Abstract
Purpose
To assess OCT angiography (OCTA) effectiveness at detecting choroidal neovascularization (CNV) in cases of suspected neovascular age related macular degeneration (nAMD), chronic central serous retinopathy (cCSR) and pathological myopia compared to FFA and how it compares to a multimodal approach (OCT, FFA and ICGA) for detecting the vascular network.
Methods
This was a retrospective observational cohort study of patients who had clinical and/or OCT findings suggestive of CNV, having further investigation with FFA, with or without ICG, and had same day OCTA using the Heidelberg Spectralis OCT2 beta angiography module. Multimodal imaging interpretation was compared to OCTA images. OCTA images were also analysed for inter-rater reliability (using kappa statistic). The diagnostic accuracy of OCTA was compared to FFA (using Cochran’s Q, p<0.05). OCTA was also compared to a multimodal approach in defining a vascular network.
Results
Overall sensitivity of OCTA compared to FFA was 71% and specificity of 81% (p=0.108). Subgroup analysis for OCTA vs FFA for detecting classic nAMD/type II CNV sensitivity was 100% and specificity of 76% (p<0.05). OCTA vs FFA for detecting occult nAMD/type-I CNV sensitivity was 47% and specificity of 76%, (p=0.248). OCTA was better than FFA at defining a vascular network overall, when OCT was suspicious (59% vs 49%).
Conclusions
OCTA was better at detecting classic nAMD/type II CNV compared to FFA and for defining a vascular network in nAMD compared to FFA and ICGA. It was able to aid in making the diagnosis in cases where evidence of CNV was uncertain following FFA/ICGA.
Similar content being viewed by others
Introduction
The development and progression of choroidal neovascularisation (CNV) can lead to rapid loss of visual function if not treated promptly. Guidelines for assessment of CNV include imaging the macula with optical coherence tomography (OCT) and fundus fluorescein angiography (FFA).1 OCT is very sensitive at detecting changes in the macular structure and often findings may be suggestive of CNV. However, it is not able to define a vascular network.2 FFA is used as the gold standard for defining the presence of CNV. The pattern of angiographic leak defines the lesion, such as the characteristic changes seen in classic and occult neovascular age related macular degeneration (nAMD).3, 4, 5 Although vascular networks maybe seen, rapid leakage from the CNV lesion often results in the loss of definition. FFA is an invasive procedure, which has a small risk of anaphylaxis. There can be a delay from first presentation to FFA being performed due to practical constraints, which can delay treatment, potentially affecting patient visual outcomes.
OCT angiography (OCTA) represents a fast, new imaging modality, which through the principles of OCT defines the retinal vascular structure, by using sequential B-scans to create a map of blood flow.6 It has been shown to be a good diagnostic test for detecting CNV in various retinal conditions, in a small number of publications.4, 7, 8 However, there are limitations with the image quality due to motion and projection artefacts, creating difficulty in determining whether neovascularisation is accurately visualized.9
There are now various commercial devices available using spectral domain and swept source OCTA.10, 11, 12
In our study, we assessed the diagnostic capability of the new Heidelberg (experimental) OCTA device for detecting CNV in anti-VEGF treatment naive patients compared to a standard multimodal approach. The OCTA images were compared with findings from FFA, indocyanine green angiography (ICGA) and OCT in eyes suspected to have CNV. We assessed the sensitivity and specificity of OCTA vs the gold standard of FFA for detecting CNV. We also reviewed the ability of OCTA to discern a clear vascular network compared to FFA and ICGA, when the OCT was suggestive of CNV.
Materials and methods
Study design
This was a retrospective, observational cohort study. Patients were seen consecutively between May 2016 and December 2016, at a tertiary Ophthalmology centre in the Royal Victoria Infirmary, Newcastle-upon-tyne, United Kingdom. There was prospective selection of the cohort with clinical information review, and then imaging with further clinical information was reviewed retrospectively. The research and development office at the Newcastle-upon-Tyne Hospitals Foundation Health Trust approved this study. This study followed the principles of the Declaration of Helsinki.
Study population
All anti-vascular endothelial growth factor (VEGF) treatment naive patients who had clinical and/or OCT findings suggestive of choroidal neovascularisation (CNV) were eligible for the study. Suspected CNV cases due to nAMD (classic, occult, retinal angiomatous proliferation (RAP), polypoidal choroidal vasculopathy (PCV)), chronic CSR (cCSR) or pathological myopia were eligible for the study. Ophthalmologists had performed the clinical examination, with slit-lamp biomicroscopy, independent of the study, as part of routine clinical practice. The patient cohort was from eye casualty as well as ophthalmology clinics. Patients were excluded if they had concomitant ophthalmology conditions such as media opacities which limited the ability to take OCT, FFA, ICGA, and OCTA, or if they had other causes of suspected CNV.
Traditional multimodal imaging
All patient underwent FFA, with or without ICGA. The OCT, FFA, and ICGA images were acquired using Heidelberg Spectralis HRA and OCT (Heidelberg Engineering, Heidelberg, Germany). The OCT was performed on the same day or within a week before FFA with or without ICGA, without therapeutic intervention in the interim.
OCT angiography
The eligible cohort of patients, whose clinical information and OCTs were reviewed prospectively, were selected by the clinical investigators (Taha Soomro (TS) and James Talks (SJT)) and had same day OCTA centered around the macula.
The Heidelberg Spectralis OCT2 beta angiography module (Heidelberg Engineering, Heidelberg, Germany) was used to acquire OCTA images. It took 85 000 A scans per second with a bandwidth of 50 nm. 15 × 10o (4.3 × 2.9 mm) area volume scans were taken with a variable number of B-scans taken (ranging from 131 to 261), at a resolution of 11 μm. A full spectrum amplitude decorrelation algorithm developed by Heidelberg Engineering was applied onto sequential B scans to obtain an OCT-B angiogram. The en-face OCTA was derived directly from this. The Heidelberg automated real time (ART) and Trutrack system was employed to reduce signal-to-noise ratio and motion artefact.9, 13 Three-dimensional OCTA images as well as cross sectional OCT B images were co-registered together, with automatic segmentation of the layers of the retinal pigment epithelium (RPE) and choroid. The photography department performed all the FFA, ICGA, OCT and OCTA imaging. All images from the different imaging modalities were used, even if the image quality was affected by artefact, with a pragmatic approach.
Image interpretation and analysis
The two clinical investigators, who were medical retina specialists with experience of using the Heidelberg OCTA, performed the image interpretation and analysis (SJT and TS).
The two sets of imaging, OCTA and traditional multimodal imaging (FFA, ICGA and OCT) were independently graded by TS and SJT. OCTA was initially assessed, with a 1-week interim before assessing multimodal imaging. This was done in order to limit confirmation bias from the results of OCTA compared to traditional multimodal imaging. The investigators were blinded to clinical information whilst grading OCTA images. Grading was split in a pragmatic manner between the two investigators. Open adjudication was done for particularly difficult cases. Inter-rater analysis was performed to confirm the reliability of grading between the two investigators.
To analyse the images automated segmentation lines had to be altered to delineate the upper and lower margins of choroidal neovascular networks. Segmented slabs of 30–50 μm were used, set at the level of Bruch’s membrane. These were moved through the enface layers of the OCTA and correlated with the cross sectional OCT findings on the OCTA platform, with allowance made for projection artefacts and areas of loss of RPE. Additionally, to detect for RAPs, 30–50 μm slabs were reviewed of the whole retina, to the level of the choriocapillaris, in each case to define the vascular network.8 In cases where CNV was seen on OCTA but not clearly defined on FFA, a repeat OCTA and OCT was performed after anti-VEGF treatment to check for response, to help confirm the presence of CNV.
The diagnosis of CNV in these conditions was based on established FFA findings, which are found to correlate closely to anatomical findings i.e. classic nAMD CNV being a type 2/subretinal lesion, occult nAMD being a type 1/sub RPE lesion, RAP nAMD being an evolving chorioretinal anastomosis, PCV being sub RPE or choroidal polyps with branching vascular networks, myopic CNV typically showing subretinal lesions and cCSR related CNV showing sub RPE related CNV, usually in the context of a pigment epithelial detachment (PED).14, 15, 16, 17, 18
The FFA definition of classic nAMD (type 2 CNV) shows either an early lacy hyperfluorescence with increasing hyperfluorescence, or focal hyperfluorescent leaks in the case of PCV or RAP.5, 15 Occult nAMD (type 1 CNV), where there is no clear vascular network on FFA, shows stippled hyperfluorescence (fibrovascular PED) with associated leak or late leakage of unknown source.8, 19 Pathological myopia CNV has similar characteristics to classic nAMD CNV, whilst cCSR with CNV has a similar angiographic profile to occult nAMD CNV.17, 20
The ICGA findings of CNV related to nAMD, particularly for PCV or RAP, pathological myopia and cCSR are characterized as a neovascular network, focal hyperfluorescent ‘hot spots’ or plaques.15, 16, 17, 21
Although OCT features are not confirmative for types of CNV, we looked at the literature for common findings that define the different conditions on OCT.
An OCT showing a PED, with or without subretinal fluid, was suggestive of occult nAMD-, PCV- or cCSR-related CNV, depending on the clinical context and other associated OCT features.14, 16, 22 Classic nAMD CNV typically shows subretinal fluid with subretinal thickening.14, 22 RAPs can show solitary intraretinal cystic spaces, which can develop into showing subretinal fluid and PEDs.14, 21 Myopic CNV can show RPE elevation, with possible associated fluid and PEDs.17
The OCTA definitions of CNV were based on various studies for occult nAMD and classic nAMD, which either have well-circumscribed networks (described as lacy-wheel, sea fan, or medusa head shaped) or poorly circumscribed networks (filamentous).8, 13 These definitions also applied to cCSR related CNV and pathological myopia related CNV.17, 20 For RAP, the OCTA definition was the finding of tufts in the outer retinal segment seen arising from the deep retinal plexus, which maybe associated with evolving sub RPE neovascularisation.21 PCV on OCTA was found by seeing abnormal vascular changes at the sub RPE level/Bruch’s membrane.16
Statistical analysis
The photography department collated all the OCTA images taken of the patients with suspected choroidal neovascularisation due to nAMD, cCSR and pathological myopia during the study period. The images were collected in JPEG form, with all clinical information hidden. All OCTA images were numbered, and 20 were randomly selected using an online random number generator (available at https://www.random.org/). Inter-rater reliability of the two specialists (SJT and TS) was determined, by a blinded grading of the 20 OCTA images. Inter-rater reliability was assessed using the kappa statistic (κ).
Sensitivity and specificity analysis was performed; comparing OCTA to the gold standard of FFA in detecting choroidal neovascularisation, with 95% confidence intervals calculated (% 95 CIs). Cochran’s Q test was used to confirm the difference in rate of choroidal neovascularisation detection between OCTA and FFA, with p<0.05 being statistically significant. Concordance of OCT findings with FFA detection of a vascular network, OCTA detection of a vascular network and ICGA detection of a vascular network was also compared.
Descriptive statistics were defined with means and standard deviation (SD). Statistical information was calculated using SPSS 20.0 for Windows package.
Results
Patient characteristics
There were 93 patients (93 eyes) in the study who had an OCTA to look for CNV, but 11 patients were excluded, as they did not have same day FFA. Five patients were excluded with possible peripapillary CNV, as the OCTA images were not focused on the lesions. There were 77 patients in this study with a mean age of 76.4 years (±12.1 years SD). The ratio of male to female was 1:1.26 (34 males to 43 females).
The images were categorized into types of CNV based on multimodal imaging (FFA, ICGA, and OCT) as follows: classic nAMD, occult nAMD, RAP-, PCV-, cCSR-related CNV and pathological myopia-related CNV.
We only had two patients in the study with motion artefact significantly affecting OCTA images.
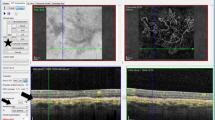
Inter-rater reliability and diagnostic accuracy of OCTA vs FFA
We found good inter-rater reliability between SJT and TS of κ=0.90. Overall, sensitivity of OCTA compared to FFA was 71% (32/45 patients) (56–84% 95% CI) and specificity was 81% (26/32 patients) (64–93% 95% CI). Subgroup analysis for classic nAMD showed OCTA vs FFA sensitivity to be 100% (14/14 patients) (77–100% 95%CI) with a specificity of 76% (13/17 patients) (50–93% 95% CI). OCTA vs FFA for occult nAMD sensitivity was 47% (7/15 patients) (21–73% 95% CI) and specificity was 76% (13/17 patients) (50–93% 95% CI). Cochran’s Q test showed OCTA to be significantly better at ruling out choroidal neovascularisation compared to FFA for suspected classic nAMD (p<0.05; see Figure 1), while showing no significant difference between FFA and OCTA in ruling out CNV in suspected occult nAMD or overall (Table 1.)
A 72-year-old female seen in eye casualty with blurring of right eye vision with suspected nAMD (VA 6/18 right eye). (a) OCT of patient showing subretinal fluid and subretinal thickening (b) FFA showing classic nAMD CNV (c) Cross sectional OCTA related OCT-B showing custom segmentation (slab of 50 μm) at level of lesion (d) OCTA showing vascular network corresponding to FFA classic nAMD CNV.
Six patients showed CNV on OCTA, where FFA did not show any angiographic leak. Two of these cases involved trying to differentiate cCSR from cCSR with CNV (Figure 2). OCTA was helpful in these cases to confirm a CNV with cCSR. Two had fluid on OCT consistent with exudative nAMD but no FFA or ICGA evidence of CNV, and the other 2 were found to have non-exudative AMD on OCT, FFA and ICGA (Figure 3). These last two 2 cases were diagnosed as non-exudative neovascular AMD, which has been reported in the literature.23
A case of chronic left recurrent central serous retinopathy in a 75-year-old female (VA 6/9 left eye). (a) FFA (left) showing stippled hyperfluorscence and a possible choroidal neovascular membrane on ICGA (right) (b) OCT of patient showing domed subretinal fluid with minimal subretinal thickening which seemed in keeping with chronic CSR (c) same day OCTA showed clear CNV and OCTA related OCT-B on the same day highlighted the subretinal CNV, with segmentation at that level (d) OCTA after first treatment with ranibizumab at 1 month shows possible reduction in CNV size and OCT at 1 month showing flattening of RPE with no subretinal fluid.
An 84-year-old woman seen in clinic with left eye metamorphopsia (VA 6/7.5 left eye) (a) OCT showing subretinal drusenoid deposits (b) FFA (left) and ICGA (right) showing no evidence of obvious leak, hotspots or plaques (c) OCTA (left) showing subretinal CNV with OCTA related OCT-B (right) confirming the level of the lesion.
There were 16 patients identified with a PED on OCT as part of the lesion. Of these, 69% (11/16) were confirmed to have a CNV with OCTA. Subgroup analysis showed 100% (3/3) detection for classic nAMD, 100% (4/4) for occult nAMD, 100% (1/1) for polyps, and 17% (1/6) for cCSR-related CNV. Two cases had a PED, with no FFA findings of CNV, but OCTA showed a vascular network. One of these cases was suspected to be nAMD on OCT, while OCT showed no evidence of fluid associated with a drusenoid PED in the other case.
FFA vs ICGA vs OCTA for defining vascular network when OCT showed signs of CNV
Further analysis was performed on the basis of OCT findings being suggestive of CNV, as a suspicious OCT usually leads to further investigations such as FFA. On OCT diagnosis alone, 14 patients were thought to have no signs of nAMD and so excluded from the analysis. One case of pathological myopia was also thought to have no evidence of CNV on OCT. We also had 1 patient with pathological myopia who did not have a recent OCT (within 1 week) and therefore was excluded from the analysis. The concordance with findings on OCT with a clear vascular network confirmed on FFA, OCTA, and on ICGA was compared. In this group 61 patients had suspicious OCT’s, with an FFA and OCTA taken with or without ICGA. OCTA was better than FFA overall in defining a clear vascular network (59%(36/61) vs 49%(30/61)), as well as when looking at occult and classic nAMD (72%(23/32) vs 44%(14/32)), and cCSR with suspected CNV (15%(2/13) vs 0%(0/13)). ICGA was the best imaging modality for defining vascular networks (70%(23/33)), however OCTA performed better than ICGA when looking at occult and classic nAMD (72%(23/32) vs 62% (8/13);Table 2).
Discussion
FFA is currently the gold standard for diagnosing CNV and therefore is recommended as part of first line investigations for suspected cases.1, 22 FFA defines CNV through evidence of angiographic leak. It is a dynamic assessment of the choroidal and retinal vasculature, with dye flow assessed from early to late phases through the network. Patterns of leak have a well-established diagnostic correspondence with histological/anatomical findings of choroidal neovascularisation.3, 4, 5 In some cases there is also a clear visualization of a vascular network, however angiographic leak particularly in the late phase does limit that.1 There are also practical limitations with it being an invasive procedure with the intravenous injection of dye, which has a small risk of anaphylaxis. The procedure is costly and time-consuming, typically taking 10–15 min to perform.1, 22 All this has meant a more selective use for FFA, with multimodal imaging (FFA, ICGA and OCT) being used to define CNV. ICGA, in comparison is able to more clearly resolve vascular networks, particularly with sub RPE lesions, due to deeper RPE penetration with the longer wavelengths used, its limited spread into the choroidal circulation and minimal leakage due to the molecular properties of the dye. So particularly leaky lesions and conditions involving the sub RPE/choroidal space such as retinal angiomatous proliferation and polypoidal choroidal vasculopathy are more easily characterised.16, 19 It has similar limitations to FFA in terms of being an invasive, time-consuming procedure, with the possibility of dye-related anaphylaxis.
OCT is a fast, non-invasive imaging modality, which has revolutionized the diagnosis and management of many ophthalmic conditions including choroidal neovascularisation.22 It is used to manage CNV as it can accurately define macular fluid, with the ability for serial morphological assessment and review of response to treatment.22 However it cannot delineate vascular structure and therefore cannot always clearly define CNV. The AMDOC study has demonstrated that OCT has moderate sensitivity for detecting new CNV compared to traditional FFA.22
OCTA, on the other hand, demonstrates the presence of CNV by detecting flow in a vascular complex such that the vascular network can be visualised, however, it does not show leak.23 There has been increasing literature available on OCTA diagnosing CNV.4, 7, 10 De Carlo et al.7 demonstrated OCTA detection for CNV vs FFA sensitivity at 50% and specificity at 91%. More recently Gong et al.8 were able to show for OCTA vs FFA detection of CNV in nAMD, the sensitivity was 86.5% and specificity was 67.6%. Coscas et al.13 have been able to show that the Heidelberg OCTA, with strict criteria for defining CNV, showed good concordance with traditional multimodal imaging.
We found the Heidelberg OCTA was significantly better at ruling out CNV compared to FFA for suspected classic nAMD CNV. However, it was worse than FFA for ruling out CNV in suspected occult nAMD and overall. This partly relates to issues of defining vascular networks when they are small and vertically orientated such as with RAP lesions.10 OCTA also does not image the choroid well and is affected by the amount of blood, fluid and RPE pigment.4 With FFA, in vascularized PEDs, the actual vascular nature of the lesion is hard to judge as such lesions are defined by seeing a stippled hyperfluorescence and late leak, rather than actually visualizing a vascular network. Inoue et al.4 have highlighted the difficulty of OCTA in detecting CNV in type 1 CNV with occult nAMD, particularly when PEDs have a large height. On the other hand, OCTA has been shown to define CNV better than traditional mutlimodal imaging in cases of cCSR with a PED apparent.18 In our study, with our small sample of PEDs, OCTA was found to be good at detecting CNV in occult nAMD with a PED and better than traditional multimodal imaging in finding CNV in cCSR with a PED, although cCSR-related PEDs showed CNV less frequently. Two cases in our study where OCT, FFA and ICGA could not pick up evidence of CNV, while OCTA did, represent the recently reported entity known as non-exudative nAMD in the literature, which may represent indolent CNV or the beginnings of new CNV.23
OCTA in our study was also better than FFA and ICGA in defining a clear neovascular network when OCT findings were suspicious of nAMD. With FFA the availability of early shots varied and FFA leakage obscured the vascular pattern. ICGA was better able to define the neovascular network overall, and its use in characterizing choroidal vascular networks is well established.1
Motion and projection artefact is a common issue which limits use of OCTA images and makes interpretation difficult.9 Due to Heidelberg OCTA eye tracking software, highly usable images were obtained for nearly all patients.9 The investigators experience over time, in using OCTA, also allowed a better ability to filter out motion and projection artefact, to delineate a CNV.
However, OCTA and FFA are not equivalent tests as FFA shows leak and OCTA the neovascular network by detecting flow; so direct comparison may not be appropriate as both add to the assessment of the neovascular lesion.
These results are important in highlighting the use of OCTA as an additional part of multimodal imaging. The neovascular network is more likely to be defined by OCTA compared to other traditional imaging techniques. In the context of fluid on OCT it may mean an FFA or ICGA is not required if a vascular network is seen, or it may help in the overall assessment by showing that there is a vascular complex. However, the finding of leak and amount of leak from FFA may still provide important information.
Changes in the vascular network with treatment may prove to be a useful way of assessing response to treatment and the requirement for on going therapy.5 This would allow more personalized treatment and management of nAMD, as well as other conditions with CNV requiring anti-VEGF, beyond traditional OCT-based approaches.
Strengths and limitations
We performed randomized, blinded grading for inter-rater reliability between the clinical investigators. There was also independent, blinded, grading of OCTA images, distinct in time from multimodal imaging review, all in a bid to reduce confirmation bias.
However, the study cohort did have issues of selection bias, as patients in this study were likely to have evidence of CNV as they had clinical signs and/or OCT findings suggestive of this. We also had a small sample size with no preceding power calculation. There was a learning curve to grading images, which also affected the results, with interpretation getting more accurate over time. Due to practical limitations, only two retinal specialists had experience with OCTA, and open adjudication of images was done when there was a particularly difficult image to interpret. Heidelberg’s OCTA (OCT2 6.7B) has been updated to a commercial product, with a new advanced probabilistic algorithm, with scan areas of 15 × 15o (11 μm resolution) 10 × 10o (5.7 μm resolution) and 15 × 30o (wide field). The new software will likely be more accurate at defining CNV than the experimental device we tested.
Conclusion
OCTA technology has the potential to be a significant adjunct to traditional multimodal imaging assessment for choroidal neovascularisation. Important factors in its more wide spread use will include increased speeds of image capture, ease of image acquisition and review, as well as the ability to network and store ever increasing image sizes.
References
The Royal College of Ophthalmologists. Age-Related Macular Degeneration: Guidelines for Management. The Royal College of Ophthalmologists Scientific Department: London, UK, 2013 pp 1–145 Available at https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2013-SCI-318-RCOphth-AMD-Guidelines-Sept-2013-FINAL-2.pdf.
Castillo MM, Mowatt G, Lois N, Elders A, Fraser C, Amoaku W et al. Optical coherence tomography for the diagnosis of neovascular age related macular degeneration: a systematic review. Eye 2014; 28: 1399–1406.
Gass JD . Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal neovascular membranes. Am J Ophthalmol 1994; 118 (3): 285–298.
Inoue M, Jung JJ, Balaratnasingam C, Dansingani KK, Dhrami-Gavazi E, Suzuki M et al. A comparison between optical coherence tomography angiography and fluorescein angiograhy for the imaging of type 1 neovascularization. Invest Ophthalmol Vis Sci 2016; 57 (9): 314–323.
Kuehlewein L, Sadda SD, Sarraf D . OCT angiography and sequential quantitative analysis of type 2 neovascularization after ranibizumab therapy. Eye 2015; 29: 932–935.
Spaide RF, Klancnik JM Jr, Cooney J . Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol 2015; 133 (1): 45–50.
De Carlo TE, Bonini Filho MA, Chin AT, Adhi M, Ferrara D, Baumal CR et al. Spectral-domain optical coherence tomography angiography of choroidal neovascularization. Ophthalmology 2015; 122 (6): 1–11.
Gong J, Yu S, Gong Y, Wang F, Sun X . The diagnostic accuracy of optical coherence tomography angiography for neovascular age-related macular degeneration: a comparison with fundus fluorescein angiography. Journal of Ophthalmology 2016; 2016: 7521478.
Coscas G, Lupidi M, Coscas F . Heidelberg spectralis optical coherence tomography angiography: technical aspects. In: Bandello F, Souied EH, Querques G (eds). OCT Angiography in Retinal and Macular Diseases (Developments in Ophthalmology). Karger Publishing Ltd: Bazel: Switzerland, 2016, pp 1–5.
Jia Y, Bailey ST, Wilson DJ, Tan O, Klein ML, Flaxel CJ et al. Quantitative optical coherence tomography angiography of choroidal neovascularization in age-related macular degeneration. Ophthalmology 2014; 121 (7): 1435–1444.
De Carlo TE, Romano A, Waheed NK, Duker JS . A review of optical coherence tomography angiography (OCTA). International Journal of Retina and Vitreous 2015; 1 (5): 1–15.
Liu G, Jia Y, Pechauer AD, Chandwani R, Huang D . Split-spectrum phase-gradient optical coherence tomography angiography. Biomed Optics Express 2016; 7 (8): 2943–2954.
Coscas GJ, Lupidi M, Coscas F, Cagini N, Souied EH . Optical coherence tomography angiography versus traditional multimodal imaging in assessing the activity of exudative age-related macular degeneration: a new diagnostic challenge. Retina 2015; 35: 2219–2228.
Liakopoulos S, Ongchin S, Bansal A, Msutta S, Walsh A, Updike PG et al. Quantitative optical coherence tomography findings in various subtypes of neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2008; 49 (11): 5048–5054.
Yannuzzi LA, Silvana Negrão S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J et al. Retinal angiomatous proliferation in age–related macular degeneration. Retina 2001; 21: 416–434.
Tanaka K, Mori R, Kawamura A, Nakashizuka H, Wakatsuki Y, Yuzawa M . Comparison of OCT angiography and indocyanine green angiographic findings with subtypes of polypoidal choroidal vasculopathy. Br J Ophthalmol 2017; 101: 51–55.
Querques L, Giuffrè C, Corvi F, Zucchiatti I, Carnevali A, Vitis LA et al. Optical coherence tomography angiography of myopic choroidal neovascularisation. Br J Ophthalmol 2016; 0: 1–7.
Bousquet E, Bonnin S, Mrejen S, Krivosic V, Tadayoni R, Gaudric A . Optical coherence tomography angiography of flat irregular pigment epithelium detachment in chronic central serous chorioretinopathy. Retina 2017; 0: 1–10.
Costanzo E, Miere A, Querques G, Capuano V, Jung C, Souied EH . Type 1 choroidal neovascularization lesion size: indocyanine green angiography versus optical coherence tomography angiography. Invest Ophthalmol Vis Sci 2016; 57: 307–313.
Bonini Filho MA, de Carlo TE, Ferrara D, Adhi M, Baumal CR, Witkin AJ et al. Association of choroidal neovascularization and central serous chorioretinopathy with optical coherence tomography angiography. JAMA Ophthalmol 2015; 133 (8): 899–906.
Querques G, Miere A, Souied E H . Optical coherence tomography angiography features of type 3 neovascularization in age-related macular degeneration. In: Bandello F, Souied E H, Querques G (eds). OCT Angiography in Retinal and Macular Diseases (Developments in Ophthamology). Karger Publishing Ltd: Bazel, Switzerland, 2016 pp 57–61.
Do DV, Gower EW, Cassard SD, Boyer D, Bressler NM, Bressler SB et al. Detection of new-onset choroidal neovascularization using optical coherence tomography the AMD DOC Study. Ophthalmology 2012; 119: 771–778.
Palejwala NV, Jia Y, Gao SS, Liu L, Flaxel CJ, Hwang TS et al. Detection of non-exudative choroidal neovascularization in age-related macular degeneration with optical coherence tomography angiography. Retina 2015; 35 (11): 2204–2211.
Acknowledgements
Heidelberg engineering and Bayer provided sponsorship to attend conferences. Heidelberg engineering gave access to the Heidelberg OCT angiography beta software module.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TS was sponsored by Heidelberg engineering to go to the Heidelberg Engineering International Spectralis Symposium 2016 and sponsored by Bayer to go the ARVO conference 2017. He was also given access to the Heidelberg OCT angiography beta module by Heidelberg engineering. James Talks was sponsored by Heidelberg engineering to go to the Heidelberg Engineering International Spectralis Symposium 2016. He was also given access to the Heidelberg OCT angiography beta module by Heidelberg engineering. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Soomro, T., Talks, J. The use of optical coherence tomography angiography for detecting choroidal neovascularization, compared to standard multimodal imaging. Eye 32, 661–672 (2018). https://doi.org/10.1038/eye.2018.2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2018.2
This article is cited by
-
Avacincaptad pegol for geographic atrophy secondary to age-related macular degeneration: 18-month findings from the GATHER1 trial
Eye (2023)
-
Optical coherence tomography angiography for the detection of macular neovascularization—comparison of en face versus cross-sectional view
Eye (2023)
-
Optical coherence tomography angiography for identifying choroidal neovascular membranes: a masked study in clinical practice
Eye (2021)
-
Sensitivity and specificity of optical coherence tomography angiography in the diagnosis of active choroidal neovascularization: a systematic review and meta-analysis
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
A practical guide to optical coherence tomography angiography interpretation
International Journal of Retina and Vitreous (2020)