Abstract
Purpose: We assessed the effectiveness of educational interventions for conveying clinical findings and information about hereditary hemochromatosis (HH) and iron overload (IO) to individuals evaluated clinically after initial screening for HH/IO with serum ferritin (SF) concentration, transferrin saturation (TS), and HFE genotyping.
Methods: A questionnaire mailed to 2300 cases and controls 1 month after a letter summarizing clinical findings measured understanding of results and recommendations, knowledge of HH/IO, and satisfaction with information received.
Results: Of 1622 (70.5%) participants completing relevant items, 83.6% were satisfied with receiving initial screening results by mail, 93.4% found information clear and easy to understand, 89.2% generally felt they got enough information, but 47.5% still had questions. C282Y/C282Y homozygosity with normal TS/SF predicted the best understanding of genetic results. Many with no mutations thought relatives were at risk. Iron levels created most confusion, and a third incorrectly recalled treatment recommendations. Having any abnormal result, lower education, older age, and being non-white, and/or non-English speaking predicted lower understanding.
Conclusions: Combining genotypic and phenotypic screening for HH/IO creates additional difficulties in communicating results—particularly to those with low health literacy. Explaining aberrant iron TS and SF levels and low-risk genotypes, follow-up recommendations, and risk to relatives will need creative, culturally appropriate strategies.
Similar content being viewed by others
Main
Hereditary hemochromatosis (HH) is a common disorder that causes some affected individuals to develop iron overload (IO) because of increased intestinal absorption of iron. This may lead to serious complications including hepatic cirrhosis, liver cancer, diabetes mellitus, cardiomyopathy, arthropathy, endocrinopathy, and a shortened lifespan.1,2 Early detection can prevent development of IO in susceptible individuals, and therapeutic phlebotomy can reverse both the IO and some of its complications in those already symptomatic.3 Because of these effective interventions and the fact that HH occurs in 0.3–0.5% of whites of Western European descent, it is a candidate for population-based screening.4
The success of such a screening program depends not only on correctly identifying those who are at risk, but also on ensuring that those who screen positive receive additional diagnostic assessment, understand the potential manifestations of the condition, learn how symptoms can be prevented or treated, and notify others in their family who could be at risk. Because misunderstandings may diminish the benefits of screening, it is important to determine the efficacy of patient education and to see if it is affected by factors such as ethnicity, preferred language, educational level, age, gender, test results, and presence or absence of disease symptoms. Identifying specific gaps in understanding and other factors that may impede risk-reducing behaviors will help to inform future screening strategies for not only HH and IO disorders, but also other variably expressed diseases for which population-based screening may become feasible.
Education and counseling for HH screening presents a number of challenges. Among these are that: (1) most people are unfamiliar with HH5; (2) only about half of those found to carry relevant HFE mutations will ever develop clinical symptoms6; (3) familial IO is genetically heterogeneous (and hence may not be detected or explained by HFE genotyping); and (4) screening by measuring transferrin saturation (TS) and serum ferritin (SF) identifies not only people with HH, but also many who have elevated (or diminished) iron levels for other reasons.7 HH/IO screening can thus identify unsuspected existing health problems that may be less treatable than those associated with HH, create anxiety about symptoms that may or may not develop in the future, and reveal that family members may be at risk.
This report describes our experience in providing screening and results education to a diverse group (44.2% white, 27.2% black, 12.8% Asian, 12.5% Hispanic, and 3.3% of other, multiple, or unknown ethnicities) who were screened for HH/IO in primary care settings as part of the Hemochromatosis and Iron Overload Screening (HEIRS) Study.8 Education about HH/IO, screening, and results occurred at several points using written materials including personalized letters and—for certain screen-positive individuals—face-to-face counseling at the time of a clinical examination (CE). In this report, we present data about subjects' understanding of results and recommendations following the CE, knowledge about HH/IO, and perceptions of the adequacy of information they received. Additional factors that affected these outcomes, including test results and demographic variables, are discussed.
MATERIALS AND METHODS
Setting
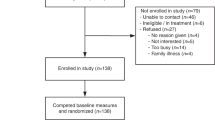
The HEIRS Study is a large observational study designed to evaluate the prevalence, risk factors, and potential clinical, personal, and societal impact of HH and IO. A multiethnic sample of 101,168 adults, aged 25 years and older, from five field centers (FCs) in North America were recruited through primary care clinics, clinical laboratories, and health plans. Details of the study design, laboratory testing, data management, and analysis have been described elsewhere.9 The study was approved by the institutional review board at each FC, the central laboratory and the coordinating center. Figure 1 illustrates study elements and hierarchy.
Recruitment and study groups
Potential study subjects who appeared to be at least 25 years of age were recruited from waiting areas of participating HEIRS clinical sites (or by mail at one site). Recruiters described the HEIRS study and obtained signed informed consent from those who expressed interest in participating. Materials were made available in English at all FCs, and also in Spanish (Howard University and UC Irvine), Vietnamese (UC Irvine and London, Ontario), or Mandarin (London, Ontario) by recruiters fluent in these languages. Participants then completed a questionnaire and had their blood drawn. Each of the 101,168 participants was screened by measuring SF and TS, and by genotyping for the normal, C282Y and H63D HFE alleles. Subjects were considered “screen positive” (and hence eligible for a CE) if their genotype was C282Y/C282Y or if their TS and SF values exceeded study thresholds for elevated iron: TS > 50% and SF > 300 μg/L for men; TS > 45% and SF > 200 μg/L for women.9 CE-eligible subjects were mailed their screening results along with an explanatory letter tailored to these results, and were then invited by telephone to participate in the CE. Those who accepted became “CE cases.” Another 642 subjects who carried neither HFE mutation and had normal TS and SF were also seen for CE. These “CE controls” were randomly selected but age-matched to CE cases at each FC. Of 2265 participants invited for CE, 1687 (74.5%) accepted. CE participants with confirmed elevations in TS and SF who had received <10 units of blood transfusion were considered for documentation of primary IO, performed outside the Study. Normal iron stores in adults are approximately 1 g.3 Primary IO was defined by removal of >2000 mg of body storage iron by phlebotomy or by an iron concentration of >30 μmol/g dry weight on liver biopsy.9
Patient education and genetic counseling
Prescreening education
Participants received information about HH/IO and their specific findings at several points in the study. At the time of initial recruitment, general information about HH and IO was outlined as part of the informed consent process. Printed materials described some of the health conditions related to IO (liver damage, liver cancer, heart disease, arthritis, diabetes, sexual impotence), the hereditary nature of the disorder, the increased risk of health problems for those possessing two HFE mutations, and the 1/250 prevalence of HH in whites. Materials emphasized the variable expression of HH due to HFE and indicated that the prevalence and role of genes predisposing to IO in other racial/ethnic groups was less well understood. Recruitment materials and screening results letters were provided in the subject's preferred language (English, Spanish, Vietnamese, or Mandarin) and study staff fluent in the relevant language usually did the recruiting at sites with large numbers of non–English-speaking patients. Bilingual staff members were also available by telephone and attended the CE as needed.
Notification about initial screening results
Most CE-eligible subjects were given their genotype and iron level results by telephone and invited to participate in the CE. Those who accepted were sent a letter appropriate to their specific screening results that contained the comment: “The results of your tests show that you may have iron overload or have a tendency to develop iron overload in the future,” their lab results sheet, and an IO pamphlet. The pamphlet outlined the nature, causes, and effects of IO, and briefly discussed monitoring and treatment options, including dietary recommendations such as avoiding alcohol, iron preparations, and Vitamin C.
CE and counseling
At the CE, all but control participants were given genetic counseling, or at least results-specific information about HH/IO by a genetic counselor, nurse, physician, or study coordinator. Staff varied in how they used a standardized counseling outline developed for the study. All FCs provided genetic counseling to C282Y homozygotes and those with other mutant genotypes conferring a lower risk for IO. H63D carriers usually got more circumscribed counseling. Only general information was given to controls. Some FCs also provided an educational brochure and other sites sent additional information on request or referred participants to relevant websites. Limited information could be provided about the significance of initial screening iron elevations (if any) because these were being investigated by further testing at the CE. Unless the counselor was fluent in the relevant language, an interpreter was used in counseling non–English-speaking participants.
Content of the sessions varied somewhat depending on the participant's situation, but always included discussion of screening test results and their possible implications. All “genotype positive” subjects (i.e., those with any HFE mutation—except, at some centers, H63D carriers) were given information about HH inheritance and the chances that their siblings, parents, and offspring would have specific genotypes. An estimate of the likelihood that each of these genotypes would lead to IO usually was provided. Most participants with a high chance of IO were given information about symptoms and clinical recommendations for prevention and treatment. The counselor assessed understanding and explored psychosocial issues, such as feelings about test results and notifying family members. Participants were also told what to expect for the remainder of the study (e.g., clinical results letter, follow-up questionnaires).
CE summary letter
After results from the CE blood work were available, a clinician at each FC wrote the participant a letter summarizing the evaluation. These letters were not standardized, but a uniform coding sheet was used by each FC to record their key contents. Messages relevant to the current study are described in Table 1. (Some letters contained more than one comment, so the sum of percentages in each category exceeds 100.) One week after the summary letter was sent each CE participant was mailed the survey described below. A follow-up mailing was sent to nonresponders approximately 1 month later. Some FCs with lower response rates also contacted nonresponders by phone or in person, or offered incentives for completion. This report focuses on the 1622 CE participants, including 464 controls, who completed relevant items on the survey (70.5%). Almost all CE summary letters included a laboratory report with TS and SF values, their reference ranges, and the HFE genotype (which also was included with screening results). The terms “heterozygote” and “homozygote” were explained as appropriate when one or more C282Y or H63D mutation(s) were reported.
Measures
Outcome measures
Table 2 describes the outcome measures and analysis variables that were created based on survey items. The following sections summarize these measures and variables.
Satisfaction with screening results notification.
The mailed survey asked subjects if they had been given screening results by phone or letter and asked: “How do you feel about the way you were FIRST notified about your results?” For analysis, response options were dichotomized.
Satisfaction with amount and quality of information provided by the study.
To determine level of satisfaction with what they were told, participants were presented with three statements related to information they received during the HEIRS study and asked to indicate their level of agreement in four increments from “strongly agree” to “strongly disagree.” Items sought their opinion on the clarity, understandability, and amount of information, and asked if they still had questions about HH/IO or their test results.
Accuracy in understanding test results.
Subjects' understanding of their genotype and IO status was measured by “yes,” “no,” or “not sure” responses to a series of four statements such as “I do not have any known hemochromatosis gene variations (mutations),” or “I do have iron overload.”
Genotype: To assess understanding of genetic test results, subjects were asked to respond to three mutually exclusive statements about the number of HFE mutations they were found to carry.
Familial implications of genotype: Response to the statement “I have hemochromatosis gene variations (mutations) that may also be present in members of my family” assessed whether subjects recognized the implications (if any) of their genotype for family members.
IO status: Subjects were asked to respond (“yes,” “no,” or “unsure”) to the statement: “I do have iron overload.”
Accuracy in understanding management recommendations.
Responses to four statements assessed subjects' understanding of recommendations that were made based on clinical and laboratory findings. Subjects were to indicate (by “yes,” “no,” or “not sure”) if they thought they had been told to: (1) “talk to personal physician,” (2) “have personal physician test the amount of iron in their blood about once a year to make sure it is not too high,” (3) “have blood drawn to lower the amount of iron,” and (4) “talk to family members about their possible risk for HH or iron overload.”
Recall of screening results and recommendations.
An overall score for understanding results and recommendations was generated by summing scores from the four questions about genetic test results and the four on recommendations.
Knowledge about HH and IO.
A global knowledge score was derived from 25 questions that tested knowledge about the symptoms, outcome, treatment, and genetics of HH/IO.
Modifying variables
Demographic and other baseline variables.
Data collected from the screening questionnaire and the informed consent document included date of birth, gender, race/ethnicity, and language preference. Educational attainment was ascertained on the post-CE survey and categorized as “high school diploma or less,” “some college,” or “bachelor's degree or more.”
Information sources accessed.
Participants were asked to indicate the degree to which they had used any of five sources to find information about HH or IO. These included: (1) a phone call or written material from the HEIRS study, (2) family members, (3) the library, (4) the Internet, or (5) their doctor or other health worker(s). A summary score (possible range of 0–10) was derived, with 0 points assigned when participants answered “none” to all five items, 1 point for each source that had been accessed “some,” and 2 points for each source used “a lot.” Participants had to answer at least one of the five items to have an “information seeking” score calculated.
Statistical analyses
For univariate analyses, the χ2 test for contingency tables was used to compare demographic characteristics (gender, race/ethnicity, preferred language, educational level, HFE genotype) and categorical outcome variables. Multivariate analyses were performed using either linear regression to predict the mean of a continuous outcome, or logistic regression to predict the probability of a binary outcome. All relevant predictor terms were used in an initial model that allowed for all possible two-way interactions. In subsequent models, nonsignificant terms were deleted. Model-based means for significant interactions effects were displayed graphically. No multiple comparisons methods were used. Statistical analyses were performed using SAS Statistical Software, version 8.02 (SAS Institute Inc., Cary, NC).
RESULTS
Respondents
Characteristics of CE subjects responding to the survey are shown in Table 3. There was some evidence of response bias with language preference, race/ethnicity, educational level, genotype, and age accounting for significant differences in the likelihood of returning the survey. Spanish speakers were less likely to respond (odds ratio, OR 0.30, 95% CI 0.20–0.44) and Vietnamese speakers more likely (OR 2.80, 1.88–4.16) than English speakers. Compared with non-Hispanic whites, African-Americans (OR 0.33, 0.15–0.42) and Hispanics (OR 0.26, 0.19–0.36) were the least likely to respond. Increased genetic risk and greater educational attainment were associated with a greater likelihood of survey response. C282Y/C282Y (OR 1.82, 1.35–2.45) and C282Y/H36D participants (OR 1.84, 1.08–3.12) were more apt to return the survey than wild-type individuals, and those with a high school degree (OR 1.49, 1.15–1.94), some college (OR 2.05, 1.57–2.45), a bachelor's (OR 2.07, 1.55–2.78) or postbaccalaureate education (OR 3.31, 2.34–4.67) responded more frequently than those who had not completed high school. Each year of increasing age was associated with a modest increase in the odds of survey participation (OR 1.04, 1.03–1.04). The likelihood of responding was not related to gender.
Satisfaction with screening results notification
Although CE-eligible participants were first called with their results, most (72.2%) remembered first receiving their screening results by letter. Of these, 83.6% were either “satisfied” or “very satisfied” with how they were notified. Satisfaction was higher among English speakers (84.6%) than non-English speakers (78.0%, P = 0.012), but was not significantly affected by whether they remembered being notified by mail or phone, or by age, genotype, educational attainment, or race/language. The nature of the screening results did, however, affect satisfaction, with more CE controls (88.4%) (normal genotype; no iron elevation) expressing greater satisfaction with how they were notified, and those with a normal genotype but elevated iron on initial screening (79.5%) less likely to report being satisfied (adjusted OR 0.53, 0.36–0.79, P = 0.009).
Satisfaction with amount and quality of information provided by the study
An additive model was fit with a specific set of covariates to identify ones associated with satisfaction with information provided during the study. Satisfaction was significantly related to age (P = 0.011), race/language (P = 0.023), iron status (P = 0.011), genotype (P < 0.0001), and how well recommendations were remembered (P = 0.018), but was not related to how much information the subject had accessed.
For the 1458 (89.9%) responding to these questions, the mean score was 9.0 (SD = 1.65) on a scale of 12, indicating a high degree of satisfaction with information provided. Nearly all (93.4%) said that they found the information they had received “clear and easy to understand,” and most (89.2%) said they had “received enough information,” but almost half (47.5%) said they still had questions. Modal scores did not differ by language preference (English versus non-English), but satisfaction differed by race/language group (P = 0.0001), with non–English-speaking Hispanics least satisfied (mean 8.48, SD 1.40), and English-speaking whites most satisfied (mean 9.19, SD 1.68). Controls differed from cases of all genotypes, including those with no mutations (mean 9.63, SD 1.70 vs. 8.69, SD 1.56; P < 0.0001). However, cases did not differ by genotype. Small but significant (P < 0.0001) differences in satisfaction with information were seen because of iron status. Participants who learned they had IO were the least satisfied (mean 8.44, SD 1.59), and those with no IO the most (mean 9.30, SD 1.65).
Accuracy in understanding test results
Genotype
Type III analysis of variance was used to identify predictors for understanding genotype information. These included genotype itself (P < 0.0001), IO status (P = 0.0002), age (P = 0.0002), race/language (P < 0.0001), educational level (P < 0.0001), and information seeking (P = 0.0055). Depending on genotype, between 41.4% (H63D/H63D homozygotes) and 77.9% (C282Y/C282Y homozygotes) of participants answered “yes” to the appropriate statement about carrying one, two, or no mutations. However, some of these subjects also incorrectly answered “yes,” did not respond, or answered “don't know” to one or both inappropriate statements. Only about 47% answered all three questions correctly (summary score 3), indicating that they fully understood their genotype. Another 24% had scores of 1 or 2, showing some understanding. The rest (29%) appeared to have no accurate recollection of their mutation status, scoring between −3 and 0.
Wild-type (+/+) controls had the highest mean score (mode 3, mean 2.23, SD 1.19), and differed from all other groups, with two thirds (67.3%) answering all three questions correctly, as did over 58% of C282Y homozygotes (mode 3, mean 1.93, SD 1.41). Interestingly, +/+ cases scored much lower on these questions (mode 1, mean 1.12, SD 1.42). H63D homozygotes were least likely to understand their genotype (mode 0, mean 0.43, SD 1.76), differing significantly (P < 0.0001) from all other groups. Nearly two thirds (64.9%) of H63D homozygotes scored ≤0 on the three questions regarding mutation status.
As suggested by the difference between +/+ cases and controls, genotype understanding was poorer when iron levels were elevated. Those without IO were more likely to correctly remember their genotype (mode 3, mean 1.92, SD 1.37) than those with IO (mode 2, mean 1.49, SD 1.58, P = 0.0016) or possible IO (mode 1, mean 1.20, SD 1.44, P = 0.0002). The latter two groups did not differ from each other.
Understanding was modestly affected by age (r = −0.10; P = 0.0002), with subjects who fully understood their genotype being somewhat younger than those with “no understanding” (mean 54.8 vs. 56.4 years; P = 0.024). Educational attainment was also an independent predictor. Those with a high school education or less recalled their genotype less well (mode 1, mean 1.08, SD 1.37) than those with some college (mode 3, mean 1.76, SD 1.45, P < 0.0001) or at least a bachelor's degree (mode 3, mean 2.06, SD 1.40, P < 0.0001). All three groups differed significantly from each other.
English-speaking whites were significantly more likely than all other race/language groups to correctly recall their genotype (mode 3, mean 2.03, SD 1.40), with English-speaking Asians (mode 2, mean 1.71, SD 1.47) also showing significantly better understanding than the four remaining groups. The latter groups did not differ significantly from each other, with modal scores of 0 or 1, means ranging from 0.45 to 1.33, and SDs from 1.10 to 1.53.
Familial implications of genotype
Over half (54.0%; N = 874) responded correctly to the statement “I have hemochromatosis gene variations (mutations) that may also be present in members of my family” (possible score range −1 to 1), but about a third (32.5%, N = 526) were unsure. Genotype significantly affected the responses (P < 0.0001). Controls were more often correct (mode 1, mean 0.75, SD 0.47), and C282Y carriers least often correct (mode 0, mean −0.19, SD 0.82).
IO status
Table 4 summarizes subjects' responses according to the messages they were given in their CE summary letters. The great majority (87.9%) who were told they had IO knew they had it. Fewer of those with normal iron levels (83.3%) recognized that they did not have IO. However, over a quarter of subjects with elevated iron levels who were told they did not have IO believed they did. When the CE letter contained a more ambiguous “message” (e.g., “you may have iron overload” or “your iron levels are elevated”) or no statement at all, 61.2% thought they had IO, 19.6% thought they did not, and 19.3% were unsure or did not answer the question.
Accuracy in understanding management recommendations
Table 5 indicates observed responses versus ones expected from recommendations in the CE summary letter. Multivariate analysis found that the accuracy of recall was affected by subjects' genotype (P < 0.0001), iron status (P < 0.0001), race/language (P < 0.0001), educational attainment (P < 0.0001), and information seeking (P = 0.023). Encouragingly, when a recommendation required action, at least two thirds of participants remembered it. This included either talking to family members about possible risk (92.7%) or telling them to be evaluated for HFE mutations or IO (82.8%), sharing results with their personal physician (79.1%), having their iron levels measured (70.0%), or having therapeutic phlebotomy (65.1%). On the other hand, when the CE letter did not contain a specific recommendation, many participants either thought they should do something or were unsure. Of particular concern were 573 respondents (44.2%) who erroneously believed or were unsure if they needed to have their physician monitor their blood iron levels and 368 (30.8%) who mistakenly thought or did not know if they needed phlebotomy. Only about half correctly recognized that they did not need to talk to their family members or to suggest that they be checked for HH/IO—meaning that at least 700 CE participants either believed or were unsure about whether their relatives were at risk.
Knowledge about hemochromatosis and IO
Of 25 questions asked about HH and IO, 9 (Table 6) were to determine whether subjects recognized health problems potentially associated with HH. Sixteen others (Table 7) assessed understanding of HH/IO causation, treatment, and inheritance. Each table presents these questions sorted (in descending order) by number of correct responses. There were more missing responses to questions about symptoms (range 6.0–12.5%) than to those about causation, treatment, and inheritance (2.8–4.5%). Questions with more “don't know” or incorrect responses also had a higher nonresponse rate. Of symptoms associated with HH/IO, fatigue was correctly recognized by nearly half, but impotence by only about a quarter. Almost two thirds were unsure or failed to recognize that HH/IO could cause diabetes. Several questions required respondents to correctly identify health problems not associated with HH/IO (i.e., asthma, prostate or ovarian cancer, multiple sclerosis, or painful menses), but only asthma was correctly recognized by over a quarter.
At least four fifths of CE participants knew that one could have HH without knowing (88.9%), that accumulation of iron causes problems (80.8%), and that it is important to treat HH before organ damage occurs (81.0%). Two thirds (66.4%) understood that siblings of an affected individual were also at risk. Slightly fewer (60.9%) knew that HH could be treated or that treatment involves phlebotomy (61.5%). Less than half (45.0%) believed that HH could be fatal. Interestingly, although over one third (37.8%) recognized that not everyone with gene variations would have “too much iron in the blood,” over half (52.3%) thought a gene test alone could find IO if it was already present. This last statement was the only one that had more incorrect than correct answers—resulting in a negative mean score (−0.33) on the item. Two questions with the highest proportions of “don't know” responses required recognizing that men usually get HH earlier than women do and that different HFE mutations confer different risks for IO.
Factors that significantly affected knowledge of HH/IO (P < 0.0001 for all comparisons) included genotype, with C282Y homozygotes scoring significantly higher than all other genotype groups (avg. score = 16.9, SD = 4.0) and 50% higher than controls (mean 9.5, SD 5.8). Greater knowledge was also related to language (English speaking, mean 12.0, SD = 5.8, vs. non-English speaking, mean 8.0, SD 4.2), age (R = −0.14) and information seeking (R = 0.22).
DISCUSSION
This portion of the HEIRS Study used data from a self-administered questionnaire completed by participants with abnormal screening results who came for further clinical evaluation (CE), and a CE control group. The survey assessed satisfaction with information received in the course of the study, knowledge of HH/IO, and understanding of test results and medical recommendations made after further evaluation. Insofar as there was a lower response rate from non–English-speaking groups that scored lower on some questions, results may not completely represent all CE participants.
Satisfaction with screening results notification
Those who screened positive were generally satisfied with getting their results by mail. However, it should be mentioned that potential CE subjects also got a telephone call asking them to participate in the clinic visit. This provided an opportunity for them to obtain additional information about their results from a staff member fluent in their preferred language. Even so, non-English speakers were significantly less satisfied with notification than English speakers. Interestingly, having elevated iron levels with a normal genotype predicted the least satisfaction with notification, suggesting that subjects may have perceived these results as incongruent, with resultant confusion or anxiety diminishing their satisfaction with notification.
Satisfaction with amount and quality of information provided by the study
Satisfaction with information—including that received during and after the CE—was lower when results were abnormal or the meaning unclear. Those with IO or a “low-risk” variant genotype were least satisfied. C282Y homozygotes found information more satisfactory—perhaps because they had more extensive counseling about risks and familial implications at the CE.
Accuracy in understanding test results
Genotype
Understanding of results and recommendations also was poorer with abnormal findings or ones with uncertain implications. Genotype recall was best among C282Y homozygotes and C282Y/H63D compound heterozygotes, whereas those with low-risk variant genotypes generally had poor recollection. An unexpected finding was that iron status was one of several factors predicting understanding of genotype, with subjects who had IO or iron elevations of unclear significance less likely to correctly remember their genotype—even if they carried no mutations.
Familial implications of genotype
When the CE summary letter indicated that the subject had a genetic change that could be present in relatives or that family members could be at risk, most responded correctly to the question about carrying a mutation that could be present in relatives. If there was no such statement, about half answered that family members were not at risk. C282Y and H63D carriers were least likely to be clear about whether their genetic status put other family members at risk, even though this issue was specifically addressed during counseling at the CE visit. Up to 97% who were advised to tell relatives about their status or to encourage them to be checked by a physician or to be seen by a genetic counselor remembered these recommendations, but over one third of those whose relatives probably were not at increased risk thought they needed to inform their relatives or to suggest that the relatives should be checked. These misunderstandings emphasize the complexity of understanding genotype, particularly when results are given for two variant alleles, and the importance of reassuring those with low-risk results.
IO status
To date, population-based screening for risk to develop symptoms of HH has focused mostly on C282Y homozygotes.5,10 Other programs have also screened for C282Y/H63D11 or H63D/H63D.12 Some have decided not to inform heterozygotes about their status13 or instead to tell +/+ individuals and C282Y carriers just that they were at “low risk to develop hemochromatosis” while inviting them to call if they wished to learn their actual genotype.5 Giving genotype information only to those at higher risk of IO is a strategy that may lessen confusion among low-risk carriers, but it reduces the chance to identify relatives with higher-risk genotypes through cascade screening.
A German program that tested only for C282Y reported that subjects misunderstood results (including implications for family members) regardless of mutation status, with wild-type individuals the most uncertain about the familial implications of their genotype.14 In this program, initial education about HH was provided via a leaflet introducing the study and an invitation to attend an information session. Few took advantage of the invitation. Test results were usually delivered and explained by the family doctor, with just a quarter of C282Y homozygotes discussing their findings with an internist or other specialist. About one in eight participants had not been given results by the time of the survey and over a quarter received them with no explanation. Only about 17% with a C282Y mutation (vs. <1% without mutations) took advantage of the proffered telephone consultation to discuss results. Many participants in this study also misunderstood results, with over one third (and 42% of C282Y homozygotes) believing that all homozygotes would develop symptoms if untreated and nearly 30% (including C282Y heterozygotes) thinking that carriers also had a high risk of developing HH. One in five carriers thought they had been clinically diagnosed with HH.14
Accuracy in understanding management recommendations
Over one fifth of participants (Table 1, 21.6%) were advised to have therapeutic phlebotomy. This was not surprising because 53% of the subjects who attended the CE had sustained elevations in iron levels. Importantly, nearly all CE participants who were clearly told that they had IO understood this message, and over 70% advised to have iron levels monitored remembered this recommendation. However, a quarter of subjects and controls that were told they did not have IO were unclear—both about whether they had IO and what they needed to do. Summary letters with qualified comments about iron status (e.g., “you don't have IO, but your iron levels are elevated”) caused confusion. A quarter who got such letters thought they did have IO, as did about two thirds of those who were told that they just had elevated iron levels or might have IO. Many were unsure if they needed follow-up for abnormal iron levels, with a third erroneously thinking they needed to have their blood monitored for iron elevation and nearly a quarter mistakenly believing they should have phlebotomy.
Lloyd et al.15 make the point that ambiguity—particularly in the context of genetic risk assessment—is psychologically aversive. This is consistent with observations from the HEIRS Study that subjects with indeterminate results were more likely to report diminished psychological and physical well-being and increased health worries.16 It appears that confusion or anxiety about iron status can spill over and adversely affect understanding of genotype, recollection of recommendations, and satisfaction with other information received in the course of screening. These findings emphasize how difficult it is to explain the meaning of elevated iron levels found through combined phenotypic and genotypic screening for HH—particularly when many with genotypes conferring increased risk will have normal iron levels and others with no mutations will have elevated iron.
Nearly half of our CE participants said that they still had questions—even after having an opportunity to discuss initial screening results with staff at the CE and receiving a personalized letter summarizing findings from this visit. This emphasizes the challenge of providing clear and conclusive information to people screened for a disease with incomplete penetrance and variable expression. Screening for thrombophilias has raised some of the same issues.17 Responding to a mailed survey, only one third of patients who had tested positive for the factor V Leiden mutation said that they felt confident in their understanding of the result, and over two thirds still had questions.18 Those seen by a hematologist or in a thrombophilia clinic were more likely to feel that their questions had been answered than patients who received care from other providers or in other settings. This suggests that in planning to screen populations for disorders that have complex genetics or that are likely to have phenocopies, it will be very important to give participants access to follow-up with knowledgeable providers who can provide appropriate additional evaluation, interpret results, and convey recommendations as clearly as possible.
Except for C282Y homozygotes, English-speaking whites and those with higher educational attainment were more likely to correctly remember recommendations than other groups. This raises issues related not only to screening in underserved and culturally diverse populations but also to health literacy in general. Although information about HH/IO and the meaning of test results were shared at several points in the study—both in written and verbal form by culturally and linguistically competent providers—there was considerable misunderstanding of test results and recommendations. HEIRS Study letters reporting initial screening results were written at an eighth grade level, but it has been reported that 20–23% of US adults read at or below a fifth grade level,19 so our letters probably exceeded the reading ability of some participants. Language barriers also compound problems with health literacy.20 One study reported that nearly two thirds of Spanish-speaking diabetes patients had health literacy that was marginal or inadequate for managing their disease,21 and another showed that Spanish-speaking women with poor health literacy were 16 times less likely than those with better health literacy to get regular Pap smears.22 This emphasizes the need to use very simple, straightforward language and concepts to convey screening results and recommendations.
Knowledge about hemochromatosis and IO
Communicating important facts about HH/IO had mixed success. In general, respondents knew more about causation, treatment, and heritability of HH/IO than about potentially associated symptoms. Nearly all understood that it was possible to have HH and not know it, that build up of iron causes organ damage, and that it is important to treat HH before damage occurs. About two thirds understood that siblings of someone with HH are at risk, that it is bad to have too much iron in your blood, and that IO can be treated by removing blood. Fewer recognized that an HFE mutation carrier could have a homozygous sibling who could be at greater risk, that IO could cause fatigue, arthritis, and heart problems, and that the disease could be fatal. Most did not understand the finer aspects of the disease—including incomplete and age/sex-dependent penetrance and subtleties of genotype-phenotype correlation. Only one in five understood that HFE genotyping could not tell if IO was already present. If genotyping is to be used for future HH screening, this point should be made clearly in pretest education.
Results from an Australian program that offered workplace genotypic screening for HH and assessed the efficacy of pretest education via either an oral or video presentation using pre- and posttest questionnaires also showed that participants were significantly more likely to accurately remember information about etiology and treatment than about penetrance or genetic heterogeneity. This study found no difference between the two methods for conveying information about etiology or treatment, but showed that an oral explanation was more effective in explaining penetrance whereas a video better conveyed the concept of genetic heterogeneity. Younger participants and those with higher educational attainment scored higher on questions about these more difficult concepts. C282Y homozygotes, who had the benefit of postscreening face-to-face counseling about their results as well as continued interaction with medical professionals as part of surveillance and treatment, best retained knowledge over time.23
In the HEIRS Study, educational level, race/language, age, and genotype all contributed to the model predicting knowledge about HH/IO. Although the study provided educational materials and counseling in subjects' preferred language, better scores correlated with being English speaking, higher educational attainment, and seeking information about HH/IO. Younger subjects generally scored higher—an effect that was also seen in patients asked about issues related to factor V Leiden.19 Encouragingly, those with genotypes conferring the highest risk knew the most, with C282Y homozygotes scoring significantly higher than all other groups. Some of this difference appears to have been due to information provided at the clinic visit, because all groups who got genetic counseling (including wild-type cases) scored significantly higher on knowledge questions than wild-type controls—suggesting that face-to-face counseling improved understanding of HH/IO. Most participants also accessed at least one other source of information about HH/IO, and English speakers were about twice as likely to do so. English speakers most frequently got information from HEIRS print materials, followed by their personal physician. In non-English speakers, this preference was reversed. The German study also found that study participants often sought more information, with 62% of C282Y homozygotes, about 31% of heterozygotes, and more than 15% of wild-type individuals searching the Internet (55%), looking at professional literature (27%) or lay literature (21%), or attending a patient support organization (nearly 6%). The sources did not differ significantly by genotype.14
Kakai et al.24 also reported that different sources of information about cancer were utilized by three ethnically distinct groups of Hawaiians. They found that whites were more likely to prefer the Internet, telephone information services, medical journals and research newsletters, whereas Japanese relied on other sources of print media, TV, and providers of complimentary or alternative medicine. Other Asian-Pacific Islanders depended more on information from physicians, their social group and other cancer patients. Catz et al. reported that non-Hispanic whites obtained health information primarily from physicians, television, and the Internet, whereas minority groups utilized more varied nonelectronic sources, preferring to first read health information in pamphlets or brochures (written in their own language), and then discuss it with friends and health care providers.25 In contrast, we found that online information was accessed by one third of non-Hispanic whites, but also by a quarter of blacks and Hispanics—including non–English-speaking Hispanics. Interestingly, fewer English-speaking Asians and only 5% of non–English-speaking Asians used the Internet to find information about HH/IO—reminiscent of the findings in Hawaiian cancer patients.
As has already been reported by the HEIRS Study, all ethnic and linguistic groups screened supported sharing genetic risk information with family members.26 However, it is now clear that educational attainment, race, and language preference significantly affect understanding of genetic test results, with non-English speakers and those with no more than a high school education being least likely to answer questions about their genotype or its familial implications correctly. This is consistent with recent observations from focus groups on genetic issues that were conducted in underserved, culturally diverse populations.25 Investigators in this study reported that although most of the people studied expressed a desire to learn more, they had limited understanding of genetics and genetic testing and did not tend to seek health information from print sources. The challenges of providing genetics education to culturally and linguistically diverse groups in Australia have also been reported with an emphasis on the need to adjust not only translations of English words, but also diagrams and other teaching aids.23,27 If broad-based population screening for HH/IO is contemplated, it will be critical to have input from all target groups to find the best strategies for providing pretest education and communicating genetic test results with familial and health implications.
There are limitations to our study design. Baseline knowledge relevant to assessing a model for results communication and patient education was not collected. There were inconsistencies in delivering information to patients with regard to the counseling outline, counseling session content, and results letters. Some examples of inconsistencies include the fact that not all H63D carriers were specifically counseled about their genotype, that FCs and clinicians used multiple formats and language in letters summarizing findings and recommendations after the CE, and that not all letters were translated into the subjects' preferred languages (as were most other study materials). Some potential effects on patients' knowledge and satisfaction include poorer understanding of genotype and implications by those at lower genetic risk, and uncertainty about recommendations among non-English speakers and those with lower health literacy.
SUMMARY
To our knowledge, this is the first population-based HH/IO screening program to provide participants with their actual HFE C282Y and H63D genotype, as well as specific TS and SF laboratory values. Communicating essential information about genotype and iron status proved challenging and was harder when there was a “low-risk” genotype or an iron elevation of unclear etiology or significance. Genotyping for both HFE mutations may have clinical relevance in identifying those at increased genetic risk for IO, but thought needs to be given to providing clear and simple information about how much health risk is actually associated with particular genotypes, and about whether other family members need to be tested. The same is true for recommendations about surveillance for iron elevation, and particularly for therapeutic phlebotomy.
Most people in the HEIRS Study understood that IO is preventable and treatable, and that HH mutations can run in families. In the future, information sent with normal screening results should emphasize when no further action is needed or appropriate. If broad-based population screening for HH/IO is to be beneficial, various dimensions of health literacy must be taken into account. This includes not just reading level and educational attainment, but also ethnicity, language, cultural beliefs, and acculturation. Past heterozygote screening programs have shown the importance of involving target communities in the planning.
To date, most genetic screening programs have been aimed at finding people at increased reproductive risk for recessive disorders that have straightforward genetics. Findings from the HEIRS Study underscore that screening for genetic disorders associated with increased personal health risk, or conditions with reduced penetrance and/or complex gene/environmental interactions will require further research to learn how to successfully convey difficult risk information, surveillance and treatment recommendations, and implications for family members to diverse populations with varying degrees of health literacy.
References
Bacon BR, Sadiq SA . Hereditary hemochromatosis: presentation and diagnosis in the 1990s. Am J Gastroenterol 1997; 92: 784–789.
Adams PC . Hemochromatosis. Clin Liver Dis 2004; 8: 735–753.
Barton JC, McDonnell SM, Adams PC, Brissot P, et al. Management of hemochromatosis. Hemochromatosis Management Working Group. Ann Intern Med 1998; 129: 932–939.
Burke W, Reyes M, Imperatore G . Hereditary haemochromatosis: a realistic approach to prevention of iron overload disease in the population. Best Pract Res Clin Haematol 2002; 15: 315–328.
Nisselle AE, Delatycki MB, Collins V, Metcalfe S, et al. Implementation of Haemscreen, a workplace-based genetic screening program for hemochromatosis. Clin Genet 2004; 65: 358–367.
Bradley LA, Haddow JE, Palomaki GE . Population screening for haemochromatosis: a unifying analysis of published intervention trials. J Med Screen 1996; 3: 178–184.
Adams PC, Kertesz AE, McLaren CE, Barr R, et al. Population screening for hemochromatosis: a comparison of unbound iron-binding capacity, transferrin saturation, and C282Y genotyping in 5,211 voluntary blood donors. Hepatology 2000; 31: 1160–1164.
Adams PC, Reboussin DM, Barton JC, McLaren CE, et al. Hemochromatosis and iron-overload screening in a racially diverse population. N Engl J Med 2005; 352: 1769–1778.
McLaren CE, Barton JC, Adams PC, Harris EL, et al. Hemochromatosis and Iron Overload Screening (HEIRS) study design for an evaluation of 100,000 primary care-based adults. Am J Med Sci 2003; 325: 53–62.
Bulaj ZJ, Ajioka RS, Phillips JD, LaSalle BA, et al. Disease-related conditions in relatives of patients with hemochromatosis. N Engl J Med 2000; 343: 1529–1535.
Patch C, Roderick P, Rosenberg W . Factors affecting the uptake of screening: a randomised controlled non-inferiority trial comparing a genotypic and a phenotypic strategy for screening for haemochromatosis. J Hepatol 2005; 43: 149–155.
Beutler E, Felitti VJ, Koziol JA, Ho NJ, et al. Penetrance of 845G→A (C282Y) HFE hereditary haemochromatosis mutation in the USA. Lancet 2002; 359: 211–218.
Patch C, Roderick P, Rosenberg W . Comparison of genotypic and phenotypic strategies for population screening in hemochromatosis: assessment of anxiety, depression, and perception of health. Genet Med 2005; 7: 550–556.
Stuhrmann M, Hoy L, Nippert I, Schmidtke J . Genotype-based screening for hereditary hemochromatosis. II. Attitudes toward genetic testing and psychosocial impact—a report from a German pilot study. Genet Test 2005; 9: 242–254.
Lloyd FJ, Reyna VF, Whalen P . Accuracy and ambiguity in counseling patients about genetic risk. Arch Intern Med 2001; 161: 2411–2413.
Anderson RT, Wenzel L, Walker AP, Ruggiero A, et al. Impact of hemochromatosis screening in patients with indeterminate results: the hemochromatosis and iron overload screening study. Genet Med 2006; 8: 681–687.
Bauer KA . Role of thrombophilia in deciding on the duration of anticoagulation. Semin Thromb Hemost 2004; 30: 633–637.
Hellmann EA, Leslie ND, Moll S . Knowledge and educational needs of individuals with the factor V Leiden mutation. J Thromb Haemost 2003; 1: 2335–2339.
Kirsch IS, Jungeblut A, Jenkins L, Kolstad A . Adult literacy in America: a first look at the results of the National Adult Literacy Survey. Washington, DC: U.S. Government Printing Office, 1993: 1–176.
Kundig D, Affonso D, Chudler E, Gaston M, et al. Health literacy: a prescription to end confusion. Washington, DC: Institute of Medicine, 2004.
Williams MV, Parker RM, Baker DW, Parikh NS, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA 1995; 274: 1677–1682.
Garbers S, Chiasson MA . Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Prev Chronic Dis 2004; 1: A07.
Nisselle AE, Collins VR, Gason AA, Flouris A, et al. Educational outcomes of a workplace screening program for genetic susceptibility to hemochromatosis. Clin Genet 2006; 69: 163–170.
Kakai H, Maskarinec G, Shumay DM, Tatsumura Y, et al. Ethnic differences in choices of health information by cancer patients using complementary and alternative medicine: an exploratory study with correspondence analysis. Soc Sci Med 2003; 56: 851–862.
Catz DS, Green NS, Tobin JN, Lloyd-Puryear MA, et al. Attitudes about genetics in underserved, culturally diverse populations. Community Genet 2005; 8: 161–172.
Tucker DC, Acton RT, Press N, Ruggiero A, et al. Predictors of belief that genetic test information about hemochromatosis should be shared with family members. Genet Test 2006; 10: 50–59.
Saleh MT, Barlow-Stewart KK . Genetics education in a culturally diverse population—lessons learnt, future directions. Ann Hum Biol 2005; 32: 211–217.
Acknowledgements
The HEIRS Study was initiated and funded by NHLBI, in conjunction with NHGRI. The study is supported by contracts N01-HC-05185 (University of Minnesota), N01-HC-05186 (Howard University), N01-HC-05188 (University of Alabama at Birmingham), N01-HC-05189 (Center for Health Research, Portland), N01-HC-05190 (University of California, Irvine), N01-HC-05191 (London Health Sciences Centre), N01-HC-05192 (Wake Forest University). Additional support was provided by the Howard University General Clinical Research Center (GCRC) grant, M01-RR10284, and the General Clinical Research Center, College of Medicine, University of California, Irvine, with funds provided by the National Center for Research Resources. 5M01RR 00827-29, US Public Health Service.
Field Centers: Birmingham, AL—University of Alabama at Birmingham: Dr. Ronald T. Acton (Principal Investigator), Dr. James C. Barton (Co-Principal Investigator), Ms. Deborah Dixon, Dr. Charles A. Rivers, Dr. Diane Tucker and Ms. Janice C. Ware. Irvine, CA—University of California, Irvine: Dr. Christine E. McLaren (Principal Investigator), Dr. Gordon D. McLaren (Co-Principal Investigator), Dr. Hoda Anton-Culver, Ms. Jo Ann A. Baca, Dr. Thomas C. Bent, Dr. Lance C. Brunner, Dr. Michael M. Dao, Dr. Korey S. Jorgensen, Dr. Julie Kuniyoshi, Dr. Huan D. Le, Dr. Miles K. Masatsugu, Dr. Frank L. Meyskens, Dr. David Morohashi, Dr. Huan P. Nguyen, Dr. Sophocles N. Panagon, Dr. Chi Phung, Dr. Virgil Raymundo, Dr. Thomas Ton, Professor Ann P. Walker, Dr. Lari B. Wenzel and Dr. Argyrios Ziogas. London, Ontario, Canada—London Health Sciences Center: Dr. Paul C. Adams (Principal Investigator), Ms. Erin Bloch, Dr. Subrata Chakrabarti, Ms. Arlene Fleischhauer, Ms. Helen Harrison, Ms. Kelly Jia, Ms. Sheila Larson, Dr. Edward Lin, Ms. Melissa Lopez, Ms. Lien Nguyen, Ms. Corry Pepper, Dr. Tara Power, Dr. Mark Speechley, Dr. Donald Sun and Ms. Diane Woelfle. Portland, OR and Honolulu, HI—Kaiser Permanente Center for Health Research, Northwest and Hawaii, and Oregon Health & Science University: Dr. Emily L. Harris (Principal Investigator), Dr. Mikel Aickin, Dr. Elaine Baker, Ms. Marjorie Erwin, Ms. Joan Holup, Ms. Carol Lloyd, Dr. Nancy Press, Dr. Richard D. Press, Dr. Jacob Reiss, Dr. Cheryl Ritenbaugh, Ms. Aileen Uchida, Dr. Thomas Vogt and Dr. Dwight Yim. Washington, D.C.—Howard University: Dr. Victor R. Gordeuk (Principal Investigator), Dr. Fitzroy W. Dawkins (Co-Principal Investigator), Ms. Margaret Fadojutimi-Akinsiku, Dr. Oswaldo Castro, Dr. Debra White-Coleman, Dr. Melvin Gerald, Ms. Barbara W. Harrison, Dr. Ometha Lewis-Jack, Dr. Robert F. Murray, Dr. Shelley McDonald-Pinkett, Dr. Juan Romagoza and Dr. Robert Williams. Central Laboratory: Minneapolis, MN—University of Minnesota and Fairview-University Medical Center: Dr. John H. Eckfeldt (Principal Investigator and Steering Committee Chair), Ms. Catherine Leiendecker-Foster, Dr. Ronald C. McGlennen, Mr. Greg Rynders and Dr. Michael Y. Tsai. Coordinating Center: Winston-Salem, NC—Wake Forest University: Dr. David M. Reboussin (Principal Investigator), Dr. Beverly M. Snively (Co-Principal Investigator), Dr. Roger Anderson, Ms. Elease Bostic, Ms. Brenda L. Craven, Ms. Shellie Ellis, Dr. Curt Furberg, Mr. Jason Griffin, Dr. Mark Hall, Mr. Darrin Harris, Ms. Leora Henkin, Dr. Sharon Jackson, Dr. Tamison Jewett, Mr. Mark D. King, Mr. Kurt Lohman, Ms. Laura Lovato, Dr. Joe Michaleckyj, Ms. Shana Palla, Ms. Tina Parks, Ms. Leah Passmore, Dr. Pradyumna D. Phatak, Dr. Stephen Rich, Ms. Andrea Ruggiero, Dr. Mara Vitolins, Mr. Gary Wolgast and Mr. Daniel Zaccaro. NHLBI Project Office: Bethesda, MD—Ms. Phyliss Sholinsky (Project Officer), Dr. Ebony Bookman, Dr. Henry Chang, Dr. Richard Fabsitz, Dr. Cashell Jaquish, Dr. Teri Manolio and Ms. Lisa O'Neill. NHGRI Project Office: Bethesda, MD—Ms. Elizabeth Thomson. Dr. Jean MacCluer, Southwest Foundation for Biomedical Research, also contributed to the design of this study.
Author information
Authors and Affiliations
Consortia
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Walker, A., Tucker, D., Hall, M. et al. Results communication and patient education after screening for possible hemochromatosis and iron overload: experience from the HEIRS Study of a large ethnically and linguistically diverse group. Genet Med 9, 778–791 (2007). https://doi.org/10.1097/GIM.0b013e318159a303
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e318159a303