Abstract
Purpose: Little is known about reasons why eligible breast cancer patients decline BRCA mutation testing. They may withdraw at different stages during genetic counseling for different reasons. We prospectively studied perceived benefits and barriers to genetic counseling and BRCA testing in 102 newly diagnosed breast cancer patients approached for genetic counseling at the start of radiotherapy.
Methods: Patients completed questionnaires and participated in interviews at different stages of the counseling protocol.
Results: Participation was not influenced by distress, knowledge about hereditary breast cancer, previous genetic testing in relatives, or perceived risks and barriers. Immediate decliners (n = 23) do not believe genetic testing is relevant for them. Patients who decline after pedigree compilation (n = 14) are more hesitant and anxious about the influence of the test result on their future often wishing to postpone further testing. Late decliners (n = 7) withdraw afraid of the test result and/or after a relative's objection. These decliners are not easily identified upon approach because they are similar to patients who receive a DNA test result (n = 58). Notwithstanding their decline, 81% agreed to the timing or would have preferred an earlier approach for genetic counseling.
Conclusion: Decliners may make more informed decisions after tailored health education, including adequate risk information.
Similar content being viewed by others
Main
Women from high-risk families can obtain risk estimations for breast and ovarian cancer through BRCA1/2 mutation testing. Carrying a BRCA1/2 gene mutation increases one's lifetime risk of developing breast and/or ovarian cancer compared with the general population.1 The most noted benefits of testing for mutations are: (1) to obtain breast cancer risk information for one's self and family members, particularly any children, (2) to learn about ovarian cancer risk, (3) to obtain certainty, and (4) to make more informed decisions about prophylactic mastectomy and prophylactic oophorectomy.2–8 Despite these evident benefits, not all eligible individuals choose to participate in genetic counseling and BRCA1/2 testing.
The uptake of presymptomatic testing is higher in persons of higher socioeconomic status, who have health insurance, who show a higher knowledge about DNA testing, who perceive the benefits as important, and who have more relatives affected by breast cancer.3 In addition, Biesecker et al.9 found that members of families with an identified BRCA mutation were more likely to have genetic testing when they become old (>40 years), married, and if there was a higher level of family cohesiveness. In these families, cancer-specific distress and worry play a significant role in the choice to test for BRCA1 mutations2,10 as does a greater perceived risk of being a mutation carrier and of developing breast or ovarian cancer, and the perception that the advantages of BRCA testing outweigh the disadvantages.2,11
For eligible individuals from mutation-positive families who decline presymptomatic genetic testing, the disadvantages outweigh the advantages; in particular, concerns about health and life insurance and job discrimination were mentioned.5,12,13 Additional barriers included the possible emotional impact on one's self and family, apprehension about the test result, travel distance to the cancer clinic, and time away from work and family. Female decliners also felt that they might receive less frequent screening if no BRCA mutation was identified.12,14 At-risk family members with a more optimistic disposition were less likely to opt for testing than those who were less optimistic.9 Comparing tested and nontested at-risk women revealed that the nontested group had a higher education level, were more often childless, showed more reluctance toward prophylactic surgery, were younger when first confronted with a relative affected by breast or ovarian cancer, and had been aware longer of the genetic nature of the disease.14,15 Anxiety does not appear to play any significant role in the choice not to undergo genetic testing,15 although cancer worry was lower among decliners in families with a BRCA mutation.14
As in unaffected individuals, the uptake of BRCA testing in women with early-onset breast cancer is higher among those who know more about BRCA1/2 testing and who have a more positive attitude to testing. In contrast to the presymptomatic test group, women with breast cancer who had genetic testing done were younger, had a higher education level, and more often had a family member who had also undergone genetic testing.16 In the same sample, low uptake was associated with lack of information on how genetic testing might alter health care decisions and fear of the test procedure, its costs, and possible false-positive results. Compared with healthy at-risk individuals who opt for presymptomatic testing, women with breast cancer are more often motivated to attend familial breast cancer clinics for the sake of their children, because of the worry about developing a second cancer themselves, or for scientific research purposes. Unaffected women attend to gain risk information for themselves, or for the sake of surveillance.17,18 If there is a prompt genetic test at the time of the initial breast cancer diagnosis, uptake is associated with a physician's recommendation for BRCA1/2 testing and indecision about definite local treatment.19 Although the mean real uptake for genetic testing among women with a personal history of breast cancer (70%, range 26–96%) does not differ from that of unaffected women with a family history of breast cancer (70%, range 20–96%), as reviewed by Ropka et al.,20 these two groups may differ as to their reasons for not having a test. The perceived importance of benefits is associated with uptake in presymptomatic DNA testing.3 Among women with a personal history of breast cancer, Capelli et al.21 identified the association between perceived benefits and intentions to test. However, there was no association found between perceived benefits and initial contact geared toward participation in testing. The latter study was limited in that it did not provide data on actual uptake for genetic testing.
Considering the motivating role of perceived benefits and barriers and perceived risks on health-related behaviors,22 women who decline genetic counseling are likely to have different motivating perceptions about genetic testing when compared with women who decline genetic testing after counseling and those who do choose to test. Addressing these differences may prove valuable in increasing breast cancer prevention and control and informed decisions about participation in genetic counseling and testing, especially now that genetic testing may increasingly influence management decisions in recently diagnosed breast cancer patients.23
In previous research, focusing on predictive factors for BRCA1/2 gene mutations in recently diagnosed breast cancer patients, a substantial proportion of the participants dropped out during the genetic counseling protocol after an active approach for genetic testing.24 The reasons for withdrawal were not thoroughly studied, although the main reason given was patients' concern for the additional psychological burden imposed by genetic testing. To our knowledge, neither the reasons for or the timing of withdrawal from genetic counseling and testing among recently diagnosed breast cancer patients have been studied. Nor have we identified studies that report on the magnitude of benefits and barriers as perceived by this population.
The aim of this study was to explore the perceived benefits and barriers, as well as the attitude and level of psychological distress, in newly diagnosed breast cancer patients actively approached for genetic counseling and BRCA1/2 testing who either (a) decline genetic counseling after the initial approach; (b) initially participate in counseling (family pedigree compilation) but then decline further counseling; or (c) participate in genetic counseling but decline BRCA1/2 testing. An additional aim was to identify the characteristics of these three groups compared with breast cancer patients who choose to have a BRCA test.
Based on a literature study and theoretical network, we expected breast cancer patients who declined genetic counseling upon approach to perceive fewer benefits to genetic testing,5,11,12,16 have a lower perceived risk of carrying a mutation,2 report less breast cancer-specific distress before approach,2,10,14 show a more optimistic disposition,9 know less about hereditary breast cancer,16 and to be older16 than patients who choose to have a BRCA test.5,11,12,16 We expect patients who decline later in the counseling protocol to differ less from patients who choose to take part in testing than from patients who decline genetic counseling upon approach. Considering psychological distress we expect immediate decliners to be motivated by an anticipated psychological burden, and patients who withdraw at a later time in counseling to do so because of an actual increase in experienced psychological distress.
MATERIALS AND METHODS
Participants
Our sample was selected from breast cancer patients participating in a longitudinal study examining the psychological impact of an active approach for genetic counseling and testing during adjuvant radiotherapy (see below). Participants for the longitudinal study were recruited from all consecutive breast cancer patients referred to the Department of Radiotherapy at the University Medical Center Utrecht in The Netherlands between January 2002 and March 2004. Participants were patients who were diagnosed with breast cancer for the first time, were between 18 and 75 years of age, and had a good comprehension of the Dutch language.
Procedure
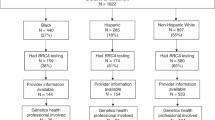
The initial approach for genetic counseling has been described elsewhere.25 During their first visit to the Department of Radiotherapy, patients were screened for eligibility for genetic counseling using factors presumed to be predictive for hereditary breast cancer. If they checked positive for at least one factor, patients were offered a family pedigree compilation; this was the initial approach. If the pedigree displayed at least one of the criteria for further counseling (e.g., (1) breast cancer in the patient or a relative <40 years of age, (2) patient had two or more relatives with breast cancer, (3) multifocal, multicentric, or bilateral breast cancer in the patient or a relative with the first breast cancer diagnosed <50 years of age, (4) ovarian cancer in the patient or a relative, or (5) a male relative with breast cancer), the patient was referred to the Department of Medical Genetics for genetic counseling and a BRCA test (Fig. 1).
All participants filled in questionnaires 1 week before the initial approach for genetic counseling (T0) and 4 weeks after the initial approach (T1). Patients who declined further genetic counseling after the initial approach were interviewed in their own home by a psychologist within 2 weeks of T1.
Patients who chose to take part in genetic counseling filled in a third questionnaire (T2) followed by an interview within 2 weeks. Of each group a random selection of 25 patients was approached for participation in an interview. The timing of T2 depended on whether the patient withdrew from the genetic counseling protocol. Participants who initially took part in counseling (family pedigree compilation) but who declined further counseling completed T2, 3 weeks after the pedigree compilation (11 weeks after initial approach). Patients who participated in genetic counseling but declined a BRCA test completed T2, 3 weeks after their first visit at the Department of Medical Genetics (27 weeks after initial approach). Patients who took part in genetic counseling and had a BRCA test completed T2, 3 weeks after receiving their test result (43 weeks after initial approach). Questionnaires were sent by mail and returned within 10 days using a prestamped return envelope. Approval for this study was obtained from the Medical Ethical Committee of the University Medical Centre Utrecht.
MEASURES
Questionnaires
Psychological distress
Psychological distress was measured at T0, T1, and T2 using the Hospital Anxiety and Depression Scale for general anxiety and depression and the Impact of Event Scale for breast cancer-specific distress.
The Hospital Anxiety and Depression Scale26 is a 14-item scale with a total score ranging from 0 to 42. A total score of >13 is indicative of an adjustment disorder.27
The Impact of Event Scale28 is a 15-item scale measuring intrusion (the extent to which individuals are overwhelmed by thoughts and feelings about breast cancer; seven items) and avoidance (the tendency to avoid thoughts and feelings about breast cancer; eight items) with a total score ranging from 0 to 75. A score of ≥26 is considered indicative of clinical adaptation difficulties.29 Items were geared toward breast cancer as the distressing event.
Perceived risk of carrying a mutation
At T1 and T2, patients were asked to indicate their perceived risk that their breast cancer was hereditary on a numerical scale from 0 to 100.
Knowledge of hereditary breast and ovarian cancer
The level of correct knowledge about hereditary breast cancer was assessed at T1 and T2 with items used by Pieterse et al.30 (adapted from Claes et al.31). The 7 items were worded as statements with three response categories: “correct,” “incorrect,” and “do not know.” The number of correct answers for the relevant items provided a total correct knowledge score (range 0–7).
Optimism
Optimism was assessed at baseline (T0) using an 8-item subscale of the Self-Assessment Questionnaire-Nijmegen.32,33 This 4-point frequency scale ranges from “almost never ” to “nearly always,” with a total score ranging between 8 and 32. Higher scores indicate a more optimistic outlook on life.
Attitude toward genetic counseling and testing
At T1 attitude toward genetic counseling and BRCA testing was assessed with five self-designed items (Appendix A).
Interview
The semistructured interview with a psychologist took place in the patient's home and lasted 60–90 minutes. It consisted of open questions, with some followed by the opportunity to provide a number between 0 and 100 to indicate the magnitude of a given answer. Other items consisted of prestated answer categories inviting patients to indicate agreement with a statement using a number between 0 and 100. Interview items selected for this report are presented in Appendix B. Interviews were taped as well as scored on paper. Two psychologists independently categorized the answers to the open questions, after which these and the prestated answers were entered into an SPSS database version 11.0 (SPSS Inc., Chicago IL).
Motivation
Patients were asked to provide up to three reasons, in order of importance, on why they had decided to take part in genetic counseling and BRCA testing, or why they had chosen not to.
Benefits and barriers
Patients were asked to state their perceived benefits from undergoing genetic counseling and BRCA testing, each followed by a number between 0 and 100 indicating the magnitude of the perceived benefit. Then the psychologist stated six possible benefits based on literature, regarding each of which patients were asked to indicate the extent to which they agreed with the statement using a number between 0 and 100. For each of the four study groups, the mean total scores for benefits and the mean scores for each individual benefit were computed. The same procedure was followed for perceived barriers.
Timing of approach
Patients were asked if there might have been a better point in time to inform them about hereditary breast cancer (yes or no). If yes, patients were asked to elaborate on when would have been a better time.
Statistics
Descriptive statistics were used to provide insight into the build up of variables among groups. For comparison between the groups nonparametric statistics were applied through SPSS version 11.0, including the Mann-Whitney U test and Kruskal-Wallis test for continuous variables and the Fisher exact test for nominal variables.
RESULTS
Sample characteristics
Of the 669 breast cancer patients approached to take part in the longitudinal psychological study, 402 breast cancer patients participated fully. Of these 402 patients, 102 (26%) were eligible for pedigree compilation and further counseling and were included in the present study. Twenty-three (23%) patients declined a pedigree compilation (Group 1). After pedigree compilation, 14 (14%) patients declined referral to the Department of Medical Genetics for further counseling (Group 2). After initial counseling at the Department of Medical Genetics seven (7%) patients declined a BRCA test (Group 3). Fifty-eight (57%) patients took part in genetic counseling and testing and received a test result (Group 4) (Fig. 1). A mutation was detected in five patients and 53 received an uninformative test result. None of the patients had previously participated in genetic counseling or BRCA1/2 testing.
Demographic characteristics and medical history
There were no differences between patients who did not reply, patients who dropped out of the psychological study, and participants on any of the sociodemographics other than that Group 4 was significantly younger (mean age: 47 years) than the dropouts (54 years) (F = 12.38, P = 0.001). Participants did not differ in medical history from patients who did not reply or who dropped out of the study, and Groups 1–3 did not differ from Group 4. Demographic characteristics and medical history of the four groups are given in Table 1. Comparing the four groups revealed a significantly older age for Group 1 than Group 4. The mean number of days postoperation showed a trend toward a significant difference in which Group 1 had the longest average time span between surgery and the approach for genetic counseling.
Psychological distress
There were no differences in psychological distress between breast cancer patients who declined genetic counseling and/or testing (Groups 1–3) and patients who received a test result (Group 4) at baseline (T0), after approach (T1), or when leaving the genetic counseling protocol (Table 2)
Group 2 demonstrated more general anxiety and depression at baseline (T0) than Group 1 (χ2 = 10.897, P = 0.012). At T1 and T2 there were no differences in psychological distress between the four groups (Table 2).
Perceived risk of carrying a mutation
After approach (T1) patients from Group 1 through 3 reported a lower perceived risk of carrying a mutation (mean 22.44, SD 24.57) than patients from Group 4 (mean 36.35, SD 25.29) (Z = −2.903, P = 0.004).
After approach (T1) patients from Group 2 demonstrated the lowest perceived risk that their breast cancer might be hereditary (mean 13.1, SD 15.48), thereby differing significantly from the patients from Group 4 (χ2 = 12.588, P = 0.006). At T1, Groups 1 and 3 reported a perceived risk of 23.3 (SD 28.67) and 37.1 (SD 18.00), respectively. There were no differences between Groups 1–3 and Group 4 or between all four groups at T2.
Knowledge of HBOC
At T1 there was no difference in mean correct knowledge score between Groups 1 through 3 (mean 4.22, SD 1.47) and Group 4 (mean 4.50, SD 1.55). Nor was there a difference between these two groups at T2. At T1 and T2, Groups 1 through 4 did not differ from each other on mean correct knowledge score.
Optimism
At baseline, patients from Groups 1 through 3 (mean 23.66, SD 4.33) did not differ from those from Group 4 (mean 23.35, SD 4.16) on level of optimism. Nor did the patients from Groups 1 through 4 differ from each other.
Attitude toward genetic testing
Regarding thoughts about hereditary breast cancer in the family there was no difference between Groups 1 through 3 and Group 4 at T1. Of the patients in Groups 1 and 2, more than half reported that the thought of hereditary breast cancer had not occurred to them or their family. Groups 3 and 4 more often reported having had this thought to some extent compared with Group 1 (Table 3).
Of the 102 participants, nine reported previous cancer genetic counseling and or BRCA testing in their family; they were evenly distributed across all four groups.
At T1 the patients from Group 1 through 3 differed from Group 4 in wanting to know if their breast cancer was hereditary (χ2 = 25.446, P < 0.001). 87% of patients in Group 4 wanted to know, and only 13% of this group was hesitant. Groups 1 through 3 were more heterogeneous; 31% wanted to know, 34% was hesitant, and 34% did not want to know. Comparing all four groups, Groups 3 and 4 displayed the same interest in genetic counseling and testing, both differing significantly from Group 1. Immediately after approach more than half of Group 2 had reported wanting to know if their breast cancer was hereditary. Group 1 most often reported having no interest (Table 3).
As to their preference of which medical specialist should provide them with information about possible hereditary breast cancer, we found no differences between Groups 1 through 3 and Group 4. The majority of breast cancer patients in all four groups preferred the surgeon to provide them with information if there was a suspicion of hereditary breast cancer. Among the four groups, Group 2 more often preferred information from their family physician than Groups 3 and 4. Groups 2 and 4 more often desired a specialist from the other category, in particular, the treating medical oncologist (Table 3).
Patients from Groups 1 through 3 expected the least influence of a possible carrier status on their future (49% very little to none). In Group 4, 27% expected a carrier status to influence their future very much compared with 10% in Groups 1 through 3 (χ2 = 11.195, P = 0.009). Group 3 anticipated the highest influence of a possible carrier status on their future.
Interview
Of the 102 participants, 67 took part in an interview: all 23 patients from Group 1, 11 of 14 from Group 2, 5 of 7 from Group 3, and from Group 4, 25 of 25 with an uninformative test result and 3 of 5 with an identified mutation.
Motivation
Motivation for genetic counseling and BRCA1/2 testing
Two psychologists independently scored the reasons for participating in genetic testing and identified eight categories as listed in Table 4. The main reason by far was for the sake of the children followed by preventive measures, the need for certainty, and to inform family members. Informing family members was the most reported second reason followed by for the sake of the children and preventive measures.
Motivation to decline genetic counseling and/or BRCA1/2 testing
The reasons identified for declining genetic counseling or testing are listed in Table 5. All of the 39 patients who declined genetic counseling and or testing gave at least one main reason for declining. Twenty-two (56%) patients gave a second reason and seven (18%) patients gave a third.
Patients from Group 1 most often gave three reasons for declining (26%) compared with patients from Group 2 (0%) and Group 3 (20%). Group 1 reported disbelief as their main reason, followed by not wanting contact with family members and not having children (other category). Patients from Group 2 most often declined to postpone genetic counseling and/or BRCA testing to a later point in time. An additional reason to decline for Group 2 was not having children (other category). In Group 3 most patients declined because of the objections by a family member or anxiety of what the test result might bring. The exact numbers and percentages per group are given in Table 5.
Benefits and barriers
Patients from Groups 1 through 3 perceived the total benefits (total mean = 237.5) as less important than patients from Group 4 (total mean = 300.7) (Z = −1.908, P = 0.050). Both groups reported barriers to the same magnitude. Patients from Group 4 perceived better medical treatment (Z = −2.537, P = 0.011) and informing family members (Z = −2.193, P = 0.028) as greater benefits than Groups 1 through 3.
The comparison between groups on endorsement of benefits and barriers to genetic counseling and testing is given in Table 6 and reveals a significantly higher endorsement of the benefit of better medical treatment by Group 4 than Group 1.
Besides the structured categories, 13 patients initiated benefits in the “other” category. These were mostly patients who declined to have a pedigree drawn up (n = 8). Two psychologists independently identified the following four benefits in the other category: (1) knowing for the children (n = 6), (2) for the sake of research (n = 3), (3) obtaining certainty (n = 3), and (4) motivation to change one's lifestyle (n = 1). Two patients said they saw no benefits from genetic counseling and testing; however, they agreed to some extent with the benefits suggested.
Five barriers in the other category were reported by 11 patients divided over all four groups and including: (1) not wanting to burden their children (n = 3), (2) fear of having to face the dilemma of prophylactic treatment brought on by a possible carrier status (n = 3), (3) worry or feeling guilty about having passed on a faulty gene (n = 2), (4) remaining uncertainty despite a test result (n = 2), and (5) fear of burdening female relatives (n = 1). One patient did not see any barriers to genetic counseling or testing. The self-initiated benefits and barriers (other category) were endorsed strongly compared with those suggested during the interview (Table 6).
Timing approach
Of the 67 patients who took part in the interview, 43 (64%) agreed with the timing of the approach for genetic counseling and the other 24 (36%) did not agree; 22 of 24 suggested a better timing for the approach. Thirteen (19%) suggested a later point in time (because of feeling overwhelmed by their diagnosis and treatment) and 9 (13%) suggested an earlier approach, e.g., upon diagnosis or before surgery. Of the 13 patients who stated that they would have preferred a later approach, 11 (85%) had declined genetic counseling at some point and for 9 of 11 (69%) this was before or just after the pedigree analysis. Patients from Groups 1 through 3 less often agreed with the timing of our approach (47%) compared with patients from Group 4 (86%) (χ2 = 10.136, P = 0.002). The agreement with the timing of approach and the suggestions about a better timing per group can be found in Table 7.
DISCUSSION
As expected, newly diagnosed breast cancer patients who declined counseling immediately after approach were older,16 reported a lower perceived risk for carrying a BRCA mutation,2 and perceived the least benefits from genetic testing5,11,12,16 when compared with patients who received a DNA test result. Contrary to our expectations, there was no difference between decliners and participants in level of hereditary breast cancer knowledge16 or reported optimism,8 and level of distress was not associated with participation in genetic testing2,10,14 or timing of withdrawal from the counseling protocol.
For the most part immediate decliners had never considered the possibility that they might have hereditary breast cancer. However, the percentage of patients with at least one relative who had undergone genetic testing for cancer was comparable to the test group. Upon approach, half of the immediate decliners did not want to know if their breast cancer was hereditary. Of all decliners, the immediate decliners gave the most reasons for declining, of which disbelief was mentioned the most. Contrary to our expectations, fear of anticipated psychological distress as a result of genetic counseling and DNA testing was not given as a reason for decline. Besides the most reasons to decline, this group also listed the most benefits beyond those suggested. The reported disbelief is not due to less knowledge about hereditary breast cancer as one would expect from earlier studies10,16 because immediate decliners did not demonstrate less knowledge upon approach. Although these patients checked positive for at least one factor presumed predictive for hereditary breast cancer, it remains unknown whether they would have fulfilled criteria for further genetic counseling after pedigree compilation. Immediate decliners may have made an adequate risk calculation based on their own age, and the number and age of their relatives with breast cancer, resulting in a low perceived risk and the thought that, in their case, genetic counseling was not relevant. Patients who declined immediately after approach had the longest average time span between surgery and the approach for genetic counseling. Although only a trend toward significance was identified, an early approach might be beneficial to uptake, creating the opportunity to provide tailored counseling.
Patients who initially took part in genetic counseling but declined referral after pedigree compilation (early decliners) are comparable to immediate decliners in that for the most part no genetic testing for cancer had taken place in their family, most of the patients had never considered hereditary breast cancer and upon approach these groups perceived comparable low risks of carrying a BRCA mutation. Equal percentages of the immediate and early decliner groups were hesitant about wanting to know if their breast cancer was hereditary. Contrary to the immediate decliners, over half of the early decliner group upon approach reported wanting to know if their breast cancer was hereditary. The second main difference between the two groups was the main reason for declining: instead of disbelief, early decliners withdrew from the protocol to postpone further counseling and testing. Accordingly this group most often disagreed with the timing of the approach for counseling, generally preferring a later point in time. Of all decliners, early decliners displayed the highest level of general anxiety at baseline, significantly differing from the immediate decliners. However, this difference was no longer apparent when they left the genetic counseling protocol. One may speculate that this anxiety may have motivated them initially to take part in genetic counseling.2,10 However, this was not the case for the late decliner group or the BRCA test group and there was no difference in breast cancer-specific distress between all four groups.
The characteristics of the late decliner group were similar to those of patients who did choose to be tested. Apart from being younger, they had a comparable perceived risk of carrying a mutation, the thought of hereditary breast cancer had occurred to them to the same extent, and upon approach they showed the same initial desire to know if their cancer was hereditary. Compared with other decliner groups, the late decliners expected more influence of a possible carrier status on their future. This consideration may have played a major role in their choice not to have a BRCA test along with their main reasons for declining, because of the objection of a family member. Contrary to our expectations, these patients did not withdraw from the protocol because of experienced psychological distress; however, an important reason for late decliners to withdraw was the anticipation of the impact of being identified as a mutation carrier. These late decliners may include possible vulnerable first messengers8 in need of support in contacting their family if they choose to pursue genetic testing in the future. This groups' identified barriers are comparable to those found in other studies, e.g., expected emotional impact on one's self and family12 and apprehension about the test result.14 Barriers concerning health insurance, travel distance to the cancer clinic, and associated time commitment were not relevant,2,12,14 first because of the Dutch mandatory health insurance policy and second simply because of the relatively short distances within The Netherlands. Patients who did receive a DNA test result reported higher total perceived benefits than decliners. In this respect this study is in line with motivators of intention to test found by Cappelli et al.,21 therefore not supporting their suggestion that motivating factors for actual uptake may differ from those for intentions to test.
One's children as the main reason to have a DNA test done agrees with an earlier study.17 The latter study and our work differ in the method for measuring motivation; in the present study motivation was posed as an open question in contrast to the fixed response categories used by Van Asperen et al.17 After noting self-initiated benefits and barriers, fixed categories were offered to measure the degree of agreement and magnitude of total perceived benefits and barriers. Though the various reasons for having the BRCA test and the benefits, as well as for declining testing and the barriers, may overlap, we conclude that the actual reason for pursuing testing or withdrawing from the protocol may differ from the perceived benefits and barriers and that these should be studied as separate concepts.
As our study has been performed in one hospital, this may have limited the generalizibility of our findings. The present study is also limited by the sample size. What started as a reasonably large study sample was eventually divided into small subsamples of decliners, resulting in necessary caution when interpreting the results. However, we consider the sample size sufficient for this essentially explorative study. The sample size also meant that in the BRCA test group (n = 58) only five patients were identified as mutation carriers and 3 of 5 participated in an interview. Of the 53 patients who received a noninformative result, a random group of 25 were approached for an interview possibly providing a limited selection of reasons, benefits, barriers, and attitudes toward genetic counseling and testing.
Although decliners in the current study were from a clinical cohort as opposed to participants from a healthy population selected for research and no differences in sociodemographics or medical history were found compared with nonparticipants or dropouts, we should consider the possibility of a self-selected group. As a result, a particular group of decliners may not have been included in the study. One general concern in an attempt to study decliners is the group of nonparticipating decliners. The characteristics of these decliners are not known, which makes it impossible to identify the true need for health education for making a fully informed decision about primary and preventive treatment for one's self and family members.
Recently diagnosed breast cancer patients can be approached for genetic counseling without causing additional psychological distress.25 Only 19% of our total sample felt overwhelmed by their cancer diagnosis and treatment to the extent that they would have preferred to be approached for genetic counseling at a later point. The other 81% agreed with the timing of approach or would have liked to have been approached earlier during their primary treatment. This high percentage and the preference to receive information about hereditary breast cancer from a treating surgeon suggest an approach for genetic counseling before surgery, especially in view of the possible advantages such as early approach may have on the decision-making process for treatment.19,34 It is possible that findings would differ for newly diagnosed patients making treatment decisions. More research is needed to explore the consequences of such timing on patients' psychological well-being.
It is clear that recently diagnosed breast cancer patients will choose to take part in genetic testing despite perceived risks and barriers. The immediate decliners differ most in their attitude from the late decliners and patients who took part in genetic testing. Upon approach, 77% wanted to know if their breast cancer was hereditary, of which 73% continued with the protocol. The other 27% changed their mind during the genetic counseling protocol. Among these decliners were patients who wanted to take part in genetic testing, but at a later point in time, and patients who wanted genetic testing at the present time, but who chose not to have a BRCA test result because a family member objected or because they were anxious about the test result. Upon approach, all decliners differed from the tested group in regard to their interest in genetic counseling. It may prove valuable to identify possible early and late decliners upon approach to adequately tailor counseling toward optimizing informed decision-making. Possible early decliners may be identified by their higher level of hesitance toward genetic testing. However, identifying late decliners may be difficult because this group was similar to the test participants group. Future research may provide insight into whether early and late decliners ever take part in genetic testing and, if so, at what point in time they choose to do so. Foster et al.14 reported 77% of decliners among BRCA mutation families considered genetic testing in the future, however, the difference between hypothetical and actual uptake must not be forgotten.20
Notwithstanding the differences in attitude toward genetic testing and the differences in perceived risks and benefits between the subgroups of decliners, all the groups may be helped to make a more informed decision by receiving tailored health education, including adequate risk information. Rapid counseling may affect their decisions about their own primary treatment,22 despite possible different viewpoints of family members. Research exploring the attitudes of probands' family members toward genetic testing may provide insight into the needs of these family members.
References
King MC, Rowell S, Love SM . Inherited breast and ovarian cancer. What are the risks? What are the choices?. JAMA 1993; 269: 1975–1980.
Lerman C, Daly M, Masny A, Balshem A . Attitudes about genetic testing for breast-ovarian cancer susceptibility. J Clin Oncol 1994; 12: 843–850.
Lerman C, Narod S, Schulman K, Hughes C, et al. BRCA1 testing in families with hereditary breast-ovarian cancer. A prospective study of patients decision making and outcomes. JAMA 1996; 275: 1885–1892.
Struewing JP, Lerman C, Kase RG, Giambarresi TR, et al. Anticipated uptake and impact of genetic testing in hereditary breast and ovarian cancer families. Cancer Epidemiol Biomarkers Prev 1995; 4: 169–173.
Armstrong K, Calzone K, Stopfer J, Fitzgerald G, et al. Factors associated with decisions about clinical BRCA1/2 testing. Cancer Epidemiol Biomarkers Prev 2000; 9: 1251–1254.
Lodder LN, Frets PG, Trijsburg RW, Meijers-Heijboer EJ, et al. Presymptomatic testing for BRCA1 and BRCA2: how distressing are the pre-test weeks?. J Med Genet 1999; 36: 906–913.
Brandt R, Hartmann E, Ali Z, Tucci R, et al. Motivations and concerns of women considering genetic testing for breast cancer: a comparison between affected and at-risk probands. Genet Test 2002; 6: 203–205.
Bleiker EM, Hahn DEE, Aaronson NK . Psychosocial issues in cancer genetics. Acta Oncol 2003; 42: 276–286.
Biesecker BB, Ishibe N, Hadley DW, Giambarresi TR, et al. Psychosocial factors predicting BRCA1/BRCA2 testing decisions in members of hereditary breast and ovarian cancer families. Am J Med Genet 2000; 93: 257–263.
Lerman C, Schwartz MD, Lin TH, Hughes C, et al. The influence of psychological distress on use of genetic testing for cancer risk. J Consult Clin Psychol 1997; 65: 414–420.
Jacobsen PB, Valdimarsdottier HB, Brown KL, Offit K . Decision-making about genetic testing among women at familial risk for breast cancer. Psychosom Med 1997; 59: 459–466.
Geer KP, Ropka ME, Cohn WF, Jones SM, et al. Factors influencing Patients' decisions to decline cancer genetic counseling services. J Genet Couns 2001; 10: 25–40.
Peterson EA, Milliron KJ, Lewis KE, Goold SD, et al. Health insurance and discrimination concerns and BRCA1/2 testing in a clinic population. Cancer Epidemiol Biomarkers Prev 2002; 11: 79–87.
Foster C, Evans DGR, Eeles R, Eccles D, et al. Non-uptake of predictive genetic testing for BRCA1/2 among relatives of know carriers: attributes, cancer worry and barriers to testing in a multicenter clinical cohort. Genet Test 2004; 8: 23–29.
Lodder L, Frets PG, Trijsburg RW, Klijn JGM, et al. Attitudes and distress levels in women at risk to carry a BRCA1/BRCA2 gene mutation who decline genetic testing. Am J Med Genet A 2003; 119: 266–272.
Peters N, Domchek SM, Rose A, Polis R, et al. Knowledge, attitudes, and utilization of BRCA1/2 testing among women with early-onset breast cancer. Genet Test 2005; 9: 48–53.
Van Asperen CJ, Van Dijk S, Zoeteweij MW, Timmermans DRM, et al. What do women really want to know? Motives for attending familial breast cancer clinics. J Med Genet 2002; 39: 410–414.
Julian-Reynier C, Eisinger F, Chabal F, Aurran Y, et al. Cancer genetic clinics: why do women who already have cancer attend?. Eur J Cancer 1998; 34: 1549–1553.
Schwartz MD, Lerman C, Brogan B, Peshkin BN, et al. Utilization of BRCA1/BRCA2 mutation testing in newly diagnosed breast cancer patients. Cancer Epidemiol Biomarkers Prev 2005; 14: 1003–1007.
Ropka ME, Wenzel J, Phillips EK, Siadaty M, et al. Uptake rates for breast cancer genetic testing: a systematic review. Cancer Epidemiol Biomarkers Prev 2006; 15: 840–855.
Cappelli M, Surh L, Humphreys L, Verma S, et al. Psychological and social determinants of women's decisions to undergo genetic counseling and testing for breast cancer. Clin Genet 1999; 55: 419–430.
Evans DG, Lalloo F, Hopwood P, Maurice A, et al. Surgical decisions made by 158 women with hereditary breast cancer aged <50 years. Eur J Surg Oncol 2005; 31: 1112–1118.
Rosenstock IM . The Health Belief Model and preventive health behavior. Health Educ Monogr 1972; 2: 354–386.
Wárlám-Rodenhuis CC, Koot VCM, Van der Luijt RB, Vasen HFA, et al. A prospective study on predictive factors linked to the presence of BRCA1 and BRCA2 mutations in breast cancer patients. Eur J Cancer 2005; 41: 1409–1415.
Schlich-Bakker KJ, Wárlám-Rodenhuis CC, Van Echtelt J, Van den Bout J, et al. Short term psychological distress in patients actively approached for genetic counselling after diagnosis of breast cancer. Eur J Cancer 2006; 42: 2722–2728.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Razavi D, Delveaux N, Farvacques C, Robayes E . Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry 1990; 156: 79–83.
Horowitz M, Wilner N, Avarez W . Impact of event scale: a measure of subjective stress. Psychosom Med 1997; 41: 209–218.
Horowitz MJ, Stress response syndromes and their treatment. In: Goldenberger L, Breznitz S, editors, Handbook of stress. Theoretical and clinical aspects. New York: Free Press, 1982: 711–732.
Pieterse AH, Ausems MGEM, Van Dulmen AM, Beemer FA, et al. Initial cancer genetic counselling consultation: change in counselees' cognitions and anxiety, and association with addressing their needs and preferences. Am J Med Genet A 2005; 137: 27–35.
Claes E, Evers-Kiebooms G, Boogaerts A, Decruyenaere M, et al. Communication with close and distant relatives in the context of genetic testing for hereditary breast and ovarian cancer in cancer patients. Am J Med Genet A 2003; 116: 11–19.
Bleiker EM, van der Ploeg HM, Hendriks JH, Ader HJ . Personality factors and breast cancer development: a prospective longitudinal study. J Natl Cancer Inst 1996; 88: 1478–1482.
Westbrook MT . A classification of coping behavior based on multi-dimensional scaling of similarity ratings. J Clin Psychol 1979; 35: 407–410.
Weitzel JN, McCaffrey SM, Nedelcu R, MacDonald DJ, et al. Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Arch Surg 2003; 138: 1323–1328.
Acknowledgements
This study was sponsored by a grant from the Dutch Cancer Society (project code UU 2001-2386).
The authors are grateful to all participants for their valuable contribution to the study and to the radio-oncologists and the genetic counselors for their collaboration. Many thanks to Jeanne van Echtelt for including patients and monitoring participation in the study and Maria Schipper for her advise on statistical methods.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Appendices
Rights and permissions
About this article
Cite this article
Schlich-Bakker, K., ten Kroode, H., Wárlám-Rodenhuis, C. et al. Barriers to participating in genetic counseling and BRCA testing during primary treatment for breast cancer. Genet Med 9, 766–777 (2007). https://doi.org/10.1097/GIM.0b013e318159a318
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e318159a318
Keywords
This article is cited by
-
Statewide trends and factors associated with genetic testing for hereditary cancer risk in Arkansas 2013–2018
Hereditary Cancer in Clinical Practice (2022)
-
A Narrative Review of Implementing Precision Oncology in Metastatic Castration-Resistant Prostate Cancer in Emerging Countries
Oncology and Therapy (2021)
-
How the “control-fate continuum” helps explain the genetic testing decision-making process: a grounded theory study
European Journal of Human Genetics (2020)
-
Discussions about predictive genetic testing for Lynch syndrome: the role of health professionals and families in decisions to decline
Familial Cancer (2018)
-
BRCA testing within the Department of Veterans Affairs: concordance with clinical practice guidelines
Familial Cancer (2017)