Abstract
The Coffin-Lowry Syndrome (CLS) is a congenital disorder that can be recognized by retarded growth and development, the characteristic appearance of the face and hands, and often by the typical deformities of the back and chest; there are many other anomalies. The history of the syndrome is reviewed, noting the x-linked semidominant pattern of inheritance, and two autopsies are presented and compared with the three autopsy reports that have been published previously. The five young patients died at ages between 18 to 28 years of advancing pneumonia, aspiration of food into the trachea, or postoperative complications. There were lesions or abnormalities in the heart, brain, lungs, liver, skeleton, kidneys, intestines, and other organs. Molecular geneticists have located the CLS gene or Rsk-2 gene at Xp22.2 and demonstrated that it works by influencing the activation of other genes. The “monopolygenic” pattern may help to explain the large number of seemingly unrelated abnormalities that make up this syndrome.
Similar content being viewed by others
Main
In 1966 Coffin, Siris, and Wegienka1 described a syndrome in two unrelated boys that has become known as the Coffin-Lowry Syndrome (CLS). Our examination of both boys showed developmental retardation, short stature, plump, soft hands with lax, extensible joints and tapered fingers, and a distinctive facial appearance, with wide-set, down-slanted palpebral fissures, epicanthi, ptosis of the upper eyelids, flat maxillae, thick nasal septa, anteverted nostrils, and prominent forehead, brows, ears, and lips. Teeth were few and misaligned. Muscles were weak and hypotonic. The skin was easily stretched. Ligaments were loose, and feet were flat. The gait was slow, awkward, and shuffling. Each boy had kyphosis, a short bifid sternum, and pectus carinatum or excavatum. Both boys fell frequently. One boy had a heart murmur. X-ray studies showed a thick calvarium, small paranasal sinuses, delayed bone age, narrow-necked or “drumstick” terminal phalanges of the fingers, and a frayed and beaked anterior contour of several vertebral bodies. Respiratory infections were frequent. Intelligence quotients (IQ) varied from 54 to 20, and, like other aspects of the syndrome, seemed to grow worse with age. The mothers of both boys, and the sister and half-sister of one of them, had similar but less distinct anomalies and less disability.
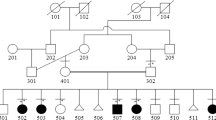
Soon after these first cases were published, we received communications from Italy, France, and Australia describing individuals and families with the same syndrome.2–4 In addition, we evaluated a family5 in which seven persons were affected in four generations, with transmission only from mother to child and with wide variation among females; some were severely disabled and others were unimpaired.
The second published report of the CLS was by Martinelli and Campailla in 19692 that described a boy whose parents and siblings showed no evidence of the syndrome. In 1970, Siris and Coffin6 published the Coffin-Siris Syndrome, a recognizable inborn error of development that is not the same as CLS. However, shared authorship has caused confusion between these names,7 and an old dictionary even cited the two syndromes as the same disorder with two different names.
The next 5 years produced additional reports of this syndrome. In 1971, Lowry et al.8 described a fourth family with CLS, and Coffin and Siris5 presented a fifth large family. In 1972, Carpentier3 reviewed two familial cases and three sporadic cases, and Procopis and Turner4 described a large Australian family showing probable x-linked dominant inheritance with variable penetrance. In 1973, a family was described by Jammes et al.9 In 1974, Hussels10 described a boy whose mother and sister were mildly affected. In 1975, De Marco11 presented a sporadic case. In 1975, Temtamy et al.12,13 presented three families. To prevent confusion, Temtamy suggested the eponym Coffin-Lowry Syndrome, which has become the standard term. In 1976, Smith14 reviewed the syndrome and accepted it as genuine.
Additional publications since 1976 are listed in the bibliography.15–54 They add several clinical and pathologic findings as probable features of the syndrome: thickened forearms,15–17 delayed closure of the anterior fontanel,8,9,18–22 and a con-spicuous longitudinal furrow or groove in the dorsum of the tongue.7,9,12,23–25 Dental anomalies have been described7,11,17,19,23–34 and include congenital absence of some teeth, delayed eruption, enamel hypoplasia, caries, early tooth loss, deformities, unusual sizes, malposition, and misalignments.
Sensorineural hearing impairment can appear in child-hood:16,26,27,31,35–37 slow conduction of the nerve impulse has been noted,38 but normal conduction has also been reported.4,9 Epilepsy does occur,1,8,17,23,25,29,39–41 although the frequent falls or “drop attacks”42–46 appear to be cataplexy or hyperexplexia (abrupt loss of muscle tone when the individual is startled). One patient ceased having attacks after surgery for scoliosis.45 Psychoses have been mentioned9,28,35,37,40 and a possible obsessive-compulsive tendency as well.30,72
Central nervous system changes are reported, including agenesis of the corpus callosum21,41,47 and calcification of the falx cerebri.23 A variety of cardiovascular abnormalities are reported, including murmur,1 increased impulse,4 and congenital heart disease.9 mitral prolapse or insufficiency,7,12,17,18,48 patent ductus arteriosus,21 and tricuspid insufficiency with decompensation and right ventricular hypertrophy.49 Inguinal hernias,1,7,12,17,27,35 umbilical hernia,3 rectal prolapse,1 and uterine prolapse7,12 have been reported. Many of these features have been listed and tabulated,17,18,23,29 and they are summarized in the standard texts.50,51 Visual problems and life expectancy have not drawn much attention.
Early searches for a metabolic disorder gave mixed results. In the first two patients,1 we found a lack of subcutaneous elastic fibers, although later observers have reported normal elastic fibers.4,7,12,15,23 Others have found radiographically detectable calcification of the elastic fibers of the ligamenta flava.55–57
Investigation of connective tissue has provided few common features. Vacuoles in skin fibroblasts,4 glycolipid-like lysosomal granules and vacuoles in cultured skin fibroblasts,10,12 and cytoplasmic granules in cultured cartilage cells58 have been observed, as have lipid droplets, which are probably normal, in fibroblasts and endothelial cells.18 Abnormal proteodermatan sulfate in cultures of skin fibroblasts from three patients,59 an accumulation of hyaluronate in cultured skin fibroblasts and the culture medium,55 and hypoprolinemia as an incidental finding in one family32 are reported here.
In 1987, Machin et al.60 presented the postmortem findings from two young adults with CLS (a brother and sister whose clinical course had been described by Lowry et al.8) In 1988, there was a brief note about a third autopsy.25 The three autopsies are summarized in Table 2. These autopsy reports redirected attention to the first two boys1 described with this syndrome in 1966. Their medical records were retrieved, giving additional clinical information, and the results of both postmortem examinations, which are presented now.
CASE A
Case A has been previously described.1 The boy’s mother was short in stature and had severe headaches but was not retarded in development. Her face and hands were characteristic of the syndrome but less affected than those of her son. Other relatives seemed healthy and unimpaired. This boy was born normally after a normal pregnancy. Development was slow in infancy, rickets were suspected, and his face appeared unusual (Fig. 1). Speech was severely delayed. Because of insomnia and restless wandering, he was admitted at age 8 to an institution for the mentally retarded. He achieved an IQ of 54 at age 10 and 25 at age 18. He had the habit of eating large amounts rapidly. There were frequent falls, frequent respiratory infections, and one rectal prolapse. He was treated with phenytoin because of an abnormal electroencephalogram and with iodochlorhydroxyquin to prevent amebiasis.
Patient A: face at age 6 months, 4 years, 9 years, and 18 years; hand at 18 years; posture and profile at 19 years. Reproduced from Coffin et al.1 (Am J Dis Child 1966;112:205–213), copyrighted 1966, American Medical Association.
Physical examination at age 18 showed small size and quite a small head, cheerful behavior, some ability to see and hear, minimal speech in unrecognizable words and short sentences, stooped posture with flat feet, bent knees, head tilted to the right, a gait that was slow and shuffling and wide based, loose, stretchable skin with many scars, weak hypotonic muscles, lax joints but minimal contractures at elbows and wrists, eyes that showed ptosis of the upper lids and some choroidal atrophy, thicker facial features (Fig. 1) with very bushy and prominent brows and also several scars and dull swollen nasal mucosa, few teeth that were badly misaligned and carious with some incisors pointed, low systolic heart murmur, chest asymmetric and anteriorly convex, stiff back with kyphoscoliosis, large plum-soft hands with loose extensible joint, and tapered fingers.
X-rays showed retarded bone age. Terminal phalanges of the fingers had wide or tufted tips, giving a collar-button or drumstick appearance. Frontal sinuses were large and maxillary sinuses small. Vertebral bodies T10 to L3 had frayed or notched anterior surfaces and an anterior prominence at L3.
Laboratory findings showed that blood was O+. Blood levels of growth hormone were normal. Chromosome appeared normal. Amino acid studies were normal. Biopsy of subcutaneous tissue showed very few elastic fibers, and biopsy of bone showed wavy epiphyseal line and misalignment of chondrocytes.
After these studies, the case was published, and the boy remained in institutional care. A hematoma of the scalp was aspirated several times. At the age of 18.5 years, he was treated for 6 weeks for pneumonia with left pulmonary abscess. Fever and weakness continued, and he died at age 18.75.
At autopsy, the lungs were adherent to the chest wall. There was acute passive congestion, and alveoli and tissues were infiltrated by neutrophilic leucocytes. The visceral pleura was thickened, and in the left interlobar fissure, there was an abscess 9 cm in diameter, with some hemorrhage around it. There was a 3 cm abscess within the right middle lobe and smaller abscesses in the left diaphragm. The pulmonary arterial walls were thick. The heart was dilated, and there was a 1.5 cm atrial septal defect. The wall of the left ventricle was thickened, and there were evidences of acute myocarditis, previous inflammatory disease, and diffuse fibrosis. The spleen was large and lobulated, with enlarged lymph follicles, congested blood vessels, amyloid around some of the arteries, and a thickened serosal capsule. Vacuoles and granules were seen in the hepatic cells (not Kupffer cells), and there were lymphocytes in the portal zones. The kidneys showed passive congestion, but the lower urinary tract was normal. The testes were small. The stomach was normal. Sections of intestinal wall showed a chronic inflammatory reaction but intact nerve plexi. The pancreas contained a small region of necrosis and scar tissue. The adrenal cortices were small and the cells were atypical in shape and staining. The pituitary gland was normal. The thyroid gland showed great variation in the size of the follicles, with follicle-free zones of scarring and lymphoid tissue. Samples of the bones from costochondral junctions showed irregular or disorderly arrangement of chondrocytes.
The external appearance of the 1290 g brain was normal, except that the gyral pattern in the cingulate area was complex. The corpus callosum was normal. The cerebellum was small and showed a tonsillar pressure cone. There was moderate patchy gliosis and loss of Purkinje cells. The anterior ventricles were slightly dilated, and the pineal body was cystic. Groups of corpora amylacea were seen in the ependyma and pia. In the cerebral cortex, there was patchy loss of neurons in the third and fifth laminae and a few anoxic neurons. Neurons in all portions of the brain showed sparse cytoplasmic granular material and possibly normal lipochrome.
CASE B
This boy’s mother had severe headaches with emesis. She was moderately retarded in mental development and had the usual features of the CLS, including the tufted phalanges. The patient’s sister and half sister also had the usual features. His birth was normal, but at the age of 1 week he was readmitted to the hospital for laryngeal dyspnea and began observation for slow development, pectus excavatum, and rapidly enlarging head. He did not learn to speak. At age 2, he had typical facies (Fig. 2).
Patient B: face at age 2 years, 9 years, and 15 years; hand at 15 years; posture and profile at 15 years. Reproduced from Coffin et al.1 (Am J Dis Child 1966;112:205–213), copyrighted 1966, American Medical Association.
He was admitted to institutional care and achieved an IQ of 44 at age 2 and 20 at age 15. He was cheerful, friendly child, speechless but able to walk, see, and hear. He fell frequently and had frequent respiratory infections. He was treated with phenytoin and iodochlorhydroxyquin. His appearance changed through the years (Fig. 2). Because of loss of teeth, he took a very soft diet and ate large amounts rapidly. At age 14, he wandered about persistently shutting doors.
Physical examination at age 15.5 showed small size, large head, typical face and teeth, typical hands, pectus carinatum with kyphoscoliosis, lax skin, simian fold, hypothenar crease, palmar teeth, many scars, hypotonic weak muscles, lax joints, but flexion-contractures at wrists and elbows, flat feet with wide first toe-space, and clumsy gait.
X-rays showed retarded bone-age, thick calvarium, small paranasal sinuses, short, bifid, very prominent sternum, vertebral anomalies including midline defects in the neural arches T12 to S2, and anterosuperior notches in vertebral bodies T9 to S3 with beak-like anterior protrusions.
Laboratory tests gave many normal results: blood A+, chromosomes normal, amino-acid levels normal, tests for mucopolysaccharides negative, blood growth-hormone concentrations normal. Biopsy of bone showed irregular alignment of chondrocytes.
After these studies, his case was published,1 and he remained contented and comfortable in the institution. At age 18.33 he was found lying on the floor apneic and moribund, and he died soon afterward.
At autopsy (Table 1), the trachea and main bronchi were completely obstructed, and the stomach and esophagus were dilated with food. There was widespread emphysema and fibrosis of the lungs and some foci of lymphocytes consistent with chronic pulmonary disease and previous episodes of pneumonia. The heart showed spotty subendocardial fibrosis, focal myocardial scars, and myocardial ischemia. The central veins of the hepatic lobules were distended, with cloudy swelling of hepatic cells but no granules. The splenic blood vessels were engorged. Fibrosis was found in the pancreas. The thyroid, pituitary, and adrenal glands were not remarkable. The kidneys showed distention of vessels and glomeruli. The urinary tract appeared normal, and the prostate was quite small (other organs were not described).
The brain weighed 1340 g. The meninges were thickened at the vertex, and the brain itself was very rounded, with a simplified gyral pattern except for small anomalous foci of microgyria. Minimal cerebellar coning was noted. The corpus callosum was not remarkable. The cerebral cortex was thin, but the deep white matter was bulky, and the ventricles were small. The microscopic studies showed faulty cortical lamination and some ectopic neurons and immature fusiform neurons. Granulations were not mentioned, and there was no evidence of mucopolysaccharidosis. The autopsy diagnoses were asphyxia caused by aspiration of food, pulmonary emphysema and fibrosis with moderate chronic pneumonitis, multiple congenital anomalies, mental retardation, focal scars in the myocardium, and subendocardial fibroelastosis.
DISCUSSION
The history of the CLS is reviewed, and two autopsies are presented from the two first cases, which were published in 1966. The autopsy reports, summarized in Table 1, reiterate well-known features of the syndrome, including chronic lung disease and heart disease and two additional items of special interest: the irregularity of cell alignment at costochondral junctions, and, in one patient, the presence of granular deposits in hepatic cells and in a few cerebral neurons. Three autopsy reports had been published previously25,60 and are summarized in Table 2.
A comparison of these five cases emphasizes the great variation from patient to patient and the wide assortment of organs and tissues involved. The causes of death were varied but showed some similarities, including aspiration of food and intolerance of surgical procedures. The four brains that were examined showed dilation of the ventricles (3 of 4 cases), unusual patterns of gyri (3 of 4), faulty cortical lamination (3 of 4), abnormal appearance of cortical neurons (2 of 4), and thickened white matter (1 of 4). Unexpectedly, the corpora callosa were normal. The lungs showed emphysema (3 of 5 cases), scarring (4 of 5), vascular congestion (2 of 5), chronic infection (2 of 5), and in one case, fatal acute superinfection. In one case, the lungs seemed normal. In the heart, endocardial fibrosis was found in four of five cases, whereas myocarditis, mitral valve disease, tricuspid insufficiency, and atrial septal defect were found in one each and evidence of dilation hypertrophy or failure in three. In the skeleton, thickened calvaria were found in two patients, confirming earlier x-ray findings. In one patient, microscopic examination of bone showed irregularity of epiphyseal lines. Two cases, sister and brother, had diverticulae of the intestine and deterioration of the myenteric plexi, whereas two other patients had normal intestines, and one had chronic inflammation but intact plexi. In the liver, nodular cirrhosis and narrow bile ducts were found in one patient, who died in hepatorenal failure. Granules and vacuoles were found in hepatic cells of another, and “cloudy swelling” in hepatic cells of a third. Other organs were also abnormal: pancreatic scarring was found in two patients, cortical cysts of the kidneys in one, and amyloid deposits in the spleen of one. Scarring and lymphocytosis of the thyroid stroma were found. These autopsy findings and clinical findings do not include all of the anomalies found in CLS and do not exclude coincidental anomalies. However, the great variation from patient to patient and the wide variety of seemingly unrelated lessons in scattered organs imply a complex pattern of causation. Genetic research, which has been reported since the 1980s, may help to explain this pattern.
Molecular genetic studies of CLS have been reviewed.17,61 The gene for CLS has been located40,62–65 on the short arm of the X chromosome at band xp22.2, and the gene product is the enzyme Ribosomal S6 kinase or Rsk2.66 The gene works mainly by its influence on the activation of other genes, a pattern which could be called monopolygenic. In a healthy person, the normal enzyme Rsk2 cooperates with a growth factor to promote mitosis and activate genes.67,68 In a person with CLS, there is an anomaly at one of the many mutation sites61,66,72,77 along this gene locus that results in reduced activity of the enzyme61,70 with consequent curtailed expression of its targeted genes.
Because of these discoveries, there are now in vitro diagnostic tests for this syndrome17,68,72–75 and hopeful speculation about future pharmacotherapy.76 Also, the CLS, or Rsk2, gene has become a promising center of study of development. The gene and its enzyme appear to be associated with the action of insulin and the synthesis of glycogen,76 with responsiveness to salicylates and susceptibility to heat shock78 and with resistance to other stresses,78 and it may prove to be essential to the survival of cells.71 The most recent genetic studies are progressing by application of novel techniques, including the use of a knockout mouse that lacks a fully effective Rsk2 gene.61,69,76,78 Already, these studies are beginning to explain the wide variety of clinical and pathologic features of the Syndrome, the great variation between one affected person and another, and the overlapping features share by one developmental syndrome and another. Eventually, these studies may identify the target genes and processes and link each important feature of CLS with its genetic causes.
In future case reports, environmental influences should be considered in addition to the genetic background. Especially important are the effects of institutional care on the development of children, the effects of repeated injury, and the side effects of chronic medication. It is possible that these first two patients received enough phenytoin to modify their abilities and facial appearance.
References
Coffin GS, Siris E, Wegienka LC . Mental retardation with osteocartilaginous anomalies. Am J Dis Child 1966; 112: 205–213.
Martinelli B, Campailla E . Contributo alla conoscenza della sindrome di Coffin, Siris, Wegienka. G Psichiatr Neuropatol 1969; 97: 449–458.
Carpentier M . Le syndrome de Coffin. Thèse pour le doctorat en médecine [thesis]. Paris: Université René Descartes, 1972.
Procopis PG, Turner B . Mental retardation, abnormal fingers, and skeletal abnormalities: Coffin’s syndrome. Am J Dis Child 1972; 124: 258–261.
Coffin GS, Siris E . Soft hand syndrome [correspondence]. Am J Dis Child 1971; 122: 181.
Coffin GS, Siris E . Mental retardation with absent fifth fingernail and terminal phalanx. Am J Dis Child 1970; 119: 433–439.
Gorlin RJ . Lapsus-caveat emptor: Coffin-Lowry syndrome vs Coffin-Siris syndrome: an example of confusion confounded. Am J Med Genet 1981; 10: 103–104.
Lowry B, Miller JR, Fraser FC . A new dominant gene mental retardation syndrome. Association with small stature, tapering fingers, characteristic facies, and possible hydrocephalus. Am J Dis Child 1971; 121: 496–500.
Jammes J, Mirhosseini SA, Holmes LB . Syndrome of facial abnormalities, kyphoscoliosis, and severe mental retardation. Clin Genet 1973; 4: 203–209.
Hussels IE . The Coffin syndrome. Birth Defects Orig Artic Ser 1974; 10: 491–494.
De Marco P . Sindrome di Coffin, Siris e Wiegenka. Descrizione clinica di un caso. Neuropsichiat Infantil 1975; 171: 637–643.
Temtamy SA, Miller JD, Dorst JP et al. The Coffin-Lowry syndrome: a simply inherited trait comprising mental retardation, faciodigital anomalies and skeletal involvement. Birth Defects Orig Artic Ser 1975; 11: 133–152.
Temtamy SA, Miller JD, Hussels-Maumenee I . The Coffin-Lowry syndrome. An inherited faciodigital mental retardation syndrome. J Pediatr 1975; 86: 724–731.
Smith DW . Recognizable patterns of human malformation, 2nd ed. Philadelphia: W.B. Saunders, 1976.
Hersh JH, Weisskopf B, De Coster C . Forearm fullness in Coffin-Lowry syndrome: a misleading yet possibly early diagnostic clue. Am J Med Genet 1984; 18: 195–199.
Rosanowski F, Hoppe U, Proschel U, Eysholdt U . Late-onset sensorineural hearing loss in Coffin-Lowry syndrome. ORL J Otorhinolaryngol Relat Spec 1998; 60: 224–226.
Jacquot S, Merienne K, Trivier E, Zeniou M, Pannetier S, Hanauer A . Coffin-Lowry syndrome: current Status. Am J Med Genet 1999; 85: 214–215.
Hunter AG, Partington MW, Evans JA . The Coffin-Lowry syndrome. Experience from four centres. Clin Genet 1982; 21: 321–335.
Tonoki H, Tomita T, Ishikiriyama S et al. The Coffin-Lowry syndrome: Four new cases in three families. Acta Paediatr Jpn 1983; 17: 298–303.
Vles JS, Haspeslagh M, Raes MM, Fryns JP, Casaer P, Eggermont E . Early clinical signs in Coffin-Lowry syndrome. Clin Genet 1984; 26: 448–452.
Soekarman D, Fryns JP . Corpus callosum agenesis in Coffin-Lowry syndrome. Genet Couns 1994; 5: 77–80.
Plomp AS, De Die-Smulders CE, Meinecke P, Ypma-Verhulst JM, Lissone DA, Fryns JP . Coffin-Lowry syndrome: clinical aspects at different ages and symptoms in female carriers. Genet Couns 1995; 6: 259–268.
Sylvester PE, Rundle AT, Richards BW . The syndrome of Coffin, Siris, and Wegienka: Report of a case. J Ment Defic Res 1976; 20: 35–54.
Oguchi H, Oikawa K . Coffin-Lowry syndrome in 2 Brothers. Shoni Shikagaku Zasshi 1986; 24: 191–199.
Gilgenkrantz S, Mujica P, Gruet P, Tridon P, Schweitzer F, Nivelon-Chevallier A et al. Coffin-Lowry syndrome: a multicenter study. Clin Genet 1988; 34: 230–245.
Wilson WG, Kelly TE . Brief clinical report: early recognition of the Coffin-Lowry syndrome. Am J Med Genet 1981; 8: 215–220.
Kousseff BG . Coffin-Lowry syndrome in an Afro-American family. Am J Med Genet 1982; 11: 373–375.
Haspeslagh M, Fryns JP, Beusen L, Van Dessel F, Vinken L, Moens E et al. The Coffin-Lowry syndrome. A study of two new index patients and their families. Eur J Pediatr 1984; 143: 82–86.
Young ID . The Coffin-Lowry syndrome. J Med Genet 1988; 25: 344–348.
Iwasaki K, Tamura Y, Nishimura K, Sakai N, Miyagi A, Higaki M . A case suggesting Coffin-Lowry syndrome. Bull Kanagawa Dent Coll 1990; 18: 107–113.
Hartsfield JK, Hall BD, Grix AW, Kousseff BG, Salazar JR, Haufe SM . Pleiotropy in Coffin-Lowry syndrome: sensorineural hearing deficit and premature tooth loss as early manifestations. Am J Med Genet 1993; 45: 552–557.
Lacombe D, Parrot-Roulaud F, Castell JF, Serville F, Hehunstre JP, Battin J . Syndrome de Coffin-Lowry et hyperprolinémie. Arch Fr Pediatr 1993; 50: 489–492.
Fryns JP . Osteopenia, abnormal dentition, hydrops fetalis and communicating hydrocephalus: unusual early clinical signs in Coffin-Lowry syndrome. Clin Genet 1996; 50: 112.
Day P, Cole B, Welbury R . Coffin-Lowry syndrome and premature tooth loss: a case report. J Dent Child 2000; 67: 148–150.
Collacott RA, Warrington JS, Young ID . Coffin-Lowry syndrome and schizophrenia: a family report. J Ment Defic Res 1987; 31: 199–207.
Higashi K, Matsuki C . Coffin-Lowry syndrome with sensorineural deafness and labyrinthine anomaly. J Larnyngol Otol 1994; 108: 147–148.
Sivagamasundari U, Fernando H, Jardine P, Rao JM, Lunt P, Jayewardene SL . The association between Coffin-Lowry syndrome and psychosis: a family study. J Intellect Disabil Res 1994; 38: 469–473.
Vine DT, Gold JT, Grant AD . Etiology of the weakness in Coffin-Lowry Syndrome [abstract]. Am J Hum Genet 1986; 39: A85.
Fryns JP, Vinken L, Van den Berghe H . The Coffin syndrome. Hum Genet 1977; 36: 271–276.
Partington MW, Mulley JC, Sutherland GR, Thode A, Turner G . A Family with the Coffin-Lowry syndrome revisited: localization of CLS to Xp21-pter. Am J Med Genet 1988; 30: 509–521.
Proud VK, Levine C, Carpenter NJ . New X-linked syndrome with seizures, acquired micrencephaly, and agenesis of the corpus callosum. Am J Med Genet 1992; 43: 458–466.
Cheyette SR, Graf WD, Hoffman M . Hyperexplexia in Coffin-Lowry syndrome. Ann Neurol 1997; 42: 505.
Nakamura M, Yamagata T, Momoi M, Yamazaki T . Drop episodes in Coffin-Lowry syndrome: exaggerated startle responses treated with clonazepam. Pediatr Neurol 1998; 19: 148–150.
Crow YJ, Zuberi SM, McWilliam R, Tolmie JL, Hollman A, Pohl K et al. “Cataplexy” and muscle ultrasound abnormalities in Coffin-Lowry Syndrome. J Med Genet 1998; 35: 94–98.
Fryns JP, Smeets E . “Cataplexy” in Coffin-Lowry syndrome. J Med Genet 1998; 35: 702.
Caraballo R, Tesi Rocha A, Medina C, Fejerman N . Drop episodes in Coffin-Lowry syndrome: an unusual type of startle response. Epileptic Disord 2000; 2: 173–176.
Özden A, Dirik E, Emel A, Sevine N . Callosal dysgenesis in a patient with Coffin-Lowry syndrome. Indian J Pediatr 1994; 61: 101–103.
Della Cella G, Stagnaro MG, Beluschi C, Forni GI . Coffin-Lowry syndrome. Description of 2 cases associated with cardiovascular anomalies. Pediatr Med Chir 1987; 9: 229–232.
Krajewska-Walasek M, Kubicka K, Ryzko J . Cardiac involvement in Coffin-Lowry syndrome. Eur J Pediatr 1988; 147: 448.
Jones KL . Smith’s recognizable patterns of human malformation, 5th Edition. Philadelphia: W.B. Saunders, 1997.
Wiedemann HR, Kunze J . Clinic syndromes, 3rd ed. Saint Louis: Mosby-Wolfe, 1997.
Merchant RH . The Coffin-Lowry syndrome. A faciodigital mental retardation syndrome: a case report. Indian Pediatr 1976; 13: 247–249.
Barajas LO, Rivera H, Fragoso R, Nazara Z, Cantu JM . Coffin-Lowry syndrome. Description of two cases. Bol Med Hosp Infant Mex 1986; 43: 378–381.
Christodorescu D . Brief clinico-genic report: the Coffin-Lowry syndrome. Neurol Psychiatr 1987; 25: 211–213.
Miyazaki K, Yamanaka T, Oohira A . Enhanced accumulation of hyaluronate in the culture of skin fibroblasts from two patients with Coffin-Lowry syndrome. Tohoku J Exp Med 1989; 158: 325–334.
Miyazaki K, Yamanaka T, Ishida Y, Oohira A . Calcified ligamenta flava in a patient with Coffin-Lowry syndrome: biochemical analysis of glycosaminoglycans. Jinrui Idengaku Zasshi 1990; 35: 215–221.
Ishida Y, Oki T, Ono Y, Nogami H . Coffin-Lowry syndrome associated with calcium pyrophosphate crystal deposition in the ligamenta flava. Clin Orthop 1992; 275: 144–151.
Gorlin RJ, Brown D, Sauk J . Coffin-Lowry syndrome: a storage disorder? Birth Defects 1978; 14: 175.
Beck M, Glössl J, Rüter R, Kresse H . Abnormal proteodermatan sulfate in three patients with Coffin-Lowry syndrome. Pediatr Res 1983; 17: 926–929.
Machin GA, Walther GL, Fraser VM . Autopsy findings in two adult siblings with Coffin-Lowry syndrome. Am J Med Genet 1987; 3(suppl): 303–309.
Delaunoy JP, Abidi F, Zeniou M, Jacquot S, Merienne K, Pannetier S et al. Mutations in the X-linked RSK2 gene (RPS6KA3) in patients With Coffin-Lowry syndrome. Hum Mutat 2001; 17: 103–116.
Hanauer A, Alembik Y, Gilgenkrantz S, Mujica P, Nivelon-Chevallier A, Pembrey ME et al. Probable localisation of the Coffin-Lowry locus in Xp22.2-p22.1 by multipoint linkage analysis. Am J Med Genet 1988; 30: 523–530.
Biancalana V, Briard ML, David A, Gilgenkrantz S, Kaplan J, Mathieu M et al. Confirmation and refinement of the genetic localization of the Coffin-Lowry syndrome locus in Xp22.1-p22.2. Am J Hum Genet 1992; 50: 981–987.
Biancalana V, Trivier E, Weber C, Weissenbach j, Rowe PS, O’Riordan JL et al. Construction of a high-resolution linkage map for Xp22.1-p22.2 and refinement of the genetic localization of the Coffin-Lowry syndrome gene. Genomics 1994; 22: 617–625.
Bird H, Collins AL, Oley C, Lindsay S . Crossover analysis in a British family suggests that Coffin-Lowry syndrome maps to a 3.4 cM interval in Xp22. Am J Med Genet 1995; 59: 512–516.
Trivier E, De Cesare D, Jacquot S, Pannetier S, Zackai E, Young I et al. Mutations in the kinase Rsk-2 associated with Coffin-Lowry syndrome. Nature 1996; 384: 567–570.
De Cesare D, Jacquot S, Hanauer A, Sassone-Corsi P . Rsk-2 activity is necessary for epidermal growth factor-induced phosphorylation of CREB protein and transcription of c-fos gene. Proc Natl Acad Sci U S A 1998; 95: 12202–12207.
Merienne K, Jacquot S, Trivier E, Pannetier S, Rossi A, Schinzel A et al. Rapid immunoblot and kinase assay tests for a syndromal form of X-linked mental retardation: Coffin-Lowry syndrome. J Med Genet 1998; 35: 890–894.
Blair HJ, Gormally E, Uwechue IC, Boyd Y . Mouse mutants carrying deletions that remove the genes mutated in Coffin-Lowry syndrome and lactic acidosis. Hum Mol Genet 1998; 7: 549–555.
Sassone-Corsi P, Mizzen CA, Cheung P, Crosio C, Monaco L, Jacquot S et al. Requirement of Rsk-2 for epidermal growth factor-activated phosphorylation of histone H3. Science 1999; 886–891.
Nebreda AR, Gavin AC . Cell survival demands some risk. Science 1999; 286: 1309–1310.
Manouvrier-Hanu S, Amiel J, Jacquot S, Merienne K, Moerman A, Coeslier A et al. Unreported RSK 2 missense mutation in two male sibs with an unusually mild form of Coffin-Lowry syndrome. J Med Genet 1999; 36: 775–778.
Hanauer A . CLS Testing Costs. CLSF News 2000; 9: 7.
Jacquot S, Merienne K, De Cesare D, Pannetier S, Mandel JL, Sassone-Corsi P et al. Mutation analysis of the RSK-2 gene in Coffin-Lowry patients; extensive allelic heterogeneity and a high rate of de novo mutations. Am J Hum Genet 1998; 63: 1631–1640.
Harum KH, Alemi L, Johnston MV . Cognitive impairment in Coffin-Lowry syndrome correlates with reduced RSK-2 activation. Neurology 2001; 56: 207–214.
Dufresne SD, Bjorbaek C, El-Haschimi K, Zhao Y, Aschenbach WG, Moller DE et al. Altered extracellular signal-regulated kinase signaling and glycogen metabolism in skeletal muscle from p90 Ribosomal S6 kinase 2 knockout mice. Mol Cell Biol 2001; 21: 81–87.
Abidi F, Jacquot S, Lassiter C, Trivier E, Hanauer A, Schwartz CE . Novel mutations in Rsk-2, the gene for Coffin-Lowry syndrome (CLS). Eur J Hum Genet 1999; 7: 20–26.
Wang X, Asea A, Xie Y, Kabingu E, Stevenson MA, Calderwood SK . RSK2 represses HSF 1 activation during heat shock. Cell Stress Chaperones 2000; 5: 432–437.
Zeniou M, Pennetier S, Fryns JP, Hanauer A . Unusual splice-site mutations in the RSK2 gene and suggestion of genetic heterogeneity in the Coffin-Lowry syndrome. Am J Hum Genet 2002; 70: 1421–1433.
Touraine RL, Zeniou M, Hanauer A . A syndromic form of X-linked mental retardation: the Coffin-Lowry syndrome. Eur J Pediatr 2002; 161: 179–187.
McCandless SE, Schwartz S, Morrison S, Garlapati K, Robin NH . Adult with an interstitial deletion of chromosome 10 [del (10) (q25.1-q25.3)]: overlap with Coffin-Lowry syndrome. Am J Med Genet 2000; 95: 93–98.
Kondoh T, Takano J, Sugawara H, Ida T, Harada N, Matsumoto J et al. Clinical manifestations of Coffin-Lowry syndrome associated with de novo 8p23 duplication. Am J Hum Genet 2001; 69(suppl): 293.
Concannon N, Hegarty AM, Stallings RL, Reardon W . Coffin-Lowry phenotype in a patient with a complex chromosome rearrangement. J Med Genet 2002; 39: E41.
Author information
Authors and Affiliations
ADDENDUM
ADDENDUM
Since acceptance of this paper, surveys of CLS79,80 showed only a minority of subjects to have a mutation of the RSK-2 gene. Moreover, one patient with CLS81 had interstitial deletion of chromosome 10, another82 had a duplication of 8p23, and another83 case showed multiple translocations involving chromosomes 2, 3, 7, and 11. Determination of serum Rsk2 might help to explain such cases.
Rights and permissions
About this article
Cite this article
Coffin, G. Postmortem findings in the Coffin-Lowry Syndrome. Genet Med 5, 187–193 (2003). https://doi.org/10.1097/00125817-200305000-00011
Issue Date:
DOI: https://doi.org/10.1097/00125817-200305000-00011