Abstract
Diabetic retinopathy (DR) is the most common microvascular complication in diabetic patients and one of the main causes of acquired blindness in the world. From the 90s until date, the incidence of this complication has increased. Reactive oxygen species (ROS) is a free radical with impaired electron that usually participates in the redox mechanisms of some body molecules such as enzymes, proteins, and so on. In normal biological conditions, ROS is maintained in equilibrium, however its overproduction can lead to biological process called oxidative stress and this is considered the main pathogenesis of DR. The retina is susceptible to ROS because of high-energy demands and exposure to light. When the balance is broken, ROS produces retinal cell injury by interacting with the cellular components. This article describes the possible role of oxidative stress in the development of DR and proposes some treatment options based on its stages. The review of the topic shows that blindness caused by DR can be avoided by early detection and timely treatment.
Similar content being viewed by others
Diabetic retinopathy
According to WHO, diabetes mellitus is a chronic degenerative disease that occurs when the pancreas does not produce enough insulin or when the body does not effectively use the insulin produced by the pancreas. The high mortality and morbidity caused by diabetes is as a result of its vascular complications. Approximately 400 million people worldwide have type 2 diabetes, and more than 45% of them have diabetic retinopathy (DR). The progress of diabetes to retinopathy happens over time thus, DR is a time-dependent disease that develops in stages. The incidence increases to 50% at 10 years after the diagnosis of diabetes, and goes up to 90% at 25 years. These figures put this complication as the most common microvascular complication in diabetic patients and one of the major causes of acquired blindness in the world. This increase in prevalence may be attributed to prolonged survival of diabetic patients. In the United States, it is the leading cause of blindness among adults aged 20–74 years.1 The more advanced form of DR is diabetic macular edema (DME), which significantly increases the risk of blindness. Diabetic maculopathy is the result of multifactorial and complex alterations of the retinal capillaries in association with diabetes mellitus and it is divided into two forms, ischemic maculopathy and DME.2 The high mortality and morbidity caused by diabetes is as a result of its vascular complications.
Two of the complications of DR that threaten the vision of the patients are DME and proliferative DR.3 Patients with DM2 usually begin to develop retinopathy 7 years after diagnosis of the disease.4
Naruse et al5 suggests that DR cause reactive oxygen species (ROS) to increase the level of reactive oxygen metabolites. Catabolites of biomolecules such as nitric oxide (NO), catalase, glutathione peroxide, and lipoperoxide increase with the progression of DR in DM2 patients.6 High glucose level and diabetically induced activation of retinal vascularization is linked with elevation in the enzymatic activity of arginase as well as in the reduction of bioavailability of NO.7 The over activity of arginase plays an important role in the development of DR through its reducing effect on NO and increase of oxidative stress. One of the pathways for the generation of NO is through the activity of inducible nitric oxide synthase, an isoform of NOS. This enzyme acts on 1-arginine and converts it to 1-citrulline.8 NO produced from S-nitrosoglutathione (GSNO) plays a second messenger role and regulates the activity and expression of some proteins by A-nitrosylation and hence plays vital role in many cellular processes. It is involved in physiological functions such as vasodilation, neurotransmission, and host defense.
Diabetic retinopathy mechanism
In the biosynthetic pathway of hexosamine, there is an increase in the activity of dumping of post-translational modifications of Ser/Thr residues through O-linked β-N-acetylglucosamine (O-GlcNAc). This increased influx of residues is dumped on the proteins and thus, reduce their capacity to capture the blood glucose and in this way leads to diabetes. It is known that as in protein phosphorylation, O-GlcN acylation plays a regulatory role in many nuclear and cytoplasmic proteins.9 The development of different vascular complications (macro and micro) is one of the key risks of suffering from diabetes and in the ocular regions, and these complications usually culminate in DR.10
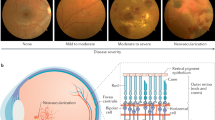
DR is the principal cause of blindness in working adults. The mechanism underlying this is the inflammation of the retinal blood vessel caused by deposit of arteriosclerotic plates produced by excess blood glucose and thus making them susceptible to microrupture leading to the leakage of fluids into the retina. If unchecked, there is a growth of new vessels that distorts the microvasculature of the retina and this eventually provokes retinal detachment.11, 12
The crucial point in the pathogenesis of the disease is inflammation in addition with oxidative stress.13 Its progress is characterized by loss of neuronal and pericytic cells that gives rise to growth of acellular-occluded capillaries. Such occlusion leads to the formation of microaneurysms and hence increased leucostasis resulting to the thickening of basal vascular membrane. The loss of pericyte cells begins with the stimulation of PKC-δ signaling by high level of blood glucose. This signaling cascade enhances the expression of protein kinase C-δ (PKC-δ, encoded by Prkcd) and p38 mitogen-activated protein kinase, and dephosphorylates PDGF receptors and diminishes its downstream signaling and thus brings about apoptotic death of the pericytic cells.14 The pericytic cell death gradually changes the architecture of the microvessels of the retina, a situation that provokes the collapse of blood–retinal barrier and hence extensive bleeding, microaneurysms exudates, and neovascularization that appear on the retinal surface.15
There is evidence indicating that local inflammation and oxidative stress are involved in the pathogenesis of DR and that they constitute crucial factors for the development of the disorder.16 In vascular inflammation, the involvement of biomolecules as lipoprotein-PLA2, pro-inflammatory cytokines (TNF-alpha and IL-1), and secretory phospholipase A2 IIA has been pinpointed.17
Since the underlying problem in this pathology is the high levels of blood glucose, the progressive damage can be retarded or completely abated by intensive insulin therapy. In addition, to reduce pericytic cell death, it has been found that thioredoxin, a novel gene and drug, is a potent therapeutic agent to prevent pericytic cell death and DR progression.18 Moreover, a comprehensive knowledge of cytokine-induced changes in lipid metabolism will promote the development of novel concepts and steer bench-to-bedside therapeutic developments.18
Screening and gene expression
DR prevention lies on its timely diagnosis achieved by a well-established medical care delivery plan based on a well-implemented screening program for the detection of its onset and its prompt medical treatment to reduce the incidence of radical management (vitrectomy) and blindness.19 British Diabetic Association established a standard value for DR screening program with a sensitivity of 80 and specificity of 95%, and has created a world record in DR screening with a coverage of 85.7%.
Chromosome 21 has a protective effect against DR as seen in Down’s syndrome patients with three copies of the chromosome and high level of endostatin, an anti-angiogenic protein from collagen XVIII whose gene is located in the chromosome 21.20 Patients with deleterious polymorphisms in the uncoupling protein 1 (UCP1) have a high risk of developing DR. In type I diabetic patients, the expression of this protein occurs in the retina and impacts downwardly in the production of ROS by the mitochondria. This was confirmed in a study carried out by Brondani et al,21 where it was reported that 3826A/G polymorphism affects UCP1 expression and decreases mitochondrial production of ROS. There is high energy consumption in the molecular pathways that contribute to retinal signal transduction with its consequences on the structure and function of this organ.22 Such elevated metabolic rates in the retina together with the vascularization play a part in the oxidative stress and influence age-related processes. In this way, high-energy demand increases the oxidative load and enhances, in chronic manner, the increase of oxidative stress and ROS to impressive levels. The frequent exposure of the eye to ambient oxygen, environmental chemicals, and sunlight makes the ocular tissues susceptible to damage by ROS. In addition, the free radical (FR) catalyzes peroxidation of long-chain polyunsaturated acids (LCPUFAs) as docosahexaenoic acid and arachidonic acid and brings about the generation of LCPUFA metabolites as well as neuroprostanes and isoprostanes, which exercise extra pharmacological and toxicological actions in the ocular tissues.23
Reactive radical species
Actually, it is known that a set of processes such as inflammation, the polyol pathway accumulation of advanced glycation end products, the flux of hexosamine pathway, and PKC activation are involved in the formation of FRs. These mechanisms appear to be associated with mitochondrial overproduction of ROS.24 In obesity and dyslipidemia, DR appears to be also associated with oxidation of fatty acids, resulting in the increased production of ROS by nicotinamide adenine dinucleotide phosphate oxidase.
The generation of FR occurs in varieties of pathways. However, an addition of an electron to a stable molecule is the most common. In the organism, majority of the molecules contain non-radicals, ie, there is only an even number of electrons in their atomic orbits. The FRs generated attain a stable state by interaction with other molecules through redox reactions involving electron transfer among the participating chemical species. In such electron transfer, a molecule is oxidized by losing free electrons (oxidation process), which is captured or gained by the other molecule (reduction process). The term oxidizing or oxidant agent refers to the molecule that loses electron, while reducing agent is the molecule that gains the electron. In a nutshell, the oxidation of one chemical species implies the reduction of another. In a reaction between a FR and a non-radical molecule, there are three possible results: (1) the FR molecule can gain an electron or (2) it can lose electron, or (3) bond with the non-radical molecule. The end result of such reaction is the conversation of the non-radical agent to FR, a situation which results in an unstoppable or chain reaction that is only detained when two FRs meet.25
FRs are classified depending on their functional groups.26 The oxygen FR has oxygen as the functional group, the thiol radical has sulfur (S), nitrogen radical contain nitrogen (N), and carbon radical has carbon (C) while phosphorous radical contains phosphorous (P). The influence of exogenous factors can exacerbate normal metabolic process of the production of FRs.27 The first and most common such exogenous influence is through normal metabolic processes and the second is from organic compounds such as alcoxyl, peroxyl, hydrogen peroxide, and singlet oxygen.28
The term ROS as hydrogen peroxide, hydroperoxides, hypochlorous acid, and epoxide metabolites, refers to chemical species that function like oxidizing agents but are not FRs (Table 1).29 Superoxide is mainly produced in the mitochondrial respiratory chain; however, the exact location and the precise mechanism underlying the production of physiologically relevant ROS remain to be known. Since the pathogenesis of many clinical disorders is linked to oxidative stress, it is very essential to have a good knowledge of the mechanism leading to the generation of ROS.30 mtDNA transcription is enhanced by mitochondrial transcription factor A. It has been found that this factor can undergo ubiquitinylation, ie, modified by covalent attachment of ubiquitin and this usually hampers its transport to the mitochondria. The end result is lower mtDNA transcription and mitochondrial dysfunction, a situation which can favor the development or progression of diabetes and hence DR. Therefore, the inhibition of ubiquitinylation restores mitochondrial homeostasis, and inhibits the development/progression of DR.31 Lipid peroxidation plays a notable role in the progression of DR.23 FRs such as hydroxyl and hydroperoxyl species with oxygen as functional group oxidize lipids and phospholipids, and at cellular level bring about membrane lipid peroxidation and in this way can trigger DR.
Prevention and treatment of diabetic retinopathy
Presently, new avenues of treatment of DR are being explored to cut down the incidence and progression of the disease. The need for adequate screening program for retinal surveillance for timely determination of retinal condition and perhaps level of damage has been reiterated. Moreover, new salvation treatment modalities have arisen and these have served as a source of hope even to patients with advanced DR, where it is calculated that 95% of them could continue with their vision when treated before the retina is severely damaged. These salvation treatment modalities are vitrectomy, corticosteroids, or Anti-VEGF injection into the eye and laser surgery. Though, all these treatment modalities are not DR curative, they can salvage the patient’s vision.
DR treatment depends on its stage or type. It should be remembered that this complication can be classified as nonproliferative and proliferative or macula edema. For the mild to moderate nonproliferative DR, the recommendation is a screening program well-implemented for the control of blood sugar and constant ophthalmological revision. Controlling diabetes and maintaining HbA1c level in the range of 6–7% are the goals in the optimal management of diabetes and DR. According to Diabetes Control and Complications Trial,32 if the levels of blood glucose are maintained, then the progression of DR will be substantially reduced. In the case of proliferative type or macular edema, the key treatment modality is surgery as photocoagulation where retinal tissues are burned using thermal energy. The principle underlying this is the injection of energy from a strong light source, which is absorbed by the retinal pigment epithelium that converts it into thermal energy that provokes necrotic coagulation with denaturation of cellular proteins as the temperature rises above 65°C.33 Actually, laser retinal photocoagulation is a therapeutic option in many retinal and eye conditions. The Early Treatment for Diabetic Retinopathy Study has found that laser surgery for macular edema reduces the incidence of moderate visual loss (doubling of visual angle or roughly a two-line visual loss) from 30 to 15% over a 3-year period.34 A 2-year result of The Diabetic Retinopathy Clinical Research network (DRCR.net) Randomized Trial Evaluating Ranibizumab Plus Prompt or Deferred Laser or Triamcinolone Plus Prompt Laser for Diabetic Macular Edema, known as the Laser-Ranibizumab-Triamcinolone for DME Study, demonstrated that ranibizumab with prompt or deferred focal/grid laser achieved superior visual acuity and optical coherence tomography outcomes compared with focal/grid laser treatment alone. In the ranibizumab groups, ~50% of the eyes had substantial improvement (10 or more letters) and 30% gained 15 or more letters. Intravitreal triamcinolone combined with focal/grid laser did not result in superior visual acuity outcomes compared with laser alone, but appear to have a visual acuity benefit similar to ranibizumab in pseudophakic eyes35 (Table 2).
Corticosteroids in diabetic retinopathy
Corticosteroids have shown to be useful in the treatment of DME. This complication of diabetes is actually treated using focal laser photocoagulation, vascular endothelial growth factor (VEGF) inhibitors, and intravitreal corticosteroid injections and implants. Anti-VEGF antibodies have revolutionized the treatment of DR but a significant subset of patients fail to respond to treatment and accumulating evidence indicates that inflammatory cytokines and chemokines other than VEGF may contribute to the disease process.36
Corticosteroids, dexamethasone, triamcinolone, and fluocinolone acetonide are an attractive treatment option because these drugs down regulate VEGF, and an array of cytokines, and in spite of increasing intraocular pressure, dexamethasone implant has demonstrated its benefit in the treatment of this disease.37 Level of intravitreal triamcinolone acetonide exposure is related to the development of elevated intraocular pressure and cataract; this does not seem to be the case for dexamethasone, where two different doses showed similar mean intraocular pressure and incidence of cataract surgery. With fluocinolone acetonide, rates of intraocular pressure elevations requiring surgery seem to be dose related, and available corticosteroids for DME exhibit different pharmacokinetic profiles that impact on efficacy and adverse events, and should be taken into account.38 In eyes with DME, intravitreal dexamethasone implant showed morphological and functional improvement as early as 1 month of its use and 4 months after the treatment,39 and switching to intravitreal corticosteroids may be of particular benefit to pseudophakic patients. Anti-VEGF combined with corticosteroid implant of sustained release is a promising option for refractory DME.40 Indeed, corticosteroids are of therapeutic benefit because of their anti-inflammatory, anti-angiogenic, and blood–retinal barrier stabilizing properties.
In spite of all these treatment options, laser photocoagulation, according to the guidelines of the Early Treatment of Diabetic Retinopathy Study (ETDRS), continues to be the primary standard care treatment in most communities.41
Anti-VEGF injection therapy
Anti-VEGF drugs are injected into the vitreous gel to block VEGF protein, which can stimulate the growth of abnormal blood vessels and leakage of fluid. VEGF is an endothelial cell-specific angiogenic factor, which plays a major role in the pathological condition as opposed to physiological and in ocular neovascularization leading to PDR. VEGF is also a vasopermeable factor, which increases vascular permeability by relaxing endothelial cell junctions and this mechanism is known to contribute to the development of DME. Inhibition of VEGF blocks these effects to some extent in DR, as demonstrated in several recent clinical trials and case series involving the anti-VEGF molecules. Currently, the anti-VEGF molecules being studied in the management of DR are: pegaptanib (Macugen), ranibizumab (Lucentis), bevacizumab (Avastin), and VEGF Trap-eye. Of the available VEGF antagonists, bevacizumab is the most frequently used outside a formal clinical trial because it is less expensive.42 Anti-VEGF therapy is currently indicated for DME associated with vision loss, whereas laser photocoagulation prevents severe vision loss in eyes with proliferative DR.43 Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME.
Vitrectomy
Vitrectomy is an important resource for the treatment of long-standing vitreous hemorrhage, tractional retinal detachment, and combined tractional and rhegmatogenous retinal detachment. However, its use in the treatment of epiretinal membrane formation and macular dragging is still uncommon. The Diabetic Retinopathy Vitrectomy Study has recommended the use of this procedure for the treatment of eyes with vitreous hemorrhage that fails to resolve spontaneously within 6 months. Early vitrectomy (<6 months, mean 4 months) results in the greater recovery of vision in patients with type 1 diabetes. Laser photocoagulation through indirect delivery systems or through the EndoProbe (Toronto, ON, Canada) can be performed as an adjunctive procedure during vitrectomy to initiate or continue laser treatment. In fact, ultrasound monitoring of the posterior segment of the eyes in search of signs of macular detachment is necessary in all cases of late type 1 diabetes.
Recent studies have focused on the introduction of NrF2 as a new treatment of DR. NrF2 is a transcription factor that masterminds cellular detoxification and redox (oxidation) response status, and so provides a protective action against various forms of oxidative stress and damage regulator. It also acts as cytoprotector and it is found in different natural compounds as polyphenols.44, 45
A deep understanding of the pathophysiology of DR and the underlying molecular mechanisms are essential for the development of new screening modalities that would improve and increase its timely detection and hence its timely prevention or treatment. Table 3 summarizes the treatment options for clinical management of DR complications.46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64 Table 4 also depicts the data of a study in an animal model where some pertinent particles believed to improve oxidative stress as well as prevent or delay DR development.65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75 It is a proven fact that oxidative stress enhances the progression of DR hence, decreasing the degree of such stress has been observed in clinical situations to contra arrest DR pathological problems. Guarantying the integrity of the neurons of the retina is a primordial factor in DR management. Damage of the retinal vessel can be protected if the retinal neurons are integrally and functionally maintained and the progression of DR can be abated. This highlights the importance of regular eye screening and aggressive control of glucose and blood pressure to prevent ocular damage,76 especially when we take into consideration that more than a half of young onset of diabetic patients manifest some degree of retinopathy within 10–12 years of diagnosis.
Conclusions
Obesity, poor glycemic control, and oxidative stress have been shown to contribute to the development of eye complications as DR. Diabetes is a complicated metabolic disorder with both short- and long-term undesirable events. Hence, diabetic patients should be educated on eye complications that may arise from their condition. Regular eye screening with fundus camera should be part of the routine management of diabetic patients. Oxidative stress reduction and restoration of retinal antioxidant system using exogenous antioxidants or anti-inflammatory drugs or food, which may improve postprandial hyperglycemia and adipose tissue metabolism, as well as dyslipidemia and insulin resistance to modulate carbohydrate and lipid metabolism should be the key modalities to fight against this disorder. We believe that all the events previously mentioned may be a promising issue for further research. The treatment depends on the stage of DR. The use of anti-VEGF in DME associated with vision loss has been recommended and laser photocoagulation can prevent severe vision loss in eyes with proliferative DR. According to the findings in the present paper, oxidative stress plays an important role in the pathophysiology of DR. Many studies have shown that different natural compounds, such as polyphenols, can suppress oxidative stress and inflammation through Nrf2 orientation and hence the activation of gene cytoprotectors related antioxidant response factor. Currently, the application of Nrf2 in the treatment of DR as cytoprotective mechanism in response to ischemic-reperfusion injury has been studied. The understanding of the mechanisms of oxidative stress is crucial in the development of new therapeutic strategies.
References
Holekamp NM . Managed care implications of diabetic macular edema. Am J Manag Care 2016; 22 (10 Suppl): s300–s306.
Haritoglou C, Kernt M, Wolf A . Diabetic maculopathy. Ophthalmologe 2015; 112: 871–883.
Kollias AN, Ulbig MW . Diabetic retinopathy early diagnosis and effective treatment. Dtsch Arztebl Int 2010; 107: 75–84.
Josifova T, Schneider U, Henrich PB, Schrader W . Eye disorders in diabetes: potential drug targets. Infect Disord Drug Targets 2008; 8: 70–75.
Naruse R, Suetsugu M, Terasawa T, Ito K, Hara K, Takebayashi K et al. Oxidative stress and antioxidative potency are closely associated with diabetic retinopathy and nephropathy in patients with type 2 diabetes. Saudi Med J 2013; 34: 135–141.
Rodríguez-Carrizalez AD, Castellanos-González JA, Martínez-Romero EC, Miller-Arrevillaga G, Villa-Hernández D, Hernández-Godínez PP et al. Oxidants, antioxidants and mitochondrial function in non-proliferative diabetic retinopathy. J Diabetes 2014; 6: 167–175.
Patel C, Rojas M, Narayanan SP, Zhang W, Xu Z, Lemtalsi T et al. Arginase as a mediator of diabetic retinopathy. Front Immunol 2013; 4: 173.
Pannu R, Singh I . Pharmacological strategies for the regulation of inducible nitric oxide synthase: neurodegenerative versus neuroprotective mechanisms. Neurochem Int 2006; 49: 170–180.
Semba RD, Huang H, Lutty GA, Van Eyk JE, Hart GW . The role of O-GlcNAc signaling in the pathogenesis of diabetic retinopathy. Proteomics Clin Appl 2014; 8 (3-4): 218–231.
Ezquer F, Ezquer M, Arango-Rodriguez M, Conget P . Could donor multipotent mesenchymal stromal cells prevent or delay the onset of diabetic retinopathy? Acta Ophthalmol 2014; 92: e86–e95.
Aylward GW . Progressive changes in diabetics and their management. Eye 2005; 19: 1115–1118.
Robison WG Jr, Kador PF, Kinoshita JH . Early retinal microangiopathy: prevention with aldose reductase inhibitors. Diabet Med 1985; 2: 196–199.
Bucolo C, Marrazzo G, Platania CB, Drago F, Leggio GM, Salomone S . Fortified extract of red berry, Ginkgo biloba, and white willow bark in experimental early diabetic retinopathy. J Diabetes Res 2013; 2013: 432695.
Geraldes P, Hiraoka-Yamamoto J, Matsumoto M, Clermont A, Leitges M, Marette A et al. Activation of PKC-δ and SHP-1 by hyperglycemia causes vascular cell apoptosis and diabetic retinopathy. Nat Med 2009; 15: 1298–1306.
Devi TS, Hosoya K, Terasaki T, Singh LP . Critical role of TXNIP in oxidative stress, DNA damage and retinal pericyte apoptosis under high glucose: implications for diabetic retinopathy. Exp Cell Res 2013; 319: 1001–1012.
Chiu CJ, Taylor A . Dietary hyperglycemia, glycemic index and metabolic retinal diseases. Prog Retin Eye Res 2011; 30: 18–53.
Williams M, Hogg RE, Chakravarthy U . Antioxidants and diabetic retinopathy. Curr Diab Rep 2013; 13: 481–487.
Chen H, Wen F, Zhang X, Su SB . Expression of T-helper-associated cytokines in patients with type 2 diabetes mellitus with retinopathy. Mol Vis 2012; 18: 219–226.
Papavasileiou E, Dereklis D, Oikonomidis P, Grixti A, Vineeth Kumar B, Prasad S et al. An effective programme to systematic diabetic retinopathy screening in order to reduce diabetic retinopathy blindness. Hell J Nucl Med 2014; 17 (Suppl 1): 30–34.
Ryeom S, Folkman J . Role of endogenous angiogenesis inhibitors in Down syndrome. J Craniofac Surg 2009; 20 (Suppl 1): 595–596.
Brondani LA, de Souza BM, Duarte GC, Kliemann LM, Esteves JF, Marcon AS et al. The UCP1 -3826A/G polymorphism is associated with diabetic retinopathy and increased UCP1 and MnSOD2 gene expression in human retina. Invest Ophth Vis Sci 2012; 53: 7449–7457.
Payne AJ, Kaja S, Naumchuk Y, Kunjukunju N, Koulen P . Antioxidant drug therapy approaches for neuroprotection in chronic diseases of the retina. Int J Mol Sci 2014; 15: 1865–1886.
Njie-Mbye YF, Kulkarni-Chitnis M, Opere CA, Barrett A, Ohia SE . Lipid peroxidation: pathophysiological and pharmacological implications in the eye. Front Physiol 2013; 4: 366, eCollection.
Brownlee M . The pathobiology of diabetic complications: a unifying mechanism. Diabetes 2005; 54: 1615–1625.
Halliwell B, Gutteridge JMC, Cross CE . Free radicals, antioxidants, and human disease: where are we now? J Lab Clin Med 1992; 119: 598–620.
Gaál T, Speake BK, Mezes M, Noble RC, Surai PF, Vajdovich P . Antioxidant parameters and ageing in some animal species. Comp Haematol Int 1996; 6: 208–213.
Miller JK, Brzezinska-SIebodzinska E, Madsen FC . Oxidative stress, antioxidants, and animal function. J Dairy Sci 1993; 76: 2812–2823.
Halliwell B, Gutteridge JMC . Oxygen toxicity, oxygen radical, transition metals and disease. Biochem J 1984; 219: 1–14.
Juarez Olguín H, Calderon Guzman D . Free radicals: formation, types and effects in central nervous system. In: Handbook of Free Radicals: Formation, Types and Effects. Nova Science Ed: New York, 2009.
Adam-Vizi V . Production of reactive oxygen species in brain mitochondria: contribution by electron transport chain and non-electron transport chain sources. Antioxid Redox Signal 2005; 7: 1140–1149.
Santos JM, Mishra M, Kowluru RA . Posttranslational modification of mitochondrial transcription factor A in impaired mitochondria biogenesis: implications in diabetic retinopathy and metabolic memory phenomenon. Exp Eye Res 2014; 121: 168–177.
Klein R . The diabetes control and complications trial. In: Kertes C (ed). Clinical Trials in Ophthalmology: A Summary and Practice Guide. Williams & Wilkins Pub, Baltimore, 1998, pp 49–70.
Glickman RD . Phototoxicity to the retina: mechanisms of damage. Int J Toxicol 2002; 21: 473–490.
Akduman L, Olk RJ . The early treatment for diabetic retinopathy study. In: Kertes C (ed). Clinical Trials in Ophthalmology: A Summary and Practice Guide. Williams & Wilkins Pub, Baltimore, 1998, 15–36.
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010; 117: 1064–1077.
Bolinger MT, Antonetti DA . Moving past anti-VEGF: novel therapies for treating diabetic retinopathy. Int J Mol Sci 2016; 17. pii: E1498.
Puliafito CA, Cousins SW, Bacharach J, Gonzalez VH, Holekamp NM, Merrill PT et al. Forming a consensus: data and guidance for physicians treating diabetic macular edema. Ophthalmic Surg Lasers Imaging Retina 2016; 47 (4 Suppl): S4–S15.
Yang Y, Bailey C, Loewenstein A, Massin P . Intravitreal corticosteroids in diabetic macular edema: pharmacokinetic considerations. Retina 2015; 35: 2440–2449.
Mastropasqua R, Toto L, Borrelli E, Di Antonio L, De Nicola C, Mastrocola A et al. Morphology and function over a one-year follow up period after intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema. PLoS One 2015; 10 (10): e0145663.
Hussain RM, Ciulla TA . Treatment strategies for refractory diabetic macular edema: switching anti-VEGF treatments, adopting corticosteroid-based treatments, and combination therapy. Expert Opin Biol Ther 2016; 16: 365–374.
Musat O, Cernat C, Labib M, Gheorghe A, Toma O, Zamfir M et al. Diabetic macular edema. Rom J Ophthalmol 2015; 59: 133–136.
Neelakshi B, Grigorian RA, Tutela A . Diabetic macular edema: pathogenesis and treatment. Surv Ophthalmol 2009; 54: 1–32.
Wong TY, Cheung CM, Larsen M, Sharma S, Simó R . Diabetic retinopathy. Nat Rev Dis Primers 2016; 2: 16012.
Nabavi SF, Barber AJ, Spagnuolo C, Russo GL, Nabavi SM, Sobarzo-Sánchez E . Nrf2 as molecular target for polyphenols: a novel therapeutic strategy in diabetic retinopathy. Crit Rev Clin Lab Sci 2016; 53 (5): 293–312.
Bai Y, Cui W, Xin Y, Miao X, Barati MT, Zhang C et al. Prevention by sulforaphane of diabetic cardiomyopathy is associated with up-regulation of Nrf2 expression and transcription activation. J Mol Cell Cardiol 2013; 57: 82–95.
McAuley AK, Wang JJ, Dirani M, Connell PP, Lamoureux E, Hewitt AW . Replication of genetic loci implicated in diabetic retinopathy. Invest Ophthalmol Vis Sci 2014; 55 (3): 1666–1671.
Kowluru RA, Zhong Q, Santos JM, Thandampallayam M, Putt D, Gierhart DL . Beneficial effects of the nutritional supplements on the development of diabetic retinopathy. Nutr Metab (Lond) 2014; 11: 8.
Hernández M, Garcia-Ramírez M, García-Rocha C, Saez-López C, Valverde AM, Guinovart JJ et al. Glycogen storage in the human retinal pigment epithelium: a comparative study of diabetic and non-diabetic donors. Acta Diabetol 2014; 51 (4): 543–552.
Rajashekhar G, Ramadan A, Abburi C, Callaghan B, Traktuev DO, Evans-Molina C et al. Regenerative therapeutic potential of adipose stromal cells in early stage diabetic retinopathy. PLoS One 2014; 9: e84671.
Elsherbiny NM, Ahmad S, Naime M, Elsherbini AM, Fulzele S, Al-Gayyar MM et al. ABT-702, an adenosine kinase inhibitor, attenuates inflammation in diabetic retinopathy. Life Sci 2013; 93: 78–88.
Abu El-Asrar AM, Nawaz MI, Siddiquei MM, Siddiquei MM . High-mobility group box-1 induces decreased brain-derived neurotrophic factor-mediated neuroprotection in the diabetic retina. Mediators Inflamm 2013; 2013: 863036.
Rivera JC, Sitaras N, Noueihed B, Hamel D, Madaan A, Zhou T . Microglia and interleukin-1β in ischemic retinopathy elicit microvascular degeneration through neuronal semaphorin-3A. Arterioscler Thromb Vasc Biol 2013; 33: 1881–1891.
Huang J, Li X, Li M, Li J, Xiao W, Ma W et al. Mitochondria-targeted antioxidant peptide SS31 protects the retinas of diabetic rats. Curr Mol Med 2013; 13: 935–945.
Omae T, Nagaoka T, Tanano I, Yoshida A . Adiponectin-induced dilation of isolated porcine retinal arterioles via production of nitric oxide from endothelial cells. Invest Ophthalmol Vis Sci 2013; 54: 4586–4594.
Zhong Q, Mishra M, Kowluru RA . Transcription factor Nrf2-mediated antioxidant defense system in the development of diabetic retinopathy. Invest Ophthalmol Vis Sci 2013; 54: 3841–3948.
He M, Pan H, Xiao C, Pu M . Roles for redox signaling by NADPH oxidase in hyperglycemia-induced heme oxygenase-1 expression in the diabetic retina. Invest Ophthalmol Vis Sci 2013; 54: 4092–4101.
Tan SM, Stefanovic N, Tan G, Wilkinson-Berka JL, de Haan JB . Lack of the antioxidant glutathione peroxidase-1 (GPx1) exacerbates retinopathy of prematurity in mice. Invest Ophthalmol Vis Sci 2013; 54: 555–562.
Ha Y, Saul A, Tawfik A, Zorrilla EP, Ganapathy V, Smith SB . Diabetes accelerates retinal ganglion cell dysfunction in mice lacking sigma receptor 1. Mol Vis 2012; 18: 2860–2870.
Qiu F, He J, Zhou Y, Bai X, Wu G, Wang X et al. Plasma and vitreous fluid levels of Dickkopf-1 in patients with diabetic retinopathy. Eye 2014; 28 (4): 402–409.
Kowluru RA, Kowluru A, Veluthakal R, Mohammad G, Syed I, Santos JM et al. TIAM1-RAC1 signalling axis-mediated activation of NADPH oxidase-2 initiates mitochondrial damage in the development of diabetic retinopathy. Diabetologia 2014; 57 (5): 1047–1056.
Cervellati F, Cervellati C, Romani A, Cremonini E, Sticozzi C, Belmonte G et al. Hypoxia induces cell damage via oxidative stress in retinal epithelial cells. Free Radic Res 2014; 48: 303–312.
Fu D, Yu JY, Wu M, Du M, Chen Y, Abdelsamie SA et al. Immune complex formation in human diabetic retina enhances toxicity of oxidized LDL towards retinal capillary pericytes. J Lipid Res 2014; 55 (5): 860–869.
Aung MH, Park HN, Han MK, Obertone TS, Abey J, Aseem F et al. Dopamine deficiency contributes to early visual dysfunction in a rodent model of type 1 diabetes. J Neurosci 2014; 34: 726–736.
Calderón GD, Juárez OH, Hernández GE, Valenzuela PA, Zamora DCD, Punzo SM . Mechanisms involved in the development of diabetic retinopathy induced by oxidative stress. Redox Rep 2016; 22 (1): 10–16.
Nebbioso M, Pranno F, Pescosolido N . Lipoic acid in animal models and clinical use in diabetic retinopathy. Expert Opin Pharmacother 2013; 14: 1829–1838.
Ola MS, Ahmed MM, Abuohashish HM, Al-Rejaie SS, Alhomida AS . Telmisartan ameliorates neurotrophic support and oxidative stress in the retina of streptozotocin-induced diabetic rats. Neurochem Res 2013; 38: 1572–1579.
Zhang SY, Li BY, Li XL, Cheng M, Cai Q, Yu F et al. Effects of phlorizin on diabetic retinopathy according to isobaric tags for relative and absolute quantification-based proteomics in db/db mice. Mol Vis 2013; 19: 812–821.
Tang J, Du Y, Lee CA, Talahalli R, Eells JT, Kern TS . Low-intensity far-red light inhibits early lesions that contribute to diabetic retinopathy: in vivo and in vitro. Invest Ophthalmol Vis Sci 2013; 54: 3681–3690.
Dong LY, Jin J, Lu G, Kang XL . Astaxanthin attenuates the apoptosis of retinal ganglion cells in db/db mice by inhibition of oxidative stress. Mar Drugs 2013; 11: 960–974.
Si YF, Wang J, Guan J, Zhou L, Sheng Y, Zhao J . Treatment with hydrogen sulfide alleviates streptozotocin-induced diabetic retinopathy in rats. Br J Pharmacol 2013; 169: 619–631.
Soufi FG, Mohammad-Nejad D, Ahmadieh H . Resveratrol improves diabetic retinopathy possibly through oxidative stress - nuclear factor κB - apoptosis pathway. Pharmacol Rep 2012; 64: 1505–1514.
Kumar B, Gupta SK, Srinivasan BP, Nag TC, Srivastava S, Saxena R et al. Hesperetin rescues retinal oxidative stress, neuroinflammation and apoptosis in diabetic rats. Microvasc Res 2013; 87: 65–74.
Silva KC, Rosales MA, Hamassaki DE, Saito KC, Faria AM, Ribeiro PA et al. Green tea is neuroprotective in diabetic retinopathy. Invest Ophthalmol Vis Sci 2013; 54: 1325–1336.
Du Y, Veenstra A, Palczewski K, Kern TS . Photoreceptor cells are major contributors to diabetes-induced oxidative stress and local inflammation in the retina. Proc Natl Acad Sci U S A 2013; 110: 16586–16591.
Gaspar JM, Martins A, Cruz R, Rodrigues CM, Ambrósio AF, Santiago AR . Tauroursodeoxycholic acid protects retinal neural cells from cell death induced by prolonged exposure to elevated glucose. Neuroscience 2013; 253: 380–388.
Rajalakshmi R, Amutha A, Ranjani H, Ali MK, Unnikrishnan R, Anjana RM et al. Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset type 1 and type 2 Diabetes. J Diabetes Complications 2014; 28 (3): 291–297.
Acknowledgements
We are grateful to Dr Cyril Ndidi Nwoye, a native English speaker and language professor, for the critical review and translation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Calderon, G., Juarez, O., Hernandez, G. et al. Oxidative stress and diabetic retinopathy: development and treatment. Eye 31, 1122–1130 (2017). https://doi.org/10.1038/eye.2017.64
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.64
This article is cited by
-
OCT biomarkers as predictors of visual improvement in diabetic macular edema eyes receiving dexamethasone implants
International Journal of Retina and Vitreous (2023)
-
Is metformin neuroprotective against diabetes mellitus-induced neurodegeneration? An updated graphical review of molecular basis
Pharmacological Reports (2023)
-
The potential effects and mechanisms of hispidulin in the treatment of diabetic retinopathy based on network pharmacology
BMC Complementary Medicine and Therapies (2022)
-
Comparison of catalase, glutathione peroxidase and malondialdehyde levels in tears among diabetic patients with and without diabetic retinopathy
Journal of Diabetes & Metabolic Disorders (2022)
-
Carvacrol protects the ARPE19 retinal pigment epithelial cells against high glucose-induced oxidative stress, apoptosis, and inflammation by suppressing the TRPM2 channel signaling pathways
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)