Abstract
Purpose: Hearing loss is a common congenital disorder that is frequently associated with mutations in the GJB2 gene encoding the connexin 26 protein (Cx26). We sought to evaluate the effectiveness of direct DNA sequencing for detection of Cx26 mutations as a clinical diagnostic test.
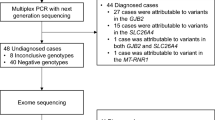
Methods: We designed a clinical assay using a three-step polymerase chain reaction (PCR)-based DNA sequencing strategy to detect all possible mutations in the open reading frame and flanking sequences of Cx26. The results of the first 324 cases of childhood deafness referred for diagnostic testing were analyzed.
Results: A total of 127 of the 324 (39.2%) cases had at least one mutant Cx26 allele (36.1% of sporadic cases, 70% of familial cases). Of these 127 case, 57 (44.8%) were homozygotes or compound heterozygotes. Thirty-four different mutations were identified, including 10 novel mutations, 6 of which (T8M, K15T, R32L, M93I, N206S, and 511-512insAACG) may be pathogenic. We also provide new evidence on the pathogenicity or nonpathogenicity of 12 previously reported mutations, and clarify the confusing nomenclature of the 313-326del14 mutation.
Conclusion: A simple and rigorous method for efficient PCR-based sequence analysis of Cx26 is a sensitive clinical assay for evaluating deaf children. Its widespread use is likely to identify additional pathogenic mutations and lead to a better understanding of the clinical significance of previously identified mutations.
Similar content being viewed by others
Main
Hearing loss is a common congenital disorder, affecting 0.1% to 0.2% of all newborns. Of these cases, ∼60% are inherited and ∼80% of inherited deafness falls under the category of autosomal recessive, nonsyndromic hearing loss.1–3 Within this category, ∼50% of severe to profound cases are classified as DFNB1 in the ethnic populations tested4,5 and are caused by mutations in the GJB2 gene,6–9 which encodes the protein connexin 26 (Cx26), a member of the connexin family of proteins. These proteins are major constituents of intercellular gap junctions, and Cx26 is believed to play a crucial role in regulating potassium ion flux during auditory transduction in the inner ear.10–12 In addition, a few autosomal dominant deafness-causing mutations in Cx26 have also been described, classified clinically as DFNA3.5 Moreover, mutations in Cx26 (and in other connexins) have been associated with syndromic deafness, including Vohwinkel syndrome, palmoplantar keratoderma, and erythrokeratodermas.13–17
Several studies have demonstrated a wide spectrum of Cx26 mutations associated with hearing loss in patients with a broad range of deafness. Although the most common mutation is 35delG, the prevalences and carrier frequencies of the different mutations vary among peoples of different ethnicities.18–32 Over 70 pathogenic recessive or dominant mutations, and close to 20 allelic variants with undetermined pathogenicity or polymorphisms, have been reported.33–35 However, no clear genotype-phenotype correlations have been established.36–41
We report here the results of a sequence-based mutation analysis of the connexin 26 (GJB2) gene in blood samples from 324 children (and appropriate family members) sent for clinical molecular diagnostic testing for familial or sporadic deafness. We detected 34 different mutations, 10 of which are novel (9 missense and 1 small insertion). In addition, this report will provide new evidence regarding the pathogenicity or nonpathogenicity of 12 previously reported mutations, and will propose the proper nomenclature for the 313-326del14 mutation.
MATERIALS AND METHODS
Sources of referred materials
A total of 324 presumably unrelated children with documented sensorineural hearing loss (SNHL) of uncertain etiology had blood samples submitted by specialists in Otolaryngology, Clinical Genetics, Audiology, and General Pediatrics for clinical molecular diagnostic testing. These samples included those from 30 children with a history of multiple deaf family members (familial cases), and 294 children with no family history of deafness (sporadic cases). This research study was approved by the Children's Hospital Boston Institutional Review Board (IRB).
Clinical classification of referred cases
Patients were clinically classified by the referring physician. When the classification was incomplete, clinical notes and audiology testing results from the medical record were examined.
Family studies and control samples
Extended family studies, including blood samples from affected family members (deaf siblings/parents), and at-risk family members (obligate or possible carriers), were undertaken after genetic counseling for the presence of a mutation in a proband. Anonymous DNA samples from 100 individuals without known genetic disorders and hearing loss were analyzed as control subjects. The Cx26 gene (GJB2) mutation analysis for all of the deaf children and their available family members, and 100 control subjects was performed by the following three-step polymerase chain reaction (PCR)-based sequencing procedure.
(1) PCR amplification
Genomic DNA was extracted from whole blood with a D-50K PureGene DNA isolation kit (Gentra), according to the manufacturer's instructions. PCR was used to amplify the entire open reading frame (ORF) of the Cx26 gene (GJB2) using a pair of PCR primers (CX26-F, TGC-TTA-CCC-AGA-CTC-AGA-GAA; CX26-R, CGA-CTG-AGC-CTT-GAC-AGC-TGA) in a 50-μL reaction mixture containing 100 to 200 ng of genomic DNA, 1× PCR buffer (10 mM Tris-HCl, pH 8.3, and 50 mM KCl, 1.5 mM MgCl2), 400 μM dNTPs, and 1 unit of Taq polymerase (Roche). PCR reactions were amplified in a Peltier Thermal Cycler (PTC-200, MJ Research) after an initial denaturation at 94°C for 4 minutes, followed by 35 cycles of 94°C denaturation for 1 minute, 60°C annealing for 1 minute, and 72°C extension for 2 minutes. The PCR product was verified by agarose gel electrophoresis (3%).
(2) Direct sequencing analysis
The PCR product was purified with a Wizard PCR Prep DNA Purification System (Promega), according to the manufacturer's instructions. A-12 μL sequencing reaction was performed with 50 ng of the purified PCR product, 10 pmol of each four sequencing primers (two original PCR primers, CX26-F and CX26-R; and two internal sequencing primers, CX26-IF, AGT-GGC-CAT-GCA-CGT-GGC-CTA; CX26-IR, TGA-TCT-CCT-CGA-TGT-CCT-TAA), and a BigDye Terminator Cycle Sequencing Ready Reaction Kit (ABI PRISM, Perkin-Elmer). Bidirectional sequencing was performed on an ABI 373 DNA Sequencer (Perkin-Elmer). Sequencher 4.1 software (GeneCode) was used for mutation analysis on a Macintosh G3 computer (Apple). The Cx26 reference sequence used for all analyses was GDB accession number M86849.
(3) Additional sequencing analysis
In the event that two different frameshift mutations were detected with the same pair of PCR primers, a third sequencing reaction was performed to enable unambiguous analysis of the sequence between the frameshifts. For example, an additional sequencing reaction (primer CX26-35F, TGT-GAA-CAA-ACA-CTC-CAC; primer CX26-167R, GGG-TGT-TGC-AGA-CAA-AGT-CG) was designed to analyze the sequence between the common 35delG and 167delT mutations. Similarly, other specific primers could be designed to analyze sequence between any two frameshifts with an appropriate distance of base pairs separating the mutations.
RESULTS
A total of 127 of the 324 (39.2%) patients tested had at least one mutant Cx26 allele. Of these 127 cases, 26 (20.4%) were homozygotes, 31 (24.4%) were compound heterozygotes, and 70 (55.1%) cases had only one detectable mutation. All of the patients had sensorineural hearing loss of varying severity. Table 1 lists each of the observed genotypes and their observed frequencies. None of these mutations were detected in 100 control subjects with no known genetic disorders and hearing loss, except 35delG and M34T, which were each detected once as heterozygotes (Table 1).
Thirty of the 324 (9.3%) patients had multiple affected family members (2–4 deaf individuals per family), and 82 of these family members underwent mutation testing. Of the 30 families tested, 70% (64 individuals in 21 families) had at least one Cx26 mutation; of these, 85.7% (18 of 21) had biallelic mutations (homozygotes or compound heterozygotes, listed in Table 1).
A total of 106 of the 294 (36.1%) patients with sporadic deafness had at least one Cx26 mutation; of these, 37% (39 of 106) had biallelic mutations. In this study, the most common biallelic mutations were 35delG/35delG (9.6%), 35delG/M34T (5.6%), 35delG/167delT (5.6%), M34T/M34T (3.2%), V37I/V37I (3.2%), and 167delT/167delT (2.4%).
One hundred seventy-nine of the 648 (27.6%) alleles/chromosomes tested contained a Cx26 mutation. Thirty-four different mutations were detected, including 10 novel (9 missense and 1 frameshift) mutations showed in bold type in Table 1 (one new silent mutation, T26T resulting from ACC→ACT, is not included). Figure 1 shows these mutations arranged by Cx26 protein domain: intercellular (IC), transmembrane (TM), and extracellular (EC). Although the IC2 domain contained the greatest number of different mutations, the most prevalent mutations, such as 35delG, M34T, V37I, and 167delT, were in domains IC1, TM1, and EC1. Figure 1 also demonstrates that the distribution of Cx26 mutations in this study was similar to previous reports (for references, see Fig. 1).
The distribution of 34 different Cx26 mutations detected in this study (see Table 1 in detail) located in the protein domains (IC, intercellular; TM, transmembrane; EC, extracellular) and the spectrum of Cx26 mutations with comparison of the references. (Note: pooled data from review articles by Kelley et al.,33 Kelsell et al.,17 Rabionet et al.,34 and their Connexin-Deafness home page,35 http://www.iro.es/deafness)
Table 2 shows the most common mutant alleles seen in both familial and sporadic cases. 35delG was the most common mutation, accounting for 39% of the total 179 mutant alleles. The other most frequent mutations were M34T (16%), 167delT (13%), and V37I (6%).
Nine novel missense mutations were identified in this study and are listed in Table 3, along with phenotype data and family history, nucleotide/codon change at protein domains, and comparison of conserved amino acid residues at their positions among connexins. The possibility of pathogenicity or indeterminate for these novel missense mutations was described in the discussion. The new frameshift mutation 511-512insAACG, a 4-bp insertion at nucleotides 508-511 resulting in a short repeat (AACGAACG), was believed to be pathogenic. None of the 10 novel mutations were found in the DNA samples from 100 control subjects with no known genetic disorders and hearing loss.
DISCUSSION
The three-step PCR-based direct sequencing strategy we designed for our diverse patient population is capable of detecting all possible mutations within the open reading frame and flanking sequences. Furthermore, this method is also able to determine whether two frameshift mutations occur in cis or in trans, in cases where an equivalent number of base pair(s) are deleted or inserted. For most samples, it is only necessary to perform one PCR and two sets of bidirectional sequencing reactions. However, although sequence analysis is robust for the detection of a single frameshift or point mutation, it could theoretically give ambiguous results in a patient with multiple frameshift mutations that occur within the same region defined by a pair of PCR primers. For example, the presence of one frameshift may obscure a second, downstream, frameshift; definitive diagnosis in this setting requires careful analysis by experienced laboratory personnel. In addition, two frameshift mutations could mask an interposed third mutation. The PCR method described in this study will not detect large deletions of the entire Cx26 gene.
In the event that two frameshift mutations occur within the same sequencing primer pair-defined region, we use a third set of sequencing primers specific for the region between the two frameshifts. This extra sequencing step not only unambiguously identifies multiple frameshift mutations but it also identifies the phase of the two mutations (cis vs. trans) and enables the detection of a third possible mutation between the two frameshift mutations. We designed flanking primers for the 35delG, 167delT, 235delC, and 313-326del14 mutations and have used them to diagnose six families with compound heterozygous mutations 35delG and 167delT and two families with 35delG and 313-326del14, without requiring other techniques, such as single strand DNA sequencing, single-strand conformation polymorphism, denaturing high performance liquid chromatography, or parental studies. Because at least 12 small deletions/insertions have been reported between nucleotides 1-350 (called Cx26–1 region in this study) and six frameshift mutations have been reported in nucleotides 320-700 (Cx26–2 region), this strategy represents a simple and rigorous method for mutation detection.
The ability of this method to detect all intragenic Cx26 mutations has allowed us to identify nine novel missense mutations, although it is not clear if all are pathogenic because segregate studies could not be performed for the sporadic cases. Of these, five (T8M, K15T, R32L, M93I, and N206S) are most likely to be responsible for the deafness phenotype observed in this study. Six factors were considered in determining the pathogenicity of a new mutation: (1) evolutionary conservation of amino acid residues over several species and across different connexins; (2) significant charge or polarity difference resulting from the mutation; (3) occurrence of mutation at the same residue in other connexins involved in deafness; (4) type of hearing loss; (5) coexistence with a second Cx26 mutation; and (6) absence of the mutation in 100 control subjects. The data regarding these points are listed in Table 3. The five novel mutations all occur at residues that are conserved among connexins, including at least three in humans (Cx26, Cx30, Cx31, or Cx32), mice (Cx30), and chickens (Cx31); all the five cause either significant amino acid changes in charge and/or polarity, or the same amino acid changes are found in other connexins associated with deafness. These mutations all occurred in patients with bilateral deafness of varying severity and no inner ear malformation; the clinical findings, thus, were consistent with autosomal recessive nonsyndromic hearing loss.
It should be noted that the case for pathogenic significance of T8M and R32L is less straightforward than for K15T, M93I, and N206S (each coupled with 35delG) because of uncertainty involving their pathogenicity of the second associated mutations. T8M was found in a compound heterozygote state with V153I, a missense mutation previously seen in control subjects,35 but was also detected in two deaf children in this study. V153I is conserved across other connexins (human Cx26, Cx30, Cx32; mice Cx30 and chicken Cx31); raising the possibility that V153I is pathogenic. Similarly, R32L was found in a compound heterozygote state with V27I, a widely reported allele variant; the possibility of another undetected pathogenic mutation cannot be excluded. Nevertheless, this amino acid residue appears to be important for normal function, as two other pathogenic mutations (R32C and R32H) responsible for hearing loss have been identified recently.35,46 In fact, of all the amino acids in the TM1 domain, R32 is one of the most highly conserved (shares identity in all four human Cx26, Cx30, Cx31, Cx32; mice Cx30; and chicken Cx31) that has been implicated in hearing loss. These facts support the presumed pathogenicity of R32L.
The pathogenicity and inheritance of the remaining four new mutations (I20M, H67R, E119K, and E129K) cannot be assessed clearly by analysis of our data (Table 3), although none of these mutations were found in the DNA samples from 100 control subjects. I20M, H67R, and E119K all occurred without accompanying pathogenic mutations, in patients with no other affected family members; furthermore, H67 and E129 are less conserved amino acid residues. However, a few interesting observations for two of these mutations (I20M and E129K) will be discussed below, along with other controversial mutations.
Of the 34 mutations seen in this series, 12 have been the subject of controversy regarding their pathogenicity, either with regard to pattern of inheritance (dominant vs. recessive) or clinical significance (pathogenic vs. nonpathogenic). For some of these mutations, previous data were incomplete due to their detection only in normal controls or as sole mutations in a few individuals. Table 4 lists these mutations, including four (T123N, S139N, R143Q, and A171T) that have been independently identified this year by us and other researchers.30,43,44,49 The mutations are listed with accompanying phenotype and family history, nucleotide/codon change at protein domain, and amino acid conservation among connexins.
In this study, E129K and R143Q (Tables 3 and 4) were detected in deaf children with unilateral high-frequency SNHL, a type of hearing impairment rarely seen in autosomal recessive nonsyndromic hearing loss. This type of high-frequency hearing loss has been described previously in association with dominant Cx26 mutations.16,52 Our patients with familial E129K and R143Q had similar hearing impairment in at least two generations. Two recent studies detected R143Q as the sole mutation in deaf patients,30,44 and one of the reports indicated that this mutation was associated with dominant high-frequency hearing loss in a family.30 These data raised the question of whether E129K and R143Q each represent dominant nonsyndromic pathogenic mutations, but because other affected family members were not available for genotyping, the possibility of these mutations being either recessive or allele variants cannot be excluded.
Three sole mutations (I20M, T123N, and A171T) occurred in the patients with other phenotypes besides hearing loss (Tables 3 and 4). Whether these may contribute to a syndromic form of deafness or may be coincidental remains to be determined. The patient with I20M had unilateral mild SNHL, bilateral colobomas, a small atrial septal defect, and other minor congenital anomalies. A few syndromic diagnoses have been ruled out by extensive DNA tests, fluorescence in situ hybridization, and karyotyping. This mutation involves a highly conserved amino acid in IC1; another pathogenic mutation (I20T) at the same residue has been identified recently,30 raising the possibility of I20M being pathogenic and responsible for the phenotype in this patient. In contrast, A171T and T123N occur in residues that are not well-conserved among connexins. A171T was detected as the sole mutation in another patient with SNHL and an abnormal cochlea,44 similar to the findings in our patient. A171T is located within EC2, a region rich in pathogenic mutations in Cx32, and its change results in a nonpolar to polar amino acid. It has thus raised question of whether A171T is causative for this type of syndromic hearing loss or totally unrelated to the phenotypes. T123N was found in this study and in another report,49 but both cases are believed to be of unknown significance.
This study has provided additional data to support the specific classification or reclassification of other controversial mutations. For example, two families had G12 V and S139N, respectively, each was observed in an affected brother-sister pair (Table 4); each was accompanied by 35delG;27,43 and both amino acid residues are highly conserved (shares identity in all four human Cx26, Cx30, Cx31, Cx32). These findings now support the designation of G12 V and S139N as recessive pathogenic mutations.
In addition, four mutations (F83L, R127H, G160S, and I203T) were initially found in individuals with normal hearing,18,21,34,35 and then detected as sole mutations in deaf children by this study and others.27,44,46,47 The supporting evidence for these mutations is limited: R127H was detected in an affected brother-sister pair, whereas F83L, G160S, and I203T occur at highly conserved residues. Therefore, it is not unreasonable to raise the question of whether these are pathogenic mutations. In contrast, two presumed allele variants, V27I and E114G, were recently described as pathogenic in a compound heterozygous state.35 Our finding of the same genotype, V27I/E114G, in a father-son pair is not compatible with the report, because although the proband had severe SNHL, his father had normal hearing. Further analysis confirmed that both alleles were in cis, demonstrating that the child's deafness is unrelated to the V27I/E114G. Nevertheless, further observations/studies will be necessary to address the essential issue of whether these novel and debated mutations are indeed associated with hearing loss, nonsyndromic or syndromic, recessive or dominant.
M34T is the most controversial allele. It was initially hypothesized to cause autosomal dominant nonsyndromic hearing loss, but then numerous studies suggested it to be either an allele variant, because of its occurrence in the heterozygous state in the general population, or a mild recessive mutation because of its occurrence with other Cx26 mutations in many deaf individuals6,19,21,24,29,34–37,42,44–46,48–51. The observation, reported by us and others,45,48 of multiple deaf families that are homozygous for the M34T allele provide lends more additional support that this is a recessive rather than a dominant allele. To date, most reported cases of M34T homozygotes or compound heterozygotes showed mild or mild-moderate deafness.21,29,37,42,45 In one family, severe nonsyndromic SNHL did not cosegregate with the compound heterozygote state M34T/167delT, but this phenotype did cosegregate with the 167delT allele.50 None of the affected individuals with M34T has had bilateral severe-to-profound hearing loss across all frequencies observed in nine families.48 Phenotypic expression of the M34T allele variant may depend on mutations segregating in the trans allele, suggested by Cucci et al.,48 after comparing audiograms and genotypes. Our study identified four additional deaf patients in three unrelated families who were homozygous for M34T, as well as eight affected compound heterozygotes (35delG/M34T x 7, M34T/V37I). All available auditory evaluations in these patients showed varying severity, including mild hearing loss in one ear with mild-to-severe hearing loss in the other; or, bilateral mild or mild-moderate hearing loss. Furthermore, the frequency of the M34T allele in deaf patients (4.3%) in this study is significantly higher than that (0.5–3.2%) seen in other published reports.19,21,43,45 This discrepancy may reflect ethnic variation differences in the populations studied or ascertainment bias resulting from differences in study inclusion criteria. For example, our study included patients with mild hearing loss, whereas other reports often included patients with only moderate-to-profound deafness.
Current data favor the hypothesis that M34T may cause a milder form of nonsyndromic recessive hearing loss and is not a common cause of severe-to-profound hearing loss. Nevertheless, it is still difficult to exclude the possibility that the frequent detection of the M34T allele in deaf individuals (sporadic cases or sibling pairs) is simply coincidental due to the high carrier rate studied in several world populations.24,34,48,49 The consequence of interaction between the M34T and wild-type Cx26 allele remains intriguing because of different phenotypic effects in some carrier parents.48 The debate will only be resolved by further studies, such as a meta-analysis of pooled data from multiple groups may be able to show whether there is a statistically significant association of M34T homozygosity with hearing loss; detecting cosegregation of M34T with deafness in large families and additional comparisons between M34T and the severity of hearing loss within patients may help to clarify the pathogenic effect of the M34T mutation.48,51
Similarly, V37I was initially described as an allele variant because of its occurrence in the heterozygous state in the general population, but it was suggested recently to be a potential pathogenic mutation causing nonsyndromic recessive hearing loss because of its occurrence together with other Cx26 mutations in some deaf individuals19,27,29,35,42–44,46. Our previous report42 and this study, as well as that of Rabionet et al.27 provide strong rationale for the reassignment of V37I from an allele variant to a pathogenic mutation due to the finding of deaf individuals in multiple families with homozygote for V37I. We detected three unrelated families with homozygotes, including one sibling pair, and two families with compound heterozygotes (V37I/M34T and V37I/167delT). Another report found V37I mutations in six patients from five families, including two unrelated patients with homozygous mutation.43 Furthermore, V37I mutation has been detected in 6% (10/179) of mutated alleles in this study, demonstrating a higher frequency of this mutation than had been previously reported27,43 (0.47% and 3.6%). As was similarly observed with M34T mutation, our inclusion of patients with a broader spectrum of hearing loss may explain the discrepancy between our results and other studies.
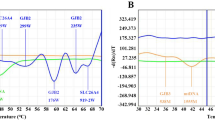
Controversy also exists regarding the nomenclature for a common 14-bp deletion occurring at nucleotides 310-314.9,19,27,36,43 The GA-rich and the 5G-strip nucleotide sequences before and after the 14-bp deletion in this region easily lead to different descriptions, such as 310-323del14, 311-324del14, 312-325del14, 313-326 del14, and 314-327del14. We have detected this deletion in three unrelated families and have identified the same sequences chromatogram (Fig. 2). We believe that these deletions, described in various positions in other studies, are probably the same mutation. Compared with our sequences chromatogram (Fig. 2 A) and the normal sequence (Fig. 2 B), Figure 2 C lists the five sequences (before and after the 14-bp deletion) deduced from various descriptions. Our analysis allows for three possible nomenclatures for description of this mutation: 311-324del14, 312-325del14, or 313-326del14. Our data are not compatible with nomenclatures of 310-323del14 or 314-327del14bp, due to malpositions of G and A nucleotides, as shown in Figure 2 C. Based on the recommendation by the Human Nomenclature Committee,53 the preferred nomenclature for this deletion should be 313-326del14. Similarly, the nomenclature for another reported 2-bp deletion at nucleotides 333-335 should be 334-335delAA.
Nomenclature for the 14-bp deletion occurring at started nucleotides 310-314. A: Chromatogram of the 14-bp deletion, the same pattern as seen in three unrelated deaf children. B: Normal sequences without the 14-bp deletion. The numbers indicate nucleotide position. C: Comparison of the sequences before and after the 14-bp deletion. (Note: a, translated from the chromatogram by this study; b, deduced from the various descriptions by the references including this study.) The sequences before the 14-bp deletion are not bold and the sequences after the 14 bp deletion are bold, according to each described position of deletion. The numbers separated by a slash indicate the original nucleotide positions before/after the 14-bp deletion. The underlined base (i.e., G at 310-323del14 and A at 314-327del14) indicates that this base is not compatible with the chromatogram.
Approximately 55% of deaf children in this series had only one Cx26 mutation, which is much higher than other reports (10–42%).18–21,27–31,36,38 Of these, 63% were seen in sporadic cases but only 15% in familial cases. Beside the common mutations in this series, the remaining 20 mutations were only seen once each; most were rare mutations with no detection in 100 control subjects (Table 1). It is unclear whether this is a true difference between the sporadic and familial cases or for some reason the mutation is being missed in the sporadic cases. There are a few possible factors that may influence the observation. First, some mutations may be overlooked by this sequencing approach; however, a 100% concordance of our initial method validation with blind tests of series known mutations and normal controls indicated that this possibility is unlikely. Second, although some patients may coincidentally be true heterozygotes for one of the most frequently observed mutations (e.g., 35delG, M34T, and 167delT), this does not explain why many patients observed in this study had such mutations (common or known pathogenic) with no relation to their hearing loss. Third, a second mutation outside the Cx26 coding region or in other connexins could remain unidentified, which is more likely to explain our observations because this series only examined the open reading frame and flanking sequences of Cx26. Particularly, two recent studies independently identified a large deletion affecting Cx30 (GJB6) in 22 of 33 Spanish patients54 and in 7 Ashkenazi Jewish patients,55 whereas it remains to be seen if both deletions are the same. All 29 positive cases were either homozygote for the deletion, or double heterozygote for the deletion and for a Cx26 mutation. Because both studies screened patients in whom only one Cx26 mutation was found previously, and the detection rate for this deletion is high, it is a good candidate for testing our patients. Its occurrence as a frequent mutation or founder mutation remains to be studied in different populations. In addition, the noncoding exon 1 of Cx2624 and the Cx43 (GJA1)56 are also reasonable candidates for searching for a second mutation.
In a summary for these novel and debated mutations: T8M, G12 V, K15T, R32L, V37I, M93I, S139N, and N206S may be recessive pathogenic mutations; I20M and A171T may possibly cause syndromic hearing loss; T123N and E114G/V27I are less likely to cause hearing loss; M34T remains controversial; and eight remaining mutations (H67R, F83L, E119K, R127H, E129K, R143Q, G160S, and I203T) are of uncertain pathogenicity and/or inheritance.
In conclusion, this study has presented a method for efficient PCR-based sequence analysis of the connexin 26 (GJB2) gene. Its widespread use in cases of congenital hearing loss is likely to identify additional pathogenic mutations and lead to a better understanding of the clinical significance of previously identified mutations, as well as to contribute to the effective counseling of deaf individuals.
References
Morton NE . Genetic epidemiology of hearing impairment. Ann N Y Acad Sci 1991; 630: –31.
Cremers CW, Marres HA, Van Rijn PM . Nonsyndromal profound genetic deafness in childhood. Ann N Y Acad Sci 1991; 630: 191–196.
Nance WE, the newborn hearing subcommittee of the public health genetics committee. Statement of the American College of Medical Genetics on universal newborn hearing screening. 2000; 2(2): 149–150. (also available at American College of Medical Genetics Home Page, 2000; http://www.faseb.org/genetics/acmg/)
Guilford P, Ayadi H, Blanchard S, Chaïb H, Le Paslier D, Weissenbach J, Petit C . A human gene responsible for neurosensory, non-syndromic recessive deafness is a candidate homologue of the mousesh-1 gene. Hum Mol Genet 1994; 3: 989–993.
Van Camp G, Smith RJH . 2001; http://www.uia.ac.be/dnalab/hhh.
Kelsell DP, Dunlop J, Stevens HP, Lench NJ, Liang JN, Parry G, Mueller RF, Leigh IM . Connexin 26 mutations in hereditary non-syndromic sensorineural deafness. Nature 1997; 387: 80–83.
Zelante L, Gasparini P, Estivill X, Melchionda S, D'Agruma L, Govea N, Mila M, Monica MD, Lutfi J, Shohat M, Mansfield E, Delgrosso K, Rappaport E, Surrey S, Fortina P . Connexin26 mutations associated with the most common form of non-syndromic neurosensory autosomal recessive deafness (DFNB1) in Mediterraneans. Hum Mol Genet 1997; 6: 1605–1609.
Carrasquillo MM, Zlotogora J, Barges S, Chakravarti A . Two different connexin 26 mutations in an inbred kindred segregating non-syndromic recessive deafness: implications for genetic studies in isolated populations. Hum Mol Genet 1997; 6: 2163–2172.
Denoyelle FD, Weil D, Maw MA, Wilcox SA, Lench NJ, Allen-Powell DR, Osborn AH, Dahl HH, Middleton A, Houseman MJ, Dode C, Marlin S, Boulila-ElGaied A, Grati M, Ayadi H, BenArab S, Bitoun P, Lina-Granade G, Godet J, Mustapha M, Loiselet J, El-Zir E, Aubois A, Joannard A, Petit C, et al. Prelingual deafness: high prevalence of a 30delG mutation in the connexin 26 gene. Hum Mol Genet 1997; 6: 2173–2177.
Kikuchi T, Kimura RS, Paul DL, Adams JC . Gap junctions in the rat cochlea: immunohistochemical ultrastructural analysis. Anat Embryol Berl 1995; 191: 101–118.
Goodenough DA, Jeffrey AG, Paul DL . Connexins, connexons, intercellular communication. Annu Rev Biochem 1996; 65: 475–502.
Simon AM, Goodenough DA . Diverse functions of vertebrate gap junctions. Trends Cell Biol 1998; 8: 477–483.
Xia JH, Liu CY, Tang BS, Pan Q, Huang L, Dai HP, Zhang BR, Xie W, Hu DX, Zheng D, Shi XL, Wang DA, Xia K, Yu KP, Liao XD, Feng Y, Yang YF, Xiao JY, Xie DH, Huang JZ . Mutations in the gene encoding gap junction protein beta-3 associated with autosomal dominant hearing impairment. Nat Genet 1998; 20: 370–373.
Richard G, White TW, Smith LE, Bailey RA, Compton JG, Paul DL, Bale SJ . Functional defects of Cx26 resulting from a heterozygous missense mutation in a family with dominant deaf-mutism palmoplantar keratoderma. Hum Genet 1998; 103: 393–399.
Maestrini E, Korge BP, Ocaña-Sierra J, Calzolari E, Cambiaghi S, Scudder P, Hovnanian A, Monaco A, Munro C . A missense mutation in connexin26, D66H, causes mutilating keratoderma with sensorineural deafness (Vohwinkel's syndrome) in three unrelated families. Hum Mol Genet 1999; 8: 1237–1243.
Heathcote K, Syrris P, Carter ND, Patton MA . A connexin-26 mutation causes a syndrome of sensorineural hearing loss in palmoplantar hyperkeratosis. J Med Genet 2000; 37: 50–51.
Kelsell DP, Di W-L, Houseman MJ . Connexin mutations in skin disease hearing loss. Am J Hum Genet 2001; 68: 559–568.
Estivill X, Fortina P, Surrey S, Rabionet R, Melchionda S, D'Agruma L, Mansfield E, Rappaport E, Govea N, Mila M, Zelante L, Gasparini P . Connexin 26 mutations in sporadic inherited sensorineural deafness. Lancet 1998; 351: 394–398.
Kelley PM, Harris DJ, Comer BC, Askew JW, Fowler T, Smith SD, Kimberling WJ . Novel mutations in the connexin 26 gene (GJB2) that cause autosomal recessive (DFNB1) hearing loss. Am J Hum Genet 1998; 62: 792–799.
Lench N, Houseman M, Newton V, Van Camp G, Mueller R . Connexin-26 mutations in sporadic non-syndromal sensorineural deafness. Lancet 1998; 351: 415.
Scott DA, Kraft ML, Carmi R, Ramesh A, Elbedour K, Yairi Y, Srisailapathy CR, Rosengren SS, Markham AF, Mueller RF, Lench NJ, Van Camp G, Smith RJ, Sheffield VC . Identification of mutations in the connexin 26 gene that cause autosomal recessive nonsyndromic hearing loss. Hum Mutat 1998; 11: 387–394.
Brobby GW, Muller-Myhsok B, Horstmann RD . Connexin 26 R143W mutation associated with recessive non-syndromic sensorineural deafness in Africa. N Engl J Med 1998; 338: 548–550.
Morell RJ, Kim HJ, Hood LJ, Goforth L, Friderici K, Fisher R, Van Camp G, Berlin CI, Oddoux C, Ostrer H, Keats B, Friedman TB . Mutations in the connexin 26 gene (GJB2) among Ashkenazi Jews with nonsyndromic recessive deafness. N Engl J Med 1998; 339: 1500–1505.
Green GE, Scott DA, McDonald JM, Woodworth GG, Sheffield VC, Smith RJH . Carrier rates in the Midwestern United States for GJB2 mutations causing inherited deafness. JAMA 1999; 281: 2211–2216.
Mueller RF, Nehammer A, Middleton A, Houseman M, Taylor GR, Bitner-Glindzciz M, Van Camp G, Parker M, Young ID, Davis A, Newton VE, Lench NJ . Congenital non-syndromal sensorineural hearing impairment due to connexin 26 gene mutations: molecular audiological findings. Int J Pediatr Otorhinolaryngol 1999; 50: 3–13.
Gasparini P, Rabionet R, Barbujani G, Melchionda S, Petersen M, Brondum-Nielsen K, Metspalu A, Oitmaa E, Pisano M, Fortina P, Zelante L, Estivill X . High carrier frequency of the 35delG deafness mutation in European populations. Genetic Analysis Consortium of GJB2 35delG. Eur J Hum Genet 2000; 8: 19–23.
Rabionet R, Zelante L, Lopez-Bigas N, D'Agruma L, Melchionda S, Restagno G, Arbones ML, Gasparini P, Estivill X . Molecular basis of childhood deafness resulting from mutations in the GJB2 (connexin 26) gene. Hum Genet 2000; 106: 40–44.
Sobe T, Vreugde S, Shahin H, Berlin M, Davis N, Kanaan M, Yaron Y, Orr-Urtreger A, Frydman M, Shohat M, Avraham KB . The prevalence expression of inherited connexin 26 mutations associated with nonsyndromic hearing loss in the Israeli population. Hum Genet 2000; 106: 50–57.
Wilcox SA, Saunders K, Osborne AH, Arnold A, Wunderlich J, Kelly T, Collins V, Wilcox LJ, McKinlay Gardner RJ, Kamarinos M, Cone-Wesson B, Williamson R, Dahl HH . High frequency hearing loss associated with mutations in the GJB2 gene. Hum Genet 2000; 106: 399–405.
Loffler J, Nekahm D, Hirst-Stadlmann A, Gunther B, Menzel HJ, Utermann G, Janecke AR . Sensorineural hearing loss the incidence of Cx26 mutations in Austria. Eur J Hum Genet 2001; 9: 226–230.
Gabriel H, Kupsch P, Sudendey J, Winterhager E, Jahnke K, Lautermann J . Mutations in the connexin26/GJB2 gene are the most common event in non-syndromic hearing loss among the German population. Hum Mutat 2001; 17: 521–522.
Hamelmann C, Amedofu GK, Albrecht K, Muntau B, Gelhaus A, Brobby GW, Horstmann RD . Pattern of connexin 26 (GJB2) mutations causing sensorineural hearing impairment in Ghana. Hum Mutat 2001; 18: 84–85.
Kelley PM, Cohn E, Kimberling W . Connexin 26: required for normal auditory function. Brain Res Rev 2000; 32: 184–188.
Rabionet R, Gasparini P, Estivill X . Molecular genetics of hearing impairment due to mutations in gap junction genes encoding beta connexins. Hum Mutat 2000; 16: 190–202.
Rabionet R, Gasparini P, Estivill X . 2001; http://www.iro.es/deafness/
Denoyelle F, Marlin S, Weil D, Moatti L, Chauvin P, Garabedian EN, Petit C . Clinical features of the prevalent form of childhood deafness, DFNB1, due to a connexin-26 gene defect: implications for genetic counseling. Lancet 1999; 353: 1298–1303.
Cohn ES, Kelley PM, Fowler TW, Gorga MP, Lefkowitz DM, Kuehn HJ, Schaefer GB, Gobar LS, Hahn FJ, Harris DJ, Kimberling WJ . Clinical studies of families with hearing loss attributable to mutations in the connexin 26 gene (GJB2/DFNB1). Pediatrics 1999; 103: 546–550.
Murgia A, Orzan E, Polli R, Martella M, Vinanzi C, Leonardi E, Arslan E, Zacchello F . Cx26 deafness: mutation analysis clinical variability. J Med Genet 1999; 36: 829–832.
Lerer I, Sagi M, Malamud E, Levi H, Raas-Rothschild A, Abeliovich D . Contribution of connexin 26 mutations to nonsyndromic deafness in Ashkenazi patients the variable phenotypic effect of the mutation 167delT. Am J Med Genet 2000; 95: 53–56.
Lefebvre PP, Van De Water TR . Connexins, hearing deafness: clinical aspects of mutations in the connexin 26 gene. Brain Res Rev 2000; 32: 159–162.
Wu BL, Lip V, Cox G, Korf B, Kenna M . Assessing the prevalence/spectrum of connexin 26 mutations and their phenotype in children with congenital sensorineural hearing loss (SNHL). The 10th International Congress of Hum Genet, Vienna, Austria, May 15–19, 2001.
Kenna MA, Wu BL, Cotanche DA, Korf BR, Rehm HL . Connexin 26 studies in patients with sensorineural hearing loss. Arch Otolaryngol Head Neck Surg 2001; 127: 1037–1042.
Marlin S, Garabedian E-N, Roger G, Moatti L, Matha N, Lewin P, Petit C, Denoyelle F . Connexin 26 gene mutations in congenitally deaf children: pitfalls for genetic counseling. Arch Otolaryngol Head Neck Surg 2001; 127: 927–933.
Lin D, Goldstein JA, Mhatre AN, Lustig LR, Pfister M, Lalwani AK . Assessment of denaturing high-performance liquid chromatography (DHPLC) in screening for mutations in connexin 26 (GJB2). Hum Mutat 2001; 18: 42–51.
Houseman MJ, Ellis LA, Pagnamenta A, Di W-L, Rickard S, Osborn A, Dahl H-H, Taylor GR, Bitner-Glindzicz M, Reardon W, Mueller RF, Kelsell DP . Genetic analysis of the connexin-26 M34T variant: identification of genotype M34T/M34T segregating with mild-moderate non-syndromic sensorineural hearing loss. J Med Genet 2001; 38: 19–24.
Prasad S, Cucci RA, Green GE, Smith RJH . Genetic testing for hereditary hearing loss: connexin 26 (GJB2) allele variants two novel deafness-causing mutations (R32C 645–648delTAGA). Hum Mutat 2000; 16: 502–508.
Antoniadi T, Gronskov K, Sand A, Pampanos A, Brondum-Nielsen K, Petersen MB . Mutation analysis of the GJB2 (connexin 26) gene by DGGE in Greek patients with sensorineural deafness. Hum Mutat 2000; 16: 7–12.
Cucci RA, Prasad S, Kelley P, Green GE, Storm K, Willocx S, Cohn ES, Van Camp G, Smith RJH . The M34T allele variant of connexins 26. Genet Test 2000; 4: 335–344.
Dahl HH, Saunders K, Kelly TM, Osborn AH, Wilcox S, Cone-Wesson B, Wunderlich JL, Du Sart D, Kamarinos M, Gardner RJ, Dennehy S, Williamson R, Vallance N, Mutton P . Prevalence nature of connexins 26 mutations in children with non-syndromic deafness. Med J Aust 2001; 175: 191–194.
Griffith AJ, Chowdhry AA, Kurima K, Hood LJ, Keats B, Berlin CI, Morell RJ, Friedman TB . Autosomal recessive nonsyndromic neurosensory deafness at DFNB1 not associated with the compound-heterozygous GJB2 (connexins 26) genotype M34T/167delT. Am J Hum Genet 2000; 67: 745–749.
Griffith AJ . Genetic analysis of the connexin-26 M34T variant. J Med Genet 2001; 38: e24.
Denoyelle F, Lina-Granade G, Plauchu H, Bruzzone R, Chaib H, Levi-Acobas F, Weil D, Petit C . Connexin 26 gene linked to a dominant deafness. Nature 1998; 393: 319–320.
Antonarakis SE, and the Nomenclature Working Group Recommendations for a nomenclature system for human gene mutations. Hum Mutat 1998; 11: 1–3.
del Castillo I, Villamar M, Moreno-Pelayo MA, del Castillo FJ, Alvarez A, Telleria D, Menendez I, Moreno F . A deletion involving the connexin 30 gene in nonsyndromic hearing impairment. N Engl J Med 2002; 346: 243–249.
Lerer I, Sagi M, Ben-Neriah Z, Wang T, Levi H, Abeliovich D . A deletion mutation in GJB6 cooperating with a GJB2 mutation in trans in non-syndromic deafness: a novel founder mutation in Ashkenazi Jews. Hum Mutat 2001; 18: 460.
Liu XZ, Xia XJ, Adams J, Chen ZY, Welch KO, Tekin M, Ouyang XM, Kristiansen A, Pandya A, Balkany T, Arnos K, Nance WE . Mutations in GJA1 (connexins 43) are associated with non-syndromic Autosomal recessive deafness. Hum Mol Genet 2001; 10: 2945–2951.
Acknowledgements
The authors thank the referring physicians and genetic counselors for their cooperation, and Pam Hawley and Hong Fang for their medical/technical assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Wu, BL., Lindeman, N., Lip, V. et al. Effectiveness of sequencing connexin 26 (GJB2) in cases of familial or sporadic childhood deafness referred for molecular diagnostic testing. Genet Med 4, 279–288 (2002). https://doi.org/10.1097/00125817-200207000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/00125817-200207000-00006
Keywords
This article is cited by
-
Phenotypic Heterogeneity in a DFNA20/26 family segregating a novel ACTG1 mutation
BMC Genetics (2016)
-
Connexinopathies: a structural and functional glimpse
BMC Cell Biology (2016)
-
Screening of genetic alterations related to non-syndromic hearing loss using MassARRAY iPLEX® technology
BMC Medical Genetics (2015)
-
A genotype–phenotype correlation in Sicilian patients with GJB2 biallelic mutations
European Archives of Oto-Rhino-Laryngology (2015)
-
Developing regional genetic counseling for southern Chinese with nonsyndromic hearing impairment: a unique mutational spectrum
Journal of Translational Medicine (2014)