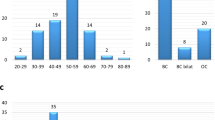
Hereditary breast and ovarian cancer (HBOC) due to mutations in BRCA1 and BRCA2 is the most common cause of hereditary forms of both breast and ovarian cancer and occurs in all ethnic and racial populations. The overall prevalence of BRCA1/2 mutations is estimated to be from 1 in 400 to 1 in 80020–22 but varies depending on ethnicity. Few studies, however, have directly compared mutation prevalence by ethnic background.23–27 In the United States, much of the focus has been on individuals of Ashkenazi (central European) Jewish ancestry.
Ashkenazi Jews have a substantially elevated risk of HBOC secondary to a high frequency of BRCA1/2 mutations mainly attributable to three well-described founder mutations: two of which are in the BRCA1 gene (187delAG and 5385insC, also known as 185delAG and 5382insC, respectively. The Human Genome Variation Society nomenclature for each is NC_000017.9:g.38529572_38529571delAG and NC_000017.9:g.38462606dupC, respectively) and one of which is in the BRCA2 gene (6174delT, the Human Genome Variation Society nomenclature for 6174delT is NC_000013.9:c.24822delT).28–30 The 187delAG mutation in BRCA1 occurs with a frequency of about 1.1% in individuals of Ashkenazi Jewish descent.26,30–32 The 5385insC mutation has an estimated prevalence of 0.1% to 0.15%,32 and the BRCA2 mutation, 6174delT occurs with a frequency of about 1.5%,28,30–32 resulting in a carrier frequency of 1 per 40 in the aggregate. The prevalence of BRCA1 mutations in Ashkenazi Jewish women aged younger than 65 years at diagnosis is 8.3%.26 The BRCA2 founder mutation, 6174delT, is present in 8% of women diagnosed with breast cancer before the age of 42 years and in 1.5% of unselected Ashkenazim,32,33 whereas the BRCA1 founder mutation, 185delAG, has been found in 20% of Ashkenazi Jewish women diagnosed with breast cancer before the age of 42 years.34 This increased frequency influences genetic testing recommendations for individuals of Ashkenazi Jewish heritage (see Testing Strategy section).
Although most BRCA1 mutations described involve only a few base pairs, studies in the Dutch population have identified three large deletions within BRCA1. These deletions were detected using Southern blot analysis and accounted for 36% of mutations in a Dutch sample of high-risk families.35
The BRCA2 mutation, 999del5, occurs in 0.6% of the Icelandic population and in 10.4% of women and 38% of men with breast cancer from Iceland.36 The mutation was seen in 17% of women diagnosed with breast cancer by the age of 50 years and in 4% of women diagnosed at later ages. Among individuals with the 999del5 mutation, 17 of 44 (39%) had no first- or second-degree relatives with cancer, suggesting incomplete penetrance of the mutation.37
There are several other populations in which founder BRCA1 and BRCA2 mutations have also been identified.38
Molecular genetics
BRCA1
The BRCA1 gene is located on the long arm of Chromosome 17 at 17q21 and contains 24 coding exons spread over 80 kb.39 Its normal allele produces a 7.8-kb mRNA that encodes the breast cancer type 1 susceptibility protein, a 1863 amino acid that contains several recognizable protein motifs, including a RING-finger domain near the N-terminus, two nuclear localization signals located on exon 11, an “SQ” cluster between amino acids 1280–1524, and a BRCT domain at the C-terminus. BRCA1 interacts with several proteins involved in cellular pathways, including cell cycle progression, gene transcription regulation, DNA damage response, and ubiquitination.40,41 From studying homozygous knockout mice, the available evidence indicates that BRCA1 serves as a “caretaker,” such as TP53, helping to maintain genomic integrity.42 When this function is lost, it probably allows for the accumulation of other genetic defects that are themselves directly responsible for cancer formation. More than 1600 mutations have been identified in BRCA1, most of which lead to frameshifts resulting in missing or nonfunctional proteins. In most, but not all cancers that have been studied from individuals with a germline mutation, the wild-type allele is deleted, strongly suggesting that BRCA1 is in the class of tumor suppressor genes.40,43,44 Loss of function of BRCA1 results in defects in DNA repair, defects in transcription, abnormal centrosome duplication, defective G2/M cell cycle checkpoint regulation, impaired spindle checkpoint, and chromosome damage.45–47
BRCA2
The BRCA2 gene is located on the long arm of the Chromosome 13 at 13q12.3 and contains 27 coding exons. Its normal allele produces a 10.4-kb mRNA that encodes breast cancer type 2 susceptibility, a 3418 amino acid with eight 30 to 40 residue motifs found in exon 11, which mediates the binding of BRCA2 to RAD51. BRCA2 is normally located in the nucleus and contains phosphorylated residues.48 The breast cancer type 2 susceptibility protein has no recognizable protein motifs and no apparent relation to the breast cancer type 1 susceptibility protein. Nonetheless, the proteins encoded by BRCA1 and BRCA2 appear to share a number of functional similarities that may suggest why mutations in these genes lead to a specific hereditary predisposition to breast and ovarian cancer. BRCA2 appears to be involved in the DNA repair process. From studying homozygous knockout mice, the available evidence indicates that BRCA2 is a “caretaker,” similar to BRCA1, which serves to maintain genomic integrity.42 More than 1800 mutations have been identified in BRCA2 with most mutations reported to date consisting of frameshift deletions, insertions, or nonsense mutations leading to premature truncation of protein transcription, consistent with the loss of function that is expected with clinically significant mutations in tumor suppressor genes. Cells lacking BRCA2 are deficient in the repair of double-strand DNA breaks, as reflected in a hypersensitivity to ionizing radiation.49
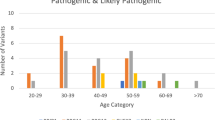
Penetrance (cancer risk)
The penetrance of BRCA1 and BRCA2 mutations is the most significant clinical aspect of HBOC with breast and ovarian cancer being the predominant phenotype. Estimates of penetrance vary considerably depending on the context in which they were derived. Multiple breast case families, especially if ovarian cancer is also present, may be enriched for mutations and have been shown to have substantial risks for both breast and ovarian cancer. In 1995, Easton et al.1 provided a lifetime breast cancer risk in BRCA1 carriers of >80%, the highest reported estimate to date. However, these risks may overestimate the risk within all families and therefore may not apply to families with less severe cancer histories or in incident cases as illustrated in studies of unselected patients with breast cancer whose estimated breast cancer risks have been in the 40% to 60% range.2 In addition to these wide-ranging risk estimates, penetrance has been shown to vary within families with the same BRCA1/2 mutation, suggesting that there is no “exact” risk estimate that can be applied to all individuals with a BRCA1 or BRCA2 mutation.
The following is a summary of cancer risks in individuals identified with mutations in the BRCA1 and BRCA2 genes. No associated benign tumors or physical abnormalities are presently known to be associated with BRCA1/2 mutations.
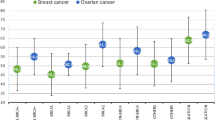
BRCA1—female breast and ovarian cancer risks
According to a combined analysis of 22 population-based studies in which cases were unselected for family history, the average risk for breast cancer in BRCA1 mutation carriers by the age of 70 years was 65% (95% confidence interval [CI]: 44–78%) and for ovarian cancer was 39% (95% CI: 18–54%).50 Another population-based study on those aged 80 years revealed BRCA1-related breast and ovarian cancer risk estimates of 90% and 24%, respectively.51 When correcting for ascertainment, a meta-analysis of 10 studies reported cumulative cancer risks for breast and ovarian cancer as 57% and 40%, respectively, to age 70 for BRCA1 mutation carriers.52 The contralateral breast cancer risk in BRCA1 carriers is 27% within 5 years of the initial breast cancer diagnosis.53 The risk of BRCA1-related breast and ovarian cancer appears to be confined to epithelial malignancies of both organs.
BRCA1—other related cancer risks
Fallopian tube carcinoma is now a well-established component tumor of the BRCA1-related cancer spectrum, with relative risks reported as high as 120.54 BRCA1 mutation carriers are also at risk of primary papillary serous carcinoma of the peritoneum, a malignancy that is indistinguishable from serous epithelial ovarian carcinoma, with cumulative risks of 3.9% to 4.3% 20 years after oophorectomy.55,56 The risk of prostate cancer in male BRCA1 carriers is increased with a relative risk of ∼1.857 although this risk may vary significantly depending on the location of the BRCA1 mutation.58 Furthermore, such cancers do not typically demonstrate a younger than usual age at diagnosis.59 Finally, a variety of other cancers have been implicated, albeit inconsistently, as part of the BRCA1-related cancer spectrum.60 The most convincing associations are an increased risk of pancreatic cancer61 and male breast cancer62,63 with the cumulative breast cancer risks to age 70 among BRCA1 male mutation carriers being 1.2%. Initial reports of increased colorectal cancer risk have generally not been replicated. The Breast Cancer Linkage Consortium also reported statistically significantly increased relative risks for cancers of the pancreas, uterine body, and cervix (only in carriers younger than age 65 years), with relative risks of 2.3, 2.6, and 3.7, respectively.57 The possibility that endometrial cancer might be a BRCA1/2-related malignancy has been inconsistent and may be related to tamoxifen exposure.64
BRCA2—female breast and ovarian cancer risks
In the same 22 population-based studies cited earlier, the BRCA2-related risk estimates to age 70 for both breast and ovarian cancer were 45% (95% CI: 33–54%) and 11% (95% CI: 4–18%), respectively.50 In another population-based study, BRCA2-related breast and ovarian cancer risk estimates to age 80 were 41% and 8.4%, respectively,51 which was the lowest ovarian cancer penetrance estimate yet reported. When corrected for ascertainment, the cumulative cancer risks to age 70 for breast and ovarian cancer in BRCA2 carriers were reported as 49% and 18%, respectively.65 The risk of ovarian cancer, although lower than that observed in BRCA1 mutation carriers, is still greatly increased above the general population (1.4%). Ovarian cancer in BRCA2 carriers is more likely to occur after the age of 50 years than those found in BRCA1 carriers.66 The contralateral breast cancer risk in BRCA2 carriers is 12% within 5 years of the initial breast cancer diagnosis.53 As in BRCA1, the risk of BRCA2-related breast and ovarian cancer appears to be confined to epithelial malignancies of both organs as well.
BRCA2—other related cancer risks
Fallopian tube carcinoma has also been associated with BRCA2 mutations,67 as has primary papillary serous carcinoma of the peritoneum, and similar to ovarian cancer, this malignancy occurs less frequently among BRCA2 when compared with BRCA1 carriers.55 Male breast cancer is more commonly associated with BRCA2 mutations when compared with BRCA1 mutations. The cumulative probability to age 70 of male breast cancer in carriers of BRCA2 mutations has been reported as 6%62 and 6.8%.63 Prostate cancer also occurs in excess in male BRCA2 carriers with a relative risk of 4.6,68 although unlike as observed in BRCA1-related prostate cancer, it may demonstrate a younger than usual age at diagnosis.69 The presence of pancreatic cancer in a breast cancer family may be a statistically significant predictor of a BRCA2 mutation70 although BRCA1 carriers have also been found to have an increased risk. The Breast Cancer Linkage Consortium also reported statistically increased relative risks for cancers of the pancreas, gallbladder and bile duct, stomach, and melanoma with relative risks of 3.5, 5.0, 2.6, and 2.6, respectively,68 the latter three sites being inconsistently associated with BRCA2.71 Finally, as with BRCA1, initial reports of increased colorectal cancer risk have generally not been replicated.
Cancer risks in specific populations
The risk of breast cancer by the age of 70 years for carriers of the two Ashkenazi founder BRCA1 mutations, 185delAG and 5282insC, is 64% (95% CI: 34–80%) and 67% (95% CI: 36–83%), respectively.72 The corresponding values for ovarian cancer are 14% (95% CI: 2–24%) and 33% (95% CI: 8–50%), respectively. In an effort to eliminate inflated penetrance estimates suspected from studies of cancer families, Satagopan et al.73 studied incident breast cancer cases and found the penetrance of breast cancer at age 80 among BRCA1 carriers to be 59% (95% CI: 40–93%) and among BRCA2 carriers to be 38% (95% CI: 20–68%). Using a similar study design, Satagopan et al.74 also found the estimated penetrance of ovarian cancer at age 70 among BRCA1 carriers to be 37% (95% CI: 25–71%) and among BRCA2 carriers to be 21% (95% CI: 13–41%). In the US population, Chen et al.52 estimated cumulative breast cancer risk in BRCA1 mutation carriers to age 70 as 46% (95% CI: 0.39–0.54%) and for ovarian cancer as 39% (95% CI: 0.30–0.50%), based on 676 Ashkenazi families and 1272 families of other ethnicities. The risk of breast cancer by age 70 for carriers of the Ashkenazi BRCA2 6174delT mutation is 43% (95% CI: 14–62%) and for ovarian cancer is 20% (95% CI: 2–35%).72 The breast cancer penetrance of the Icelandic BRCA2 999del5 mutation was 17% by age 50 and 37% by age 70.36
Genotype-phenotype correlations
In addition to differences in cancer risks by gene, cancer risks in BRCA1 and BRCA2 mutation carriers may differ by mutation position as well. It has been suggested that families with mutations in the ovarian cancer cluster region of exon 11 of the BRCA2 gene have a higher ratio of ovarian to breast cancer than families with mutations elsewhere in the BRCA2 gene. In 2004, Lubinski et al.75 investigated 440 families with a BRCA2 mutation for the presence of cancer of the ovary, male breast, pancreas, prostate, colon, and stomach as well as melanoma in first- and second-degree relatives of mutation-positive individuals. Families with ovarian cancer were more likely to harbor mutations in the ovarian cancer cluster region than elsewhere in the gene. Differences in ethnic groups were documented as well. Families of Polish ancestry had a lower frequency of pancreatic cancer than families of other ethnic origins, suggesting that both position of mutation and ethnic background may contribute to the phenotypic variation observed in families with BRCA2 mutations.75 More recently, Cybulski et al.58 found that the odds ratio of prostate cancer varied substantially by the position of the mutation. Despite such interesting findings, these correlations are not currently being used for definitive clinical management decisions.
Breast cancer prognosis
The distinct pathologic features of BRCA1-related breast tumors (and perhaps BRCA2-related breast tumors) coupled with the relative paucity of somatic BRCA1/2 mutations in breast cancer occurring in individuals with no known family history of breast cancer suggest that breast cancer in individuals with BRCA1 or BRCA2 germline mutations has a specific pathogenetic basis, which could lead to differences in prognosis. However, prospective longitudinal studies with large numbers of women to accurately estimate breast cancer prognosis in individuals with BRCA1/2 mutations are lacking. The available data, derived mostly from retrospective or indirect data, are based on small numbers (<50 cases), are probably confounded by different biases, and lack appropriate controls. Given these limitations, most studies on prognosis of breast cancer have not found a significant difference in survival between individuals with BRCA1 or BRCA2 mutations and controls,76–81 and studies reporting both better prognosis3,4 and worse prognosis exist.5–8
In a retrospective cohort study of individuals of Ashkenazi heritage with breast cancer, those with a BRCA1 mutation experienced poorer disease-specific survival compared with controls who did not have a BRCA1 mutation but only among women not receiving adjuvant chemotherapy.82 Several studies have reported higher rates of contralateral breast cancers7,8,83,84 and ipsilateral breast cancers68–85 in women with BRCA1/2 mutations who are treated with breast conservation. In one case-control study, the increased rate of ipsilateral breast cancers was only seen in individuals with a BRCA1 or BRCA2 mutation who had not undergone prophylactic oophorectomy.86 The increase in second primary cancers reported in these studies has not yet translated into significant differences in survival. Clearly, additional prospective studies with more rigorous designs will help to clarify these complex interactions and better define the true prognosis of BRCA1/2-related breast cancer.
Ovarian cancer prognosis
Studies on ovarian cancer survival in women with BRCA1/2 mutations have yielded conflicting results as well, at least in part because of the same methodologic issues encountered in studies on breast cancer prognosis. Two small population-based studies in Sweden (n = 38) and a Canadian study (n = 44) found no differences in survival between women with BRCA1 mutations with ovarian cancer and controls.9,77 A short-term improvement seen in a case-control study from the Netherlands did not persist after 5 years,10 and a case-control study at the University of Iowa also failed to find a survival advantage for women with BRCA1 mutations with ovarian cancer.11 However, data suggesting a survival advantage for BRCA1/2 mutation carriers are growing. The first study in which women with BRCA1 mutations were identified by molecular genetic testing found improved survival in 43 women with BRCA1-associated ovarian cancer (median survival of 77 months compared with 29 months in controls).12 This study was criticized for selection bias, lead-time bias (increased surveillance leading to earlier diagnosis in familial cases),13,14 and differences in treatment received by individuals with mutations compared with historical controls.15 A similar improved survival rate was noted in a study of 25 women with BRCA1 mutations with stage III ovarian cancer,16 and in Ashkenazi Jewish women treated with platinum-based chemotherapy.17 More recent studies also support the finding of improved survival among mutation carriers. A small case-control study from the United Kingdom found both higher complete response rates (81.8% vs. 43.2%; P = 0.004) and overall survival (95.5% vs. 59.1%; P = 0.002) for BRCA-positive patients.18 The National Israeli Study of Ovarian Cancer reported significantly better median survival (53.7 vs. 37.5 months; P = 0.002) and 5-year survival rates (38.1% vs. 24.5%; P = <0.001) for carriers of an Ashkenazi founder mutation compared with noncarriers.19 Two population-based studies report a greater survival benefit among BRCA2 mutation carriers than BRCA1 mutation carriers with ovarian cancer.87,88
Studies finding a survival advantage for BRCA1/2 mutation carriers are supported by in vitro data that shows increased sensitivity to platinum-based drugs in BRCA1-mutant cells, thus providing a potential biologic rationale for improved survival in women treated for ovarian cancer with platinum-based therapies.89,90
Prostate cancer prognosis
A number of case-control studies have reported a significant number of men with deleterious BRCA2 mutations presenting at a young age at diagnosis, with high-grade histopathology and experiencing decreased survival compared with men with sporadic prostate cancer.91–93
Breast cancer pathology
BRCA1-related breast tumors show an excess of medullary histopathology, are of higher histologic grade, and are more likely than sporadic tumors to be estrogen receptor negative and progesterone receptor negative, and are less likely to demonstrate HER2/neu overexpression, thus falling within the category of “triple-negative” breast cancer.94 At the molecular level, a higher frequency of TP53 mutations is observed than in sporadic tumors. Emerging data suggest that BRCA1-related breast cancers are more likely than sporadic tumors to be derived from the basal epithelial layer of cells of the mammary gland, to be triple negative and to stain positive for CK5/6 markers.95–97 Information regarding BRCA2-related breast tumors is more limited, but they do not seem to have a characteristic histopathology and are more likely to resemble sporadic breast cancers.
Ductal carcinoma in situ is now recognized as part of the spectrum of breast neoplasia in BRCA1/2 mutation carriers, however, its frequency compared with sporadic breast cancer is controversial.98–100
Ovarian cancer pathology
An excess of ovarian serous adenocarcinomas has been observed in women with BRCA1 and BRCA2 mutations compared with controls. More than 90% of tumors in women with BRCA1 mutations are serous, compared with ∼50% in women without a BRCA1 mutation.12,16,101,102 Serous adenocarcinomas are generally of higher grade and are more frequently bilateral than mucinous cancers. Preliminary support for distinct molecular pathways of carcinogenesis comes from the finding of differential expression of genes in BRCA1, BRCA2, and sporadic ovarian cancer using DNA microarray technology.103 This approach may ultimately lead to the identification of unique histopathologic subtypes.
Careful histopathologic analysis of the fallopian tubes removed at the time of prophylactic oophorectomy has identified the fimbria as a potential site for primary fallopian tube carcinoma and tubal intraepithelial carcinoma. Many of these tubal carcinomas also stain for p53 protein, which is overaccumulated in serous carcinoma.104 These findings suggest that in addition to primary tubal carcinoma, the fimbria may represent the origin of some peritoneal and ovarian serous carcinomas.105
DIAGNOSIS AND TESTING
Clinical diagnosis
HBOC is suspected if one or more of the following features are present in a family and thus would warrant further risk evaluation106:
-
Early-age-onset breast cancer (younger than 50 years of age) including both invasive and ductal carcinoma in situ breast cancers.
-
Two breast primaries or breast and ovarian/fallopian tube/primary peritoneal cancer in a single individual or two or more breast primaries or breast and ovarian/fallopian tube/primary peritoneal cancers in close (first-, second-, and third-degree) relative(s) from the same side of family (maternal or paternal).
-
Populations at risk (Ashkenazi Jewish).
-
Member of a family with a known BRCA1 or BRCA2 mutation.
-
Any male breast cancer.
-
Ovarian/fallopian tube/primary peritoneal cancer at any age.
Situations that may lower the threshold of suspicion for HBOC would include families with a limited family structure, defined as having fewer than two first- or second-degree female relatives surviving beyond the age of 45 years in either lineage, as this may lead to an underrepresentation of female cancers despite the presence of a predisposing family mutation107; oophorectomy at a young age in family members, which reduces the risk of both breast and ovarian cancer, as this might mask a hereditary susceptibility to both breast and ovarian cancer; the presence of adoption in the lineage, and populations at risk of carrying a BRCA1/2 mutation (e.g., individuals of Ashkenazi Jewish descent).
Mutation probability models
Probability models have been developed to estimate the likelihood that an individual or family has a mutation in BRCA1 or BRCA2. Each model has its own unique attributes determined by the methods, sample size, and population used to create it. Two such widely used models include BRCAPRO and Myriad (Table 1).
BRCAPRO is a computer-based Bayesian probability model that uses breast and/or ovarian cancer family history in first- and second-degree relatives to determine the probability that a BRCA1 or BRCA2 gene mutation accounts for the pattern of these cancers in the family.108 Key attributes include the population prevalence of mutations, age-specific penetrance, and Ashkenazi Jewish heritage. BRCAPRO is available as part of the CancerGene software (http://www4.utsouthwestern.edu/breasthealth/cagene/).
The Myriad model is a set of mutation prevalence tables categorized by ethnic ancestry (Ashkenazi Jewish or non-Ashkenazi Jewish), the age of onset (younger than 50 years or ≥50 years of age) of breast cancer, and the presence of ovarian cancer in the patient and/or first- or second-degree relatives, and is based on actual test data from Myriad Genetic Laboratories through its clinical testing service.109 These tables are periodically updated online (http://www.myriadtests.com/provider/brca-mutation-prevalence.htm).
Other less commonly used probability models include the Manchester Scoring System, Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA), and Tyrer-Cuzick.110–112
In 2003, the American Society of Clinical Oncology updated their policy statement on genetic testing for cancer susceptibility stating, “Given the known limitations and wide variations inherent in models for estimating mutation probability in a given family or individual, and the lack of such models for many cancer predisposition syndromes, it is neither feasible nor practical to set numerical thresholds for recommending genetic risk assessment services. The American Society of Clinical Oncology therefore recommends that evaluation by a health care professional experienced in cancer genetics should be relied on in making interpretations of pedigree information and determinations of the appropriateness of genetic testing, including determinations of appropriateness for reimbursement.”113 As such, when evaluating family histories for HBOC, a quantitative and qualitative assessment of the pedigree should be conducted before making testing recommendations.
Molecular genetic testing
BRCA1 and BRCA2 are the only genes known to be associated with HBOC. Clinical uses of molecular genetic testing include diagnosis of symptomatic individuals, as well as predisposition testing in at-risk relatives. Clinical testing in the United States is available exclusively at Myriad Genetic Laboratories because of patent protections and is summarized in Table 2. Targeted mutation analysis may be population specific and includes mutations known to be found at greater frequencies in certain ethnicities. Comprehensive analysis includes sequence analysis combined with other methods, which can detect both common and family-specific BRCA1 and BRCA2 mutations, including five specific large genomic rearrangements of BRCA1. Sequence analysis or other mutation scanning methods are recommended when the mutation in a family is not known, except in individuals of Ashkenazi Jewish descent, which is further explained under testing strategy. Large rearrangement testing analyzes for rearrangements above and beyond the five common rearrangements of BRCA1 and thus is complementary to comprehensive analysis. In addition, large rearrangement testing examines for rearrangements in BRCA2 as well.
Interpretation of test results in a proband
-
Targeted mutation analysis: When testing an Ashkenazi Jewish individual for the three founder mutations, typically the result will either be negative or positive.
-
Mutation is absent: Because this testing detects only the three founder mutations associated with Ashkenazi Jewish ancestry, failure to detect a mutation (i.e., a negative result) does not exclude the possibility that the individual has another predisposing BRCA1 or BRCA2 mutation. The recommendation to proceed with comprehensive analysis following the failure to detect one of the three common Ashkenazi Jewish mutations in this population is based on clinical judgment, the a priori risk of harboring a mutation, and the residual likelihood that a BRCA1 or BRCA2 mutation (other than the three common mutations) is present in that individual.
-
Mutation is present: The presence of a germline mutation (i.e., a positive result) confers an increased risk for HBOC-related cancers. It is recommended that follow-up testing of at-risk relatives, particularly if both sides of the family are Ashkenazi Jewish, includes targeted mutation analysis for all three of the common Ashkenazi Jewish mutations regardless of which mutation is found in the proband because coexistence of more than one founder mutation has been reported in some Ashkenazi Jewish families.119
-
Result is inconclusive: Given the testing methodology that is used, rarely a novel BRCA1 or BRCA2 variant of uncertain clinical significance (VUS) has been inadvertently detected in the DNA adjacent to the three common Ashkenazi Jewish mutations. Generally, this is a change in a single DNA nucleotide (missense mutation) that may or may not disrupt protein function. To further evaluate this result, the laboratory may request blood samples from additional members of the family (usually affected individuals and/or parents of the individual tested) to determine if the variant cosegregates with the cancer in the family. Such studies could reveal that the variant is either a pathogenic mutation or a polymorphism of no clinical significance. Between 10% and 15% of individuals undergoing genetic testing for BRCA1 and BRCA2, mutations will be found to have a VUS,109 but this result is more commonly found after comprehensive analysis.
Comprehensive analysis: Any of the following results are possible in an individual undergoing comprehensive analysis.
-
Mutation is absent: Failure to detect a mutation (i.e., a negative result) must be interpreted with caution because the underlying cause of the cancer in the family has not been established. The possibility remains that the cancer in the family is either associated with a mutation not detectable by the method of genetic testing used, is caused by a change in a different cancer susceptibility gene, or is the result of nonhereditary factors. Consequently, the family should be cautioned that the failure to detect a mutation does not eliminate the possibility of a hereditary susceptibility in the family.
-
Mutation is present: The presence of a germline BRCA1 or BRCA2 mutation (i.e., a positive result) confers an increased risk for HBOC-related cancers.
-
Result is inconclusive: Comprehensive analysis may reveal a novel BRCA1 or BRCA2 VUS. Again, family studies may be initiated in an attempt to determine the significance of the variation.
Large rearrangement test: Either of the following results is possible in individuals undergoing large rearrangement testing.
-
Rearrangement is absent: Failure to detect a rearrangement (i.e., a negative result) must be interpreted with caution because the underlying cause of the cancer in the family has not been established. The possibility remains that the cancer in the family is either associated with a mutation not detectable by the method of genetic testing used, is caused by a change in a different cancer susceptibility gene, or is the result of nonhereditary factors. Consequently, the family should be cautioned that the failure to detect a rearrangement does not eliminate the possibility of a hereditary susceptibility in the family.
-
Rearrangement is present: The presence of a germline BRCA1 or BRCA2 rearrangement (i.e., a positive result) confers an increased risk for HBOC-related cancers.
Interpretation of test results in an at-risk relative
-
Family-specific mutation: When testing at-risk relatives for a mutation known to be present in the family, either of the following results could occur.
-
Mutation is absent: Failure to detect the mutation (i.e., a negative result) means that the person has not inherited the family-specific mutation and has at least the general population risks for HBOC-related cancers.
-
Mutation is present: Presence of the germline mutation (i.e., a positive result) means that the person has inherited the family-specific mutation and is at an increased risk for HBOC-related cancers.
Testing strategy
-
Probands of Ashkenazi Jewish ancestry: As mentioned previously, in persons of Ashkenazi Jewish heritage, three founder mutations are observed: 187delAG (BRCA1), 5385insC (BRCA1), and 6174delT (BRCA2). As many as 1 in 40 Ashkenazim have one of these three founder mutations.28 Consequently, testing a person of Ashkenazi Jewish heritage initially for these three founder mutations by targeted mutation analysis can be an effective way to assess if the individual has a BRCA1 or BRCA2 mutation rather than first performing comprehensive analysis as recommended for all other populations. If no mutation is identified by targeted mutation analysis, the recommendation may be to proceed with comprehensive analysis. This recommendation is often based on clinical judgment, the a priori mutation risk, and the residual likelihood that a BRCA1 or BRCA2 mutation is present in that individual.
-
Family not known to have a BRCA1 or BRCA2 mutation: Testing in families is most likely to be informative if the first person to undergo testing has already had breast cancer and/or ovarian cancer, especially if the breast cancer occurred at an earlier age than is typical (i.e., before age 50 years). Thus, whenever possible, molecular genetic testing should be performed on the individual in the family who is most likely to have a BRCA1 or BRCA2 mutation, and who is less likely to have developed sporadic breast or ovarian cancer. In many families, this approach is not feasible because the affected relative is deceased or is not willing or able to participate in molecular genetic testing. In these instances, testing may be performed on individuals without a cancer history with the understanding that failure to detect a mutation does not eliminate the possibility of a BRCA1 or BRCA2 mutation being present in the family.
-
Family known to have a BRCA1 or BRCA2 mutation: Once a germline mutation has been identified within a family, adult relatives in the same lineage (including family members without a cancer history) may then be tested for the same family-specific mutation with great accuracy. In most cases, relatives at risk need only be tested for the family-specific mutation. However, exceptions to this would include any of the following:
-
Individuals of Ashkenazi Jewish heritage who should be tested for all three founder mutations because of reports of the coexistence of more than one founder mutation in some Ashkenazi Jewish families.
-
Individuals in whom a BRCA1 or BRCA2 mutation may be present in both maternal and paternal lines. For example, if a mutation is identified on the maternal side of the family and if HBOC is also suspected on the paternal side, it is appropriate to recommend that the individual undergo comprehensive analysis of BRCA1 and BRCA2, which would (1) detect the familial mutation from the maternal side and also (2) address whether a mutation is tracking on the paternal side.
Genetically related (allelic) disorders
Germline mutations in BRCA2 have been associated with familial pancreatic cancer120,121 and Fanconi anemia complementation group FANCD1.122
Differential diagnosis
Other inherited cancer susceptibility syndromes and/or genes that predispose to breast cancer include Li-Fraumeni syndrome, Cowden syndrome, hereditary diffuse gastric cancer, CHEK2, ataxia-telangiectasia, Lynch syndrome (also known as hereditary nonpolyposis colorectal cancer), Peutz-Jeghers syndrome, Bloom syndrome, Werner syndrome, and xeroderma pigmentosum (Table 3). The PALB2 and BRIP1 genes have also been implicated in hereditary forms of breast cancer.126,127 In many instances, HBOC can be distinguished from these other disorders based on the constellation of tumors present in the family; however, in some cases, molecular analysis may be necessary to differentiate.
MANAGEMENT
Individuals who are diagnosed with a mutation in BRCA1 or BRCA2 are counseled at the time of disclosure about their options for screening and primary prevention.
Primary prevention
Several strategies have been suggested to reduce cancer risk in individuals who have a BRCA1 or BRCA2 mutation. These include prophylactic mastectomy and/or oophorectomy and chemoprevention. Although several studies have provided compelling evidence to support the use of risk-reducing surgery in high-risk women, this strategy has not been evaluated by randomized trials.
A retrospective cohort study of all women receiving prophylactic mastectomy at the Mayo Clinic in the state of Minnesota during a 30-year period estimated a 90% reduction in breast cancer risk from the procedure. One third of the women in the Mayo Clinic study were considered to have a strong family history of cancer and experienced a risk reduction similar to that of the whole group.128 In a subsequent follow-up of this cohort, 176 women were tested for BRCA1 and BRCA2 mutations. Of the 26 with a germline BRCA1 or BRCA2 mutation, none had developed breast cancer after a median follow-up of 13 years.129 In a more recent study, the incidence of breast cancer in 483 individuals with a BRCA1/2 mutation was measured. Breast cancer was diagnosed in 2 of 105 women (1.9%) who underwent bilateral prophylactic mastectomy and in 184 of 378 matched controls (48.7%) who did not have surgery, suggesting that bilateral prophylactic mastectomy reduces the risk of breast cancer by ∼90% in women who have a BRCA1/2 mutation.130
Several studies have documented a significant (80–96%) risk reduction in ovarian cancer after risk-reducing oophorectomy.131–133 Histologic evaluation of the tissues removed for risk reduction has revealed a wide spectrum of both occult ovarian cancers and primary fallopian tube tumors, supporting the removal of both ovaries and fallopian tubes at the time of surgery.134–136 However, after risk-reducing oophorectomy, the peritoneum remains at risk for primary peritoneal cancer, with rates of ∼2% after surgery.55,137
Rebbeck et al.130 also found a 53% risk reduction for breast cancer in women undergoing bilateral prophylactic oophorectomy. These observations were consistent with the findings of Olopade and Artioli.138 One multisite study of 1079 women followed up for a median of 30 to 35 months found that although there was a reduction in breast cancer risk for all mutation carriers undergoing prophylactic oophorectomy, the risk reduction was more pronounced in BRCA2 carriers.139 Several important questions regarding prophylactic surgery remain, such as what is the optimal timing for these procedures and how should individuals undergoing these procedures be followed up long term. The side effects of surgical menopause, including vasomotor symptoms, vaginal dryness, osteoporosis, and heart disease, must also be considered.
Chemoprevention
A randomized clinical trial of treatment with tamoxifen (a partial estrogen antagonist) in women identified by the Gail model to have an increased breast cancer risk reported a 49% reduction in breast cancer in the treated group.140 In 1999, Gail et al. concluded that tamoxifen prophylaxis was most beneficial in women with an elevated risk of breast cancer who were younger than 50 years. However, tamoxifen reduced the incidence of breast cancers that were estrogen receptor positive but not estrogen receptor negative.141 Because breast cancers occurring in women with BRCA1 mutations are more likely to be estrogen receptor negative, it is predicted that tamoxifen may provide more benefit in women with BRCA2 mutations.
A subset analysis of the randomized trial evaluated the effect of tamoxifen on the incidence of breast cancer among cancer-free women with inherited BRCA1 or BRCA2 mutations and showed that tamoxifen reduced the risk of breast cancer by 62% among healthy women with a BRCA2 mutation.142 In a case-control study of 538 women with a BRCA1/2 mutation, tamoxifen use was associated with a 50% reduction in the risk of developing contralateral breast cancer.143 In a more recent historical cohort study of 491 women with hereditary breast cancer, a 41% reduction in the risk of contralateral breast cancer was observed after 10 years.144 Statistically significant adverse consequences of tamoxifen treatment included higher rates of endometrial cancer and thromboembolic episodes (including pulmonary embolism) in those individuals who took the medication when compared with those who did not.
Oral contraceptives
As in the general population, oral contraceptives have been shown to have a protective effect against ovarian cancer in women with BRCA1/2 mutations. Two large multicenter case-control studies have reported risk reductions of 33% to 38%, with the maximum observed protection after ∼5 years of use.145,146
Breastfeeding
One recent study found that women with BRCA1 mutations who breastfed for a cumulative total of >1 year had a reduced risk of breast cancer that was statistically significant.147 However, the International BRCA1/2 Carrier Cohort Study found no association of breastfeeding with risk of breast cancer, and a trend for reduced ovarian cancer risk that was not statistically significant.148,149
Surveillance
Breast cancer screening
The breast cancer screening guidelines are based on data from families with BRCA1 or BRCA2 mutations, which indicate that elevated breast cancer risk begins in the late 20 s or early 30 s,150 and which report an increased risk of interval cancers.151 The guidelines reflect recent studies that have evaluated the efficacy of breast magnetic resonance imaging (MRI) screening in women with BRCA1/2 mutations.152–157 Despite variability in terms of the underlying population being studied, equipment and signal processing protocols, and the manner in which sensitivity and specificity are calculated, the studies consistently demonstrate that breast MRI is more sensitive than either mammography or ultrasound for the detection of hereditary breast cancer. In the combined studies, 82% of the cancers were identified by MRI compared with 40% by mammography, leading the American Cancer Society to recommend the use of annual MRI screening for women at hereditary risk for breast cancer.158
The National Comprehensive Cancer Network has published practice guidelines for the management of individuals with HBOC.106 Breast cancer screening guidelines include the following:
-
Monthly breast self-examination starting at the age of 18 years.
-
Semiannual clinical breast examination starting at the age of 25 years.
-
Annual mammogram and breast MRI screening starting at the age of 25 years or individualized based on the earliest age of breast cancer onset in the family.
Men with BRCA1/2 mutations are also at an increased risk for breast cancer. Although no formal program of surveillance has been recommended, breast self-examination training and regular monthly practice are advised, in addition to semiannual clinical breast examination and the consideration of a baseline mammogram followed by annual mammograms if gynecomastia or parenchymal/glandular breast density is detected on baseline study.
Ovarian cancer screening
The ovarian cancer screening measures available (transvaginal ultrasound examination and serum CA-125 concentration) have limited sensitivity and specificity and have not been shown to reduce ovarian cancer mortality,159 which is why prophylactic bilateral salpingo-oophorectomy is recommended for BRCA1/2 mutation carriers. However, semiannual concurrent transvaginal ultrasound and CA-125 are recommended for those women who have not elected to undergo prophylactic oophorectomy or who are delaying the procedure, starting at the age of 35 years, or individualized based on the earliest age of ovarian cancer onset in the family.
Prostate cancer screening
Men with BRCA1/2 mutations have an increased risk of prostate cancer and therefore should be informed about options for prostate cancer screening.150 The American Cancer Society recommends annual digital rectal examination and prostate-specific antigen testing beginning at the age of 50 years in the general population, with consideration of earlier screening for men in high-risk groups including those with a “strong familial predisposition.”160 Therefore, for men with BRCA1/2 mutations, prostate cancer surveillance is consistently recommended at the age of 40 years and older.
Pancreatic cancer screening
Pancreatic cancer is an established feature of the BRCA2 phenotype. However, the association of pancreatic cancer susceptibility and mutations in BRCA1 is less strong. Screening asymptomatic individuals for pancreatic cancer is not generally recommended but is available in research settings.
Melanoma screening
Because both cutaneous and ocular melanomas are part of the BRCA2 phenotype, annual clinical examinations of the skin and eye examinations by a specialist are recommended.161
Testing of relatives at risk
Once a BRCA1 or BRCA2 mutation has been identified in a family, testing of at-risk relatives can identify those family members who also have the familial mutation and thus need increased surveillance and early intervention when a cancer is diagnosed. See Genetic Counseling section for issues related to testing of at-risk relatives.
Hormone replacement therapy
General population studies suggest that long-term hormone replacement therapy (HRT) in postmenopausal women may increase breast cancer risk but that short-term use to treat menopausal symptoms does not. However, even relatively short-term combined estrogen plus progestin use was shown to increase the incidence of breast cancers in a randomized, placebo control trial of HRT.162
In 2005, Rebbeck et al.163 evaluated breast cancer risk associated with HRT after bilateral prophylactic oophorectomy in a cohort of 462 women with BRCA1/2 mutations and found that HRT of any type after bilateral prophylactic oophorectomy did not significantly alter the reduction in breast cancer risk associated with the surgery. The postoperative follow-up was 3.6 years. It was concluded that short-term HRT does not negate the protective effect of bilateral prophylactic oophorectomy on the risk of subsequent breast cancer in women with a BRCA1 or BRCA2 mutation. A second matched case-control study of 472 premenopausal women with BRCA1 mutations also failed to find an increased risk of breast cancer in HRT users.164
Smoking
Smoking does not appear to be a risk factor for breast cancer among individuals with a BRCA1 or BRCA2 mutation.165
Therapies under investigation
Therapies specifically targeted to the BRCA1 and/or BRCA2 pathways are under investigation166 but are beyond the scope of this review.
GENETIC COUNSELING
Mutations in the BRCA1 and BRCA2 genes are inherited in an autosomal dominant manner. Molecular genetic testing of asymptomatic family members at risk of inheriting either a BRCA1 or a BRCA2 mutation is feasible once the family-specific mutation has been identified. Prenatal testing is possible for pregnancies at an increased risk for a BRCA1 or BRCA2 mutation; however, requests for prenatal diagnosis of adult-onset diseases are uncommon and require careful genetic counseling.
Risk to parents of a proband with a BRCA1/2 mutation
Virtually, all individuals with a mutation in BRCA1 or BRCA2 have inherited it from a parent. However, the parent may or may not have had a personal cancer diagnosis depending on the penetrance of the mutation, the gender and age of the parent with the mutation, as well as other variables. It is appropriate to offer molecular genetic testing to both parents of an individual with a BRCA1 or BRCA2 mutation to determine which side of the family is at risk. Occasionally, neither parent will be identified as having the BRCA1 or BRCA2 mutation. The exact number of individuals with a BRCA1 or BRCA2 mutation that has occurred as a de novo event is not known but is believed to be small.167–169
Risk to siblings of a proband with a BRCA1/2 mutation
The risk to full siblings of an individual with a mutation in BRCA1 or BRCA2 depends on the genetic status of their parents. If one parent has the BRCA1 or BRCA2 mutation, then the risk for siblings to also carry the family-specific mutation is 50%. However, the risk of developing cancer depends on numerous variables including the penetrance of the mutation, the gender of the individual, and the age of the individual.
Risk to offspring of a proband with a BRCA1/2 mutation
The children of an individual identified as having a BRCA1 or BRCA2 mutation have a 50% chance of having inherited the mutation at the moment of conception. However, the risk of developing cancer again depends on numerous variables including the penetrance of the mutation, the gender of the individual, and age of the individual.
Risk to other family members of a proband with a BRCA1/2 mutation
The risk to other family members depends on the status of the proband's parents. If the parents are found to have the BRCA1 or BRCA2 mutation, their family members are also at risk to carry the same mutation. However, their exact risk depends on their position in the family. For example, the risk to a niece or nephew of a proband with a BRCA1 or BRCA2 mutation will be 25% based on pedigree assessment.
Related genetic counseling issues
-
Considerations in families with an apparent de novo mutation: When neither parent of a proband with an autosomal dominant condition has the disease-causing mutation or clinical evidence of the disorder, it is likely that the proband represents a new or de novo mutation. However, possible nonmedical explanations including alternate paternity or undisclosed adoption could also be explored. Although rare, de novo mutations in both BRCA1 and BRCA2 have been reported.167–169
-
Family planning: The optimal time for the determination of genetic risk is before pregnancy.
-
Genetic cancer risk assessment and counseling: There are medical, psychosocial, and ethical ramifications of identifying at-risk individuals through cancer risk assessment with or without molecular genetic testing that should be considered.170
-
At-risk asymptomatic adult relatives: In general, relatives of an individual who has a BRCA1 or BRCA2 mutation should be counseled regarding their risk of having inherited the same mutation, their options for molecular genetic testing, their cancer risk, and recommendations for cancer screening and prophylactic surgery. For those who choose to learn more about molecular genetic testing, it is suggested that pretest education includes discussion of the following113,171–173:
-
The individual's motivation for requesting testing and preconceived beliefs about the test (some at-risk asymptomatic adult family members may seek testing to make personal decisions regarding issues such as reproduction, financial matters, and career planning; others may simply “need to know.”)
-
The individual's perceptions of their risk of developing cancer.
-
The individual's readiness for testing and optimal timing for testing.
-
DNA banking (see below for explanation).
-
Inability of genetic testing to detect the presence or absence of cancer.
-
The individual's support systems and possible need for additional psychological support.
-
The individual's need for privacy and autonomy.
-
The possible effects of positive, negative, or uninformative test results on the following:
-
Cancer risk.
-
Cncer screening protocols.
-
Risk status for other family members.
-
Insurance coverage and employment. An individual found to have an inherited susceptibility to cancer could face discrimination in access to health insurance and/or employment although federal laws including the recent passage of the Genetic Information Non-Discrimination Act and state laws protect against health insurance and employment discrimination.
-
Individual's emotional status (e.g., depression, anxiety, and guilt).
-
Relationships with partner, children, extended family, and friends.
At-risk adult relatives who have not inherited the mutation identified in the proband are presumed to be at or above the general population risk of developing cancer, depending on personal risk factors. For example, a female at-risk relative who does not carry the family-specific BRCA1 or BRCA2 mutation may still be at an elevated risk of breast cancer based on a breast biopsy history, which revealed atypical ductal hyperplasia. For family members determined to be at general population risk of developing cancer, appropriate cancer screening such as that recommended by the American Cancer Society or the National Comprehensive Cancer Network for individuals of average risk is recommended. It is important to note that this presumption cannot apply to individuals who tested negative for a BRCA1 or BRCA2 mutation if the affected proband in the family either has not undergone molecular genetic testing of BRCA1 or BRCA2 or did not have an identified BRCA1 or BRCA2 mutation.
-
At-risk asymptomatic minor relatives: Legitimate concerns regarding testing of at-risk individuals younger than 18 years of age for adult-onset conditions (including BRCA1 or BRCA2 mutations) exist, including issues of informed consent among minors, the lack of proven surveillance or prevention strategies at that age, and concerns about stigmatization and discrimination. Such testing is typically not recommended.174
-
DNA banking: DNA banking is the storage of DNA (typically extracted from white blood cells) for possible future use. Because it is likely that testing methodology and our understanding of genes, mutations, and diseases will improve in the future, consideration should be given to banking DNA of affected individuals. DNA banking is particularly relevant in situations in which the sensitivity of currently available testing is <100%.
Prenatal testing
Prenatal testing for BRCA1 or BRCA2 mutations is technically feasible by analysis of DNA extracted from fetal cells obtained by amniocentesis usually performed at about 15 to 18 weeks' gestation or chorionic villus sampling at about 10 to 12 weeks' gestation. The BRCA1 or BRCA2 mutation must be identified in the family before prenatal testing can be performed.
Requests for prenatal testing for adult-onset conditions, including BRCA1 and BRCA2 mutations, that do not affect intellect and have some treatment options available are uncommon. Differences in perspective may exist among medical professionals and within families regarding the use of prenatal testing, particularly if the testing is being considered for the purpose of pregnancy termination rather than early diagnosis. Although most centers would consider decisions about prenatal testing to be the choice of the parents, careful discussion of these issues is appropriate.
-
Preimplantation genetic diagnosis: This technology may be available for families in which the mutation has been identified in the family.
RESOURCES
Web-based resources and links for HBOC due to BRCA1 and BRCA2 mutations:
Genomic databases
-
Breast Cancer Information Core National Human Genome Research Institute Cancer Genetics Branch (research. nhgri.nih.gov/bic/resources.shtml).
-
GeneReviews (genetests.org), BRCA1 and BRCA2 (http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=brca1).
-
National Cancer Institute (NCI), Breast cancer (http://www.cancer.gov/templates/doc.aspx?viewid=0b3dd146-d194-4dac-a447-8484b552c072).
-
NCI, Ovarian cancer (Ovarian cancer, http://www.cancer.gov/cancertopics/types/ovarian/).
-
NCI, Genetics of breast and ovarian cancer (http://www.cancer.gov/cancertopics/pdq/genetics/breast-and-ovarian/HealthProfessional/page1).
-
Online Mendelian Inheritance in Man, Breast Cancer, Type 1 (http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=113705).
-
Online Mendelian Inheritance in Man, Breast Cancer, Type 2 (http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=600185).
Organizations and lay websites
-
American Cancer Society (www.cancer.org).
-
Breast Cancer Network of Strength (www.networkofstrength.org).
-
CancerCare (www.cancercare.org).
-
Facing Our Risk of Cancer Empowered (www.facingourrisk.org).
-
Gilda's Club (www.gildasclub.org).
-
Hereditary Breast and Ovarian Cancer Foundation (www.hboc.ca).
-
National Alliance of Breast Cancer Organizations (www.nabco.org).
-
The National Breast Cancer Coalition (www.stopbreastcancer.org).
-
National Library of Medicine Genetics Home Reference, Breast Cancer (http://ghr.nlm.nih.gov/ghr/disease/breastcancer).
-
National Ovarian Cancer Coalition (www.ovarian.org).
-
National Center for Biotechnology Information Genes and Disease, Breast and ovarian cancer (http://www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View.ShowSection&rid=gnd.section.99).
-
The National Coalition for Cancer Survivorship (www.canceradvocacy.org).
-
Sharsheret (www.sharsheret.org).
-
The Susan G. Komen Breast Cancer Foundation (www.breastcancerinfo.com).
Published statements and policies regarding genetic testing
-
American Society of Clinical Oncology (2003) Policy statement: Genetic testing for cancer susceptibility.113
-
American Society of Clinical Oncology; recommended breast cancer surveillance guidelines.171
-
National Society of Genetic Counselors (1997) Statement on genetic testing for adult-onset disorders.173
-
American Society of Human Genetics and American College of Medical Genetics (1995) Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents.174
References
Easton DF, Ford D, Bishop DT . Breast and ovarian cancer incidence in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Am J Hum Genet 1995; 56: 265–271.
Hopper JL, Southey MC, Dite GS, et al. Population-based estimate of the average age-specific cumulative risk of breast cancer for a defined set of protein-truncating mutations in BRCA1 and BRCA2. Australian Breast Cancer Family Study. Cancer Epidemiol Biomarkers Prev 1999; 8: 741–747.
Porter DE, Cohen BB, Wallace MR, et al. Breast cancer incidence, penetrance and survival in probable carriers of BRCA1 gene mutation in families linked to BRCA1 on chromosome 17q12-21. Br J Surg 1994; 81: 1512–1515.
Marcus JN, Watson P, Page DL, et al. Hereditary breast cancer: pathobiology, prognosis, and BRCA1 and BRCA2 gene linkage. Cancer 1996; 77: 697–709.
Foulkes WD, Wong N, Brunet JS, et al. Germ-line BRCA1 mutation is an adverse prognostic factor in Ashkenazi Jewish women with breast cancer. Clin Cancer Res 1997; 3: 2465–2469.
Ansquer Y, Gautier C, Fourquet A, Asselain B, Stoppa-Lyonnet D . Survival in early-onset BRCA1 breast-cancer patients. Institut Curie Breast Cancer Group. Lancet 1998; 352: 541.
Stoppa-Lyonnet D, Ansquer Y, Dreyfus H, et al. Familial invasive breast cancers: worse outcome related to BRCA1 mutations. J Clin Oncol 2000; 18: 4053–4059.
Brekelmans CT, Seynaeve C, Menke-Pluymers M, et al. Survival and prognostic factors in BRCA1-associated breast cancer. Ann Oncol 2006; 17: 391–400.
Brunet JS, Narod SA, Tonin P, Foulkes WD . BRCA1 mutations and survival in women with ovarian cancer. N Engl J Med 1997; 336: 1256.
Zweemer RP, Verheijen RH, Coebergh JW, et al. Survival analysis in familial ovarian cancer: a case control study. Eur J Obstet Gynecol Reprod Biol 2001; 98: 219–223.
Buller RE, Shahin MS, Geisler JP, Zogg M, De Young BR, Davis CS . Failure of BRCA1 dysfunction to alter ovarian cancer survival. Clin Cancer Res 2002; 8: 1196–1202.
Rubin SC, Benjamin I, Behbakht K, et al. Clinical and pathological features of ovarian cancer in women with germ-line mutations of BRCA1. N Engl J Med 1996; 335: 1413–1416.
Burk RD . BRCA1 mutations and survival in women with ovarian cancer. N Engl J Med 1997; 336: 1255.
Whitmore SE . BRCA1 mutations and survival in women with ovarian cancer. N Engl J Med 1997; 336: 1254–1255.
Cannistra SA . BRCA1 mutations and survival in women with ovarian cancer. N Engl J Med 1997; 17: 1254.
Aida H, Takakuwa K, Nagata H, et al. Clinical features of ovarian cancer in Japanese women with germ-line mutations of BRCA1. Clin Cancer Res 1998; 4: 235–240.
Cass I, Baldwin RL, Varkey T, Moslehi R, Narod SA, Karlan BY . Improved survival in women with BRCA-associated ovarian carcinoma. Cancer 2003; 97: 2187–2195.
Tan DSP, Rothermundt C, Thomas K, et al. “BRCAness” syndrome in ovarian cancer: a case-control study describing the clinical features and outcome of patients with epithelial ovarian cancer associated with BRCA1 and BRCA2 mutations. J Clin Oncol 2008; 26: 5530–5536.
Chetrit A, Jirsh-Yechezkel G, Ben-David Y, Lubin F, Friedman E, Sadetzki S . Effect of BRCA1/2 mutations on long-term survival of patients with invasive ovarian cancer: the National Israeli Study of Ovarian Cancer. J Clin Oncol 2008; 26: 20–25.
Claus EB, Schildkraut JM, Thompson WD, Risch NJ . The genetics attributable risk of breast and ovarian cancer. Cancer 1996; 77: 2318–2324.
Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE . Risks of cancer in BRCA1-mutation carriers. Breast Cancer Lingage Consortium. Lancet 1994; 343: 692–695.
Whittemore AS, Gong G, Itnyre J . Prevalence and contribution of BRCA1 mutations in breast cancer and ovarian cancer: results from 3 population-based case-control studies of ovarian cancer. Am J Hum Genet 1997; 60: 496–504.
Szabo CI, King MC . Population genetics of BRCA1 and BRCA2. Am J Hum Genet 1997; 60: 1013–1020.
Leide A, Narod SA . Hereditary breast and ovarian cancer in Asia: genetic epidemiology of BRCA1 and BRCA2. Hum Mutat 2002; 20: 413–424.
Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C . Breast cancer genetics in African Americans. Cancer 2003; 97( suppl 1): 236–245.
John E, Miron A, Gong G, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 racial/ethnic groups. JAMA 2007; 298: 2869–2876.
Haffty BG, Silber A, Matloff E, Chung J, Lannin D . Racial differences in the incidence of BRCA1 and BRCA2 mutations in a cohort of early onset breast cancer patients: African American compared to white women. J Med Genet 2006; 43: 133–137.
Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 1997; 336: 1401–1408.
King MC, Marks JH, Mandell JB, New York Breast Cancer Study Group Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 2003; 302: 643–646.
Oddoux C, Struewing JP, Clayton CM, et al. The carrier frequency of the BRCA2 6174delT mutation among Ashkenazi Jewish individuals is approximately 1%. Nat Genet 1996; 14: 188–190.
Struewing JP, Abeliovich D, Peretz T, et al. The carrier frequency of the BRCA1 185delAG mutation is approximately 1 percent in Ashkenazi Jewish individuals. Nat Genet 1995; 11: 198–200.
Roa BB, Boyd AA, Volcik K, Richards CS . Ashkenazi Jewish population frequencies for common mutations in BRCA1 and BRCA2. Nat Genet 1996; 14: 185–187.
Berman DB, Costalas J, Schultz DC, Grana G, Daly M, Godwin AK . A common mutation in BRCA2 that predisposes to a variety of cancers is found in both Jewish Ashkenazi and non-Jewish individuals. Cancer Res 1996; 56: 3409–3414.
Offit K, Gilewski T, McGuire P, et al. Germline BRCA1 185delAG mutations in Jewish women with breast cancer. Lancet 1996; 347: 1643–1645.
Petrij-Bosch A, Peelen T, van Vliet M, et al. BRCA1 genomic deletions are major founder mutations in Dutch breast cancer patients. Nat Genet 1997; 17: 341–345.
Thorlacius S, Struewing JP, Hartge P, et al. Population-based study of risk of breast cancer in carriers of BRCA2 mutation. Lancet 1998; 352: 1337–1339.
Thorlacius S, Olafsdottir G, Tryggvadottir L, et al. A single BRCA2 mutation in male and female breast cancer families from Iceland with varied cancer phenotypes. Nat Genet 1996; 13: 117–119.
Ferla R, Calo V, Cascio S, et al. Founder mutations in BRCA1 and BRCA2 genes. Ann Oncol 2007; 18: vi93–vi98.
Miki Y, Swensen J, Shattuck-Eidens D, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science 1994; 266: 66–71.
Deng CX . BRCA1: cell cycle checkpoint, genetic instability, DNA damage response and cancer evolution. Nucleic Acids Res 2006; 34: 1416–1426.
Rosen EM, Fan S, Ma X . BRCA1 regulation of transcription. Cancer Lett 2006; 236: 175–185.
Zhang H, Tombline G, Weber BL . BRCA1, BRCA2, and DNA damage response: collision or collusion?. Cell 1998; 92: 433–436.
Smith SA, Easton DF, Evans DG, Ponder BA . Allele losses in the region 17q12–21 in familial breast and ovarian cancer involve the wild-type chromosome. Nat Genet 1992; 2: 128–131.
King TA, Li W, Brogi E, et al. Heterogenic loss of the wild-type BRCA allele in human breast tumorigenesis. Ann Surg Oncol 2007; 14: 2510–2518.
Brodie SG, Deng CX . BRCA1-associated tumorigenesis: what have we learned from knockout mice?. Trends Genet 2001; 17: S18–S22.
Deng CX . Tumor formation in Brca1 conditional mutant mice. Environ Mol Mutagen 2002; 39: 171–177.
Venkitaraman AR . Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 2002; 108: 171–182.
Bertwistle D, Swift S, Marston NJ, et al. Nuclear location and cell cycle regulation of the BRCA2 protein. Cancer Res 1997; 57: 5485–5488.
Venkitaraman AR . Functions of BRCA1 and BRCA2 in the biological response to DNA damage. J Cell Sci 2001; 114: 3591–3598.
Antoniou A, Pharoah PD, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected fro family history: a combined analysis of 222 studies. Am J Hum Genet 2003; 72: 1117–1130.
Risch HA, McLaughlin JR, Cole DE, et al. Population BRCA1 and BRCA2 mutation frequencies and cancer penetrances: a kin-cohort study in Ontario, Canada. J Natl Cancer Inst 2006; 98: 1694–1706.
Chen S, Iversen ES Jr, Friebel T, et al. Characterization of BRCA1 and BRCA2 mutations in a large US sample. J Clin Oncol 2006; 24: 863–871.
Metcalfe K, Lynch HT, Ghadirian P, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol 2004; 22: 2328–2335.
Medeiros F, Muto MG, Lee Y, et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am J Surg Pathol 2006; 30: 230–236.
Casey MJ, Snyder C, Bewtra C, Narod SA, Watson P, Lynch HT . Intraabdominal carcinomatosis after prophylactic oophorectomy in women from hereditary breast/ovarian syndrome kindreds associated with BRCA1 and BRCA2 mutations. Gynecol Oncol 2005; 97: 457–467.
Finch A, Beiner M, Lubinski J, et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube and peritoneal cancers in women with a BRCA1 or BRCA2 mutation. JAMA 2006; 296: 185–192.
Thompson D, Easton DF . The breast cancer linkage consortium. Cancer incidence in BRCA1 mutation carriers. J Natl Cancer Inst 2002; 94: 1358–1365.
Cybulski C, Gorski B, Gronwald J, et al. BRCA1 mutations and prostate cancer risk in Poland. Eur J Cancer Prev 2008; 17: 62–66.
Giusti RM, Rutter JL, Duray PH, et al. A twofold increase in BRCA-mutation-related prostate cancer among Ashkenazi Israelis is not associated with distinctive histopathology. J Med Genet 2003; 40: 787–792.
Brose MS, Rebbeck TR, Calzone KA, Stopfer JE, Nathanson KL, Weber BL . Cancer risk estimates for BRCA1 mutation carriers identified in a risk evaluation program. J Natl Cancer Inst 2002; 94: 1365–1372.
Lynch HT, Deters CA, Snyder CL, et al. BRCA1 and pancreatic cancer—pedigree findings and their causal relationships. Cancer Genet Cytogenet 2005; 158: 119–125.
Fentiman IS, Fourquet A, Hortobagyi GN . Male breast cancer. Lancet 2006; 367: 595–604.
Tai YC, Domchek S, Parmigiani G, Chen S . Breast cancer risk among male BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 2007; 99: 1811–1814.
Beiner ME, Finch A, Rosen B, et al. The risk of endometrial cancer in women with BRCA1 and BRCA2 mutations—a prospective study. Gynecol Oncol 2007; 104: 7–10.
Chen S, Parmigiani G . Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 2007; 25: 1329–1333.
Risch HA, McLaughlin JR, Cole DE, et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 2001; 68: 700–710.
Aziz S, Kuperstein G, Rosen B, et al. A genetic epidemiology study of carcinoma of the fallopian tube. Gynecol Oncol 2001; 80: 341–345.
Breast Cancer Linkage Consortium Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 1999; 91: 1310–1316.
Tryggvadottir L, Vidarsdottir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst 2007; 99: 929–935.
Petersen GM, Hruban RH . Familial pancreatic cancer—where are we in 2003?. J Natl Cancer Inst 2003; 95: 180–181.
Van Asperen CJ, Brohet RM, Meijers-Heijboer EJ, et al. Cancer risks in BRCA2 families: estimates for sites other than breast and ovary. J Med Genet 2005; 42: 711–719.
Antoniou AC, Pharoah PD, Narod S, et al. Breast and ovarian cancer risks to carriers of the BRCA1 5382insC and 185delAG and BRCA2 6174delT mutations: a combined analysis of 22 population based studies. J Med Genet 2005; 42: 602–603.
Satagopan JM, Offit K, Foulkes W, et al. The lifetime risks of breast cancer in Ashkenazi Jewish carriers of BRCA1 and BRCA2 mutations. Cancer Epidemiol Biomarkers Prev 2001; 10: 467–473.
Satagopan JM, Boyd J, Kauff ND, et al. Ovarian cancer risk in Ashkenazi Jewish carrier of BRCA1 and BRCA2 mutations. Clin Cancer Res 2002; 8: 3776–3781.
Lubinski J, Phelan CM, Ghadirian P, et al. Cancer variation associated with the position of the mutation in the BRCA2 gene. Fam Cancer 2004; 3: 1–10.
Gaffney DK, Brohet RM, Lewis CM, et al. Response to radiation therapy and prognosis in breast cancer patients with BRCA1 and BRCA2 mutations. Radiother Oncol 1998; 47: 129–136.
Johannsson OT, Ranstam J, Borg A, Olsson H . Survival of BRCA1 breast and ovarian cancer patients: a population-based study from southern Sweden. J Clin Oncol 1998; 16: 397–404.
Verhoog LC, Brekelmans CT, Seynaeve C, et al. Survival and tumour characteristics of breast-cancer patients with germline mutations of BRCA1. Lancet 1998; 351: 316–321.
Lee JS, Wacholder S, Struewing JP, et al. Survival after breast cancer in Ashkenazi Jewish BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 1999; 91: 259–263.
Verhoog LC, Brekelmans CT, Seynaeve C, et al. Survival in hereditary breast cancer associated with germline mutations of BRCA2. J Clin Oncol 1999; 17: 3396–3402.
Rennert G, Bisland-Naggan S, Barnett-Griness O, et al. Clinical outcomes of breast cancer in carriers of BRCA1 and BRCA2 mutations. N Engl J Med 2007; 357: 115–123.
Robson ME, Chappuis PO, Satagopan J, et al. A combined analysis of outcome following breast cancer: difference in survival based on BRCA1/BRCA2 mutation status and administration of adjuvant treatment. Breast Cancer Res 2004; 6: R8–R17.
Robson M, Levin D, Federici M, et al. Breast conservation therapy for invasive breast cancer in Ashkenazi women with BRCA gene founder mutations. J Natl Cancer Inst 1999; 91: 2112–2117.
Haffty BG, Harrold E, Khan AJ, et al. Outcome of conservatively managed early-onset breast cancer by BRCA1/2 status. Lancet 2002; 359: 1471–1477.
Seynaeve C, Verhoog LC, van de Bosch LM, et al. Ipsilateral breast tumour recurrence in hereditary breast cancer following breast-conserving therapy. Eur J Cancer 2004; 40: 1150–1158.
Pierce LJ, Levin AM, Rebbeck TR, et al. Ten-year multi-institutional results of breast-conserving surgery and radiotherapy in BRCA1.2-associated stage I/II breast cancer. J Clin Oncol 2006; 24: 2437–2443.
Byrd LM, Shenton A, Maher ER, et al. Better life expectancy in women with BRCA2 compared with BRCA1 mutations is attributable to lower frequency and later onset of ovarian cancer. Cancer Epidemiol Biomarkers Prev 2008; 17: 1535–1542.
Pal T, Permuth-Wey J, Kapoor R, Cantor A, Sutphen R . Improved survival in BRCA2 carriers with ovarian cancer. Fam Cancer 2007; 6: 113–119.
Lafarge S, Sylvain V, Ferrara M, Bignon Y . Inhibition of BRCA1 leads to increased chemoresistance to microtubule-interfering agents, an effect that involves the JNK pathway. Oncogene 2001; 20: 6597–6606.
Quinn JE, Kennedy RD, Mullan PB, Gilmore PM, Carty M, Johnston PG . BRCA1 functions as a differential modulator or chemotherapy-induced apoptosis. Cancer Res 2003; 63: 6221–6228.
Narod SA, Neuhausen S, Vichodez G, et al. Rapid progression of prostate cancer in men with a BRCA2 mutation. Br J Cancer 2008; 99: 371–374.
Agalliu I, Gern R, Leanza S, Burk RD . Associations of high-grade prostate cancer with BRCA1 and BRCA2 founder mutations. Clin Cancer Res 2009; 15: 1112–1119.
Tryggvadóttir L, Vidarsdóttir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst 2007; 99: 929–935.
Rakha EA, Reis-Filho JS, Ellis IO . Basal-like breast cancer: a critical review. J Clin Oncol 2008; 26: 2568–2581.
Foulkes WD, Stefansson IM, Chappuis PO, et al. Gerrmline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 2003; 95: 1482–1485.
Lacroix M, Leclercq G . The “portrait” of hereditary breast cancer. Breast Cancer Res Treat 2005; 89: 297–304.
Lakhani SR, Reis-Filho JS, Fulford L, Breast Cancer Linkage Consortium et al. Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res 2005; 11: 5175–5180.
Claus EB, Petruzella S, Matloff E, Carter D . Prevalence of BRCA1 and BRCA2 mutations in women diagnosed with ductal carcinoma in situ. JAMA 2005; 293: 964–969.
Hwang ES, McLennan JL, Morre DH, Crawford BB, Esserman LJ, Ziegler JL . Ductal carcinoma in situ in BRCA mutation carriers. J Clin Oncol 2007; 25: 642–647.
Smith KL, Adank M, Kauff N, et al. BRCA mutations in women with ductal carcinoma in situ. Clin Cancer Res 2007; 13: 4306–4310.
Berchuck A, Heron KA, Carney ME, et al. Frequency of germline and somatic BRCA1 mutations in ovarian cancer. Clin Cancer Res 1998; 4: 2433–2437.
Lu KH, Cramer DW, Muto MG, Li EY, Niloff J, Mok SC . A population-based study of BRCA1 and BRCA2 mutations in Jewish women with epithelial ovarian cancer. Obstet Gynecol 1999; 93: 34–37.
Jazaeri AA, Yee CJ, Sotiriou C, Brantley KR, Boyd J, Liu ET . Gene expression profiles of BRCA1-linked, BRCA2-linked, and sporadic ovarian cancers. J Natl Cancer Inst 2002; 94: 990–1000.
Crum CP, Drapkin R, Kindelberger D, Medeiros F, Miron A, Lee Y . Lessons from BRCA: the tubal fimbria emerges as an origin for pelvic serous cancer. Clin Med Res 2007; 5: 35–44.
Carlson JW, Miron A, Jarboe EA, et al. Serous tubal intraepithelial carcinoma: its potential role in primary peritoneal serous carcinoma and serous cancer prevention. J Clin Oncol 2008; 26: 4160–4165.
National Comprehensive Cancer Network, Clinical Practice Guidelines in Oncology, Genetic/Familial High-Risk Assessment: Breast and Ovarian, 2009. Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed October 30, 2009.
Weitzel JN, Lagos VI, Cullinane CA, et al. Limited family structure and BRCA gene mutation status in single cases of breast cancer. JAMA 2007; 297: 2587–2595.
Parmigiani G, Berry D, Aguilar O . Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet 1998; 62: 145–158.
Frank TS, Deffenbaugh AM, Reid JE, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 2002; 20: 1480–1490.
Evans DG, Eccles DM, Rahman N, et al. A new scoring system for the chances of identifying a BRCA1/2 mutation outperforms existing models including BRCAPRO. J Med Genet 2004; 41: 474–480.
Antoniou AC, Pharoah PP, Smith P, Easton DF . The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer 2004; 91: 1580–1590.
Tyrer J, Duffy SW, Cuzick J . A breast cancer prediction model incorporating familial and personal risk factors. Stat Med 2004; 23: 1111–1130.
ASCO Working Group on Genetic Testing for Cancer Susceptibility American society of clinical oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol 2003; 21: 1–10.
Frank TS, Manley SA, Olopade OI, et al. Sequence analysis of BRCA1 and BRCA2: correlation of mutations with family history and ovarian cancer risk. J Clin Oncol 1998; 16: 2417–2425.
BRCA1 Exon 13 Duplication Screening Group The exon 13 duplication in the BRCA1 gene is a founder mutation present in geographically diverse populations. Am J Hum Genet 2000; 67: 207–212.
Rohlfs EM, Puget N, Graham ML, et al. An Alu-mediated 7.1 kb deletion of BRCA1 exons 8 and 9 in breast and ovarian cancer families that results in alternative splicing of exon 10. Genes Chromosomes Cancer 2000; 28: 300–307.
Walsh T, Casadei S, Coats KH, et al. Spectrum of mutations in BRCA1, BRCA2, CHEKs, and TP53 in families at high risk of breast cancer. JAMA 2006; 295: 1379–1388.
Unger MA, Nathanson KL, Calzone K, et al. Screening for genomic rearrangements in families with breast and ovarian cancer identifies BRCA1 mutations previously missed by conformation-sensitive gel electrophoresis or sequencing. Am J Hum Genet 2000; 67: 841–850.
Ramus SJ, Fishman A, Pharoah PD, Yarkoni S, Altaras M, Ponder BA . Ovarian cancer survival in Ashkenazi Jewish patients with BRCA1 and BRCA2 mutations. Eur J Surg Oncol 2001; 27: 278–281.
Naderi A, Couch FJ . BRCA2 and pancreatic cancer. Int J Gastrointest Cancer 2002; 31: 99–106.
Hahn SA, Greenhalf B, Ellis I, et al. BRCA2 germline mutations in familial pancreatic carcinoma. J Natl Cancer Inst 2003; 95: 214–221.
Howlett NG, Taniguchi T, Olson S, et al. Biallelic inactivation of BRCA2 in Fanconi anemia. Science 2002; 297: 606–609.
Lindor NM, McMaster ML, Lindor CJ, Greene MH . Concise handbook of familial cancer susceptibility syndromes—second edition. J Natl Cancer Inst Monogr 2008; 38: 1–93.
Westenend PJ, Schutte R, Hoogmans MM, Wagner A, Dinjens WN . Breast cancer in an MSH2 gene mutation carrier. Hum Pathol 2005; 36: 1322–1326.
Muller A, Edmonston TB, Corao DA, et al. Exclusion of breast cancer as an integral tumor of hereditary nonpolyposis colorectal cancer. Cancer Res 2002; 62: 1014–1019.
Foulkes W, Ghadirian P, Akbari MR, et al. Identification of a novel truncating PALB2 mutation and analysis of its contribution to early-onset breast cancer in French-Canadian women. Breast Cancer Res 2007; 9: 1–9.
De Nicolo A, Tancredi M, Lombardi G, et al. A novel breast cancer-associated BRIP1 (FANCJ/BACH1) germ-line mutation impairs protein stability and function. Clin Cancer Res 2008; 14: 4672–4680.
Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med 1999; 340: 77–84.
Hartmann LC, Sellers TA, Schaid DJ, et al. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst 2001; 93: 1633–1637.
Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2004; 22: 1055–1062.
Kauff ND, Satagopan JM, Robson ME, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 2002; 346: 1609–1615.
Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 2002; 346: 1616–1622.
Rutter JL, Wacholder S, Chetrit A, et al. Gynecologic surgeries and risk of ovarian cancer in women with BRCA1 and BRCA2 Ashkenazi founder mutations: an Israeli population-based case-control study. J Natl Cancer Inst 2003; 95: 1072–1078.
Leeper K, Garcia R, Swisher E, Goff B, Greer B, Paley P . Pathologic findings in prophylactic oophorectomy specimens in high-risk women. Gynecol Oncol 2002; 87: 52–56.
Olivier RI, van Beurden M, Lubsen MA, et al. Clinical outcome of prophylactic oophorectomy in BRCA1/BRCA2 mutation carriers and events during follow-up. Br J Cancer 2004; 90: 1492–1497.
Powell CB, Kenley E, Chen LM, et al. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol 2005; 23: 127–132.
Piver MS, Jishi MF, Tsukada Y, Nava G . Primary peritoneal carcinoma after prophylactic oophorectomy in women with a family history of ovarian cancer. A report of the Gilda Radner Familial Ovarian Cancer Registry. Cancer 1993; 71: 2751–2755.
Olopade OI, Artioli G . Efficacy of risk-reducing salpingo-oophorectomy in women with BRCA-1 and BRCA-2 mutations. Breast J 2004; 1: S5–S59.
Kauff ND, Domchek SM, Friebel TM, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol 2008; 26: 1331–1337.
Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 1998; 90: 1371–1388.
Gail MH, Costantino JP, Bryant J, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst 1999; 91: 1829–1846.
King MC, Wieand S, Hale K, National Surgical Adjuvant Breast and Bowel Project et al. Tamoxifen and breast cancer incidence among women with inherited mutations in BRCA1 and BRCA2: National Surgical Adjuvant Breast and Bowel Project (NSABP-P1) Breast Cancer Prevention Trial. JAMA 2001; 286: 2251–2256.
Narod SA, Brunet JS, Ghadirian P, Hereditary Breast Cancer Clinical Study Group et al. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Hereditary Breast Cancer Clinical Study Group. Lancet 2000; 356: 1876–1881.
Metcalfe KA, Lynch HT, Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol 2005; 96: 222–226.
Narod SA, Risch H, Moslehi R, et al. Oral contraceptives and the risk of hereditary ovarian cancer. Hereditary Ovarian Cancer Clinical Study Group. N Engl J Med 1998; 339: 424–428.
Whittemore AS, Balise RR, Pharoah PD, et al. Oral contraceptive use and ovarian cancer risk among carriers of BRCA1 or BRCA2 mutations. Br J Cancer 2004; 91: 1911–1915.
Jernstrom H, Lubinski J, Lynch HT, et al. Breast-feeding and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 2004; 96: 1094–1098.
Andrieu N, Goldgar D, Easton DF, EMBRACE GENEPSO GEO-HEBON IBCCS Collaborators Group et al. Pregnancies, breast-feeding, and breast cancer risk in the International BRCA1/2 Carrier Cohort Study (IBCCS). J Natl Cancer Inst 2006; 98: 535–544.
Antoniou AC, Rookus M, Andrieu N, et al. Reproductive and hormonal factors, and ovarian cancer risk for BRCA1 and BRCA2 mutation carriers: results from the International BRCA1/2 Carrier Cohort Study. Cancer Epidemiol Biomarkers Prev 2009; 18: 601–610.
Burke W, Daly M, Garber J, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer Genetics Studies Consortium. JAMA 1997; 277: 997–1003.
Hagen AI, Kvistad KA, Maehle L, et al. Sensitivity of MRI versus conventional screening in the diagnosis of BRCA-associated breast cancer in a national prospective series. Breast 2007; 16: 367–374.
Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol 2005; 23: 8469–8476.
Kriege M, Brekelmans CT, Boetes C, Magnetic Resonance Imaging Screening Study Group et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 2004; 351: 427–437.
Warner E, Plewes DB, Hill KA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA 2004; 292: 1317–1325.
Warner E, Causer PA . MRI surveillance for hereditary breast-cancer risk. Lancet 2005; 365: 1747–1749.
Lehman CD, Blume JD, Weatherall P, et al. Screening women at high risk for breast cancer with mammography and magnetic resonance imaging. Cancer 2005; 103: 1898–1905.
Leach MO, Boggis CR, Dixon AK, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 2005; 365: 1769–1778.
Saslow D, Boetes C, Burke W, American Cancer Society Breast Cancer Advisory Group et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57: 75–89.
Clarke-Pearson DL . Screening for ovarian cancer. N Engl J Med 2009; 361: 170–177.
Mettlin C, Jones G, Averette H, Gusberg SB, Murphy GP . Defining and updating the American Cancer Society guidelines for the cancer-related checkup: prostate and endometrial cancers. CA Cancer J Clin 1993; 43: 42–46.
Liede A, Karlan BY, Narod SA . Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol 2004; 22: 735–742.
Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women's Health Initiative Randomized Trial. JAMA 2003; 289: 3243–3253.
Rebbeck TR, Friebel T, Wagner T, PROSE Study Group et al. Effect of short-term hormone replacement therapy on breast cancer risk reduction after bilateral prophylactic oophorectomy in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2005; 23: 7804–7810.
Lubinski EA, Gronwald J, Moller P, et al. Hormone therapy and the risk of breast cancer in BRCA1 mutation carriers. J Natl Cancer Inst 2008; 100: 1361–1367.
Ghadirian P, Lubinski J, Lynch H, et al. Smoking and the risk of breast cancer among carriers of BRCA mutations. Int J Cancer 2004; 110: 413–416.
Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005; 434: 917–921.
Tesoriero A, Anderson C, Southey M, et al. De novo BRCA1 mutation in a patient with breast cancer and an inherited BRCA2 mutation. Am J Hum Genet 1999; 65: 567–569.
Robson M, Scheuer L, Nafa K, Ellis N, Offit K . Unique de novo mutation of BRCA2 in a woman with early onset breast cancer. J Med Genet 2002; 39: 664–669.
van der Luijt RB, van Zon PH, Jansen RP, van der Sijs-Bos CJ, Warlam-Rodenhuis CC, Ausems MG . De novo recurrent germline mutation of the BRCA2 gene in a patient with early onset breast cancer. J Med Genet 2001; 38: 102–105.
Trepanier A, Ahrens M, McKinnon W, et al. Genetic cancer risk assessment and counseling: recommendations of the National Society of Genetic Counselors. J Genet Couns 2004; 13: 83–114.
American Society of Clinical Oncology Recommended breast cancer surveillance guidelines. J Clin Oncol 1997; 15: 2149–2156.
Geller G, Botkin JR, Green MJ, et al. Genetic testing for susceptibility to adult-onset cancer. The process and content of informed consent. JAMA 1997; 277: 1467–1474.
McKinnon WC, Baty BJ, Bennett RL, et al. Predisposition genetic testing for late-onset disorders in adults. A position paper of the National Society of Genetic Counselors. JAMA 1997; 278: 1217–1220.
The American Society of Hum Genet Board of Directors The American College of Medical Genetics Board of Directors ASHG/ACMG Report. Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents. Am J Hum Genet 1995; 57: 1233–1241.
Acknowledgements
The authors thank Dr. Roberta Pagon and the staff at www.genetests.org for their continued direction and editorial assistance in the development and updates of the GeneReview on BRCA1 and BRCA2 as well as their support and encouragement for its adaptation in the form of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Petrucelli, N., Daly, M. & Feldman, G. Hereditary breast and ovarian cancer due to mutations in BRCA1 and BRCA2. Genet Med 12, 245–259 (2010). https://doi.org/10.1097/GIM.0b013e3181d38f2f
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181d38f2f
Keywords
This article is cited by
-
PALB2 germline mutations in a large cohort of Middle Eastern breast-ovarian cancer patients
Scientific Reports (2023)
-
Screening and identification of phytochemical drug molecules against mutant BRCA1 receptor of breast cancer using computational approaches
Molecular and Cellular Biochemistry (2022)
-
Prostata- und Mammakarzinom: Gemeinsamkeiten und Unterschiede
Die Urologie (2022)
-
Efficient C•G-to-G•C base editors developed using CRISPRi screens, target-library analysis, and machine learning
Nature Biotechnology (2021)
-
Sustained, local delivery of the PARP inhibitor talazoparib prevents the development of mammary gland hyperplasia in Brca1-deficient mice
Scientific Reports (2021)