Abstract
Medical genetics has been formally recognized as a medical specialty in the United States only within the past decade. Initially, medical genetics was concerned with relatively rare single gene or chromosomal disorders, but with the sequencing of the human genome, genetics has become the driving force in medical research and is now poised for integration into medical practice. This article offers a perspective on the role of genetics in medical practice and how this role may evolve over the next several years. The author classifies the genetic contribution to medical practice into three categories: monogenic or chromosomal disorders, more common disorders due to a monogenic or single gene mutation, and common multifactorial disorders in which the interaction of multiple genes and the environment contribute to the cause of the condition. The author discusses the positives and the potential pitfalls facing primary care physicians and specialists as they incorporate medical genetics into their practices and points out some of the anticipated changes medical genetics will necessitate, such as an increased medical genetics workforce, including geneticists and genetic counselors. The Human Genome Project has made information of inestimable diagnostic and therapeutic importance available. The medical profession now must rise to both the opportunities and challenges that this wealth of information presents.
Similar content being viewed by others
Main
Medical genetics is a young discipline. Its roots go back to around the middle of the 20th century, and it was formally recognized as a medical specialty in the United States only within the past decade. For most of its history, medical genetics has concerned itself with relatively rare single gene or chromosomal disorders—conditions that are very important to the families who must deal with them, but occupy little of the attention of most medical practitioners. With the elucidation of the human genome sequence and efforts to understand the links between the genome and human health, genetics is now a major driving force in medical research. It is clear that genetics is relevant to all aspects of medicine. Exciting predictions have been made,1 questions have been raised about the complexity of presymptomatic genetic diagnosis,2 and concerns have been raised about ethical implications of genetics in medical practice. How will physicians use genetics in their practice in the coming years? In this review, I will offer a perspective on the role of genetics in medical practice and how this role is likely to evolve over the next several years.
How do genetics and genomics fit into medical practice?
It has been argued that all medical conditions and encounters have a genetics component and can be viewed through a “genetic lens.”3 The contribution of genetics to medical practice is sometimes close to the surface and other times runs more deeply. Here we classify the genetic contribution to medical practice into three categories. The first is composed of monogenic or chromosomal disorders, such as phenylketonuria, sickle cell anemia, neurofibromatosis, or Down syndrome. This is the classical domain of medical genetics, and most physicians would agree that medical geneticists have a role to play in the care of individuals with these disorders in diagnosis, counseling, and, in some cases, management. The second category comprises the more common disorders in which a substantial subset of affected individuals are affected due to a monogenic cause or, at least, where single gene mutations can, in some families, cause the disorder. Examples are breast and ovarian cancer, colon cancer, hemochromatosis (as a cause of liver disease), and cardiomyopathy. These disorders tend to have incomplete and age-dependent penetrance. Here, too, the physician might agree that genetics is important to the care of some of their patients. The challenge is in recognizing which of their patients have a substantial genetic cause and would benefit from further evaluation. The third and largest category comprises the common disorders such as diabetes, hypertension, cancer, cardiovascular disease. Some of these—perhaps most—have rare single gene causes, but, for the most part, the genetics contribution is more complex. These are multifactorial disorders, in which multiple genes interact with one another and with the environment to contribute to the cause of the condition.
We will examine each of these categories in terms of their role in medical practice. In doing so, we will consider the impact of genetics on the activities of three types of medical practitioners. First is the primary care provider, the pediatrician, internist, family practitioner, etc. Second is the specialist, such as the gastroenterologist, the oncologist, or the neurologist. Third is the medical geneticist. We will create a matrix, looking at how these three types of professionals are likely to address the three categories of genetic influence on health and disease.
These three categories are, admittedly, somewhat arbitrary. There is probably no example of a true “single gene disorder”—the environment and modifying genes make all disorders “complex.” The borderline between “rare” and “common” is also ambiguous. The designation of three categories of practitioners is likewise artificial. Primary care providers might include pediatricians, internists, and family practitioners with very different levels of knowledge about genetics. Geneticists themselves may be grouped according to area of subspecialty, and the category subsumes both physician geneticists and genetic counselors. Nevertheless, this simplified scheme may be helpful in identifying major arenas in which geneticists will work alongside other practitioners in providing genetic services.
Monogenic and chromosomal disorders
Disorders due to mutations in single genes or abnormalities of chromosome number or structure are individually rare, but collectively comprise a significant proportion of morbidity as measured, for example, by hospital admissions.4 Physicians who practice pediatrics or obstetrics and gynecology tend to be most aware of genetic disorders, since many present in childhood or are subject to prenatal testing.5 Those who care for adults tend to be less aware, since the more severe disorders may not be compatible with survival to adulthood, or the issues may have already been addressed by the time an affected individual has reached adulthood (although review of genetic counseling issues with the patient as he or she reaches adulthood may not have occurred).
Although the genetic contribution to these disorders has long been recognized, there has been a steady increase in the understanding of these conditions over the years and a corresponding increase in opportunities for intervention. Major triumphs of the “pregenomics era” included the advent of newborn screening programs for inborn errors of metabolism, development of approaches for routine cytogenetic analysis (including high resolution analysis), development of methods for prenatal diagnosis and population screening for carrier status of some disorders, and the use of DNA analysis for diagnosis. More recently, we have seen the advent of tandem mass spectrometry, which promises to increase the range of disorders detected by newborn screening. Methods of prenatal diagnosis continue to be refined, and new ones, such as preimplantation diagnosis, have been introduced. Cytogenetic analysis has been brought to new levels of resolution, revealing ever more subtle, but clinically important, structural alterations. The pathophysiology of genetic disorders is increasingly becoming understood, with the promise of development of new methods of treatment. Gene therapy is an active area of investigation. The scope and precision of molecular diagnosis is rapidly increasing.
The roles of the various medical practitioners in the care of individuals and families with monogenic or chromosomal disorders are fairly clear. The primary care physician must be alert to these disorders and will likely rely on the specialist to establish the diagnosis. Once a diagnosis is made (or suspected), the primary provider works with the specialist to provide longitudinal care and must be prepared to support the patient and family in making medical decisions. Specialists are involved in diagnosis and management of genetic problems that lie within their area of expertise, for example, neurologists with neurodegenerative disorders or nephrologists with polycystic kidney disease. The medical geneticist is usually called upon to establish a diagnosis, usually of multisystem disorders, to provide counseling to patients and families, and may be involved in the longitudinal care of patients with such disorders, for example, inborn errors of metabolism or chromosomal abnormalities.
A number of changes might be anticipated over the next several years. The scope of carrier testing for couples contemplating pregnancy is increasing, exemplified by the introduction of cystic fibrosis carrier screening.6 This will increase the need for a medical genetics workforce, especially genetic counselors. Tandem mass spectrometry is increasing the scope of newborn screening, which may place additional demands on clinical services for inborn errors of metabolism.7 Prenatal tests may become more widely applicable as refined approaches to screening and less invasive diagnostic methods become available. Improved precision of molecular diagnosis will increase the likelihood that individuals with genetic disorders will be accurately diagnosed early in life, and, in some cases, management options will increase.
Monogenic causes of common disorders
Virtually all disorders have monogenic forms in which multiple family members are affected and exhibit single gene transmission. Examples are MODY for diabetes8 or Liddle syndrome for hypertension.9 These, however, are rare causes of these disorders, and most physicians will see very few such patients. Some of these monogenic traits, however, occur more frequently, and comprise a significant proportion of the individuals who might seek care. Upwards of 10% of individuals with breast or ovarian cancer, for example, may have mutation in the BRCA1 or BRCA2 gene.10 Approximately 10% of Caucasians have a mutation in the HFE gene, one of the major causes of hemochromatosis. One in 400 individuals will be homozygous, creating a risk of cirrhosis, among other problems.11 Recognition of these disorders can be challenging, since usually the presentation of the monogenic disorder is not significantly different from more usual instances where single genes make less of a contribution. The major clues are likely to be age of onset (younger in the monogenic variants) and the presence of a family history of similarly affected relatives. The “payoff” on recognition can be significant. Individuals at risk can be offered surveillance, and in some cases, such as hemochromatosis, can be offered treatment. There are also major opportunities to provide counseling, both for individuals at high risk, and for others who may think that their risk is higher than it really is.
How will the three types of physicians approach the care of individuals with these disorders? As noted above, the primary care physician is faced with the major challenge of recognizing patients who face the increased risks associated with a genetic cause to their disorders. In part, this requires education of primary providers to recognize these disorders and the indications for further evaluation. Because family history is a major clue to diagnosis, primary providers will need to have access to information about the family history of their patients. This may require asking directed questions focusing on areas of known risk, such as cancer or liver disease. Development of tools, such as questionnaires or computer systems that will allow physicians to learn of major issues in their patients' family histories, may be helpful to facilitate this process. Information on how and when to refer patients for specialty evaluation will need to be placed at the physician's fingertips. The medical specialist faces similar challenges within his or her area of focus and will benefit from similar education and access to information.
The medical geneticist has long had a role in counseling individuals and families affected with single gene disorders, and has increasingly become involved in areas such as cancer genetics and hemochromatosis. It is less likely that the geneticist will assume responsibility for the medical care of individuals with these disorders; individuals at risk of colon cancer, for example, require surveillance (e.g., colonoscopy) that must be provided by an appropriate specialist. The medical genetics community is faced with an educational challenge for these disorders since most geneticists were trained to deal with rare disorders, such as inborn errors of metabolism and congenital anomaly syndromes. The geneticist may be an expert in the interpretation of genetic tests and family history information but may have little familiarity with the natural history and management of breast cancer or hemochromatosis. There will be a need for the geneticist to form partnerships with other medical specialists to provide appropriate diagnostic, counseling, and management services for what is likely to be an increasing number of patients.
The demand for genetic risk assessment and counseling, incidentally, may exceed what might be expected based on the frequency of this group of disorders. For every individual who is at risk for breast cancer due to BRCA1 mutation, for example, there are probably several who have a relative with breast cancer and think that their risk is increased. These people may not need to have genetic testing or surveillance for disease, but they may benefit from meeting with a counselor to get an accurate assessment of risk. The outcome usually will be reassurance; occasionally it will result in testing and the subsequent institution of a management program.
The approach to this group of disorders is in rapid evolution and will likely see major changes in the next several years. First, many additional disorders are likely to be added to the list. The identification of the major genes for breast and ovarian cancer spawned a rapid demand for counseling and testing. Will the same thing happen when genes for psychiatric illness are identified? Second, advances in information technology are likely to have a major impact on the care of these disorders. Physicians will increasingly need to use computers to access medical information about their patients, to recognize patterns that require intervention, and to access testing and referral services as well as patient information material. Furthermore, patients themselves are increasingly turning to computer resources, especially the Internet, for medical information. It seems likely that counseling and testing services may at some point be available directly to patients, without the intermediary of their primary care physician. A third change that might be anticipated concerns the ethical context in which genetic information is used in patient care. There is major concern now about the risks of loss of privacy and discrimination. Some of this has been addressed through passage of laws that ban at least some use of genetic information for employment or insurance. National legislation remains unenacted. It is not clear that the issues raised by genetics are really unique in medicine, but genetics is drawing attention to these issues and will likely drive responses both in terms of legislation and regulation. A final change concerns the public health implications of genetics in medicine. There is a long history of public health initiatives in genetics, particularly in the area of newborn screening. As testing becomes possible for genetic causes of common disorders, and especially as interventions become available, there is likely to be increasing attention given toward the possibility of wide-scale screening.12,13 This debate is already under way with respect to hemochromatosis.11
Common disorders
Genetics will become truly integrated into medical practice when the genetic contributions to common disorders, such as diabetes or cardiovascular disease, are understood and can be used to improve the quality of care. Although most of these disorders include rare single gene causes (see above), most are due to an interaction of multiple genes and environmental causes. A large number of genes may be involved in any particular disorder, and the specific genes involved may differ from one individual to the next. Some genes will contribute substantially toward risk; others will make a slight contribution. Genetics will be important not only to understanding the cause of a disease, but also to recognizing the manner in which an individual responds to particular therapies. Drug metabolism is itself under genetic control, and susceptibility to side effects in some cases is governed by genetic predispositions.14
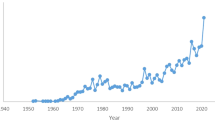
A scheme for thinking about the genetic contribution to common disorders is presented in Figure 1. Individuals inherit genes that may predispose them to disease but will only develop the signs and symptoms if exposed to appropriate environmental factors. Chance may also play a role in determining whether an individual who is at risk becomes symptomatic. Genetic testing may have a role both in the presymptomatic phase and after signs and symptoms have emerged.
Individuals are born with a genetic liability to disease but remain in a presymptomatic state until exposure to environmental factors leads them to cross a threshold into recognizable disease. The y axis depicts progression from prenatal life to a presymptomatic state to a state in which disease is present.
Presymptomatic genetic testing raises many controversial issues, both technical and ethical. In some instances, genetic test results may contribute very small increments of relative risk, which may not provide guidance for management.2 The genetic contribution to some disorders may be diverse, making it difficult to generate experience with any particular combination to provide meaningful risk estimation to an individual. There is a risk of overestimation of penetrance from databases on ascertainment of families in which many individuals are affected, and it may be many years before the risk of disease in a carrier is known.15 Finally, there are concerns about the usefulness of information if intervention is not possible and about risks of stigmatization and discrimination. Despite all these challenges, however, it is likely that at least some disorders will be subject to presymptomatic testing, particularly where early treatment improves the natural history.
Genetics may have its greatest role in the care of individuals with common disorders in the realms of diagnosis and therapy. Identification of genes that contribute to these conditions, even if they convey only small increments of risk, will reveal pathological mechanisms that may have been previously unsuspected. This, in turn, will provide an opportunity to develop new approaches to therapy, in some cases by the design of new drugs that target particular cellular pathways. Choice of therapy may, at some point, be guided by genetic tests that identify subcategories of disease that will respond to specific treatments. Drug dosage may be influenced by tests of drug metabolism polymorphisms, and serious side effects may be avoided by avoiding the use of specific drugs in individuals at risk.
Most of these changes will have their greatest impact on the day-to-day practice of medicine by primary care providers and by medical specialists. Physicians may one day make treatment decisions based on tests without realizing or needing to know whether the tests are based on analysis of DNA, proteins, or other markers. The role of the medical geneticist for common disorders is likely to be more in the background than for the other categories of disease. There will always be a subset of patients with multisystem disorders with a significant genetic component for which the medical geneticist will be able to provide comprehensive assessment. But for most of the common disorders, the geneticist will play a role in the development of testing systems and the interpretation of test results.
Into the future
We have created a matrix that is shown in Table 1. The integration of genetics into medical practice will occur at a variable pace for different disorders and in different areas of medicine. Medical geneticists will need to work together with primary care providers and other specialists; their roles in risk assessment, diagnosis, management, counseling, and development of approaches to testing will need to be customized to the specific disorders. Major advances in understanding genetic contributions to pathogenesis and development of new approaches to testing and treatment can be expected. Similarly, it is likely that advances in information technology will empower both primary care providers and patients in taking more control of the management of complex disorders. All of this will place major demands on the education of the medical community and the general public. It will also require action by policy makers to address concerns about discrimination, and to maintain wide-scale access to high quality testing. The information placed at our disposal by the Human Genome Project offers great opportunities, and we will be judged by future generations on how well we rise to both the opportunities and the challenges.
References
Collins FS . Shattuck lecture: medical and societal consequences of the Human Genome Project. N Engl J Med 1999; 341: 28–37.
Holtzman NA, Marteau TM . Will genetics revolutionize medicine?. N Engl J Med 2000; 343: 141–144.
Childs B, Valle D . Genetics, biology and disease. Annu Rev Genomics Hum Genet 2000; 1: 1–19.
Hall JG, Powers EK, Mcllvaine RT, Ean VH . The frequency and financial burden of genetic disease in a pediatric hospital. Am J Med Genet 1978; 1: 417–436.
Hayflick SJ, Eiff MP, Carpenter L, Steinberger J . Primary care physicians' utilization and perceptions of genetics services. Genet Med 1998; 1: 13–21.
Grody WW, Desnick RJ . Cystic fibrosis population carrier screening: here at last—are we ready?. Genet Med 2001; 3: 87–90.
Albers S, Waisbren SE, Ampola MG, Brewster TG, Burke LW, Demmer LA, Filiano J, Greenstein RM, Ingham CL, Korson MS, Marsden D, Schwartz RC, Seashore MR, Shih VE, Levy HL . New England Consortium: a model for medical evaluation of expanded newborn screening with tandem mass spectrometry. J Inherit Metab Dis 2001; 24: 303–304.
Winter WE, Silverstein JH . Molecular and genetic bases for maturity onset diabetes of youth. Curr Opin Pediatr 2000; 12: 388–393.
Shimkets RA, Warnock DG, Bositis CM, Nelson-Williams C, Hansson J, Schambelan M, et al. Liddle's syndrome: heritable human hypertension caused by mutations in the b subunit of the epithelial sodium channel. Cell 1994; 79: 407–414.
Newman B, Mu H, Butler LM, Millikan RC, Moorman PG, King MC . Frequency of breast cancer attributable to BRCA1 in a population-based series of American women. JAMA 1998; 279: 915–921.
Hanson EH, Imperatore G, Burke W . HFE gene and hereditary hemochromatosis: a HuGE review. Human Genome Epidemiology. Am J Epidemiol 2001; 154: 193–206.
Burke W, Coughlin SS, Lee NC, Weed DL, Khoury MJ . Application of population screening principles to genetic screening for adult-onset conditions. Genet Test 2001; 5: 201–211.
Yoon PW, Chen B, Faucett A, Clyne M, Gwinn M, Lubin IM, Burke W, Khoury MJ . Public health impact of genetic tests at the end of the 20th century. Genet Med 2001; 3: 405–410.
Evans WE, Relling MV . Pharmacogenomics: translating functional genomics into rational therapeutics. Science 1999; 286: 487–491.
Welch HG, Burke W . Uncertainties in genetic testing for chronic disease. JAMA 1998; 280: 1525–1527.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Korf, B. Genetics in medical practice. Genet Med 4 (Suppl 6), 10–14 (2002). https://doi.org/10.1097/00125817-200211001-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/00125817-200211001-00003
Keywords
This article is cited by
-
Genetics education in primary care residency training: satisfaction and current barriers
BMC Primary Care (2022)
-
Heart rate variability and vibration perception threshold in healthy young adults with parental history of type 2 diabetes mellitus
International Journal of Diabetes in Developing Countries (2015)