Abstract
Purpose: Niemann-Pick disease type C (NP-C) is an autosomal recessive lipid storage disease manifested by an impairment in cellular cholesterol homeostasis. The clinical phenotype of NP-C is extremely variable, ranging from an acute neonatal form to an adult late-onset presentation. To facilitate phenotype-genotype studies, we have analyzed multiple Israeli NP-C families.
Methods: The severity of the disease was assessed by the age at onset, hepatic involvement, neurological deterioration, and cholesterol esterification studies. Screening of the entire NPC1 coding sequence allowed for molecular characterization and identification of disease causing mutations.
Results: A total of nine NP-C index cases with mainly neurovisceral involvement were characterized. We demonstrated a possible link between the severity of the clinical phenotype and the cholesterol esterification levels in fibroblast cultures following 24 hours of in vitro cholesterol loading. In addition, we identified eight novel mutations in the NPC1 gene.
Conclusions: Our results further support the clinical and allelic heterogeneity of NP-C and point to possible association between the clinical and the biochemical phenotype in distinct affected Israeli families.
Similar content being viewed by others
Main
Niemann-Pick disease type C (NP-C) is an autosomal recessive lipid storage disease manifested by an impairment in cellular cholesterol homeostasis (OMIM number 257220). The prevalence has been estimated at 1:150,000 in Europe, yet the incidence in early life is probably underestimated, because of nonspecific presentations and possible under-diagnosis. Acadians in Nova Scotia, individuals of Hispanic descent in Colorado and New Mexico, and a Bedouin group in Israel represent genetic isolates each with a common founder. In the Acadians of Nova Scotia, a milder variant of the disease that has been at first erroneously considered to be a distinct entity termed Niemann Pick disease type D (NPD), proved later by molecular analysis to be allelic to NP-C.1
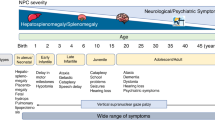
The disease is clinically characterized by progressive degeneration of the central nervous system with visceral accumulation of cholesterol and sphingomyelin. The clinical phenotype of NP-C is extremely variable ranging from an acute neonatal form, showing mainly liver involvement and rapid neurologic deterioration, to an adult late-onset presentation, with slowly progressive ataxia and a movement disorder. The late infantile and juvenile forms are considered to be the most common classical presentations with the insidious onset of ataxia, vertical supranuclear gaze palsy, and cognitive impairment in up to 80% of the patients.1
The underlying cellular defect is a disruption in the sterol trafficking, which leads to accumulation of free cholesterol within the lysosomal and late-endosomal compartment of the cell. The biochemical nature of NP-C became clear following the identification of a natural murine NP-C model presenting with degenerative lipid storage disease.2 The affected mice had elevated levels of unesterified cholesterol in various tissues. Although a defect in cholesterol esterification was shown in NP-C patients,3 acyl CoA:cholesterol acyltransferase (ACAT) deficiency was ruled-out.4 The accumulation of lysosomal unesterified cholesterol was found to be due to reduced release of free cholesterol from lysosomes to other cellular organelles such as plasma membrane and the Golgi apparatus.5,6 Hence, the definitive diagnosis of NP-C is based on the demonstration of abnormal cholesterol esterification in skin fibroblasts cultured with LDL-derived tritiated oleate. This assay provides the means for diagnosis of affected individuals, yet it cannot be utilized for the identification of carriers. Attempts to identify a correlation between the clinical phenotype and the severity of the disruption of cellular cholesterol homeostasis have been inconclusive.7–10 Although a “variant” biochemical phenotype was described for patients with the adult-onset presentation, no definitive correlation has been observed for the late infantile and juvenile forms.
The NPC1 gene has been cloned following its mapping to the long arm of chromosome 18 using linkage and positional cloning.11,12 The NPC1 cDNA sequence predicts a protein of 1,278 amino acids with an estimated molecular mass of 142 kDa. Recently, topological analysis of the NPC1 protein has revealed the existence of 13 transmembrane domains, 7 luminal loops, 6 cytoplasmic loops, and a cytoplasmic tail.13 To date, more than 100 NPC1 mutations, mostly missense, have been identified throughout the gene, with no apparent hot spots.14–16 Most patients with NPC1 mutations are compound heterozygotes with private unique mutations. The two known exceptions are a common I1061T mutation found in the Hispanic population in the upper Rio Grande Valley in the southwestern United States, and in the United Kingdom, and France15 and the mutation G992W in the Acadian population of Nova Scotia.17
According to accumulated data so far, NPC1 is associated with approximately 80% of known cases; however, both linkage techniques and cellular complementation studies have shown the existence of genetic heterogeneity, providing proof for the presence of an additional disease-causing gene.18 Recently, HE1 encoding a ubiquitously expressed lysosomal cholesterol binding protein was identified as a second gene for NP-C.19 NP-C patients from both complementation groups demonstrate similar clinical and biochemical phenotypes, suggesting that NPC1 and HE1 may interact or function sequentially in a common metabolic pathway.
NP-C is observed in a relatively high frequency in Israel,20 especially among the Israeli non-Jewish population comprising Muslim Arabs, Bedouins, Druze, and Samaritans subgroups. A relatively high rate of autosomal recessive disorders is observed as a consequence of the high consanguinity rate among these various groups. In this study, we characterized the clinical, biochemical, and molecular features of NP-C in Israel.
PATIENTS AND METHODS
Patients
The analyzed patients were part of a larger group of 13 affected individuals that were referred to the Biochemical Genetics laboratory in the Department of Human Genetics with a tentative clinical diagnosis of NP-C. This study was approved by the Institutional Review Board in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from the participants in the study or from their parents. The laboratory at the Hadassah University Hospital serves as a national referral lab for the diagnosis of lysosomal storage disorders.
Fibroblast culture and biochemical studies
Skin biopsy was obtained from affected individuals. Fibroblasts were propagated as monolayers in 37°C, 5% CO2, humidified incubator using minimal essential medium (MEM) supplemented with 10% (v/v) fetal calf serum and antibiotics according to standard protocols. [3H]Oleic acid mixture was prepared by sonicating 5 mCi [3H]oleic acid and 16.75 mg of sodium oleate in 4.4 mL of 14% fatty acid free bovine serum. Cholesteryl ester synthesis was assayed as follows. Normal and patients' cells (in 4th passage) were grown in T-25 flasks containing Eagles' MEM medium with 5% bovine lipoprotein-deficient serum (LPDS) obtained from Sigma (Medium A). After 4 days, the medium was replaced by either 2 mL of medium A + 0.02 mL of [3H]oleic acid mixture (2 flasks), or medium A + 0.02 mL of [3H]oleic acid mixture + 100 μg of human LDL (Biomedical Technologies)/1 mL of Eagles' MEM medium (Medium B). Cells were incubated for 4.5 and 24 hours at 37°C after which the cells were harvested and homogenized by ultrasonication in 0.5 mL of distilled water. For lipid extraction, 0.1 mL of the homogenate was added to 1 mL of chloroform:methanol (2:1). The lipid phase was dried under nitrogen and dissolved in 0.1 mL of chloroform:methanol (2:1) of which 0.025 mL were spotted on plastic Silica Gel 60 thin layer chromatography plates. The plates were developed in hexane:ethyl ether:glacial acetic acid (90:10:1, v/v/v). The radioactive cholesteryl ester was visualized by exposing the plates to iodine vapors. The cholesteryl ester spot was scraped from the plate, and radioactivity was counted. Cholesteryl ester formation was determined by subtracting the counts obtained from the extracted lipids incubated in medium A from the counts obtained from the extracted cells that were incubated in medium B. The values were expressed as cholesteryl 3H-oleate/mg protein for 4.5 and 24 hours of incubation.
Molecular studies
Total RNA was extracted from fibroblast monolayers using the TRI Reagent® (Molecular Research Center, Inc.) according to manufacturer's instructions. Reverse transcription was performed using AMV Reverse Transcriptase (Promega) and standard protocols. The NPC1 cDNA was amplified in overlapping fragments, checked by agarose gel electrophoresis, and purified with the AGTC Gel Filtration Cartridges (Edge BioSystems) according to manufacturer's instructions. Sequencing reactions were performed with 50 ng of purified PCR product, 10 pmol primer, and 8 μL of ABI PRISM® BigDye TM Terminator Cycle Sequencing Kits with AmpliTaq® DNA Polymerase (Applied Biosystems). Automated sequencing was performed on an ABI PRISM® 310 Genetic Analyzer and processed by means of ABIView version 3.0 software. Every mutation was confirmed by sequencing the product of an independent PCR reaction. Restriction digests were performed in those cases where the mutation introduced a new restriction site or alternatively abolished a site present in the wild-type DNA. Base-pair numbers used refer to GenBank accession AF002020. In order to rule out the possibility of polymorphisms, 100 chromosomes obtained from healthy individuals from similar ethnic backgrounds were screened for the presence of these molecular changes.
RESULTS
Clinical features of NP-C patients
We characterized 9 of 13 families that were referred to our department for investigation because of clinical suspicion of NP-C. In 5 of the families, there were more than one affected sibling. In total, we analyzed 19 affected NP-C patients, of which 12 were assayed biochemically. Demographic and clinical characteristics of the 9 index patients are shown in Table 1. In 8 of 9 families, parents' consanguinity resulted in homozygous individuals. Two of 9 of the families were of Jewish origin, 1 was Christian, and 6 were of Muslim Arab ancestry. Mostly, the patients were investigated because of hepatosplenomegaly (8 of 9), neonatal jaundice (4 of 9), and neurological symptoms that were identified during the first 2 years of life (4 of 9). The various clinical forms ranged from neonatal and infantile to adult presentations (Table 1). In 4 families, we observed patients with a juvenile onset of symptoms (SB, SG, AM, SL). In 3 of these families (SB, SG, AM), consanguinity at the first cousin level was demonstrated. One previously described patient (AN) had an adult onset NP-C.21 This patient was investigated at first because of hepatosplenomegaly and mild ataxia. The presence of supranuclear ophthalmoplegia and “sea-blue” histiocytes at bone marrow biopsy led to clinical suspicion of NP-C. The provisional diagnosis of NP-C was based on filipin staining and linkage analysis. An additional affected family (ARZ) was previously described due to the striking phenotypic variation within family members.22 Three NP-C affected individuals died following several months of progressive hepatic failure, while another child presented with hepatosplenomegaly and no other abnormality to the age of 30 months. Neurologic deterioration developed from that point with progressive mental retardation and severe pneumonitis leading to death at the age of 5 years. Considerable variability in the clinical presentation was also observed in the ABR kinship. In addition to the currently investigated ABR patients, two previously confirmed NP-C cases presenting with hydrops fetalis and hepatomegaly were reported.23
Esterification assays correlate with the clinical phenotype
The biochemical diagnosis of NP-C in fibroblasts was done using both filipin fluorescence tests (data not shown), and esterification assays. We performed the esterification measurements following 4.5 and 24 hours incubation periods. Two groups were distinctive following 4.5 hours of incubation: one that showed low esterification levels (0.88 ± 0.85 and 2.10 ± 1.96 nmol/mg protein) and corresponded to the severe infantile and the intermediate juvenile clinical phenotypes; and a second group with a “variant” biochemical phenotype that did not differ at large from normal controls (23.40 ± 23.00 as compared with 50.00 ± 32.00 nmol/mg protein). Following 24 hours of incubation, we were able to classify three biochemical phenotypes: a “variant” phenotype appearing in adult-onset patients with no differences in cholesterol esterification values when compared to the control (627 ± 247 and 738 ± 262 nmol/mg protein, respectively); a “severe” biochemical phenotype corresponding to the early infantile phenotype that showed no increase in esterification levels following 24 hours of incubation (26.00 ± 18.20 nmol/mg protein); and an “intermediate” biochemical phenotype that clearly demonstrated a recovery in cholesterol ester production following 24 hours of incubation and was distinguishable from both the “variant” phenotype and the severe infantile biochemical phenotype (Table 2). Although these results are indicative for possible correlation between the clinical and the biochemical phenotypes, the small number of assayed patients preclude drawing statistically significant conclusions.
Molecular characterization of Israeli NPC patients
Table 1 documents the various mutations that were detected in multiple NP-C patients. Of the 13 index patients that were analyzed, we characterized NPC1 mutations in 9 (69%). The mutations were identified in the various clinical phenotypes of NP-C. In order to confirm that these indeed are mutations and not polymorphisms, we have screened a total of 100 chromosomes from 50 independent individuals that belong to similar ethnic groups and found none of these changes among healthy individuals.
We observed both missense and nonsense mutations spread throughout the gene with no apparent clustering. The adult-onset phenotype (AN) was homozygous for a missense conversion of an aliphatic valine for alanine. Within the early infantile group (SA, MH, ABR), there were both nonsense and missense homozygotes. The only compound heterozygote belonged to the juvenile group (SL) having both nonsense and missense alleles.
A G992W mutation previously detected in the Nova Scotian genetic isolate17 was found in two independent Muslim Arab families originating from the northern part of Israel (AM and SG). We examined four affected individuals in these families and found the phenotypic severity to be similar to that previously described in the Nova Scotian patients.24
DISCUSSION
In this study, we characterized the clinical, molecular, and biochemical features of Israeli NP-C patients. We show that in our patients NP-C has a striking inter- and intrafamilial phenotypic variability. This variability may result from either genetic or environmental factors.
In accordance with previous observations that showed a high prevalence of the severe infantile neurological form in the Middle East,8 we observed in four of the nine characterized families a phenotype conforming to the neonatal appearance of jaundice and rapid neurological deterioration.
Cholesterol esterification assays following 4.5 and 24 hours of incubation allowed us to differentiate among three distinct biochemical patterns: (I) an ongoing block of esterification following 4.5 and 24 hours of incubation with LDL-cholesterol, (II) a block in esterification that partially resolved following 24 hours of incubation, and (III) a normal esterification profile following 4.5 and 24 hours that was observed in affected adult-onset patients from the AN family. Following 24 hours of incubation, three distinctive biochemical phenotypes emerged. A previously recorded “variant” phenotype that did not differ from the normal control and two additional biochemical phenotypes that correlated with the clinical findings. In patients with severe infantile course (MH, ABR, SA), we found reduced levels of esterification that did not increase following 24 hours of incubation with LDL and H3-oleic acid. In comparison, in patients with a moderate phenotype represented by juvenile onset of clinical symptoms (SB, AM, SG), we observed a severe esterification block following 4.5 hours of incubation, as previously shown,7,8 with partial removal of the block following 24 hours of incubation was seen (Table 2). This may point to either residual activity of the NPC1 protein or to contribution of additional proteins participating in cellular sterol trafficking. The attempted correlation between the clinical and the biochemical phenotype is based on 12 assayed affected individuals and, thus, needs validation by adding more patients. This may help in the utilization of the biochemical tests as means for predicting the disease prognosis. Our findings confirm previous reports that focused on the differences in esterification and cholesterol homeostasis between cells obtained from patients with the classical NP-C phenotype as compared with cells obtained from the Nova Scotian milder phenotype.9,10 Indeed, two individuals with “moderate” biochemical phenotype (AM, SG) had the same mutation as that described in the Nova Scotian genetic isolate17,24 (Table 1).
In accordance with the high degree of consanguinity among our tested population, we found 8 of the 9 families characterized, to be homozygotes. We identified eight novel mutations and one previously described mutation. Homozygous patients offer an opportunity to study the phenotypic effect of specific molecular changes. Among severely affected patients, we identified one nonsense mutation (3347 del TC) truncating the protein within the 9th transmembrane domain, and three missense mutations. C63R is positioned in the luminal N-terminus of the NPC1 protein proximal to the first transmembrane domain. R404Q is located to the luminal side of the NPC1 protein between the 2nd and 3rd transmembrane domains in a region that is predicted to harbor several potential N-glycosylation sites. G1012D, which is associated with the severe phenotype, is located in the luminal side between the 8th and 9th transmembrane domains in the same region as is the A927 V mutation that was identified within the mildly affected phenotype. Of the homozygous mutations causing an intermediate phenotype, N1156S and G992W are located within the luminal portion of the protein between the 10th and 11th, and the 8th and 9th transmembrane domains, respectively. Thus, based on our study, no obvious correlation between the site of the molecular defect and the clinical phenotype can be determined.
Of the various NP-C mutations identified within the Israeli families, 7 were found to be private and 2 were common to more than one family. One of the common mutations, R404Q, was identified in several affected individuals originating from a Bedouin isolate in the Southern part of Israel. This mutation is easily detected using an Msp I restriction analysis that may be useful for carrier screening. It should be noted that, in the Bedouin society, marriages are often prearranged by parents, and there is a known reluctance for prenatal diagnosis and termination of pregnancies.25–27 Thus, by administering proper information and counseling, NP-C genetic screening could be applied within this isolate.
An additional common mutation, G992W, was detected in two distinct nonrelated families that originated from the northern part of Israel. This mutation was previously described as causing the Nova Scotia variant.24 The clinical and biochemical characteristics of the individuals with the G992W mutation is similar to that previously reported. It remains to be shown whether this mutation occurred twice or results from a common founder.
An important aspect of molecular diagnosis applies to cases with adult onset of symptoms. In these patients, the known biochemical assays do not allow adequate diagnosis and cannot be applied for prenatal diagnosis.21,28 Thus, molecular diagnosis of the specific mutation aids both in direct diagnosis of affected individuals and in accurate detection of carriers among this highly consanguineous population.
It is interesting to note that, although three of our affected NP-C individuals originated from villages within a small geographic area, each had a distinct mutation. This finding has been previously described and discussed with regard to other autosomal recessive disorders, mainly Hurler (MIM 252800),29 primary hyperoxaluria type 1 (PH1 MIM 259900),30 and metachromatic leukodystrophy (MLD MIM 250100).31 The finding of multiple recessive mutations in a single gene as the cause for an increased disease frequency may result from selective advantage for heterozygotes, although no evidence for this has been shown. A plausible possibility is that each newly occurring recessive mutation in a distinct homogeneous population could lead to a homozygous affected individual within a small number of generations due to the high rate of consanguinity in families in combination with a large number of offspring.
References
Patterson MC, Vanier MT, Suzuki K, Morris JA, Carstea E, Neufeld EB, Blanchette-Mackie EJ, Pentchev PG . Niemann-Pick disease type C: a lipid trafficking disorder. In: Scriver SR, Beaudet AL, Valle D, Sly WS, Childs B, Kinzler KW, Vogelstein B editors. The metabolic and molecular bases of inherited disease. New York: McGraw-Hill, 2001: 3611–3633.
Pentchev PG, Boothe AD, Kruth HS, Weintroub H, Stivers J, Brady RO . A genetic storage disorder in BALB/C mice with a metabolic block in esterification of exogenous cholesterol. J Biol Chem 1984; 259: 5784–5791.
Pentchev PG, Comly ME, Kruth HS, Vanier MT, Wenger DA, Patel S, Brady RO . A defect in cholesterol esterification in Niemann-Pick disease (type C) patients. Proc Natl Acad Sci USA 1985; 82: 8247–8251.
Pentchev PG, Kruth HS, Comly ME, Butler JD, Vanier MT, Wenger DA, Patel S . Type C Niemann-Pick disease. A parallel loss of regulatory responses in both the uptake and esterification of low density lipoprotein-derived cholesterol in cultured fibroblasts. J Biol Chem 1986; 261: 16775–16780.
Pentchev PG, Comly ME, Kruth HS, Tokoro T, Butler J, Sokol J, Filling-Katz M, Quirk JM, Marshall DC, Patel S, Vanier MT, Brady RO . Group C Niemann-Pick disease: faulty regulation of low-density lipoprotein uptake and cholesterol storage in cultured fibroblasts. FASEB J 1987; 1: 40–45.
Blanchette-Mackie EJ, Dwyer NK, Amende LM, Kruth HS, Butler JD, Sokol J, Comly ME, Vanier MT, August JT, Brady RO, Pentchev PG . Type-C Niemann-Pick disease: low density lipoprotein uptake is associated with premature cholesterol accumulation in the Golgi complex and excessive cholesterol storage in lysosomes. Proc Natl Acad Sci USA 1988; 85: 8022–8026.
Vanier MT, Pentchev P, Rodriguez-Lafrasse C, Rousson R . Niemann-Pick disease type C: an update. J Inherit Metab Dis 1991; 14: 580–595.
Vanier MT, Rodriguez-Lafrasse C, Rousson R, Duthel S, Harzer K, Pentchev PG, Revol A, Louisot P . Type C Niemann-Pick disease: biochemical aspects and phenotypic heterogeneity. Dev Neurosci 1991; 13: 307–314.
Byers DM, Douglas JA, Cook HW, Palmer FB, Ridgway ND . Regulation of intracellular cholesterol metabolism is defective in lymphoblasts from Niemann-Pick type C and type D patients. Biochim Biophys Acta 1994; 1226: 173–180.
Sidhu HS, Rastogi SA, Byers DM, Cook HW, Palmer FB, Spence MW . Cultured fibroblasts from patients with Niemann-Pick disease type C and type D exhibit distinct defects in cholesterol esterification. Biochim Biophys Acta 1992; 1124: 29–35.
Carstea ED, Polymeropoulos MH, Parker CC, Detera-Wadleigh SD, O'Neill RR, Patterson MC, Goldin E, Xiao H, Straub RE, Vanier MT, Brady RO, Pentchev PG . Linkage of Niemann-Pick disease type C to human chromosome 18. Proc Natl Acad Sci USA 1993; 90: 2002–2004.
Carstea ED, Morris JA, Coleman KG, Loftus SK, Zhang D, Cummings C, Gu J, Rosenfeld MA, Pavan WJ, Krizman DB, Nagle J, Polymeropoulos MH, Sturley SL, Ioannou YA, Higgins ME, Comly M, Cooney A, Brown A, Kaneski CR, Blanchette-Mackie EJ, Dwyer NK, Neufeld EB, Chang TY, Liscum L, Strauss JF, Ohno K, Zeigler M, Carmi R, Sokol J, Markie D, O'Neill RR, van Diggelen OP, Elleder M, Patterson MC, Brady RO, Vanier MT, Pentchev PG, Tagle DA . Niemann-Pick C1 disease gene: homology to mediators of cholesterol homeostasis. Science 1997; 277: 228–231.
Davies JP, Ioannou YA . Topological analysis of Niemann-Pick C1 protein reveals that the membrane orientation of the putative sterol-sensing domain is identical to those of 3-hydroxy-3-methylglutaryl-CoA reductase and sterol regulatory element binding protein cleavage-activating protein. J Biol Chem 2000; 275: 24367–24374.
Greer WL, Dobson MJ, Girouard GS, Byers DM, Riddell DC, Neumann PE . Mutations in NPC1 highlight a conserved NPC1-specific cysteine-rich domain. Am J Hum Genet 1999; 65: 1252–1260.
Millat G, Marcais C, Rafi MA, Yamamoto T, Morris JA, Pentchev PG, Ohno K, Wenger DA, Vanier MT . Niemann-Pick C1 disease. the I1061T substitution is a frequent mutant allele in patients of Western European descent and correlates with a classic juvenile phenotype. Am J Hum Genet 1999; 65: 1321–1329.
Yamamoto T, Nanba E, Ninomiya H, Higaki K, Taniguchi M, Zhang H, Akaboshi S, Watanabe Y, Takeshima T, Inui K, Okada S, Tanaka A, Sakuragawa N, Millat G, Vanier MT, Morris JA, Pentchev PG, Ohno K . NPC1 gene mutations in Japanese patients with Niemann-Pick disease type C. Hum Genet 1999; 105: 10–16.
Greer WL, Riddell DC, Gillan TL, Girouard GS, Sparrow SM, Byers DM, Dobson MJ, Neumann PE . The Nova Scotia (type D) form of Niemann-Pick disease is caused by a G3097–>T transversion in NPC1. Am J Hum Genet 1998; 63: 52–54.
Vanier MT, Duthel S, Rodriguez-Lafrasse C, Pentchev P, Carstea ED . Genetic heterogeneity in Niemann-Pick C disease: a study using somatic cell hybridization and linkage analysis. Am J Hum Genet 1996; 58: 118–125.
Naureckiene S, Sleat DE, Lackland H, Fensom A, Vanier MT, Wattiaux R, Jadot M, Lobel P . Identification of HE1 as the second gene of Niemann-Pick C disease. Science 2000; 290: 2298–2301.
Zlotogora J, Chemke J . Medical genetics in Israel. Eur J Hum Genet 1995; 3: 147–154.
Lossos A, Schlesinger I, Okon E, Abramsky O, Bargal R, Vanier MT, Zeigler M . Adult-onset Niemann-Pick type C disease. Clinical, biochemical, and genetic study. Arch Neurol 1997; 54: 1536–1541.
Yatziv S, Leibovitz-Ben Gershon Z, Ornoy A, Bach G . Clinical heterogeneity in a sibship with Niemann-Pick disease type C. Clin Genet 1983; 23: 125–131.
Meizner I, Levy A, Carmi R, Robinsin C . Niemann-Pick disease associated with nonimmune hydrops fetalis. Am J Obstet Gynecol 1990; 163: 128–129.
Winsor EJ, Welch JP . Genetic and demographic aspects of Nova Scoti Niemann-Pick disease (type D). Am J Hum Genet 1978; 30: 530–538.
Jaber L, Dolfin T, Shohat T, Halpern GJ, Reish O, Fejgin M . Prenatal diagnosis for detecting congenital malformations: acceptance among Israeli Arab women. Isr Med Assoc J 2000; 2: 346–350.
Jaber L, Shohat M, Halpern GJ . Demographic characteristics of the Israeli Arab community in connection with consanguinity. Isr J Med Sci 1996; 32: 1286–1289.
Sheiner E, Shoham-Vardi I, Weitzman D, Gohar J, Carmi R . Decisions regarding pregnancy termination among Bedouin couples referred to third level ultrasound clinic. Eur J Obstet Gynecol Reprod Biol 1998; 76: 141–146.
Vanier MT, Rodriguez-Lafrasse C, Rousson R, Gazzah N, Juge MC, Pentchev PG, Revol A, Louisot P . Type C Niemann-Pick disease: spectrum of phenotypic variation in disruption of intracellular LDL-derived cholesterol processing. Biochim Biophys Acta 1991; 1096: 328–37.
Bach G, Moskowitz SM, Tieu PT, Matynia A, Neufeld EF . Molecular analysis of Hurler syndrome in Druze and Muslim Arab patients in Israel: multiple allelic mutations of the IDUA gene in a small geographic area. Am J Hum Genet 1993; 53: 330–338.
Rinat C, Wanders RJ, Drukker A, Halle D, Frishberg Y . Primary hyperoxaluria type I: a model for multiple mutations in a monogenic disease within a distinct ethnic group. J Am Soc Nephrol 1999; 10: 2352–2358.
Heinisch U, Zlotogora J, Kafert S, Gieselmann V . Multiple mutations are responsible for the high frequency of metachromatic leukodystrophy in a small geographic area. Am J Hum Genet 1995; 56: 51–57.
Acknowledgements
This study was supported in part by a research grant from the Chief Scientist of the Israeli Ministry of Health. (4626 to VM)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Meiner, V., Shpitzen, S., Mandel, H. et al. Clinical-biochemical correlation in molecularly characterized patients with Niemann-Pick type C. Genet Med 3, 343–348 (2001). https://doi.org/10.1097/00125817-200109000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/00125817-200109000-00003
Keywords
This article is cited by
-
Niemann–Pick disease type C in Palestine: genotype and phenotype of sixteen patients and report of a novel mutation in the NPC1 gene
BMC Medical Genomics (2021)
-
Different Niemann-Pick C1 Genotypes Generate Protein Phenotypes that Vary in their Intracellular Processing, Trafficking and Localization
Scientific Reports (2019)
-
Niemann-Pick Disease Type C: Mutation Spectrum and Novel Sequence Variations in the Human NPC1 Gene
Molecular Neurobiology (2019)
-
Pulmonary involvement in Niemann-Pick C type 1
European Journal of Pediatrics (2018)
-
An uncommon inheritance pattern in Niemann-Pick disease type C: identification of probable paternal germline mosaicism in a Mexican family
BMC Neurology (2016)