Abstract
Purpose
To elucidate the prevalence and risk factors of age-related macular degeneration (AMD) in people with diabetes.
Methods
Of the 5495 subjects ≥60 years of age recruited in the population-based study in south India, 4791 subjects with gradable images on 30° three-field retinal photographs were analyzed. AMD and diabetic retinopathy (DR) were graded based on the International ARM Epidemiological Study Group classification and International Clinical Diabetic Retinopathy Disease Severity Scale, respectively. All subjects underwent a detailed history, physical examination, and a comprehensive ocular examination.
Results
Of the 4791 subjects, 1256 had diabetes. In those with diabetes, 166 (13.2%) had DR: of which, 9.6% had AMD. Of those with diabetes but no DR, 15.6% had AMD. Presence of DR (OR=0.57, 95% CI: 0.33–0.99, P=0.046) was a protective factor for AMD in diabetes. When adjusted for potential confounding factors, those with AMD and diabetes were from urban areas (OR=1.65, 95% CI: 1.09–2.49, P=0.018), had raised systolic blood pressure (OR=1.02, 95% CI: 1.00–1.03, P=0.01), higher BMI (OR=1.06, 95% CI: 1.02–1.10, P=0.005), and higher serum triglycerides (OR=1.00, 95% CI: 1.00–1.01, P=0.011). A higher level of high-density lipoprotein (HDL) (OR=0.98, 95% CI: 0.96–0.99, P=0.038) was a protective factor for AMD in subjects with diabetes.
Conclusions
The presence of DR and higher serum HDL are protective factors whereas obesity and higher systolic blood pressure are risk factors for AMD in subjects with diabetes.
Similar content being viewed by others
Introduction
In developed and developing countries, age-related macular degeneration (AMD) is the leading cause of vision loss in those aged 60 years or older,1 and the morbidity is expected to rise with the increase in life expectancy. India has about 77 million people at or above the age of 60 years representing a large group vulnerable to vision-related disorders, and the number is estimated to reach 180 million by 2026. As reported in population-based studies, the prevalence of AMD in India ranges from 39.5% to 0.3%.2, 3, 4 These proportions are likely to increase further with an increase in the proportion of aging populations. Diabetes mellitus (DM) has been reported as a significant risk factor for AMD in a few studies5, 6, 7, 8 whereas few others have reported diabetes as a protective factor.9, 10 Chen et al11 in their meta-analysis showed that a majority of studies that reported DM as a risk factor for AMD had adjusted only for age and gender and may be confounded by other factors and, therefore, requires well-designed studies. In our recent study,9 we reported lower prevalence of AMD in subjects with diabetes than in those without diabetes; we observed that diabetes is a protective factor for AMD when adjusted for several potential confounding factors. In this study, we further explore and characterize in those with AMD, the distribution of systemic and ocular risk factors that may have contributed to the difference in the prevalence and the risk of AMD in subjects with and without diabetes.
Materials and methods
Sankara Nethralaya: Rural-Urban Age-related Macular Degeneration study (SN-RAM study), a population-based cross-sectional study, was conducted in India between 2009 and 2011. The study was approved by the institutional review board and a written consent was obtained from all the participating subjects as per the Declaration of Helsinki.
Study participants
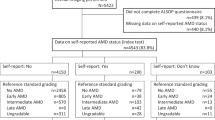
The study design and methodology have been described earlier.9, 12 Briefly, a total of 6617 people (rural (n=3904) and urban (n=2713)) were enumerated. Of which, 5495 (83%) participated in the study for eye examination; after excluding those who did not have retinal photographs and those with ungradable images, 4791 subjects (rural (n=2743) and urban (n=2048)) were included in this study.
Clinical examination protocol
A detailed history, including data on demographic, socioeconomic, and ocular history, was obtained from all patients at the base hospital in the urban arm and in a customized mobile examination unit in the rural arm. The socioeconomic status (SES) was assessed using a multiple index questionnaire and the scoring was characterized as low (score, 0–14), middle (score, 15–28), and high (score, 29–42).13 The questionnaire included the following variables: family possession such as refrigerator, television, washing machine, and so on, own or rented house, type of house (thatched or brick), possession of vehicle (car, scooter, etc), and other financial liability or commitment. The same questionnaire and scoring has been used in a previous population-based study.12 A detailed questionnaire was administered regarding the medical history, a general physical examination, smoking, tobacco and alcohol consumption history, and educational and occupational history. Blood pressure (BP) was recorded in the sitting position in the right arm to the nearest 2 mm Hg using the mercury sphygmomanometer (Diamond Deluxe BP apparatus, Pune, India). Two readings were taken, 5 min apart, and their mean was taken as the BP.14
Ophthalmic examination
All subjects underwent detailed ophthalmic evaluation, which included assessment of visual acuity and refraction using modified Early Treatment Diabetic Retinopathy Study chart (Low Vision Products; LightHouse, New York, NY, USA), anterior segment examination using a Zeiss SL 130 (Carl Zeiss, Jena, Germany) slit-lamp, intraocular pressure measurement using Goldmann applanation tonometer (Zeiss AT 030; Carl Zeiss), and fundus examination using binocular indirect ophthalmoscope (Keeler Instruments, Broomall, PA, USA). Grading of lens opacities was performed using the Lens Opacities Classification System (LOCS III; Leo T. Chylack, Harvard Medical School, Boston, MA, USA) by two experienced ophthalmologists. The grading agreements were as follows: nuclear opalescence (k=0.84), nuclear color (k=0.88), cortical (k=0.89), and posterior subcapsular (k=0.89). Overall, the average grading agreement was high (k=0.85).
Retinal photographs were obtained after pupillary dilatation (FF450 Fundus Camera, Carl Zeiss, Jena, Germany). AMD was graded according to the International ARM Epidemiological Study Group and stratified into stages based on the grading in the worst eye.15 The grading agreement, which was done by two independent observers (retina specialists) in a masked manner, was found to be 0.62 for early AMD and 0.87 for late AMD.
Diabetic retinopathy (DR) was graded using the International Clinical Diabetic Retinopathy Disease Severity Scale. The grading agreement between the observers was 0.80.16
All subjects underwent estimation of fasting blood glucose by enzymatic assay (Merck Micro Lab 120 semi-automated analyzer), total serum cholesterol (CHOD-POD method), high-density lipoproteins (HDL; CHOD-POD method after protein precipitation), serum triglycerides (CHOD-POD method), hemoglobin (calorimetric hemoglobinometer), and packed cell volume (capillary method).
Definitions
Refractive errors
Emmetropia was defined as a spherical equivalent between −0.50 and +0.50 diopter sphere (DS).17 Myopia was defined as a spherical equivalent of less than −0.50 DS. Hyperopia was defined as a spherical equivalent of greater than +0.50 DS. Astigmatic correction was measured in minus cylinder format and was defined as a cylindrical error of less than −0.50 diopter cylinder at any axis. Axial length (mm) was assessed by B-scan ultrasonography (USG), (Ultrascan, Alcon Laboratories, Sinking Spring, PA, USA) by applanation technique. Three readings were taken within 0.02 mm of each other and averaged.
Age-related maculopathy
AMD was graded according to the International AMD Epidemiological Study Group15 and stratified into stages based on the grading in the worst eye. Early AMD was defined as the presence of drusen (discrete whitish-yellow spots located external to the neuroretina or retina pigment epithelium [RPE]) or drusen with RPE abnormalities (areas of hyper- or hypopigmentation). Late AMD was defined as the presence of dry AMD (geographic atrophy of the RPE in the absence of neovascular AMD) or neovascular AMD (RPE detachments, which may be associated with neurosensory retinal detachment, subretinal or sub-RPE neovascular membranes, epiretinal, intraretinal, subretinal, or subpigment epithelial scar/glial tissue or fibrin-like deposits, and subretinal hemorrhages not related to other retinal vascular disease).
Diabetic retinopathy
In the study, levels of retinopathy were used and defined as follows: no DR, no abnormality; mild nonproliferative diabetic retinopathy (NPDR), only microaneurysms; moderate NPDR, more than mild but less than severe; severe NPDR, any of the following—20 or more intraretinal hemorrhages in 4 quadrants, venous beading in >2 quadrants, or intraretinal neovascularization in 1 quadrant; proliferative diabetic retinopathy, one or more of the following—neovascularization or preretinal or vitreous hemorrhage.
Diabetes
Known diabetes: if they were using hypoglycemic drugs, either oral or insulin or both. Provisional diabetes: if fasting blood glucose was ≥110 mg/dl (Accutrend Alpha, Roche Diagnostics, Indianapolis, IN, USA), done twice in new asymptomatic subject.18
Newly diagnosed diabetes: all individuals with provisional diabetes underwent oral glucose tolerance test for confirmation.19
All continuous variables were assessed for normality of distribution. Variables that did not follow a normal distribution were assessed using non-parametric tests. The proportions were examined using the χ2-test. The associations were examined by univariate and step-wise multiple logistic regression analysis.
Results
In the overall 5495 subjects, DM was present in 20.9% in the rural (n=681/3266) and 30.9% in the urban population (n=689/2229), and the differences between rural and urban populations were significant, P<0.0001. After excluding those who did not have retinal photographs and those with ungradable images, there were 4791 eligible subjects with gradable retinal photographs. The prevalence of AMD in this cohort was 22.1% (n=619/2743) in the rural and 18.1% (n=370/2048) in urban populations, and the differences were significant, P<0.0001.
In the cohort of 4791 subjects, there were 1256 subjects with DM (26.2%) and 3535 subjects with no DM (73.8%). Figure 1 shows the prevalence of AMD in subjects with diabetes (DM), no diabetes, DR, and no DR. The prevalence of AMD was found to be lower among people with diabetes than among those without diabetes (14.8 vs 22.7%, P<0.0001). In those subjects with DM, 166 (13.2%) had DR whereas 1090 (86.8%) had no DR. AMD was present in 16 subjects (9.6%) with DR (87.5% moderate NPDR and 12.5% mild NPDR) and in 170 (15.6%) with DM but no DR. The above difference in the proportion of subjects with AMD in those with and without DR was significant, z=−2.013, P=0.044. In the non-diabetic group, AMD was present in 803 (22.7%) subjects as compared to only 186 (14.8%) in subjects with DM, and the differences were statistically significant, z=−5.947, P<0.001. With regards to the type of AMD in DM group, a majority (170/186=91.4%) of those with DM had Early AMD, while the remaining (16/186=8.6%) subjects had Late AMD. The differences in the proportion of subjects with Early and Late AMD did not differ in the groups with and without DM, P=0.606. (Table 1) With regards to the subtypes of AMD in DM group, 48.9% (95% CI: 41.8–56.1) had only drusen, 21.0% (95% CI: 15.7–27.4) had drusen with hyperpigmentation, 21.5% (95% CI: 16.2–30.0) had drusen with hypopigmentation, 3.2% (95% CI: 1.5–6.9) had dry AMD and the remaining 5.4% (95% CI: 3.0–9.6) had wet AMD. In the No DM group, 90.2% had Early AMD and the remaining 9.8% had Late AMD. With regards to the subtypes of AMD in the No DM group, 51.6% had only drusen, 22.7% had drusen with hyperpigmentation, 15.8% had drusen with hypopigmentation, 6.5% had dry AMD and the remaining 3.4% had wet AMD. We then examined for likely risk and protective factors for AMD in subjects with DM (n=186) and without DM (n=803).
Table 2 shows the demographic and clinical variables in subjects with AMD, with and without DM. There were significant differences in the rural-urban distribution of subjects with AMD with and without DM, P<0.0001. Subjects in the DM group had raised mean systolic BP (132.7 mm Hg) when compared with those in the non-diabetic group (126.5 mm Hg), P<0.001. Those with AMD and DM had higher mean body mass index (BMI; 23.5 kg/m2) compared to those with AMD and No DM (21.7 kg/m2), P<0.001. The mean serum triglyceride levels were higher in those with AMD with DM (115.1 mg/dl) than in those with AMD but no DM (103.9 mg/dl), P=0.013. Among those who were from middle socioeconomic group, 53.2% of the subjects had AMD and DM, while among those from low socioeconomic group, only 42.5% had AMD and DM. The two groups did not differ in terms of age (P=0.701), gender distribution (P=0.560), diastolic BP (P=0.445), serum total cholesterol (P=0.053) or serum HDL cholesterol (P=0.062).
When compared to subjects with AMD but No DM, subjects with AMD and DM had an average 0.8 mm Hg higher intraocular pressure, which although not clinically significant, was statistically significant (P=0.001); a greater proportion of subjects were found to have hyperopia (44.4%; P=0.001) and a lesser proportion (38.3%) of subjects had myopia (P<0.001). As a subsequent analysis, subjects who had myopia and nuclear sclerosis were excluded and the remaining proportion of subjects were compared between the two groups. There were 14 subjects with myopia (not related to nuclear sclerosis (NS)) and AMD. Of which, a majority (n=13, 92.8%) belonged to the No DM group. The difference in the proportion of subjects with myopia (not related to NS) in the group with AMD and DM vs AMD with No DM was not significant, P=0.140. Sixteen (8.6%) subjects with DM and AMD had DR. The presence of DR was a protective factor for AMD in subjects with DM (OR=0.57, 95% CI: 0.33–0.99, P=0.046). Axial length was stratified into three groups; axial length did not differ significantly in the groups with AMD, with DM and with No DM (P≥0.076).
A subsequent analysis was performed in subjects with AMD and DM, with and without DR, with regards to type of AMD, axial length, BP, BMI, and serum lipids levels. A summary of these variables is presented in Table 3. In those with DR, 87.5% of subjects had Early AMD and the remaining 12.5% subjects had Late AMD. In the No DR group, 91.8% had Early AMD and the remaining 8.2% had Late AMD (P=0.558). The systolic BP (P=0.519), diastolic BP (P=0.521), axial length (P=0.913), BMI (P=0.495), serum total cholesterol (P=0.794), and HDL (P=0.622) did not differ between subjects with and without DR. The serum triglycerides were higher in the group with DR compared to those with DM but no DR (mean±SD: 110.0±49.3 mg/dl vs 168.3±84.6 mg/dl, P=0.014).
While in the no AMD and diabetes group, the mean±SD of systolic BP in subjects with no DR was 130.5±18.5 mm Hg compared with 136.7±20.8 mm Hg in the DR group and the differences were significant, P<0.0001. The diastolic BP in the two groups was not significantly different (P=0.842).
Table 4 shows the multivariate analysis of risk and protective factors in the AMD population with and without DM. Those with AMD and diabetes were predominantly from urban areas (OR=1.65, 95% CI: 1.09–2.49, P=0.018), had raised systolic BP (OR=1.02, 95% CI: 1.01–1.03, P=0.01), higher BMI (OR=1.06, 95% CI: 1.03–1.11, P<0.005) when adjusted for age, gender, SES, BP, serum lipids, smoking, cataract status, intraocular pressure, axial length and refractive error in the multivariate model. Higher HDL level was a protective factor for AMD in subjects with diabetes (OR=0.98, 95% CI: 0.96–0.99, P=0.038). Serum triglycerides demonstrated an OR of 1.00, 95% CI: 1.00–1.01, P=0.011.
Discussion
This study was a subgroup analysis of the SN-RAM cohort to elucidate the prevalence and risk factors for AMD in subjects with diabetes. The prevalence of AMD was found to be lower among people with diabetes than among those without diabetes (14.8 vs 22.7%). The prevalence was lower in subjects with DR than in those with no DR (9.6 vs 15.6%). The factors associated with AMD in subjects with diabetes were higher systolic BP, higher BMI, and urban population, whereas the protective factors were higher serum HDL cholesterol and presence of DR.
In the literature, there is no consistently observed association between AMD and diabetes. We recently9 reported lower prevalence of AMD in subjects with diabetes than in those without diabetes and we concluded that diabetes seems to be a protective factor for AMD. In this study, we further examined and characterized the distribution of systemic and ocular factors in subjects with AMD in the groups with and without diabetes, which may possibly shed more light on this finding.
The proportion of subjects with Early AMD as well as that of Late AMD did not differ significantly between the groups with DM and with No DM. Furthermore, the subtypes of AMD did not differ significantly in those with AMD and DM compared with AMD and No DM. A previous study6 reported that DM is a risk factor for early AMD compared with no early AMD; the multivariate analysis was slightly different to that of the present study whereby, the model was adjusted for age, gender, smoking, obesity and hypertension and hence the association may be different from that of our study. In our study, we compared Early AMD in DM and No DM and found no significant association.
We observed that DR is a protective factor for AMD in subjects with diabetes. We observed no significant association between early AMD and DR or that between late AMD and DR probably because of relatively smaller sample sizes.
The findings of our study are in agreement with those of Borrone et al10 who observed lower prevalence of AMD among subjects with diabetes and a further lower prevalence among those with DR. Mitchell and Wang et al7 observed a significant relationship only between diabetes and geographical atrophy (a type of late AMD) but not with early AMD, and they reported that there is no consistent relationship between AMD and diabetes. The Framingham Eye Study20 found no significant association between diabetes and AMD.
The conflicting results may be probably due to various systemic and ophthalmic variables examined, variations in age group examined, and the study design (longitudinal or cross-sectional). DR is a disease that affects predominantly the inner retina whereas AMD affects the outer retina altering the macula, possibly having different mediating mechanisms. Sander et al21 reported that in diabetic macular edema, there is signaling from the damaged inner blood–retina barrier (BRB) that induces upregulation of the transport function of the RPE (outer BRB), thus delaying the development of the age-related maculopathy.
Inner BRB damage has been documented with increasing severity of DR. Qaum et al22 have shown a vascular endothelial growth factor (VEGF)-driven inner BRB damage in early diabetes. Thus, the influence on outer BRB seems to be evident in diabetes both with and without DR. This feature may offer a likely explanation for observing lower prevalence of AMD in both groups.
In the diabetic population (n=1256), a comparison of systolic and diastolic BP was performed in those with and without DR. The systolic BP was significantly higher in those with DR (mean SD: 136.4±20.6 vs 130.8±18.3, P<0.0001) compared to those with No DR; while diastolic BP was not significantly different (P=0.691; data not shown). In those with DM and No AMD, the mean systolic BP was about 6 mm Hg higher in those with DR compared to those with no DR. In contrast, in those with AMD and DM, we observed no significant differences between those with and without DR, probably because of relatively lower sample sizes. Previous studies have shown that a rise in systolic BP is associated with RPE depigmentation and AMD, probably due to the effect on choroidal circulation. Dimitrova et al23 have shown that both choroidal and retinal circulation is affected in diabetes. Nagaoka et al24 also found a significant reduction in choroidal blood flow in the foveal region among people with diabetes. Probably due to the additive effect on choroidal circulation in aging diabetes, rise in systolic BP may be a risk factor for AMD.
Some studies25, 26, 27 have found an increased risk of AMD in individuals with higher BMI, whereas others have failed to observe this correlation.4, 28 We have earlier reported9 the risk factors for AMD in the same cohort and did not find increasing BMI as a risk factor. However, in the subgroup with diabetes, increasing BMI is a risk factor for AMD; BMI is not significantly associated with DR in this group. Studies have shown that angiogenic/anti-angiogenic factors are associated with obesity, diabetes, and complications related to diabetes.29 For example, pigment epithelium-derived factor, a major angiogenic inhibitor, is an active player in adipose tissue formation, insulin resistance, and vascular function. The increased risk of AMD in people with diabetes may be due to interplay of these factors. We had previously9 reported an association of middle SES and AMD in the general population (with or without diabetes). In this subgroup analysis, we observed no significant association between SES and AMD in people with diabetes when adjusted for several potential confounding factors. Likewise, we have earlier reported that the prevalence of diabetes is higher in people belonging to middle and high socioeconomic status, but there was no difference in prevalence of DR.30
Similar to our study, Beaver Dam Study25 and the study by Reynolds et al26 found a protective effect of higher serum HDL cholesterol on AMD. This could be probably due to the anti-inflammatory and anti-oxidant properties of HDL, which may play a role in regulating the inflammatory markers and endothelial dysfunction in diabetes, thus offering protection against AMD. However, we observed that serum triglycerides did not show a significant association with AMD and diabetes, when adjusted for potential confounding factors.
We observed that AMD in diabetes is more common in urban populations than in rural populations. We previously9 reported that AMD is more frequent in rural populations. In this study, we observed that DM is more common in the urban population than rural populations. Modernization and changes in lifestyle including lack of physical exercise or sedentary work31 may be an explanation for observing more frequent DM in urban populations and for observing greater proportion of people with AMD in urban diabetic population.
The strengths of this study included the use of standardized protocol and the photographic documentation of the macula. However, due to the cross-sectional design, a cause–effect relationship could not be established. In addition, the OR for the associated factors are only just above 1.00 and this observation must be kept in mind when interpreting the results.
AMD and DR are responsible for much of the legal blindness worldwide. Despite the epidemiological importance of both these conditions and the shared pathophysiological aspects, the works of literature on association of these are conflicting and scarce. This study highlights the prevalence, risk factors, and protective factors of AMD in people with diabetes. It also identifies the modifiable risk factors for AMD in those with diabetes. Thus, there could be a role in modifying lifestyle in reducing the burden of blindness from AMD in people with diabetes.

References
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the y ear 2002. Bull World Health Organ 2004; 82: 844–851.
Krishnan T, Ravindran RD, Murthy GVS, Vashist P, Fitzpatrick KE, Thulasiraj RD et al. Prevalence of early and late age-related macular degeneration in India: The INDEYE Study. Invest Ophthalmol Vis Sci 2010; 51: 701–707.
Kulkarni SR, Aghashe SR, Khandekar RB, Deshpande MD . Prevalence and determinants of age-related macular degeneration in the 50 years and older population: A hospital based study in Maharashtra, India. Indian J Ophthalmol 2013; 61: 196–201.
Krishnaiah S, Das T, Nirmalan PK, Nutheti R, Shamanna BR, Rao GN et al. Risk factors for age-related macular degeneration: Findings from the Andhra Pradesh eye disease study in South India. Invest Ophthalmol Vis Sci 2005; 46: 4442–4449.
Topouzis F, Anastasopoulos E, Augood C, Bentham GC, Chakravarthy U, de Jong PT et al. Association of diabetes with age-related macular degeneration in the EUREYE study. Br J Ophthalmol 2009; 93: 1037–1041.
Choi JK, Lym YL, Moon JM, Shin HS, Cho B . Diabetes mellitus and early age-related macular degeneration. Arch Ophthalmol 2011; 129: 196–199.
Mitchell P, Wang JJ . Diabetes, fasting blood glucose and age-related maculopathy: The Blue Mountains Eye Study. Aust N Z J Ophthalmol 1999; 27: 197–199.
Hahn P, Acquah K, Cousins SW, Lee PP, Sloan FA . Ten-year incidence of age-related macular degeneration according to diabetic retinopathy classification among medicare beneficiaries. Retina 2013; 33: 911–919.
Raman R, Pal SS, Ganesan S, Gella L, Vaitheeswaran K, Sharma T . The prevalence and risk factors for age-related macular degeneration in rural–urban India, Sankara Nethralaya Rural–Urban Age-related Macular Degeneration Study, Report No. 1. Eye (Lond) 2016; 30: 688–697.
Borrone R, Saravia M, Bar D . Age-related maculopathy and diabetes. Eur J Ophthalmol 2008; 18: 949–954.
Chen X, Rong SS, Xu Q, Tang FY, Liu Y, Gu H et al. Diabetes mellitus and risk of age-related macular degeneration: A systematic review and meta-analysis. PLoS One 2014; 9: e108196.
Agarwal S, Raman R, Paul PG, Rani PK, Uthra S, Gayathree R et al. Sankara Nethralaya-Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS 1): Study design and research methodology. Ophthalmic Epidemiol 2005; 12: 143–153.
Oakes JM, Rossi PH . The measurement of SES in health research: Current practice and steps towards a new approach. Soc Sci Med 2003; 56: 769–784.
van Leeuwen R, Ikram MK, Vingerling JR, Witteman JC, Hofman A . de Jong PT. Blood pressure, atherosclerosis, and the incidence of age-related maculopathy: The Rotterdam Study. Invest Ophthalmol Vis Sci 2003; 44: 3771–3777.
Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD et al. The international ARM epidemiological study group. An international classification and grading system for age related maculopathy and age related macular degeneration. Surv Ophthalmol 1995; 39: 367–374.
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003; 110: 1677–1682.
Dandona L, Dandona R, Naduvilath TJ, Srinivas M, McCarty CA, Rao GN . Refractive errors in an urban population in Southern India: The Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci 1999; 40: 2810–2818.
Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan DM, Peterson CM et al. Tests of glycemia in diabetes. Diabetes Care 2003; 26 (Suppl 1): S106–S108.
American Diabetes Association. Summary of revisions for the 2007 clinical practice recommendations. Diabetes Care 2007; 30 (Suppl 1):S3.
Kahn HA, Leibowitz HM, Ganley JP, Kini MM, Colton T, Nickerson RS et al. The Framingham Eye Study. II. Association of ophthalmic pathology with single variables previously measured in the Framingham Heart Study. Am J Epidemiol 1977; 106: 33–41.
Sander B, Larsen M, Moldow B, Lund-Andersen H . Diabetic macular edema: Passive and active transport of fluorescein through the blood–retina barrier. Invest Opthalmol Vis Sci 2001; 42: 433–438.
Qaum T, Xu Q, Joussen AM, Clemens MW, Qin W, Miyamoto K et al. VEGF-initiated blood retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci 2001; 42: 2408–2413.
Dimitrova G, Kato S, Tamaki Y, Yamashita H, Nagahara M, Sakurai M et al. Choroidal circulation in diabetic patients. Eye (Lond) 2001; 15 (Pt 5): 602–607.
Nagaoka T, Kitaya N, Sugawara R, Yokota H, Mori F, Hikichi T et al. Alteration of choroidal circulation in the foveal region in patients with type 2 diabetes. Br J Ophthalmol 2004:88: 1060–1063.
Klein R, Cruickshanks KJ, Nash SD, Krantz EM, Nieto FJ, Huang GH et al. The prevalence of age-related macular degeneration and associated risk factors: The Beaver Dam Offspring Study. Arch Ophthalmol 2010; 128: 750–758.
Reynolds R, Rosner B, Seddon JM . Serum lipid biomarkers and hepatic lipase gene associations with age-related macular degeneration. Ophthalmology 2010; 117: 1989–1995.
Zhang QY, Tie LJ, Wu SS, Lv PL, Huang HW, Wang WQ et al. Overweight, obesity, and risk of age-related macular degeneration. Invest Ophthalmol Vis Sci 2016; 57: 1276–1283.
Klein R, Clegg L, Cooper LS, Hubbard LD, Klein BE, King WN et al. Prevalence of age-related maculopathy in the atherosclerosis risk in Communities Study. Arch Ophthalmol 1999; 117: 1203–1210.
Friedman E . The role of the atherosclerotic process in the pathogenesis of age-related macular degeneration. Am J Ophthalmol 2000; 130: 658–663.
Raman R, Rani PK, Reddi Rachepalle S, Gnanamoorthy P, Uthra S, Kumaramanickavel G et al. Prevalence of diabetic retinopathy in India: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study Report 2. Ophthalmology 2009; 116: 311–318.
Ramachandran A, Snehalatha C, Latha E, Manoharan M, Vijay V . Impacts of urbanisation on the lifestyle and on the prevalence of diabetes in native Asian Indian population. Diabetes Res Clin Pract 1999; 44: 207–213.
Acknowledgements
This work has been funded by Jamsetji Tata Trust, Mumbai, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Srinivasan, S., Swaminathan, G., Kulothungan, V. et al. Age-related macular degeneration in a South Indian population, with and without diabetes. Eye 31, 1176–1183 (2017). https://doi.org/10.1038/eye.2017.47
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.47
This article is cited by
-
Effects of diabetic retinopathy on longitudinal morphological changes in AMD-associated type 1 macular neovascularization
Scientific Reports (2023)
-
Prevalence of age-related macular degeneration among optometric telemedicine users in Spain: a retrospective nationwide population-based study
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)