Abstract
The utility of molecular diagnostics in clinical practice has been steadily increasing and is expected to continue to do so as the applications of genomic medicine increase. The goal of this article was to describe the roles and responsibilities of genetic counselors who work in the customer service area of molecular diagnostics laboratories. In this role, genetic counselors provide recommendations to clinicians on issues that are specific to DNA-based testing. This article will address some issues that are specifically relevant to disease genetic tests. Many molecular diagnostic laboratories employ genetic counselors, who have extensive training in how to communicate genetic information, to provide information in the preanalytic, analytic, and postanalytic stages of testing. To maximize the quality of the service, it is important to establish an understanding of what can be expected of both the practitioner and the laboratory genetic counselor. Although some complications in the laboratory cannot be anticipated, discussing the case with the laboratory genetic counselors beforehand may avert certain problems. This article discusses real cases from laboratory genetic counselors to illustrate issues that arise due to technical difficulties and the inherent limitations of molecular testing. The summary describes practical ways in which clinicians and laboratory personnel can work together to either avoid or, when unavoidable, better manage problems and delays. The responsibilities of genetic counselors working in molecular diagnostics are discussed.
Similar content being viewed by others
Main
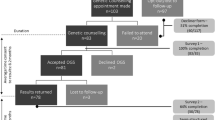
Physicians and other health care providers are finding molecular diagnostics to be a useful part of their practice, and the number of genetic tests available continues to grow at a rapid pace. Although there are similarities between genetic testing and other diagnostic tests, occasional issues arise in molecular diagnostics that suggest that clinical professionals and their patients may benefit from an ongoing dialogue with the laboratory personnel. The purpose of this article is to describe the roles and responsibilities of genetic counselors (GC) who work in molecular diagnostics laboratories, and to provide recommendations to health care professionals who wish to improve the experience they and their patients have when they order DNA-based testing. Molecular diagnostics comes with its own set of issues including labor-intensive methods; test sensitivity that often depends on factors such as patient ethnicity, family history, and clinical presentation; time constraints due to pregnancy or scheduled surgery; and unanticipated complexities related to the fickle nature of biology or lack of available knowledge. Laboratories doing clinical testing are regulated by the Centers for Medicare & Medicaid Services through the Clinical Laboratory Improvement Amendments (CLIA), and have specific requirements governing the training and certification of their directors.1 To assist clinical professionals, many molecular diagnostic laboratories employ masters-level trained GCs. In the preanalytic stage, even before a sample is sent, the laboratory GC is available to discuss specific testing strategies, assist in pedigree assessment, discuss the benefits and limitations of genetic testing for a patient, describe the experience the laboratory has with that test, and discuss ethical and other considerations with the clinical professional. Once a sample is sent, the laboratory GC may become involved in a case in a number of ways. Responsibilities that may be under the purview of a laboratory GC include ensuring that the proper test is ordered, communicating with the laboratory to prioritize samples of an urgent clinical nature, and providing updates of the test status to the referring health care professional. Once the laboratory has completed its analysis, in the postanalytic stage, a GC may request a repeat of the analysis if the clinical information is inconsistent with the molecular results. In addition, the laboratory GC will often assist the ordering physician with interpreting the test results in the clinical context of his/her patient, make recommendations for follow-up testing, and mention potential research opportunities. Although many of these job responsibilities are shared by a number of masters- and doctoral-level members of the laboratory team, GCs are frequently involved in these steps of the process and are often one of the primary contacts for the laboratory.
Although the goal of providing high quality results to the patient is shared, the laboratory GC and the clinician are each faced with different challenges. Even before a patient is seen for care, communication between the laboratory and clinician is recommended for cases with unusual circumstances and for tests with which the clinician is unfamiliar. The primary purpose of this communication is to establish an understanding of what can be expected of both the clinician and the laboratory. Specifically, the clinician may want to know the sensitivity of the testing, limitations of the test, the laboratory's methods and detection rate, and the estimated turnaround time (TAT). The laboratory will want to discuss the preferred specimen type, an appropriate testing strategy given the available medical information, the potential limitations of the analysis given the clinical context, and the family members from whom samples would be most helpful for interpretation. In some cases, laboratories will not perform a test for a variety of reasons including lack of required samples, failure to include informed consent, or incomplete billing information or paperwork. When the laboratory and clinician are able to discuss and agree upon the expectations of a case, the patient is the ultimate beneficiary of this partnership. Although some complications in the laboratory cannot be anticipated, some problems may be averted by discussing the case with the laboratory beforehand. Additionally, patients and referring clinicians can be made aware of possible delays. This article presents real cases from laboratory-based GCs to illustrate some of the issues that arise due to occasional technical difficulties and the inherent limitations of molecular testing. In our summary, we describe practical ways in which health care providers and laboratory GCs can work together to either avoid, or better manage, problems and delays. The responsibilities of the genetics professional, particularly the laboratory GC, working in molecular diagnostics are discussed.
CASE HISTORIES
Case 1: Results that are inconsistent with clinical phenotype—A polymorphism may lead to incorrect results
A chorionic villus sample (CVS) specimen was received in a molecular genetics laboratory with an order for cystic fibrosis (CF) genetic testing. The accompanying paperwork indicated that both parents were carriers of the common delta F508 mutation in the CFTR gene, but the laboratory reports were not included. Analysis of the prenatal specimen revealed apparent homozygosity for the mutant delta F508 allele. However, a second peak, at a height consistent with normal background “noise,” was also observed and initially interpreted as negligible. The results were consistent with a homozygous affected fetus (Fig. 1). However, a review of the parental results indicated that the unaffected mother also appeared homozygous for the delta F508 mutation on her previous carrier test (data not shown). Because she does not have CF, the most likely interpretation of this is that she is a heterozygous carrier for the delta F508 mutation and a technical issue caused a failure to detect the normal allele. This result requires further studies to determine the actual genotype of the patient. In the first laboratory report, sequencing of the primer-binding site of the gene was recommended to evaluate for a polymorphism. However, this was not ordered by the referring practitioner. Because the fetus seemed to be homozygous and affected, and there was suspicion that it may have instead been an unaffected carrier, the laboratory strongly recommended sequence analysis of the primer-binding site for both the maternal and the fetal samples. This information as well as the laboratory's suspicion that the fetus was unaffected was conveyed by the laboratory GC to the patient's GC. This allowed the patient to have a measure of calm during the extended testing period. Analysis of the prenatal and the maternal samples did reveal the presence of a heterozygous polymorphism at the primer site. Through this additional testing, a normal allele was observed in both the mother and fetus, correctly identifying the fetus as an unaffected heterozygous delta F508 carrier (Fig. 2).
The methodology used, called allele-specific amplification, uses primers specific to each mutation being tested. When a specimen is heterozygous for a mutation (or a compound heterozygous for two mutations), two peaks are seen. Homozygosity for the wild type allele or a specific mutation reveals only one peak. The results shown here demonstrate one peak for the delta F508 mutation in a CVS (chorionic villus sample) specimen, which is consistent with the fetus being affected with cystic fibrosis (CF). Because the unaffected mother of this fetus also had a similar, seemingly affected, genotype the possibility that a normal allele failed to amplify was raised. This was proven by sequencing the primer-binding sites of the mother and fetus, which revealed a polymorphism that prevented amplification of the wild type allele.
Case 2: Technical complications may arise from not sending the preferred sample type
A fragile X (FX) premutation carrier had a CVS procedure for prenatal diagnosis of FX syndrome. A cultured CVS specimen was submitted to the molecular diagnostics laboratory after chromosome analysis, and the fetal karyotype was reported to be normal female (46,XX).
Two phenomena are associated with an FX phenotype: triplet repeat expansion and methylation of the polymorphic CGG region of the FMR1 gene. As a first step, polymerase chain reaction and Southern blot analyses were performed on DNA extracted from the cultured cells to determine the size of the CGG triplet repeat region in the FMR1 gene of the at-risk fetus. Polymerase chain reaction analysis revealed one allele that was clearly in the normal range. A second allele was not observed in the female fetus, and Southern blot analysis resulted in an incomplete digest, a technical problem that required a second run of the test. In addition, studies to determine the methylation status of the gene were necessary to predict the phenotype; however, methylation studies are not reliable on CVS cultures. Because the specimen received by the laboratory was not adequate to perform the tests that were ordered, a second invasive prenatal procedure (i.e., amniocentesis) was required to obtain a final prenatal result.2
After being repeated, Southern blot analysis on the cultured villi showed that the fetus inherited the maternal expanded allele. Final results, including the methylation studies on an amniotic fluid specimen, diagnosed the presence of a methylated expansion within the full mutation range, predicting that the female fetus was affected with FX.
Case 3: Challenges in custom analysis—Importance of a positive control
A mutation in a gene associated with an adult-onset condition was identified in a CLIA-certified laboratory. For economic reasons, the clinician elected to use a second laboratory for presymptomatic testing of family members. The second laboratory designed a custom test to detect the family's point mutation, and specimens were sent from two asymptomatic relatives of the affected proband for testing. At the time, the laboratory GC recommended to the referring GC that a positive control from the proband be sent; however, there was a cost associated with that analysis. Based on this a positive control sample was not sent. Sequence analysis was performed, and both samples were homozygous for the normal (wild type) sequence at the position of the mutation. A written report was issued including a disclaimer that mentioned that the analysis relied on the accuracy of the information provided by the first laboratory.
Two months later, a sample was sent from another family member. Clinical information was provided stating that the previous two family members were asymptomatic (which was consistent with the molecular result), and that this patient was experiencing what might be early symptoms of the disorder. Laboratory analysis using sequencing proceeded, and the results were negative for the mutation. The laboratory questioned this result, because it seemed to be inconsistent with the clinical history. The testing was repeated. Results were again negative. The laboratory looked further into the published literature about this gene and it was discovered that the nomenclature used in the publication differed from the nomenclature on which they had based their custom test. On discovering this, the second laboratory had to consider the possibility that the mutation identified by the first laboratory used different nomenclature and that they were not looking in the correct region of the gene to identify the mutation.
After retesting all three patients, using new primers based on the published report of the mutation, the final results showed that the first two individuals were indeed negative for the familial mutation and the third patient (the one with early symptoms) was positive for the mutation. (The laboratory has since changed its policy and requires a positive control specimen, which is analyzed for internal control purposes at no cost to the patient and with no formal report issued.)
Case 4: Indeterminate results—Understanding results of unknown significance
A sample was sent to a diagnostic laboratory for predictive DNA-based testing because of an extensive family history of cancer. Using sequence analysis to evaluate the coding region and intron–exon boundaries of a cancer predisposition gene, the laboratory observed heterozygosity at a position in the gene that causes an amino acid change in the coding region. However, the criteria for calling the change a mutation were not met.3 Without functional studies, the contribution of this variant to the relative risk of cancer could not be established; therefore, the laboratory interpreted this finding as having unknown clinical significance. Testing an affected individual was recommended, but was not an option because the affected family members were deceased.
In cases with variants of unknown significance, the DNA results yield no additional useful information, thereby requiring all medical decisions (surveillance and prophylactic surgeries, etc.) to be based on the patient's personal and family history of cancer. The genetic laboratory's staff may be able to further explain the uncertainty of what the substitution means, in addition to providing some information regarding follow-up for the patient (e.g., further studies in the diagnostic laboratory or referral to a research study). When a patient has been tested without a previous genetics consultation, a recommendation for such a consultation can be made to the clinician.
DISCUSSION
GCs working in molecular diagnostics laboratories serve as liaisons between health care providers and the laboratories in which they work. In one publication, clinical GCs said that they had contacted a member of the molecular laboratory staff in advance of sending a sample 58% of the time.4 When contacting the laboratory, over 94% of the time the clinician asked for information regarding cost, TAT, and specimen requirements.4 Although these are important things to know when ordering DNA testing, the purpose of this article is to describe a number of other ways that the laboratory staff can be helpful to health care professionals who wish to order a genetic test. We feel strongly that the job description of the laboratory GC includes not only serving as a resource to the referring clinician, but also advocating for them and their patients within the lab. This can be done before, during, and after testing is ordered by the health care provider. In fact, beginning the communication process with the laboratory before offering testing to a patient allows the laboratory and clinician (and, consequently, the patient) to establish a realistic plan and reasonable expectations of the case (Table 1). Although in most cases a patient's sample will go through the laboratory process without any issues, good communication becomes imperative in the occasional cases where complications arise.
Before a patient is seen, a GC working in a diagnostic laboratory is typically available to discuss the medical literature as well as the laboratory's own experience with a gene, the sensitivity of testing and the methodologies used by the laboratory. This can be particularly helpful when the clinician has questions regarding the clinical utility or appropriateness of a test given a particular patient's medical and family history. The laboratory GC can provide advice on appropriate testing strategies, and the possible limitations of testing given the specific circumstances. In some cases recommendations to send the testing to another laboratory may be made if it is in the patient's best interest. This pretest discussion helps the health care provider and laboratory to establish expectations of the testing, which in turn allows the clinician to prepare the patient for the possible outcomes of testing.
Following receipt of a specimen by the laboratory, the health care professional may communicate clinical information or special instructions to the scientists and technicians in the laboratory through the laboratory GC. The communication process works the other way as well, as there are a number of reasons why the laboratory may need to communicate with the clinician. These reasons include updates on the status of testing if it may be delayed; the need for an additional or different type of sample on the patient or a family member; and requesting family or medical history, incidence of consanguinity, ethnicity, or other information.
RECOMMENDATIONS TO THE CLINICAL PROFESSIONAL FOR HOW TO IMPROVE THE EXPERIENCE OF EACH CASE SCENARIO
Provide all requested information, the correct specimen type and samples from all individuals required by the laboratory
Many laboratories will not perform testing if they receive the wrong specimen type, incomplete paperwork, or if they do not have samples from all of the individuals they require. Laboratories differ on this, however, so it is essential to find out the specific requirements of the laboratory you plan to use for a specific test. As seen in Case 1, even if a laboratory will accept a prenatal specimen for DNA testing without the parental results, this can lead to difficulty in interpreting laboratory findings and may even cause an incorrect result to be reported. Much of laboratory work, even in diagnostics, has some degree of subjectivity. In Case 1, the fetus may have been considered affected with CF without the parental information. It is an unfortunate fact that, even with the best information, laboratories do make mistakes.5 In Case 3, submitting the positive control with the first two family samples would have shown a problem with the laboratory's nomenclature before any results were reported.
For the above reasons, some laboratories require that the relevant familial samples be submitted for any prenatal diagnostic test, along with maternal blood to rule out maternal cell contamination. Other laboratories recommend that such samples be submitted but do not make it a requirement. The American College of Medical Genetics published guidelines (section G19.3) recommend that the parental mutation analyses and the maternal cell contamination testing be performed in the same laboratory for the highest accuracy.1 If a sample is sent without all of the requested samples or information, a disclaimer may be included in the report that casts some uncertainty on the results. Ideally, any anticipated limitations of a test would be discussed with the patient before the decision is made to undergo testing, supporting our recommendation for the health care professional to contact the laboratory as one of the early steps in preparing for a case (Tables 1 and 2).
Whenever possible, follow through on the recommendations made by the laboratory in the report
As evidenced in Cases 1, 2, and 4, even when the analysis ordered on the patient is complete, further testing may be recommended by the laboratory. Following these recommendations may be critical to obtaining the most accurate interpretation of the laboratory's findings, and these recommendations are generally made to optimize the usefulness of the results. In Case 1, CFTR gene sequencing was recommended on the maternal report before the prenatal specimen was received. This testing was ordered only after the routine prenatal test was complete and the fetus had an apparent affected genotype. Without the same laboratory having the mother's data showing that her normal allele was undetectable with their methods, the abnormal prenatal result might not have been questioned, thereby creating a devastating false positive result for the patient. Ultimately, accuracy was not compromised; however, had the laboratory's recommendations been followed when the mother's initial report was issued, the analysis would have been completed in less time and not under the duress of a pregnancy in progress. In Case 2, a second invasive prenatal procedure, which also delayed the results, was required because a complete FX result was not possible on the original specimen. In Case 4, the recommendation to test an affected family member was made, but was not possible. Following these recommendations may provide one or more missing pieces of information to complete the understanding of the patient's results. It should be understood that, although it is not always avoidable, not following the recommendations may limit the health care professional's and the laboratory's ability to interpret the results of the testing. All of this can be discussed with a GC working at the diagnostics laboratory.
Discuss realistic TAT with the patient
The TAT quoted by a laboratory is the best estimate for how long it will take to complete the average test. However, even when a request is made to prioritize a sample, one cannot guarantee the results in a specified time frame because of a number of variables. There are many reasons for delays, such as assay failures that necessitate repeating the analysis, inadequate DNA from the original specimen, and unanticipated follow-up tests that the laboratory must perform to complete a particular case. Cases 1, 2, and 3 each demonstrate different reasons for delays. The extended TAT in Case 1 was caused by the need to perform follow-up sequence analysis, which was not part of the original test, to evaluate for a polymorphism in the CF gene. In Case 2, not only did the test need to be repeated, but working with a suboptimal specimen type required a second procedure and specimen. In Case 3, the nomenclature error necessitated not only repeating the analysis, but redesigning the tests, which created delays. To fulfill the order, laboratories will redesign tests to obtain results for cases with problems. The laboratory may also elect to repeat analyses that seem inconsistent with clinical information (Cases 1 and 3) or when there is the possibility of an internal laboratory error. This takes additional time, making the TAT longer than anticipated and delaying the final results. Because laboratories want to provide a good service, consistent communication between the laboratory GC and health care professional provides the clinician with a glimpse of what is happening in the laboratory so that they can use this information to explain to their patient why the results are taking longer than expected without compromising the patient's trust in the final results.
Consider using the same laboratory for family members
Both Cases 1 and 3 demonstrate why it is preferable to use the same laboratory for familial testing. Recognizing that this is not always possible due to insurance constraints or laboratories that do not offer the service you want to order (e.g., mutation-specific analysis, prenatal diagnosis), patients should be counseled accordingly. As Case 3 illustrates, mutation nomenclature is not standardized and laboratories may use different reference sequences and numbering conventions to describe a mutation.6 In this example, the previous laboratory had used numbering for the mature protein, whereas the second laboratory began counting from the ATG initiation codon. This misunderstanding resulted in the second laboratory evaluating the wrong part of the gene for its analysis. Had the family members been tested by the same laboratory as the proband, no confusion regarding the nomenclature would have occurred. Methodologies used to test for specific mutations vary between laboratories and, while rare, a mutation detected on one testing platform may be missed on another (as in Cases 1 and 3). Although it may be necessary to use a different laboratory for family members of a proband, the inconsistency in nomenclature and variability in the testing conditions due to many laboratories using “home brews” for their tests can introduce laboratory errors. The laboratory and health care professional can work together to discuss the ideal process for reducing these errors.
Be aware of, and discuss with patients, the realistic possibility of inconclusive results
When sequence analysis is used to identify mutations, there is always a chance that a novel or unfamiliar genetic variant will be identified. In instances such as Case 4, there is not enough evidence to definitively interpret the change as a pathogenic mutation, and the clinical implications are unknown. These cases are further complicated when there is no phenotype in the patient (i.e., predictive testing or prenatal diagnosis) to suggest an association with disease. These are frustrating cases for the laboratory, health care providers, and patients alike. In Case 4, it has not yet been established whether the variant increases cancer risk for the patient, and the laboratory GC was able to share her knowledge of the gene and its possible association with cancer with the clinical counselor. Although inconclusive results may not provide the desired information, the increasing utility of sequence analysis means that many health care providers will have to explain this type of finding to their patients at one time or another. For this reason, it is critical for the informed consent process to address the possibility of identifying a variant of unknown clinical significance with certain methods. Although genetic tests are ordered with the hope that results of genetic testing will provide useful information to the patient, this is not always the case at this point in time. Addressing the limitations of molecular testing up front can help to allay patients concerns later on, particularly if there is a complex or indeterminate result. Following-up the laboratory's recommendations for further testing or testing of family members may help with interpreting such results and this is an issue that can be discussed with a laboratory GC or geneticist.
Laboratories trust the clinical expertise of the referring professional
Although most laboratories have guidelines and sometimes strict requirements under which they will accept certain specimens, when it comes to deciding if a test is appropriate for a patient, the staff at the diagnostic laboratory will usually rely on the decision of the referring clinician. The unique relationship and the in-depth discussion that takes place between the health care providers and their patients enables the clinician to be the best judge of whether a test is appropriate for a given patient or not. This applies to many situations, from predictive testing on minors7 to prenatal diagnosis for an adult-onset condition. As part of obtaining informed consent for testing, the patient should be made aware of the limitations of the test being ordered, and the implications of a positive or negative result under a given set of circumstances. In cases such as these, genetics professionals at the laboratory can be of great assistance and may be able to provide guidance concerning the utility, benefits, and limitations of a test. The laboratory relies on the referring clinical professional to provide full and accurate information to the patient and to review the advantages and disadvantages of the testing. Although some laboratories have policies where they reject samples for particular reasons or they do not offer a particular service (e.g., prenatal diagnosis), whenever it is technically possible, most laboratories want to provide the service the clinical professional has requested. This is done with the implicit understanding that the clinical professional knows what is appropriate for their patient. The appropriateness of testing, ultimately, is sometimes a difficult decision that is borne from extensive discussions between the patient and his/her clinician. Thoughtful guidelines for genetic testing are provided by professional societies and patient advocacy organizations.8–10 As with clinical genetics professionals, those of us who are in the laboratory are also guided by our training, professional codes of ethics, and our own personal experiences in the field.
SUMMARY
Imparting information to patients is one of the most significant aspects of the genetic counseling process. Discussing genetic testing with a patient or family entails being comfortable with the risks, benefits, and limitations of that test in the clinical context of the patient's phenotype, ethnicity, or family history. The authors encourage health care professionals to use the genetics professionals employed by molecular diagnostics laboratories as resources when they are obtaining background information before offering testing to a patient. This will help the clinician relay information about important factors such as test sensitivity, TAT, specimen requirements, etc., to the patient, thereby establishing realistic expectations for the person being tested. In addition, we encourage clinical professionals to communicate phenotype data to the laboratory once a sample has been sent. By doing so, the laboratory will have a clinical context in which to interpret their findings, the importance of which was illustrated by the cases described in this article. Finally, even after the results of the laboratory's analyses have been reported, there may be reasons for ongoing communication between the clinical and laboratory professionals. Perhaps family members will want to discuss testing, or the laboratory may have recommendations for follow-up, or new data may shed light on an unclear variant. In sharing some of our experiences and making recommendations through this commentary, we hope that readers learn from our experiences from within the “black box” of molecular diagnostics and will consider how using the personnel at DNA laboratories can help us all provide excellent and comprehensive clinical genetics services to individuals and their families.
References
American College of Medical Genetics (ACMG). Standards and Guidelines for Clinical Genetics Laboratories, 2005 ed. [online]. Copyright, 2001–2005. Available at: www.acmg.net. Accessed October 28, 2005.
Maddalena A, Richards CS, McGinniss MJ, Brothman A, et al. Technical standards and guidelines for fragile X: the first of a series of disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics. Quality Assurance Subcommittee of the Laboratory Practice Committee. Genet Med 2001; 3: 200–205.
ACMG Laboratory Practice Committee Working Group. ACMG recommendations for standards for interpretation of sequence variations. Genet Med 2000; 2: 302–303.
McGovern MM, Benach M, Zinberg R . Interaction of Genetic Counselors with Molecular genetic testing laboratories. Am J Med Genet 2003; 119A: 297–301.
Bonini P, Plebani M, Ceriotti F, Rubboli F . Errors in laboratory medicine. Clin Chem 2002; 48: 691–698.
Den Dunnen JY, Antonarakis E . Nomenclature for the description of human sequence variations. Hum Genet 2001; 109: 121–124.
ACMG Policy Statement. Genetic Testing in Children and Adolescents, Points to Consider: Ethical Legal and Psychosocial Implications of (ACMG/ASHG). Am J Hum Genet 1995; 57: 1233–1241.
National Society of Genetic Counselors Position Statements Web Page, 1995–2005. Available at: http://www.nsgc.org/about/position.asp. Accessed April 22, 2005.
American College of Medical Genetics Policy Statements and Practice Guidelines Web Page, 2001–2005. Available at: http://www.acmg.net/resources/policy-list.asp. Accessed April 22, 2005.
IHA (International Huntington Association) the World Federation of Neurology (WFN) Research Group Huntington's Chorea Guidelines for the molecular genetics predictive test in Huntington's disease. Neurology 1994; 44: 1533–1536.
Acknowledgements
The authors acknowledge the contributions of Karen Giger, Erin O'Rourke, and Cynthia Frye.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Scacheri, C., Redman, J., Pike-Buchanan, L. et al. Molecular testing: improving patient care through partnering with laboratory genetic counselors. Genet Med 10, 337–342 (2008). https://doi.org/10.1097/GIM.0b013e31817283a5
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31817283a5