Abstract
Purpose
To characterize the type, and the causes of visual impairment (VI) in various stages of early and late age-related macular degeneration (AMD) and the factors associated with visual impairment in subjects with AMD
Methods
6617 subjects ≥60 years were enumerated; 5495 (83.04%) participated in eye examination. Of which, 4791 subjects had gradable fundus images. AMD was graded per International ARM Epidemiological Study Group. Subjects underwent detailed ophthalmic exam. VI was defined per the WHO classification. Mild VI was defined as VA less than 6/12 to 6/18, moderate VI–VA less than 6/18 but up to 6/60, severe VI–VA less than 6/60 but up to 3/60 and legal blindness–VA worse than 3/60. Factors associated with VI in AMD was analyzed with univariate and logistic regression analysis.
Results
Nine hundred and eighty-eight subjects were identified as having AMD (893 with early AMD and 95 with late AMD); 85% of the subjects (95% CI: 82.7–87.1) had no VI, 13.1% had mild VI (95% CI: 11.1–15.3), 0.8% had severe VI (95% CI: 0.4–1.6), 1.1% had legal blindness (95% CI: 0.6–1.9). Prevalence of any VI was 13.7% in early AMD and 27.4% in late AMD, P=0.0004; age group 65–70 years (OR=1.89, 95% CI: 1.16–3.08, P=0.011), and those ≥75 years (OR=3.67, 95% CI: 1.95–6.91, P=0.0001) had greater odds of VI compared with age group 60–64 years. Male gender was a protective factor for VI (OR=0.57, CI: 0.36–0.90, P=0.016). Cataract (31.8%) and refractive error (28.4%) accounted for a majority of the VI.
Conclusions
Cataract and refractive error account for a significant proportion of VI in the south Indian population with AMD. Early AMD is the third leading cause of VI. Greater age and female gender are associated with VI in subjects with AMD.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) in its late stage is the most common cause of adult blind registration in many developed countries,1, 2, 3, 4 with the prevalence of visual loss due to AMD being higher from 70 years of age.5, 6, 7 The INDEYE study observed that all cases of advanced AMD were visually impaired with visual acuity (VA) worse than 6/24.8 In a hospital-based study in Maharashtra, west India, the prevalence of legal blindness (VA worse than 3/60) was 4.2% in AMD.9 Although previous studies conducted in the Indian population have reported visual impairment, there is lack of sufficient information regarding the burden of visual impairment (VI) in various sub-types or lesions of AMD. In our previous study,10 we reported age- and gender-adjusted prevalence of early AMD to be 20.91 and 16.37% in the rural and urban populations, respectively and the prevalence of late AMD as 2.26 and 2.32% in the rural and urban populations, respectively. In the present study, we intended to characterize the type, and the causes of visual impairment in various stages of early and late AMD and the factors associated with visual impairment in subjects with AMD.
Materials and methods
Sankara Nethralaya: Rural-Urban Age-related Macular Degeneration study (SN-RAM study), a population-based cross-sectional study, was conducted in south India between 2009 and 2011. The study was approved by the institutional review board and a written consent was obtained from all the participating subjects per the Declaration of Helsinki.
Study participants
The study design and methodology has been described earlier.10 Briefly, a total of 6617 people (rural (n=3904) and urban (n=2713)) were enumerated. Of which, 5495 (83%) participated in the study for eye examination; after excluding those who did not have retinal photographs and those with ungradable images, 4791 subjects were included in this study.
Clinical examination protocol
A detailed history, including data on demographic, socioeconomic, and ocular history, was obtained from all patients at the base hospital in the urban arm and in a customized mobile examination unit in the rural arm. The socioeconomic status (SES) was assessed using a multiple index questionnaire and the scoring was characterized as low (score, 0–14), middle (score, 15–28), and high (score, 29–42). A detailed questionnaire was administered regarding the medical history, smoking, tobacco and alcohol consumption history, educational and occupational history. The blood pressure (BP) was recorded in the sitting position, in the right arm to the nearest 2 mm Hg using the mercury sphygmomanometer (Diamond Deluxe BP apparatus, Pune, India). Two readings were taken, 5 min apart, and their mean was taken as the BP.11
Diagnostic criteria for Diabetes
Known diabetes
if they were using hypoglycemic drugs, either oral or insulin or both along with dietary recommendations.
Provisional diabetes
if fasting blood glucose was ≥110 mg/dl done twice in new asymptomatic subject.
Newly diagnosed diabetes
all individuals with provisional diabetes underwent oral glucose tolerance test for confirmation.
First step was screening at the household: capillary blood glucose by finger prick using Accutrend Alpha (Roche Diagnostics) was carried out with a minimum of 8 h of overnight fasting. Second step was confirmatory in the mobile van in rural and base hospital in the urban arm, all underwent OGTT, a reading of ≥200 mg% was the cutoff point.
All subjects underwent estimation of fasting blood glucose by enzymatic assay (Merck Micro Lab 120 semi-automated analyzer), total serum cholesterol (CHOD-POD method), high-density lipoproteins (HDL; CHOD-POD method after protein precipitation), serum triglycerides (CHOD-POD method), hemoglobin (calorimetric hemoglobinometer), and packed cell volume (capillary method).
Ophthalmic examination
All subjects underwent detailed ophthalmic evaluation, which included assessment of visual acuity and refraction using modified Early Treatment Diabetic Retinopathy Study chart (Low Vision Products; LightHouse, New York, USA), anterior segment examination using a Zeiss SL 130 (Carl Zeiss, Jena, Germany) slit-lamp, intraocular pressure measurement using Goldmann applanation tonometer (Zeiss AT 030; Carl Zeiss Jena, Germany), and fundus examination using binocular indirect ophthalmoscope (Keeler Instruments, Broomall, PA, USA). Grading of lens opacities was performed using the Lens Opacities Classification System (LOCS III; Leo T. Chylack, Harvard Medical School, Boston, MA, USA) by two experienced ophthalmologists. The grading agreements were as follows: nuclear opalescence (k=0.84), nuclear color (k=0.88), cortical (k=0.89), and posterior subcapsular (k=0.89). Overall, the average grading agreement was high (k=0.85).
Visual acuity assessment
Visual acuity was estimated using the modified ETDRS chart (Light House Low Vision Products, New York, USA). For those who could not read the English alphabet, Landolt’s ring test was used. Objective refraction (streak retinoscope, Beta 200, Heine, Germany) was always followed by a subjective refraction. If the subject was unable to read the 4/40 (log MAR 1.0) line, vision was checked at one meter, and if the subject was still unable to identify any of the larger optotypes, perception of hand movements was assessed; if the vision was less than hand movements, perception of light was tested. Visual impairment (VI) was defined based on the WHO criteria.12 Mild VI was defined as visual acuity (VA) less than 6/12 to 6/18, moderate VI was defined as VA was less than 6/18 but up to 6/60, severe VI was defined as VA was less than 6/60 but up to 3/60 and blindness was defined as VA worse than 3/60.
Emmetropia was defined as a spherical equivalent between −0.50 and +0.50 diopter sphere (DS). Myopia was defined as a spherical equivalent of less than −0.50 DS. Hyperopia was defined as a spherical equivalent of greater than +0.50 DS. Astigmatic correction was measured in minus cylinder format, and astigmatism was defined as a cylindrical error less than −0.50 diopter cylinder (DC) at any axis.13
Retinal photographs were obtained after pupillary dilatation (FF450 Fundus Camera; Carl Zeiss). Diabetic retinopathy (DR) was graded using the International Clinical Diabetic Retinopathy Disease Severity Scale. The grading agreement between the observers was 0.80.
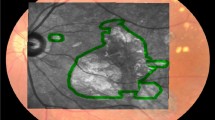
AMD was graded according to the International AMD Epidemiological Study Group14 and stratified into stages. The grading agreement, which was done by two independent observers (retina specialists) in a masked manner, was found to be 0.62 for early AMD and 0.87 for late AMD. Early AMD was defined as the presence of drusen (discrete whitish-yellow spots located external to the neuroretina or retina pigment epithelium (RPE)) or drusen with RPE abnormalities (areas of hyper- or hypopigmentation). Late AMD was defined as the presence of geographic atrophy of the RPE in the absence of neovascular AMD or neovascular (wet) AMD (RPE detachments, which may be associated with neurosensory retinal detachment, subretinal or sub-RPE neovascular membranes, epiretinal, intraretinal, subretinal, or subpigment epithelial scar/glial tissue or fibrin-like deposits, and subretinal hemorrhages not related to other retinal vascular disease).
For statistical analysis, we examined the data of eligible subjects for evidence of AMD. The eye with a diagnosis of AMD was first chosen. In case of bilateral diagnosis of AMD, the eye with the ‘worse’ stage of AMD was chosen. Therefore, one eye of each (eligible) subject was included. We then examined for proportions of subjects with various levels of visual impairment defined per WHO classification in the chosen eye.
All continuous variables were assessed for normality of distribution. The proportions were examined using a chi-square test. The associations were examined by univariate and a step-wise multiple logistic regression analysis.
Results
Prevalence of visual impairment in subjects with AMD
Table 1 shows the prevalence of VI in subjects with AMD. Of the total 4791 subjects with gradable photographs, 988 subjects had evidence of AMD (893 with early AMD and 95 subjects with late AMD).
Of the 988 subjects with AMD, eight hundred and forty (85%, 95% CI: 82.7–87.1) subjects had no VI, 129 (13.1%, 95% CI: 11.1–15.3) had mild VI, 8 (0.8%, 95% CI: 0.4–1.6) had severe VI and the remaining 11 (1.1%, 95% CI: 0.6–1.9) had legal blindness.
Prevalence of visual impairment in early and late AMD
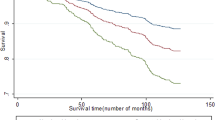
Table 2 shows the prevalence of visual impairment in early and late AMD. The proportion of subjects with no VI was higher in early AMD compared with late AMD (86.3 vs 72.6%, P=0.0004).
The prevalence of any VI was 13.7% in early AMD and was 27.4% in late AMD and the difference was statistically significant, P=0.0004. Among those with visual impairment, a majority of the subjects (87% in the early AMD group and 88% in the late AMD group) had mild VI.
Prevalence of visual impairment in sub-types of early and late AMD
Table 3 shows the prevalence of VI in various sub-types of early and late AMD. Among those with visual impairment, a majority of the subjects had mild VI in all sub-types of early and late AMD. The prevalence of mild VI ranged from 12 to 14% in early AMD, while that in late AMD ranged from 16.2 to 29.3%. severe VI ranged from 0.4 to 1.1% in early AMD, and 1.7% in the late AMD. The prevalence of legal blindness ranged from 0.5 to 1.1% in early AMD and was 5.4% in late AMD.
Risk factors for visual impairment in AMD
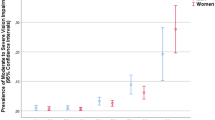
Table 4 shows the risk factors associated with VI in subjects with AMD with univariate analysis. VI was significantly higher in age group ≥75 years than those with no VI, (23 vs 13%, P=0.001); prevalence of VI was greater in the low SES (67.6 vs 50.2%, P=0.001). VI was more prevalent among those with slightly lower BMI than those with higher BMI (22.3 vs 20.9 kg/m2, P=<0.0001) and in those with slightly lower intraocular pressure (13.2 vs 13.7 mm Hg, P=0.016).
Table 5 shows the risk factors for VI in subjects with AMD using multiple logistic regression.
When adjusted for SES, systolic and diastolic BP, BMI, serum lipids, smoking, and tobacco intake, the presence of cataract, intraocular pressure, presence of DR and refractive errors, the odds of having VI was higher in the age groups 65–70 years (OR=1.89, 95% CI: 1.16–3.08, P=0.011) and in those aged ≥75 years (OR=3.67, 95% CI: 1.95–6.91, P=0.0001) compared with 60–64 years of age. Male gender was a protective factor for VI (OR=0.57, CI: 0.36–0.90, P=0.016) compared with female gender.
Ocular associations (causes) of visual impairment in AMD
The causes for reduced vision were documented separately and distinctly by the examining retina specialist involved in this research study. Even in the presence of combination of findings, for instance, cataract and AMD, the cause predominantly contributing to visual impairment was specifically documented by the specialist. Cataract, refractive error and early AMD accounted for 31.8, 28.4, and 21.6% of the causes of VI in these subjects with AMD, respectively. Myopic maculopathy, corneal opacity, late AMD and posterior capsule opacification accounted for 6.8, 3.4, 3.4, and 2.0% of all causes of VI, respectively. Findings such as DR ischemic vasculopathy, macular scar, (post) retinal detachment, retinitis pigmentosa each contributed to 0.7% to the overall causes of VI in subjects with AMD.
Discussion
We examined the prevalence of and the risk factors for VI in subjects with AMD in a south Indian population aged 60 years or above. The main findings of our study are that the prevalence of mild, severe VI and legal blindness in subjects with AMD was 13.1%, 0.8%, and 1.1%, respectively. The prevalence of visual impairment is higher in subjects with late AMD compared with early AMD. Cataract and refractive error together are responsible for about 59% of the visual impairment. About 22% of the VI was attributed to early AMD and another 3% to late AMD.
A systematic review by Owen et al5 reported on the studies conducted in populations world-wide that examined visual impairment in relation to geographic and neovascular AMD (both being late stages of AMD). Data were pooled from Beaver Dam Eye Study,15 Blue Mountains Eye Study,16 Melbourne Visual Impairment Project,17, 18, 19 Rotterdam Eye study,20 Copenhagen City Eye Study,21, 22 and Northern London Eye Study.23 The review reported that the prevalence of late stages of AMD increased with the age, and so did the visual impairment. Geographic AMD was noted to be prevalent from the age 55 years, while the neovascular AMD was noted to be prevalent from the age 50 and above. The prevalence of partially sighted (PS) defined as VA 6/18 and better than 6/60 was noted to be 0.00% up to 64 years. The prevalence of PS was noted to be 0.13% in the age group 65–69 years, which showed an increasing trend to a maximum of 6.63% in the group of subjects aged 90 years or above. Blindness defined as best VA of 6/60 and up to 3/60 was seen in 0.03% in the age group 50–59 years. The prevalence of blindness was 0.00% in the age group 60–69 years, and then increased from 0.06% for the age group 70–74 years, reaching a maximum prevalence of 6.12% for those aged 90 years or above. The pooled estimate showed that 3.5% of those aged 75 years or older were visually impaired due to AMD. Our data on late AMD also shows similar results wherein, 3.4% of those with Late AMD had visual impairment. Another study24 conducted in a GP practice population in London reported a comparable prevalence of 2.8% in those aged 75 years or older.
Klein et al25 in their systematic review conducted a pooled analysis from various studies namely, Barbados Eye Study, Beaver Dam Eye Study, Baltimore Eye Survey, Blue Mountains Eye Study, Melbourne Vision Impairment Project, Proyecto VER, Vision Evaluation Research, Rotterdam Study, Salisbury Eye Evaluation Project, and the Eye Diseases Prevalence Research Group.26 Individuals aged 80 years or older had the heaviest burden of age-related eye disease having 30% of all cases of early AMD and about 62% of all cases of late AMD. In black persons, severe VI was due to cataract whereas in white persons, it was attributed to AMD. Similarly, we noticed that those aged 75 years or above had greater risk of VI compared with those aged 60–64 years.
In the Indian population, the INDEYE study conducted in a population aged 50 years or older observed that all cases of advanced AMD were visually impaired with visual acuity worse than 6/24 which according to our study is defined as moderate VI.8 In a hospital-based study conducted in a population aged 50 years or older in Maharashtra, west India, the prevalence of legal blindness (VA worse than 3/60) was 4.2% in AMD.9 The prevalence of blindness in other Asian countries such as Pakistan, Bangladesh and Nepal are reported to vary from 2.1 to 8.7% for all blindness attributable to AMD.27 But the aforementioned studies examined different or younger age groups and the prevalence therefore varies across studies or is lesser compared with our study. We have attempted to characterize the severity of VI in early and late stages of AMD in a population aged 60 years or older and may be a likely explanation for a higher prevalence of legal blindness.
The proportion of subjects with VI was significantly higher in those aged 75 years or more compared with those in the age group 60–64 years. When adjusted for SES, BP, serum lipids, presence of cataract, presence of DR, smoking, and refractive error, the odds of having VI was greater in subjects in the age group 65–70 years and in those ≥75 years compared with those in the age group 60–64 years. Our study results are consistent with that reported in previous studies, whereby greater age is a risk factor for VI in subjects with AMD.28, 29, 30
We observed that men with AMD are at a lower risk of VI compared to women with AMD. Previous studies conducted in the general population reported that, visual impairment increases with age and especially in women, while no such relationship was observed in men.30, 31, 32, 33 In the AMD population, female gender was associated with greater prevalence of drusen and neovascular AMD than male gender.34 We observed a similar association of age and gender with VI in subjects with AMD.
Age group ≥75 years and those in the low SES showed significantly higher proportion of subjects with VI than with the other age groups. However, after adjusting for potential confounders examined in this study, the association between SES and VI was not significant.
The mean BMI was only slightly lower (difference in means=1.4 kg/m2) in the group with VI compared to those with no VI, and the mean intraocular pressure was 13.7 mm Hg in those with normal visual acuity and 13.2 mm Hg in the group with VI. Although we observed statistically significant differences in the intraocular pressures between those with and without VI, the differences do not appear clinically significant.
Visual impairment in Early vs late AMD
The prevalence of any VI was greater in late AMD compared with that in early AMD. However, we were unable to perform similar comparison for the prevalence of severe VI and legal blindness between early and late AMD due to lesser number of subjects. In both early and late AMD, the majority of the VI was mild VI.
Lamoureux et al35 reported that late rather than early AMD is associated with poorer visual function when assessed by VF-11 scale. In contrast, Scilley et al36 reported that despite good visual acuity, subjects with early AMD may experience near vision complaints, and glare during night driving. Midena et al37 reported impairment of macular function except colour vision in early AMD. Increase in the number of drusen is negatively associated with the macular function. Similarly, Tolentino et al38 reported that subjects with early AMD possess good visual acuity but may experience distortion, and hypothesised as being related to alternation of the photoreceptor layer function. It is evident that visual acuity is not a good indicator of visual function; nevertheless, it continues to be used in several clinical trials for monitoring of the outcome.2
In the older age group, VI has been reported to be associated with falls and fall-related injuries.39, 40, 41, 42 Therefore, our findings have greater implications for subjects in this aged population with AMD.
Associations (Causes) of VI in subjects with AMD
In our study, cataract was the leading cause of VI contributing to about one-third of all VI in this AMD population, the second and the third highest cause being refractive error and early AMD, respectively. Visual impairment attributable to late AMD is further lower. A likely explanation could be the lower prevalence of subjects with late AMD as compared to early AMD. An interesting observation was that early AMD was the third highest cause of VI, but the majority of the subjects had mild VI (as seen in Table 3).
Studies conducted in Asian27 and in Indian population8, 9 report cataract and refractive error as the leading cause of VI in the elderly population in general. In our study, after stratifying the VI based on associated ocular findings, we observed that 21% of the VI was attributed to early AMD and about 3% to late AMD. Cataract and refractive error represents the treatable or correctable cause of VI. In the western population, AMD is reported as the leading cause of VI contributing to as high as 50% of all causes of VI.2 Therefore, identification of potential risk factors in the early stages becomes crucial for early referral and timely management.
For patients diagnosed with early or late AMD, a detailed evaluation of visual requirements for everyday tasks is indicated. For the reason that AMD is predominantly associated with impairment of central vision such as central scotoma, patients may often complain of difficulty in near vision or inability to maintain fixation. Such patients can be provided training for eccentric viewing, whereby, an off-foveal point in the retina will be preferred by the patient for fixation and be trained to maintain fixation using that point. Magnifiers may be prescribed for near vision difficulty in the form of spectacle or stand magnifiers, tailored to the visual requirements of the patients. In cases where the above two options are not feasible, video magnifiers may be a viable option that is available with a variety of adjustments such as brightness and contrast enhancement.
We have compared studies predominantly from the Indian sub-continent because there are likely to be geographical variations in the prevalence of AMD in association with genetic and/or environmental factors.5
The strengths of our study is that this was a population-based study and we utilized the International AMD Epidemiological Study Group protocol. We assessed for the prevalence and severity of VI in subjects with unilateral AMD and in the eye with worse stage of AMD in case of bilateral diagnosis of AMD. The prevalence of AMD and accordingly the VI, may vary if bilateral AMD are considered or if both eyes are analyzed.
In conclusion, we observed the prevalence of mild, severe VI and legal blindness to be 13.1, 0.8, and 1.1%, respectively, in a south Indian population with AMD. Prevalence of any visual impairment is greater in subjects diagnosed with late AMD compared with early AMD. Early AMD is the third leading cause of VI in this south Indian population aged 60 years or above; a majority of the subjects had only mild visual impairment. Greater age and female gender are factors associated with VI in subjects with AMD. Cataract and refractive error account for a significant proportion of VI, representing preventable visual loss in this elderly population.

References
Rosenberg T, Klie F . The incidence of registered blindness caused by age-related macular degeneration. Acta Ophthalmol Scand 1996; 74: 399–402.
Hogg RE, Chakravarthy U . Visual function and dysfunction in early and late age-related maculopathy. Prog Retin Eye Res 2006; 25: 249–276.
Sunness JS, Gonzalez-Baron J, Applegate CA, Bressler NM, Tian Y, Hawkins B et al. Enlargement of atrophy and visual acuity loss in the geographic atrophy form of age-related macular degeneration. Ophthalmology 1999; 106: 1768–1779.
Hassan SE, Lovie-Kitchin JE, Woods RL . Vision and mobility performance of subjects with age-related macular degeneration. Optom Vis Sci 2002; 79: 697–707.
Owen CG, Fletcher AE, Donoghue M, Rudnicka AR . How big is the burden of visual loss caused by age related macular degeneration in the United Kingdom? Br J Ophthalmol 2003; 87: 312–317.
McCarty CA, Mukesh BN, Fu CL, Mitchell P, Wang JJ, Taylor HR . Risk factors for age-related maculopathy: The Visual Impairment Project. Arch Ophthalmol 2001; 119: 1455–1462.
Leibowitz HM, Krueger DE, Maunder LR, Milton RC, Kini MM, Kahn HA et al. The Framingham Eye Study monograph: an ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973-1975. Surv Ophthalmol 1980; 24: 335–610.
Gupta SK, Murthy GV, Morrison N, Price GM, Dherani M, John N et al. Prevalence of early and late age-related macular degeneration in a rural population in northern India: the INDEYE feasibility study. Invest Ophthalmol Vis Sci 2007; 48: 1007–1011.
Kulkarni SR, Aghashe SR, Khandekar RB, Deshpande MD . Prevalence and determinants of age-related macular degeneration in the 50 years and older population: a hospital based study in Maharashtra, India. Indian J Ophthalmol 2013; 61: 196–201.
Raman R, Pal SS, Ganesan S, Gella L, Vaitheeswaran K, Sharma T . The prevalence and risk factors for age-related macular degeneration in rural-urban India, Sankara Nethralaya Rural-Urban Age-related Macular degeneration study, Report No. 1. Eye (Lond) 2016; 30: 688–697.
Agarwal S, Raman R, Paul PG, Rani PK, Uthra S, Gayathree R et al. Sankara Nethralaya-Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS 1): study design and research methodology. Ophthalmic Epidemiol 2005; 12: 143–153.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th revision Current Version for 2003 Chapter VII H54 Blindness and low vision. Available at: http://www.who.int/classifications/icd/en/ (accessed 21 November 2016).
Dandona L, Dandona R, Naduvilath TJ, Srinivas M, McCartyCA, Rao GN . Refractive errors in an urban population in Southern India: The Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci 1999; 40: 2810–2818.
The International ARM Epidemiological Study Group. An international classification and grading system for age related maculopathy and age related macular degeneration. Surv Ophthalmol 1995; 39: 367–374.
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Mitchell P, SmithW, Attebo K, Wang JJ . Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology 1995; 102: 1450–1460.
VanNewkirk MR, Nanjan MB, Wang JJ, Mitchell P, Taylor HR, McCarty CA . The prevalence of age-related maculopathy: the visual impairment project. Ophthalmology 2000; 107: 1593–1600.
VanNewkirk MR, Weih L, McCarty CA, Taylor HR . Cause-specific prevalence of bilateral visual impairment in Victoria, Australia: the Visual Impairment Project. Ophthalmology 2001; 108: 960–967.
Weih LM, VanNewkirk MR, McCarty CA, Taylor HR . Age-specific causes of bilateral visual impairment. Arch Ophthalmol 2000; 118: 264–269.
Vingerling JR, Dielemans I, Hofman A, Grobbee DE, Hijmering M, Kramer CF et al. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology 1995; 102: 205–210.
Vinding T . Visual impairment of age-related macular degeneration. An epidemiological study of 1000 aged individuals. Acta Ophthalmol (Copenh) 1990; 68: 162–167.
Vinding T . Age-related macular degeneration. An epidemiological study of 1000 elderly individuals. With reference to prevalence, funduscopic findings, visual impairment and risk factors. Acta Ophthalmol Scand Suppl 1995; (217): 1–32.
Reidy A, Minassian DC, Vafidis G, Joseph J, Farrow S, Wu J et al. Prevalence of serious eye disease and visual impairment in a North London population: population based, cross sectional study. BMJ 1998; 316: 1643–1646.
Wormald RP, Wright LA, Courtney P, Beaumont B, Haines AP . Visual problems in the elderly population and implications for services. BMJ 1992; 304: 1226–1229.
Klein R, Klein BE . The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 2013; 54: ORSF5–ORSF13.
Congdon N, O’Colmain B, Klaver CC, Klein R, Muñoz B, Friedman DS et al. Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 2004; 122: 477–485.
Woo JH, Sanjay S, Au Eong KG . The epidemiology of age-related macular degeneration in the Indian subcontinent. Acta Ophthalmol 2009; 87: 262–269.
Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT . Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol 1998; 116: 653–658.
Evans JR, Fletcher AE, Wormald RPL . 28 000 Cases of age related macular degeneration causing visual loss in people aged 75 years and above in the United Kingdom may be attributable to smoking. Br J Ophthalmol 2005; 89: 550–553.
Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Fotouhi A . Visual impairment in the 40- to 64-year-old population of Shahroud, Iran. Eye (Lond) 2012; 26: 1071–1077.
Dandona R, Dandona L, Srinivas M, Giridhar P, Prasad MN, Vilas K et al. Moderate visual impairment in India: The Andhra Pradesh Eye Disease Study. Br J Ophthalmol 2002; 86: 373–377.
Taylor HR, Livingston PM, Stanislavsky YL, McCarty CA . Visual impairment in Australia: distance visual acuity, near vision, and visual field findings of the Melbourne Visual Impairment Project. Am J Ophthalmol 1997; 123: 328–337.
Khandekar R, Mohammed AJ, Negrel AD, Riyami AA . The prevalence and causes of blindness in the Sultanate of Oman: The Oman Eye Study (OES). Br J Ophthalmol 2002; 86: 957–962.
Zetterberg M . Age-related eye disease and gender. Maturitas 2016; 83: 19–26.
Lamoureux EL, Mitchell P, Rees G, Cheung G, Yeo I, Lee SY et al. Impact of early and late age-related macular degeneration on vision-specific functioning. Br J Ophthalmol 2011; 95: 666–670.
Scilley K, Jackson GR, Cideciyan AV, Maguire MG, Jacobson SG, Owsley C . Early age-related maculopathy and self-reported visual difficulty in daily life. Ophthalmology 2002; 109: 1235–1242.
Midena E, Degli Angeli C, Blarzino MC, Valenti M, Segato T . Macular function impairment in eyes with early age-related macular degeneration. Invest Ophthalmol Vis Sci 1997; 38: 469–477.
Tolentino MJ, Miller S, Gaudio AR, Sandberg MA . Visual field deficits in early age-related macular degeneration. Vision Res 1994; 34: 409–413.
Wood JM, Lacherez P, Black AA, Cole MH, Boon MY, Kerr GK . Risk of falls, injurious falls, and other injuries resulting from visual impairment among older adults with age-related macular degeneration. Invest Ophthalmol Vis Sci 2011; 52: 5088–5092.
Freeman EE, Munoz B, Rubin G, West SK . Visual field loss increases the risk of falls in older adults: The Salisbury eye evaluation. Invest Ophthalmol Vis Sci 2007; 48: 4445–4450.
Klein BE, Klein R, Lee KE, Cruickshanks KJ . Performance-based and self-assessed measures of visual function as related to history of falls, hip fractures, and measured gait time. The Beaver Dam Eye Study. Ophthalmology 1998; 105: 160–164.
Coleman AL, Cummings SR, Yu F . Binocular visual-field loss increases the risk of future falls in older white women. J Am Geriatr Soc 2007; 55: 357–364.
Acknowledgements
This work was funded by Jamshetji Tata trust, Mumbai, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Srinivasan, S., Swaminathan, G., Kulothungan, V. et al. Prevalence and the risk factors for visual impairment in age-related macular degeneration. Eye 31, 846–855 (2017). https://doi.org/10.1038/eye.2017.72
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.72
This article is cited by
-
Prevalence and sociodemographic factors associated with vision difficulties in Ghana, Gambia, and Togo: a multi-country analysis of recent multiple Indicator cluster surveys
BMC Public Health (2021)
-
Gender variation in central serous chorioretinopathy
Eye (2018)
-
RETRACTED ARTICLE: A comparison of risk factors for age-related macular degeneration and polypoidal choroidal vasculopathy in Chinese patients
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)