Abstract
Purpose: The study goals were to (1) determine the proportion of unselected individuals at increased risk for diseases with known genetic components and (2) compare the documentation and quality of risk assessment between a questionnaire, a pedigree interview, and chart review.
Methods: Seventy-eight patients seen in a division of internal medicine were randomized into two groups, which completed a questionnaire or underwent a pedigree interview. Chart notes were compared to both study tools.
Results: Sixty-two (79.5%) of the 78 participants scored at increased risk for at least one category. Either of the two study tools found significantly more people at high risk (48/78, 61.5%) than the chart review (31/78, 39.7%) (P = 0.01).
Conclusions: Approximately 20% of patients in an unselected internal medicine practice were at an increased risk that was not documented in reviewed chart notes. Targeted family history analysis reveals patients who require increased medical surveillance, preventive measures, or genetic counseling/testing.
Similar content being viewed by others
Main
Medical genetics isn’t what it used to be and it never will be again.1
In the past, clinical genetics has served a minority of the general population, dealing mostly with rare conditions, providing preconception or prenatal counseling for couples, or working with families affected by rare pediatric or adult-onset genetic diseases, such as Huntington disease.2 Genetic medicine has recently begun to enter the realm of primary care, with the increasing availability of predictive testing for specific cancer-predisposing syndromes, population-based carrier screening, and the molecular diagnosis of common recessive disorders such as hemochromatosis.1–2 It has long been known that several common diseases of adulthood arise from complex genetic and environmental interactions. The newly published map of the human genome will accelerate the pace of gene discovery related to the etiology of common complex diseases, such as diabetes, atherosclerosis, and Alzheimer disease, moving medical genetics even further into mainstream medicine.2–3
Research indicates that primary care physicians and other nongenetic specialists have a lack of knowledge, understanding, and interest in medical genetics.4–9 Many physicians report little training in genetics; they are uncomfortable providing genetic counseling and wary of interpreting genetic test results.7 For example, in a review of the medical records of patients who underwent testing of the APC gene for familial adenomatous polyposis, fewer than 20% of the patients were provided pretest genetic counseling and the physician’s interpretation of the genetic test results was incorrect in 31.6% of the cases.5 As similar predictive tests become available for common diseases, more patients will seek genetic services from their primary care providers. Emery and Hayflick2 suggest that this impending demand for genetic services could be met if specific elements of genetic medicine are incorporated into primary care. These elements would include recognition of common genetic disorders, collaboration between primary care providers and genetic specialists in the long-term care of patients with a genetic disease, and appropriate referral of those in need of genetic services.
One of the most effective measures of a person’s risk for a genetic disease is analysis of his or her family medical history. The family history, or pedigree, has long been the backbone of a clinical genetic visit. It contributes to making a diagnosis, determining risk, and assessing the needs for patient education and psychosocial support.10 However, a three-generation pedigree with subsequent family history analysis is usually reserved for patients referred to genetic clinics. Research on pedigree analysis in unselected patient populations has shown that pedigrees often reveal additional, previously unidentified genetic risk factors.11–13 In an unselected reproductive setting and self-selected primary care setting, 10% to 40% of included patients were identified to have additional genetic risk factors, for which molecular testing was often available.12–13 This suggests that personal and family medical history can serve as a cost-effective, population-based screening tool for genetic risk and will allow patient-tailored care when genetic risk factors are revealed prior to conception or development of disease.11 In addition to detecting increased risk for mendelian conditions, the family history can also indicate genetic risk factors for common adult diseases, particularly for specific cancers, including breast, ovarian, and colorectal cancer.11 A “mild” family history (e.g., a single first-degree relative affected at a younger than average age of onset) can moderately increase an individual’s risk for one of these diseases by two to five times the general population risk, while a stronger family history indicative of a dominantly inherited predisposition may make an individual’s risk for disease 50% or more.14 Information gained through the family history can then be applied to decisions regarding potential genetic testing, surveillance, and prophylactic treatments. In many cases, screening based on family history and appropriately tailored treatment for many of these disorders is available, and when applied to a patient’s care, it can significantly reduce the occurrence of premature illness and death.15 For example, family history information about thromboembolic disease is a good predictor for the factor V Leiden mutation and other related coagulation factors, and it may alter health care management.16,17 Failure to identify clinically significant family histories denies patients access to specialty services for people who are at risk or affected by a disease with genetic components.18 In addition, overlooking other at-risk relatives limits this tool’s potential benefits and impact on public health.
While the family history as a screening tool for adult-onset disease has been demonstrated to be effective, limited training and clinical time significantly impede the routine use of a comprehensive three-generation pedigree in internal medicine clinics.2,11,19 However, the potential role of primary care practitioners to incorporate genetic services has been demonstrated in population-based screening for common recessive disorders such as Tay Sachs disease in the Ashkenazi Jewish population.16 It is likely that family history analysis will become a crucial means of risk assessment in primary care practices.1–2 The family history may be used to determine when referrals for genetic testing, increased surveillance, and tailored disease therapy would be medically appropriate.1–3,19 However, neither the percentage of high-risk patients in an unselected internal medicine practice nor the quality of risk assessment as gathered by an internist compared with a genetic counselor have been examined. We studied an unselected academic internal medicine population and compared risk assessments from (1) a newly developed questionnaire and (2) a three-generation pedigree generated and interpreted by genetics professionals, versus (3) previously documented chart information. We then determined the differences in referrals and health care recommendations that could be generated from each approach.
METHODS
Subjects
The subjects were 78 male and female patients, aged 18 years or older, who were seen for a return visit at the Northwestern Medical Faculty Foundation Division of Internal Medicine between December 2001 and May 2002. Pregnant women and patients with cognitive deficits were excluded. Participants were alternately assigned to Group A or Group B.
Screening tools
Participants in Group A (n = 39) were provided a questionnaire that elicits family history information, with special attention to known mendelian disorders and common diseases of adulthood including cardiovascular disease, non–insulin-dependent diabetes mellitus (NIDDM), specific cancers, and thromboses (available upon request from T.M.F.). Reproductive risks were assessed if the subject indicated plans to have biological children in the next 5 years.
Group B participants (n = 39) were privately interviewed by a genetic counseling intern (T.M.F.), who created a three-generation pedigree (four-generation pedigree if the participant had children). The pedigree interviews were documented according to the specifications depicted by Bennett20 in a manner that allowed follow-up questions and clarifications of vague diagnoses. Upon completion of each pedigree drawing, specific symptoms and diseases were reviewed for comprehensive evaluation of categories under study, including diabetes, cardiovascular disease, cancer, strokes, thromboembolic events, mental retardation, and reproductive plans.
A template for measuring level of risk (high, moderate, and low risk) based on family history was designed based on related literature, consensus statements, and current practice guidelines (Appendix). This template determined status in nine risk categories: (1) mendelian conditions, (2) coronary artery disease (CAD), (3) NIDDM, (4) breast/ovarian cancer, (5) prostate cancer, (6) colon cancer, (7) predisposition to thrombosis, (8) ethnicity-based carrier screening, (9) factors that may affect reproductive success. The adult-onset disease categories (2–7) were chosen on the basis of their frequency and practice guidelines and because increased surveillance and preventive counseling may prevent disease or premature mortality in genetically susceptible individuals. Reproductive genetic concerns (categories 8 and 9) were included for those individuals who reported desiring pregnancy in the next 5 years, since genetic evaluation is important for both members of a prenatal couple, implying that reproductive assessment could also be within the purview of primary care practitioners.
Both a board-certified genetic counselor (K.E.O.) and a board-certified medical geneticist (W.S.R.) reviewed the collected information according to the above methods to generate an interpretation of genetic risk and health care recommendations as described in the Appendix. Unless participants explicitly declined (n = 2), recommendations based on this information were sent in a letter to the participant’s primary care provider following participation in this study.
For participants in both groups, a subsequent review of the participant’s medical records was used to gather family history information previously elicited by the participant’s physician(s). The reviewed medical records were generated by attending physicians in a single academic practice. This information was applied to the same scoring measure to compare it with the data obtained directly from participants. Based on the documented family history data available from the medical record, it was recorded whether or not the data available from the participant’s chart would produce similar health care recommendations as the data gathered by the research tools.
The Northwestern University Institutional Review Board approved the study’s recruitment methods, questionnaire, risk assessment tools, and protocol.
Data analysis
For each participant, family history data were analyzed to classify risk assessment (low, moderate, high) in each disease category, using the previously described scoring measure. Data analysis was performed with SPSS 10.0 for Windows, Student Version (2001).33 Demographic information was quantified and compared as well. Linear discriminant analysis was used to predict group membership based on potential confounding variables, such as gender, anxiety, and reason for the current physician visit, to ensure random group assignment. This analysis was performed with the assumption of equal prior probabilities for all groups. In addition, cross-validation was performed to evaluate classifier performance. Results showed that 53.8% of participants were correctly classified in comparison with the 50% random assignment expected by chance. These data indicate no significant differences between the two groups (P = 0.74).
The number of individuals identified at an increased risk in each category was documented for each intervention (questionnaire and pedigree) and compared to the medical record chart review. The total number of at-risk individuals recognized by a study tool was compared to those who would have been identified through chart review. This internal comparison was used to demonstrate the number of at-risk individuals potentially identified by a genetics professional compared with those presumably recognized by an internist. Chi-square contingency statistics were performed on this comparison.
The prevalence of individuals at an increased risk specifically for an adult-onset disease identified by each study tool was compared to risk category assignment made possible from review of information in the participants’ charts. These totals were compared using χ2 contingency statistics.
RESULTS
Family history analysis was performed on 78 participants in this study, including 39 participants in Group A (questionnaire) and 39 participants in Group B (pedigree). The average time for questionnaire completion was 8.1 (±2.9) minutes, and the average time required for the pedigree interview was 17.1 (±7.5) minutes. Both study tools were scored using the same scoring template (Appendix). Scoring of the questionnaire generally required less time than that of the pedigree.
Charts were requested for all participants in order to compare the family history information acquired through the study tools to the family history information that is documented in each participant’s chart. Data analysis was performed using these charts as an internal control for 78 study participants.
Demographic characteristics of the 78 participants are described in Table 1. There were no significant differences between Groups A and B with regard to age, gender, race, reason for appointment, or self-reported anxiety. The range of ages was 21 to 76 years. Of the 78 cases analyzed 29 (37.2%) were male, with an average age of 44.6 years (±14.1); 49 (62.8%) were female with an average age of 41.6 years (±12.6).
Documentation of individuals at increased risk
Sixty-two (79.5%) of the 78 participants scored at increased risk for at least one of the nine categories assessed; the most commonly reported disorder was CAD. Table 2 describes the risk assessment made by each study tool compared to that of the chart review for each condition evaluated (mendelian conditions were excluded from the table; the eight categories listed are those in which specific preventive recommendations can be made). In addition to the diseases listed in Table 2, one individual from Group A was found to be at a moderately increased risk for prostate cancer. No individuals from review of Group A’s medical records were assigned an increased level of risk for this disease. No individuals from Group B were found to be at increased risk for prostate cancer, through pedigree analysis or chart review. One participant reported a family history of a known mendelian disease (a cousin who tested positive for a BRCA1 or BRCA2 mutation). Five participants from Group A and 10 participants from Group B had family histories suggestive of a single-gene disorder that would warrant further investigation. These included family members affected with NIDDM, CAD, or autoimmune disease that seemed to segregate in an autosomal dominant pattern. In addition, one participant reported a sibship in which all four members had open-angle glaucoma, but neither parent was affected; this history suggests an autosomal recessive disease. Two participants in Group A were themselves affected with mendelian disorders: hereditary hemochromatosis and polycystic kidney disease. Two additional participants in Group A reported that their reproductive partner had a mendelian condition—Charcot-Marie-Tooth disease and hemophilia—directly affecting these participants’ reproductive risks and indicating further evaluation for their children.
While many individuals were found to be at increased risk for just one disease category (28, 35.9%), a high percentage of individuals were at risk for more than one condition: 19 (24.4%) in two disease categories; 10 (12.8%) in three disease categories; 4 (5.1%) in four disease categories; and 1 individual (1.3%) was at increased risk in five disease categories. Only 12 (15.4%) participants did not score at an increased risk level for any of the categories assessed. The remaining four individuals were already affected with at least one of the diseases under evaluation and did not score at an increased risk for any of the remaining disease categories. The level of anxiety reported by the participant did not significantly correlate with the number of conditions for which he/she was found to be at increased risk.
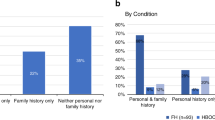
Comparison of study tools to chart documentation
The study groups were combined to demonstrate the prevalence of unselected individuals with an increased risk for adult-onset conditions with known genetic components in an internal medicine practice. Table 3 documents the number of individuals identified at moderate and high risk by both interventions compared to chart review. The prevalence of individuals at an increased risk for an adult-onset disease (CAD, NIDDM, the cancers, and thromboembolic disease) identified by each study tool was compared to risk category assignment made possible from review of information in the participants’ charts. All of the individuals who were found to be at an increased risk for one of the evaluated categories by review of their medical records were also captured by one of the study tools. Group A’s questionnaires revealed a total of 32 individuals at an increased risk for one or more diseases, compared with 18 who were identifiable through chart review. Group B’s pedigree analysis revealed a total of 30 individuals at an increased risk for one or more diseases, compared with 15 who were identifiable through chart review. When combined, a total of 48 (61.5%) individuals were identified to be at an increased risk for an adult-onset disease by one of the study tools, compared with 31 (39.7%) individuals identifiable through chart review (χ2, P = 0.010, df = 1). While difference in ability to identify these individuals between Group A and the chart review was not significant, the difference between Group B and the chart review was (χ2, P = 0.023, df = 1). The difference in identifying any risk factor using either of the study tools versus the chart review was significant (χ2, P = 0.010, df = 1).
With regard to the characterization as moderate or high, 11 participants who scored at a moderately increased risk based on their chart information were found to be at a highly increased risk by one of the study tools. Specifically, participants’ medical records were better at identifying their risk for CAD and NIDDM than for the various cancers, thromboembolic disease, population-based carrier screening, and other reproductive risks.
DISCUSSION
This study demonstrates that a majority of unselected patients in this internal medicine practice have one or more significant genetic risk factors for which preventive medical recommendations are available. In addition, the results of this investigation indicate that the prevalence of patients at an increased risk for diseases with known genetic components in an internal medicine practice is substantially higher than appreciated by current medical documentation. A targeted review of the genetic family history, through either questionnaire or interview methodology, can provide more accurate risk stratification for common, adult-onset genetic disorders and identify patients in need of increased screening or surveillance, further genetic counseling, and/or further genetic testing.
Patient and physician awareness of an increased risk for a preventable disease provides the opportunity to counsel a patient about lifestyle modifications or surveillance that may potentially decrease the risk of disease.34 Several studies suggest that for individuals at high risk, family-targeted screening and treatment has the potential to significantly reduce the occurrence of premature illness and could have a significant impact on public health.11,15 In the model of preventive medicine, genetic information can potentially produce reduction of disease and suffering by targeting prevention, screening, and modifiable risk factors according to each person’s unique biological susceptibilities.35 Such evidence suggests that documentation of the medical family history is a crucial part of any preventive health care risk assessment. While each individual reacts differently to learning about increased risks, some studies suggest that a person who is made aware of his or her inherited risk factors is more likely to comply with preventive recommendations.36
Therefore, we suggest that documentation and risk assessment of a thorough family history, including information regarding common chronic diseases of adulthood, should be a component of any medical practice aimed at the prevention of disease. An approach for risk stratification based on family history can impact a significant proportion of the population.11,36 Identification of high-risk families and individuals can allow behavior modification and preventive interventions for adult-onset disease. For example, it has been shown that individuals with a family history of cardiovascular disease are more susceptible to the harmful effects of smoking than those without a positive family history.37 These factors signify that individuals identified through family history analysis can benefit from preventive interventions.11,15,36,37
This study provides new evidence regarding the family history-taking practice of internists compared to a genetic counselor and to a family history questionnaire designed and interpreted by a genetics professional. The medical literature supports our finding that genetics-oriented questionnaires or pedigrees detect a higher proportion of patients at increased genetic risk than is customarily documented in medical records. A recent study that retrospectively compares the genetic risk assessment provided by an obstetrician with that of a genetic counselor found that a genetic counselor’s risk assessment identified additional risks for genetic disorders in 38% (55/145) of prenatal genetics patients.8 In a similar population, Scheuner et al.11 found that 42.5% (170/400) of patients referred for prenatal genetic counseling had a positive family history for adult-onset diseases with a known genetic component. Finally, Sweet et al.9 found similar discrepancies between oncologists’ documentation of family history and a computerized family history risk assessment tool for cancer. A large proportion of these patients had inadequate documentation of their family history of cancer, and 16% of the participants had a personal or family history suggestive of a hereditary cancer syndrome. These findings demonstrate that incorporating a genetic counselor and a three-generation pedigree into a patient’s risk assessment significantly improves detection of identifiable genetic risk factors.8 It is not clear from our study data, however, whether the incorporation of a study tool without a genetics professionals’ interpretation would provide the same benefit and increase in detection of high-risk families.
We found that when all participants were combined, the risk assessment generated by either of the two screening tools implemented in this study was better at revealing familial risk factors for disease than a review of the family history information documented by internal medicine providers. However, barriers such as time, training, comfort, knowledge, and resources have historically been an impediment in the integration of genetic services in primary care medicine.2,4,6 Use of a fast and effective screening tool to determine a population worthy of further evaluation may facilitate utilization of genetic services by internal medicine providers; a family history questionnaire with a simple scoring measure would meet such needs. Anecdotally, participants found it mostly straightforward and were able to complete it quickly (averaging 8.1 minutes). In addition, scoring the questionnaire was typically faster than scoring the pedigree. In contrast, the pedigree interview allows for thorough descriptions, clearer documentation, and follow-up questioning. The interviews were conducted according to the standards described by Bennett,20 allowing for clarification and adjustment based on the participant’s information more so than the questionnaire. However, this analysis is time- and labor-intensive, with an average of 17.1 minutes spent with each individual in Group B, and it required a longer amount of time for review and scoring.
It is important to point out that while most of the medical records reviewed in this study contained relevant family history information, accurate risk stratification was not always possible because of a lack of comprehensive detail. Increases in risk for familial diseases are associated with an increasing number of affected relatives, as well as with premature ages of disease onset.14 Documentation of age at diagnosis in affected relatives and information on second-degree relatives were missing in most patients’ charts. It may be that primary care physicians use the family history information only to support a suspected diagnosis, rather than as a predictive tool for assessing the risk of adult-onset disease.38 Several additional explanations may also account for the discrepancy between chart documentation of family history and that generated by either genetics tool: patients may withhold family history information from their physicians, fearing documentation of genetic risks in their medical records; patients may share genetic information with their physicians, but request that the information not be documented, for fear of discrimination or other reasons; or physicians may not be asking specific enough questions regarding their patients’ family history and/or documenting the patients’ replies. For example, one participant in this study discussed a family history of a genetic disease that places her at a significantly increased risk for cancer; there was no documentation of such information in this participant’s chart. The study tools were able to capture all at-risk individuals revealed by chart review. A key difference between risk analysis was that the study tools provided more detailed information, permitting stratification of risk into high and moderate, whereas many of the charts were not as comprehensive. Several participants who scored at a moderately increased risk based on their chart information were found to be at a highly increased risk by one of the study tools.
An interesting finding was that the participant’s medical records were better at identifying their risk for CAD and NIDDM than for the various cancers, thromboembolic disease, population-based carrier screening, and other reproductive risks. It may be that internists are accustomed to screening for heart disease and diabetes and therefore ask (or perhaps document) related family history information for these conditions more frequently than for the other categories assessed in this study.
An important limiting factor that may have affected the outcome of this study is that the data used for analysis are based on the participants’ recall of family disease rather than medical documentation. Another potential bias would occur if people concerned with their family history of disease were more likely to participate in the study; however, participant-reported anxiety level did not significantly correlate with the number of increased-risk categories identified in each patient, making this circumstance less likely. In addition, some participants (approximately four) scored at increased risk for more than one category based on the report of a single occurring diagnosis. For example, one woman reported that a first cousin was a positive carrier of a BRCA1 or BRCA2 mutation; therefore, this woman scored at an increased risk for a mendelian disorder as well as for breast cancer. While such occurrences may have increased the number of risk categories for a few participants, their significance is probably negligible. The population that participated in this study was remarkably diverse in race, age, and gender. The random assignment of participants to Group A and Group B was based purely on alternating participant numbers. The groups were not matched for any demographic features. The randomization of participants should minimize this study’s biases.
Further studies researching the role of the family history in general medicine would be valuable. This study was based on a relatively small number of participants, and both the chart review and obtaining of family history by pedigree were performed by the same investigator, which may have biased the scoring to some degree. Clearly, larger participant populations examined using blinded methodology may be more generalizable. It would be interesting to determine whether a larger number of participants would strengthen or weaken the trends noted in this study, such as the incidence of genetically based disease in an internal medicine practice’s population and the lack of comprehensive documentation in these patients’ medical records.
The development of a tool that is amenable to primary care practitioners, with clear history-taking recommendations, risk categorization assignment, and referral guidelines for genetic risk factors, would be indispensable. Genetics professionals will be invaluable in designing and implementing such a tool in the practice of internal medicine.
CONCLUSIONS
Family history collection in the internal medicine clinic can reveal previously unknown risk factors for the patient and may result in important changes in the health care and surveillance of the patient and his or her family members. The integration of genetics into primary care has already begun; it requires the incorporation of more genetics professionals in primary care medicine, along with further education and referral guidelines for nongenetics professionals to facilitate this process and prepare primary care practitioners for the future implications that the “new genetics” will have on public health.2 Genetic services will become an integral component of health care and preventive medicine, as genetic risk factors become better understood and interventions to reduce risk become available.6,36 Use of the genetic pedigree in place of conventional medical history-taking in primary care should be considered.36 Family history evaluation reveals risk factors for the patient and may provide important implications for his or her family members, potentially providing a significant impact on the preventive practice of public health.16,20,36 Further research and education on the benefits of comprehensive family history analysis will facilitate its incorporation into the practice of general preventive medicine.
References
Guttmacher AE, Jenkins J, Uhlman WR . Genomic medicine: who will practice it? A call to open arms. Am J Med Genet 2001; 106: 216–222.
Emery J, Hayflick S . The challenge of integrating genetic medicine into primary care. BMJ 2001; 322: 1027–1030.
Greendale K, Pyeritz RE . Empowering primary care health professionals in medical genetics: How soon? How fast? How far? Am J Med Genet 2001; 106: 223–232.
Hofman KJ, Tambor ES, Chase GA, Geller G, Faden RR, Holtzman NA . Physician’s knowledge of genetics and genetic tests. Acad Med 1993; 68: 625–632.
Giardiello FM, Brensinger JD, Petersen GM, Luce MC, Bacon JA, Booker SV et al. The use and interpretation of commercial APC testing for familial adenomatous polyposis. N Engl J Med 1997; 336: 823–847.
Hayflick SJ, Eiff MP, Carpenter L, Streinberger J . Primary care physicians’ utilization and perceptions of genetics services. Genet Med 1998; 1: 13–21.
Fetters MD, Doukas DJ, Dinh Phan KL . Family physicians’ perspectives on genetics and the Human Genome Project. Clin Genet 1999; 56: 28–34.
Koscica KL, Canterino JC, Harrigan JT, Dalaya T, Ananth CV, Vintzileos AM . Assessing genetic risk: comparison between the referring obstetrician and genetic counselor. Am J Obstet Gynecol 2001; 185: 1032–1034.
Sweet KM, Bradley TL, Westman JA . Identification and referral of families at high risk for cancer susceptibility. J Clin Oncol 2002; 20: 528–537.
Schuette JL, Bennett RL . Lessons in history: obtaining the family history and constructing a pedigree. In: Baker DL, Schuette JL, Uhlmann WR, editors. A guide to genetic counseling. New York: Wiley-Liss, 1998: 28–50.
Scheuner MT, Wang SJ, Raffel LJ, Larabell SK, Rotter JI . Family history: a comprehensive genetic risk assessment for the chronic conditions of adulthood. Am J Med Genet 1997; 71: 315–324.
Rose P, Humm E, Hey K, Jones L, Huson SM . Family history taking and genetic counselling in primary care. Fam Pract 1999; 16: 78–83.
Meschede D, Albersmann S, Horst J . The practical importance of pedigree analysis in women considering invasive prenatal diagnosis for advanced maternal age or abnormal serum screening tests. Prenat Diagn 2000; 20: 865–869.
King RA, Rotter JI, Motulsky AG, editors. The genetic basis of common diseases. New York: Oxford University Press, 1992.
Lubin MB, Lin HJ, Vadheim CM, Rotter JI . Genetics of common diseases of adulthood: implications for prenatal counseling and diagnosis. Clin Perinatol 1990; 17: 889–910.
Emery J, Rose P . Expanding the role of the family history in primary care. Br J Gen Pract 1999; 49: 260–261.
Grody WW, Griffin JH, Taylor AK, Korf BR, Heit JA . American College of Medical Genetics consensus statement on factor V Leiden mutation testing. Genet Med 2001; 3: 139–148.
Donnai D, Kerzin-Storrar LK, Craufurd D, Evans G, Clayton-Smith J, Kingston H . Genetic counsellors could be based in genetic centres but be formally linked to general practices. BMJ 2000; 321: 241–242.
Emery J, Watson E, Rose P, Andermann A . A systematic review of the literature exploring the role of primary care in genetic services. Fam Pract 1999; 16: 426–445.
Bennett RL . The practical guide to the genetic family history. New York: Wiley-Liss, 1999.
Offit K . Clinical cancer genetics. New York: Wiley-Liss, 1998.
American Diabetes Association. Position statement on screening for diabetes. Diabetes Care 2002; 25: 521–524.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. National Cholesterol Education Program’s ATP III Guidelines (2001). JAMA 2001; 285: 2486–2497.
Burk W, Daly M, Garber J, Botkin J, Kahn MJ, Lynch P et al. Recommendations for follow up care of individuals with an inherited predisposition to cancer, II: BRCA1 and BRCA2. Cancer Genetics Consortium. JAMA 1997; 277: 997–1003.
American Cancer Society. American Cancer Society guidelines for the early detection of breast cancer: update 1997. CA Cancer J Clin 1997; 47: 150–153.
American Cancer Society. Recommendations from the American Cancer Society Workshop on Early Prostate Cancer Detection, May 4–6, 2000 and ACS Guideline on testing for early prostate cancer detection: update 2001. CA Cancer J Clin 2001; 51: 39–44.
American Gastroenterological Association. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 1997; 112: 594–642.
Grody WW, Cutting GR, Klinger KW, Richards CS, Watson MS, Desnick RJ . Laboratory standards and guidelines for population-based cystic fibrosis carrier screening. Genet Med 2001; 3: 149–154.
American College of Obstetricians and Gynecologists. Screening for Tay-Sachs disease. ACOG Technical Bulletin No. 162. Washington, DC: American College of Obstetricians and Gynecologists, 1995.
American College of Medical Genetics. Position statement on carrier testing for Canavan disease. Bethesda, MD: American College of Medical Genetics, 1998.
American College of Obstetricians and Gynecologists. Genetic screening for hemoglobinopathies. ACOG Technical Bulletin No. 238, July 2000. Int J Gynaecol Obstet 2001; 74: 309–310.
American College of Obstetricians and Gynecologists. Antenatal diagnosis of genetic disorders. ACOG Technical Bulletin No. 188. Washington, DC: American College of Obstetricians and Gynecologists, 1987.
SPSS 10.0 for Windows, Student Version, 2001.
Matzen RN, Lang RS, editors. Clinical preventive medicine. Chicago: Mosby, 1998.
Khoury MJ . Relationship between medical genetics and public health: changing the paradigm of disease prevention and the definition of a genetic disease. Am J Med Genet 1997; 71: 289–291.
Benkendorf JL, Peshkin BN, Lerman C . Impact of genetic information and genetic counseling on public health. In: Khoury MJ, Burke W, Thomson EJ, editors. Genetics and public health in the 21st century. New York: Oxford University Press, 2000: 361–383.
Khaw KT, Barrett-Connor E . Family history of heart attack: a modifiable risk factor? Circulation 1986; 74: 239–244.
Roseman JM, Acton RT, Bamberg R . Health and genetic risk assessment instruments. In: Matzen RN, Lang RS, editors. Clinical preventive medicine. St. Louis: Mosby, 1993: 784–798.
Acknowledgements
The authors thank the patients and staff of the Division of Internal Medicine at Northwestern Medical Faculty Foundation who participated in the study, and Reed Pyeritz, who provided helpful feedback on the design of this questionnaire and the scoring measure.
Author information
Authors and Affiliations
Appendix: Study methodology to determine genetic risk
Appendix: Study methodology to determine genetic risk
-
1
The level of risk for mendelian disorders was determined by recognition of a specific diagnosis or a pattern of inheritance consistent with single-gene transmission.20 Participants whose family history was negative for known genetic diseases and who had no suspicious inheritance pattern were assigned the lowest level of risk. Participants whose family history of a disease trait (i.e. NIDDM, glaucoma, or CAD) was suggestive of a single-gene disorder were assigned a moderate level of risk. In addition, participants with a family history of multiple neoplasms suggestive of an inherited cancer predisposition syndrome (e.g., colon cancer and breast cancer in a single individual or in closely related individuals) were given a moderate risk level for a mendelian disorder, but personal levels of risk for these cancers were assessed under the relevant disorder category (i.e. breast cancer, or colon cancer).21 Participants with a family history of a known genetic disease (e.g., hemochromatosis) were assigned the highest level of risk. Participants who were affected with a mendelian disorder were recorded as such.
-
2
The level of risk for adult-onset complex diseases, including NIDDM, CAD, breast cancer, ovarian cancer, prostate cancer, and colon cancer was adapted from Scheuner et al.11 and relevant consensus statements and practice guidelines.22–27 A positive family history was one that contained at least one affected first-degree relative or two affected second-degree relatives from the same lineage. General population risk, coded as low risk, was assigned to individuals whose family history was negative for these diseases and to participants who reported a single affected second-degree relative on the maternal and/or paternal side of the family. In a model developed by Scheuner et al.,11 participants who reported a family history of NIDDM or of breast, ovarian, prostate, or colon cancer were assigned a high level of risk if one of the following conditions was met: (1) one first-degree relative with premature onset of disease (<50 years); (2) two or more affected first-degree relatives; (3) a first-degree relative with late or unknown onset of disease and an affected second-degree relative with premature disease onset from the same lineage; (4) two second-degree relatives from the same lineage with at least one occurrence of premature disease; or (5) three or more affected maternal or paternal relatives.11 A similar design was followed for risk assessment of CAD, but the age for premature disease in men was considered to be 55 years or less and the age for premature disease in women was 60 years or less (Reed Pyeritz, personal communication, 2001).
-
3
The level of risk for thromboembolic disease was scored on the basis of the consensus statement generated by the American College of Medical Genetics.17 This statement recommends that factor V Leiden testing, in conjunction with or followed by an evaluation of additional heritable thrombophilic factors, should be performed in individuals who meet one of the following criteria: (1) any venous thrombosis before age 50; (2) venous thrombosis in unusual sites (such as hepatic, mesenteric, and cerebral veins); (3) recurrent venous thromboses; (4) venous thrombosis and a strong family history of thrombotic disease; (5) venous thrombosis in pregnant women or women taking oral contraceptives; (6) relatives of individuals with venous thrombosis under age 50; (7) myocardial infarction in female smokers under age 50; (8) relatives of individuals known to have factor V Leiden; or (9) women with recurrent pregnancy loss or unexplained severe preeclampsia, placental abruption, intrauterine fe tal growth retardation, or stillbirth. Participants whose personal or family history met one of these criteria were assigned a high level of risk for thromboembolic disease, and individuals with a suspicious history of relative symptoms were assigned a moderate level of risk.
-
4
The level of risk for population-based carrier screening was determined if a participant reported that he or she was planning to have biological children in the next 5 years. Recommendations were generated on the basis of the ethnicity of the participant and the ethnicity of his or her partner (if reported), from population-based screening recommendations supported by the American College of Obstetricians and Gynecologists, the American College of Medical Genetics, and the National Institutes of Health.28–31 These recommendations recognize the higher incidence of certain autosomal recessive conditions in particular ethnic groups, such as cystic fibrosis in Caucasians, Tay-Sachs disease and Canavan disease in the Ashkenazi Jewish population, and hemoglobinopathies in people of African, Asian, and Mediterranean ancestries. When both members of a couple were at increased risk for carrying a mutation associated with the same disease, the highest level of risk was assigned in this category. When either member of the couple was determined to be at an elevated risk for carrying a recessive mutation, a moderate level of risk was assigned.
-
5
The level of risk for additional reproductive issues was also evaluated if a participant indicated that he or she was planning on having biological children in the next 5 years. Patients were considered at risk for reproductive difficulties, and were referred for further risk assessment and genetic counseling, if their personal or family medical history indicated an increased risk for mental retardation, children with birth defects, multiple spontaneous abortions, premature ovarian failure, congenital absence of the vas deferens, or oligospermia and infertility in the patient, the patient’s partner, or close relatives of either member of the couple.32
Rights and permissions
About this article
Cite this article
Frezzo, T., Rubinstein, W., Dunham, D. et al. The genetic family history as a risk assessment tool in internal medicine. Genet Med 5, 84–91 (2003). https://doi.org/10.1097/00125817-200303000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/00125817-200303000-00006