Abstract
Purpose
To correlate function and structural optical coherence tomography (OCT) to optical coherence tomography angiography (OCT-A) measures in patients affected by central serous chorioretinopathy (CSC) and to describe their changes after treatments (ie oral eplerenone, half-fluence photodynamic therapy (PDT)).
Patients and methods
Twenty eyes of 16 consecutive patients with treatment-naïve CSC undergoing either eplerenone or PDT were enrolled in this prospective, observational study. All patients underwent structural OCT and OCT-A at baseline and after therapy at months 1 and 3.
Results
Eleven eyes of nine patients and nine eyes of seven patients underwent eplerenone or PDT treatment, respectively. Central macular thickness (CMT) and subretinal fluid (SRF) correlated to fovea avascular zone (FAZ) area (r=0.74 and r=0.71, P=0.01) and vessel density (r=0.77 and r=0.68, P=0.01) at deep capillary plexus (DCP). CMT (P=0.0011), SRF (P=0.0005), SFCT (P=0.0016), FAZ area at DCP (P=0.0334) improved at 3-month visit. A significant reduction of deep FAZ area was appreciated in eplerenone (P=0.0204) but not in PDT (P=0.5) group. SFCT reduction was significantly higher in PDT than eplerenone group (P=0.0347).
Conclusion
Structural and vascular parameters are correlated in CSC and they improve after different treatments. Both half-fluence PDT and oral eplerenone do not permanently damage choriocapillaris or other choroidal layers as evaluated by OCT-A.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is the fourth cause of vision-threatening retinopathy affecting people aged between 39 and 51 years with an estimated incidence of 9.9 and 1.7 per 100 000 individuals in men and women, respectively.1, 2 CSC is characterized in its acute stage by accumulation of subretinal fluid (SRF) beneath the neurosensory retina and pigment epithelium detachment (PED).3 Despite being usually self-resolving, CSC sometimes evolves into a chronic, persistent form often accompanied by retinal pigment epithelium (RPE) and photoreceptors changes. Treatments of CSC include observation, discontinuation of drug at risk, laser photocoagulation, micropulse laser, rifampin, photodynamic therapy (PDT), anti-vascular endothelial growth factor (VEGF) and mineralocorticoid receptor (MR) antagonists (ie spironolactone, eplerenone).3
Multimodal imaging is extremely useful in the initial evaluation and follow-up of CSC after treatment. Beyond structural optical coherence tomography (OCT), several imaging modalities are routinely used in clinical practice of CSC, including fundus autofluorescence (FAF), fluorescein angiography (FA) and indocyanine green angiography (ICGA). Optical coherence tomography angiography (OCT-A) is a novel technology that allows the visualization of retinal and choroidal vessel vasculature in a rapid, non-invasive and dye-less fashion.4 Previous studies have shown that OCT-A is able to highlight qualitative defects and textural changes in affected eyes or to identify choroidal neovascularization (CNV) complicating CSC.5, 6, 7, 8 Using en face OCT, Kuroda et al9 found increased choroidal vascular area in patients with CSC. No study evaluating quantitative changes in retinal and choroidal vasculature using OCT-A has been published yet. Moreover, correlation between novel OCT-A measures and well-known clinical and OCT features is still undetermined. Finally, effects of different therapies on OCT and OCT-A measures have not been elucidated.
The aims of our work were to (i) correlate functional and structural parameters to OCT-A measures in patients affected by CSC; (ii) describe changes in clinical, structural OCT and OCT-A measures after therapy using two different treatments (ie eplerenone, PDT).
Methods
Study population
Consecutive patients affected by CSC undergoing either eplerenone or PDT between January 2016 and June 2016 at the Medical Retina & Imaging Unit of the Department of Ophthalmology, University Vita-Salute, San Raffaele Hospital, Milan, Italy were enrolled in this non-randomized prospective study. The study was conducted in compliance with the Declaration of Helsinki and all patients signed a written general consent to participate in clinical studies, which was approved by the ethics committee of San Raffaele Hospital.
Inclusion criteria were: diagnosis of CSC with no spontaneous regression for at least 2 months; age ≥18 years old; refractive status between −6 and +6 diopters, no previous ocular surgery other than uncomplicated cataract extraction and intraocular lens implantation, no previous CSC therapy. Diagnosis of CSC was established on the basis of the following criteria: (i) SRF and/or PED within the macular area; (ii) idiopathic leakage from the RPE during FA/ICGA; (iii) exclusion of other possible causes of SRF/PED. CSC was further classified in acute or chronic whether its onset was ≤12 or >12 weeks, respectively. Exclusion criteria were: presence of CNV; any other retinal disease; significant media opacity to ensure proper images quality; presence of systemic contraindication for eplerenone treatment (liver or renal disease, hyperkalemia, defined as >5.5 mmol/l, or concomitant drugs that increase the potassium level, pregnancy).
Enrolled patients were evaluated at baseline and after therapy at months 1 and 3. The ophthalmologic examination included best-corrected visual acuity (BCVA) on Snellen charts, anterior segment biomicroscopy, intraocular pressure (IOP) measured with Goldmann applanation tonometry, indirect fundus exam, structural spectral-domain (SD)-OCT (Spectralis, HRA Heidelberg, Heidelberg, Germany) and 3 × 3 mm OCT-A (Angioplex, CIRRUS HD-OCT models 5000, Carl Zeiss Meditec, Inc., Dublin, OH, USA) scans of the macula. The minimum strength of OCT-A images was 7 out of 10. BCVA was converted to the logarithm of the minimal angle of resolution (logMAR) for calculation purposes. Medical history and demographic data were also recorded.
Treatment regimen
Eplerenone (Inspra, Pfizer, Paris, France) was administrated orally 25 mg/day for a week followed by 50 mg/day for 4 weeks. The 50 mg/day eplerenone treatment was continued for other 8 weeks depending on the presence of SRF at SD-OCT scans. Treatment tolerance was assessed by blood analyses of kalemia and creatinine performed at baseline and every 4 weeks. The treatment was stopped in case of kalemia increase (>5 mmol/l) or creatinine clearance rate decrease (<60 ml/min).
Verteporfin (6 mg/m2) PDT (Visudyne; Novartis Pharma, New York, NY, USA) with a half-fluence rate (25 J/cm) by one single experienced physician (GQ), as described elsewhere.10 Briefly, verteporfirin was infused for 10 min and 15 min after the start of the infusion, a laser light at 689 nm was delivered at 25 J/cm, with an intensity of 300 mW/cm for 83 s.
Structural SD-OCT measurements
The structural SD-OCT acquisition protocol included: 19 horizontal raster linear B-scans, each composed by 9 averaged OCT B-scans (1024A-scans per line) at 240 μm intervals, covering an area of 20 degrees by 15 degrees; 6 radial linear B-scans, each composed by 25 averaged OCT B-scans (768A-scans per line) at 30 degrees centered on the fovea; 49 horizontal raster dense linear B-scans, each composed by 16 averaged OCT B-scans (384A-scans per line) at 30 μm intervals, covering an area of 15 degrees by 5 degrees. The latter two scan sequences were acquired in enhanced depth imaging (EDI) mode. All acquisition following baseline visit were acquired using the follow-up function. Central macular thickness (CMT) in the central 1-mm-diameter circle of the ETDRS thickness map was recorded with the Spectralis Software (Heidelberg Eye Explorer, Version 1.9.11.0, Heidelberg Engineering, Heidelberg, Germany). SRF, subfoveal choroidal thickness (SFCT) and PED height were manually measured by an independent operator (DM). SRF was defined as the vertical distance between the end of the outer segment and the RPE at the foveal center. SFCT measured vertically from the outer border of the RPE to the inner border of the sclera. PED height was calculated as the distance between the RPE at the base and the peak of the PED.
OCT-A images acquisition and analysis
OCT-A images were acquired with the Cirrus HD-OCT (Angioplex, CIRRUS HD-OCT models 5000, Carl Zeiss Meditec, Inc., Dublin, OH, USA). Automatic segmentation of full-thickness (internal limiting membrane to Bruch’s membrane) retina vasculatures, superficial (SCP) and deep (DCP) capillary plexuses was evaluated by a single operator (AR) and manually adjusted in case of segmentation errors. All 3 × 3 OCT-A images were exported into the National Institutes of Health ImageJ 1.50 (National Institutes of Health, Bethesda, MD, USA) software and analyzed by a second independent operator (AR).
The FAZ area was manually measured using a previously published method.11, 12 Briefly, the FAZ area was manually outlined using the polygon selection tool in all the three selected plexuses (full-thickness, superficial, SCP and DCP), and its dimension expressed as squared millimeters was calculated. The FAZ area was evaluated in full-thickness (internal limiting membrane to Bruch’s membrane) OCT-A angiogram (ftFAZ), SCP (sFAZ) and DCP (dFAZ).
Vessel density was calculated through image thresholding and binarization, according to previous studies.13, 14 Specifically, (i) the ImageJ mean threshold, which automatically calculates the threshold as the mean of the local greyscale distribution, was applied to each image; (ii) binarized 8-bit image was converted to RGB color model; (iii) FAZ area was contoured and colored to pure blue. White pixels were considered as vessel, black pixels as background, and blue pixels were automatically excluded from the analysis in order to prevent FAZ inclusion in vessel density calculation. Vessel density was calculated as the ratio between the white pixel and the total pixels after FAZ exclusion.
Statistical analysis
Variables included in the analysis were: age, sex, race, eye (right/left), BCVA, CMT, SRF, presence and height of PED, SFCT, FAZ area in the full-thickness, SCP and DCP; vessel density in full-thickness, SCP, DCP, choriocapillaris and Sattler+Haller layers. Differences between groups were calculated by means of student’s t-test for continuous variables and χ2 or Fisher exact test for categorical variables. Variables change during the follow-up period was assessed with analysis of variance (ANOVA) for repeated measures and Tukey test was used as post-hoc test. The relationship between variables was explored using Pearson correlation test and multiple correlations were adjusted by means of Benjamini–Hochberg test. All data were expressed as the mean±standard deviation and all tests were two-sided. A P-value less than 0.05, after adjustment when required, was considered to be significant. Prism 6.0 software (GraphPad Software, San Diego, CA, USA) was used to analyze the data.
Results
Baseline data and pre-treatment correlation analysis
Twenty eyes of 16 patients were enrolled. Eleven active eyes of nine patients and nine eyes of seven patients underwent to eplerenone or PDT treatment, respectively. No significant difference was appreciated between the two groups for clinical, OCT and OCT-A measures at the baseline visit (Table 1).
At correlation analysis, BCVA was not related to any of structural OCT variables, including CMT (P=0.3), SRF (P=0.4) and SFCT (P=0.9). No significant correlation was seen also between BCVA and OCT-A measures, including FAZ area and vessel density at every plexus.
Among OCT-parameters a robust association between CMT and SRF was disclosed (r=0.90, P<0.01); whereas no relationship was found between SFCT and CMT (P=0.3) or SRF (P=0.5). Both CMT and SRF strongly correlated to FAZ area (r=0.74 and r=0.71, P=0.01 and P=0.01, respectively) and vessel density (r=0.77 and r=0.68, P=0.01 and P=0.01, respectively) at DCP. Neither CMT or SRF significantly correlated to any other OCT-A-derived parameters, including arFAZ (P=0.1 and P=0.3, respectively) and sFAZ (P=0.2 and P=0.3, respectively) areas, vessel density at full thickness retina (P=0.2 and P=0.2, respectively), SCP (P=0.13 and P=0.08, respectively), choriocapillaris (P=0.8 and P=0.3, respectively) and Sattler–Haller (P=0.7 and P=0.8, respectively) vascular layers.
SFCT was negatively correlated to patient age (r=−0.59, P=0.048). SFCT was not significantly correlated to any other OCT-A variables (P>0.05).
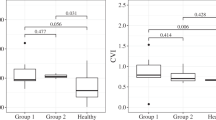
Clinical, structural OCT and OCT-A changes after treatment
Enrolled patients were evaluated at 36±5 and 103±25 days after treatment (eplerenone or PDT). BCVA improved from 20/32 (0.20 logMAR) at baseline to 20/29.5 (0.17 logMAR) at 1 month and 20/28 (0.15 logMAR) at 3 months, although this difference was not statistically significant (P=0.2). BCVA improvement was more pronounced in patients who underwent eplerenone than PDT therapy, even if neither eplerenone (P=0.12) or PDT (P=0.9) group reached a significant change in BCVA from baseline. Moreover, no difference between eplerenone and PDT (P=0.18) was appreciated at 3 months regarding BCVA. Figure 1a shows BCVA changes after treatments.
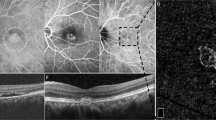
Functional and structural variables at baseline and at 1- and 3-month visit after treatment (ie overall, eplerenone, photodynamic therapy (PDT)). (a) Best corrected visual acuity (BCVA), (b) central macular thickness (CMT), (c) subretinal fluid (SRF), (d) subfoveal choroidal thickness (SFCT). LogMAR indicates the logarithm of the minimal angle of resolution.
CMT significantly decreased from 404.6±120.3 μ at baseline to 337.1±97.9 μ and 286.8±76.6 μ at 1 and 3 months, respectively (P=0.0011). CMT reduction from baseline was significant at both 1 (P=0.049) and 3 (P=0.0037) months; a significant difference was appreciated also between 1- and 3-month visit (P=0.0203). A significant CMT reduction from baseline was appreciated in the eplerenone (P=0.0022) but not in the PDT (P=0.18) group, although no difference between the two groups was found at 3 months (P=0.5). In the eplerenone group, CMT significantly decreased both at 1 (P=0.033) and 3 (P=0.0079) months; conversely no difference between 1- and 3-month visits was disclosed (P=0.09). Figure 1b shows CMT changes after treatments.
Similarly, SRF decreased from 155.3±113.0 μ at baseline to 87.5±75.5 μ and 34.6±57.4 μ at 1 and 3 months, respectively (P=0.0005). SRF reduction from baseline was significant at 1 (P=0.0379) and 3 (P=0.0018) months and also between those two follow-up visits (P=0.01). A significant reduction in SRF was disclosed in eplerenone (P=0.0015) but not in PDT (P=0.14) group, although no difference between the two groups was found at 3 months (P=0.7). In the eplerenone group, SRF reduction from baseline was significant at both 1 (P=0.0239) and 3 (P=0.0058) months and also between the two follow-up visits (P=0.0239). Figure 1c shows SRF changes after treatments.
PED completely resolved in only one eye after treatment and PED mean height did not significantly improve during the follow-up period (P=0.6). The case of PED resolution occurred in the eplerenone group.
SCFT significantly decreased from 426.6±82.2 μ at baseline to 398.1±66.9 μ and 359.4±72.6 μ at 1 and 3 months, respectively (P=0.0016). SFCT at 3-month visit was significantly lower than at both baseline (P=0.0053) and 1-month (P=0.0007) visits, whereas SCFT at 1 month did not differ from baseline (P=0.4). Significant reduction of SFCT was appreciated in both eplerenone (P=0.0212) and PDT (P=0.0267) groups; however, magnitude of reduction at 3 months was significantly higher in PDT than eplerenone group (P=0.0347). Figure 1d shows SRF changes after treatments.
Regarding full thickness retina vasculature, no significant change in FAZ area and vessel density was found overall (P=0.5 and P =0.7, respectively), in the eplerenone (P=0.3 and P=0.9, respectively) or in the PDT (P=0.4 and P=0.9, respectively) group, as shown in Figures 2a and b.
Optical coherence tomography angiography-derived measures at baseline and at 1- and 3-month visit after treatment (ie overall, eplerenone, photodynamic therapy (PDT)). Full-thickness retina foveal avascular zone (FAZ) area (a) and vessel density (b); superficial capillary plexus (SCP) FAZ area (c) and vessel density (d), deep capillary plexus (DCP) FAZ area (e) and vessel density (f); choriocapillaris (CC) (g) and Sattler+Haller (h) vessel densities.
No significant difference was disclosed in SCP for FAZ area and vessel density overall, in eplerenone or in PDT group, as shown in Figures 2c and d.
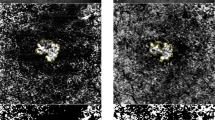
With regards to DCP, dFAZ area (Figure 2e) significantly decreased from 1.966±1.76 mm2 at baseline to 1.25±1.03 mm2 and 0.88±0.55 mm2 at 1 and 3 months, respectively (P=0.0334). A significant reduction of dFAZ area was appreciated in eplerenone (P=0.0204) but not in PDT (P=0.5) group. DCP vessel density reduction following treatment disclosed a nearly significant trend (P=0.058), as shown in Figure 2f. Interestingly, vessel density significantly changed after eplerenone (P=0.0397) but not PDT (P=0.4) treatments. Figure 3 shows changes in structural OCT and DCP at OCT-A after oral eplerenone and PDT.
Structural optical coherence tomography (OCT) and optical coherence tomography angiography (OCT-A) at deep capillary plexus (DCP) at baseline and at 3-month visit after oral eplerenone (a,b) and photodynamic therapy (PDT) (c,d). Structural OCT (a) revealing serous neuroretinal detachment, intraretinal hyperreflective dots, atrophy of outer retinal layers, thicken subfoveal choroid and dilated choroidal vessels prior to eplerenone treatment. OCT-A at DCP (b) after binarization (c) discloses increased foveal avascular zone (FAZ) area (depicted in blue) and higher vessel density. At 3-month visit after eplerenone, structural OCT (d) shows a marked reduction of subretinal fluid; OCT-A (e) after image binarization (f) reveals recovery in FAZ area and vessel density at DCP. Structural OCT (g) revealing serous neuroretinal detachment, intraretinal hyperreflective dots, thicken subfoveal choroid and dilated choroidal vessels prior to PDT. OCT-A at DCP (h) after binarization (i) discloses moderate increase in foveal avascular zone (FAZ) area (depicted in blue) and vessel density. At 3-month visit after PDT, structural OCT (j) shows a resolution of subretinal fluid; OCT-A (k) after image binarization (l) mild improvement in FAZ area and vessel density.
Vessel density in both choriocapillaris (Figure 2g) and Sattler+Haller (Figure 2h) vascular layers did not exhibit any significant modification after treatment (P=0.3 and P=0.5, respectively), even when considering the eplerenone (P=0.6 and P=0.3, respectively) and the PDT (P=0.4 and P=0.6, respectively) groups separately. Figure 4 shows structural OCT and CC at OCT-A changes after eplerenone or PDT treatments.
Structural optical coherence tomography (OCT) and optical coherence tomography angiography (OCT-A) at choriocapillaris (CC) at baseline and at 3-month visit after oral eplerenone (a,b) and photodynamic therapy (PDT) (c,d). Both oral eplerenone and PDT cause a reduction or marked reduction of subretinal fluid at 3-month visit detected by means of structural OCT, respectively. No difference in CC vessel density after image binarization is disclosed between baseline and 3-month visit in both groups.
Discussion
In the present study, we investigated the relationship between clinical (ie BCVA), structural OCT (ie CMT, SRF, SFCT) and vascular OCT-A (ie FAZ area, vessel density) data in patients affected by treatment naïve CSC. In this cohort of patients, a positive correlation has been found between structural, namely CMT and SRF, and vascular variables, namely FAZ area and vessel density at DCP. In addition, changes in such measures have been prospectively evaluated over a 3-month period following two different treatment modalities: oral eplerenone and PDT. Most of the structural parameters (ie CMT, SRF, SFCT) as well as vascular parameters (ie dFAZ) significantly improved after treatment. Although structural OCT is the primary test in most macular diseases, diagnosis and follow-up of CSC are based on a multimodal approach. Structural OCT reveals several features of acute (ie SRF, CMT, PED) and chronic (ie photoreceptor elongation, RPE hypertrophy or atrophy, outer nuclear layer thinning, disruption of the ellipsoid zone (EZ) or external limiting membrane (ELM), cystoid macular degeneration) disease. EDI-OCT identified thicker choroid in both affected and unaffected eyes.15, 16 FAF may provide useful information about the status of RPE, especially in chronic disease.17 FA is useful in order to individuate origin of leakage at baseline3; whereas ICGA allows to identify choroidal vascular changes (ie delayed filling, congestion, hyperpermeability, punctate hyperfluorescent spots) and to exclude the presence of CNV.18, 19, 20, 21
Structural OCT and OCT-A assessment of eyes with CSC could provide information about the anatomical status of the retinal and choroidal structure and vessels, which can result altered even after therapy and episode resolution. Although the choroid plays a major pathogenic role, neuroretina may be subjected to several pathological changes in chronic as well acute CSC, which could cause secondary alterations in retinal vasculature.3 An impairment in retinal vein dilation in response to flicker light has been recently described in eyes with active CSC and this could reflect either a primary dysregulation linked to autonomic imbalance or a secondary phenomenon caused by SRF accumulation.22
Thus, we designed a prospective study in order to quantitatively investigate the structural and vascular status of eyes affected by CSC using respectively structural OCT and OCT-A at baseline and their modifications following two different treatments (ie eplerenone, PDT). Even though some qualitative abnormalities have been previously described on OCT-A, such as textural changes or presence of CNV complicating CSC, no quantitative assessment was attempted.5, 6, 7, 8 Moreover, no study has characterized the quantitative OCT-A modifications following treatment in the retina as well in the choroid vasculatures. To obtain quantitative data, OCT-A angiograms were post-processed and two indices, namely FAZ area and vessel density, were calculated. In correspondence to the foveola, the superficial and deep plexuses interrupt to form a capillary-free zone called FAZ.23 Macular vessel density reflects the percentage of vessels covering the macular area in the retina as well in the underlying choroidal layers. Both indices are stable and reliable parameters commonly adopted in quantitative analysis of OCTA, and they reflect the vascular status of the macular area.24, 25, 26
In accordance with previous studies,27 we did not observe any correlation between BCVA and CMT, SRF or SFCT. In addition, our data indicate that none of OCT-A measure is significantly associated with BCVA. A strong positive correlation among CMT, SRF and vessel analysis at DCP (ie FAZ area, vessel density) was observed. We hypothesize that such correlation can be explained by the mechanic effect exerted by the fluid beneath the neuroretina, causing a centrifugal displacement and squeezing of retinal vessels, which could, in turn, generate enlargement of FAZ and increasing of vessel density.
Several treatment strategies have been proposed in CSC including observation, discontinuation of drug at risk, laser photocoagulation, micropulse laser, PDT, anti-VEGF agents and MR antagonists (ie spironolactone, eplerenone). However, evidence for those treatment strategies is low and current literature does not provide enough information about the best approach with regard to safety and efficacy in CSC.28 Among interventional modalities, PDT is the preferred practice pattern of retina specialist.29 Therapeutic effect of PDT is accomplished through the production of oxygen-free radical in choroidal vasculature with subsequent vascular obliteration. PDT improves choroidal morphology and functionality leading to a reduction in choroidal congestion, vascular hyperpermeability, and extravascular leakage.30 However, several sight-threatening adverse events following PDT have been reported, including RPE tear, sub-RPE hemorrhage, RPE atrophy, and choriocapillaris nonperfusion.31, 32 In order to avoid side effects of standard PDT, other regimens have been applied including half-dose or lower-fluence PDT. According to a recent meta-analysis, those regimens seem to be as effective as standard PDT.33
In a recent study, Zhao et al34 demonstrated that choroidal vascular dilation and leakage induced by high-dose glucocorticoid or aldosterone was reverted by MR antagonists. Following this observation, oral MR antagonists have been applied in CSC treatment. Of the two commercially available oral MR antagonist, eplerenone is usually preferred to spironolactone for the highest specificity toward MR and, thus, less anti-androgen (ie gynecomastia, feminization, loss of libido, erectile dysfunction) and metabolic (hyperglycemia, hypercortisolism) side effects.35
In our study, both half-fluence PDT and eplerenone had similar outcomes. BCVA did not change significantly after treatments, although a trend toward improvement was observed, especially in the eplerenone group. Lack of statistically significant change in BCVA could be related to several factors, including (i) small sample size, (ii) high BCVA at baseline, (iii) high percentage of long-standing CSC which is often accompanied by photoreceptor injury. CMT and SRF were strongly correlated at baseline, and significantly improved after treatment. Interestingly, CMT and SRF changes were significant in the eplerenone group, while a trend toward reduction was observed also in the PDT group. With regards to retinal vascular indices, reduction of FAZ area and vessel density in DCP was appreciated, and this difference was driven by the eplerenone group. We speculate that normalization of OCT-A measures in DCP could be linked to SRF decrease and, thus, related to the reduction of mechanical vascular displacement exerted by the fluid. SRF reduction was more pronounced in eplerenone than PDT group and this finding may explain why modifications in DCP were more pronounced in eplerenone group. Given that PED, which can exert a displacement of retinal vessels, actually did not improve after therapy, the higher number of PED in PDT group could at least in part explain the differences between those two groups at OCT-A. Since eplerenone, differently from PDT that acts locally, is a systemic treatment, it is possible to hypothesize a global circulatory improvement seen at DCP.
On the other hand, OCT-A did not disclose any vascular modifications of FAZ area and vessel density at SCP. This might be explained by the fact that CSC is a disease characterized by the involvement of the choroid and outer retina, while inner retinal layers are generally preserved.
Choroidal thickening has been extensively described in affected and fellow eyes of CSC patients due to choriocapillaris hyperpermeability and dilation of large vessels in Haller layer.36, 37 In the present study, we have investigated the choroid using both structural OCT (ie SFCT) and OCT-A (ie vessel density in choriocapillaris and in Sattler+Haller layer). In accordance with previous studies,38, 39 our results indicate that SFCT significantly improved after treatment overall and in both subgroups. Notably, we observed a reduction in SFCT significantly greater in eyes treated with PDT than eplerenone. A recent study by Kinoshita et al40 showed that reduction in SFCT following half-dose PDT may be ascribed both to a decrease of exudation from choriocapillaris in the inner choroidal stroma and a reduction of vessel dilation in Haller layer. The reduction of SFCT exerted by both treatments could be due to a reduction in choroidal hyperpermeability and, thus, in stromal exudation. Another interesting finding of our work is that no significant change in choriocapillaris and Sattler+Haller layers has been found using OCT-A. Histopathological studies have shown that standard PDT induces selective damage and obliteration of choriocapillaris.41 Interestingly, we did not find any change in both choriocapillaris and Sattler+Haller layers following either eplerenone or half-fluence PDT. This observation suggests that half-fluence PDT, opposite to standard PDT, exerts its action without significantly damaging choroidal vascular structure similarly to other less invasive therapeutic strategies (ie eplerenone).
The main limitation of our study relies on the small sample size and, thus, some correlation and differences during the follow-up could have been therefore missed. Furthermore, our study provides a relatively short follow-up period and long-term modifications could occur. Finally, visualization of the choroid, especially in the case of thickening (as in CSC), could have been improved using a swept source instead of spectral domain OCT and OCT-A. Despite the above limitations, our study has got several strengths including its prospective design and the quantitative assessment of OCT and OCT-A images.
Several conclusions can be drawn from the present study. A correlation between structural (ie CMT, SRF) and vascular (ie FAZ area and vessel density at DCP at OCT-A) parameters exists and all those parameters significantly improve after different treatments. SFCT decreases with both treatments, although the change is more pronounced following half-fluence PDT. A significant reduction of dFAZ area was appreciated in eplerenone but not in PDT group, possibly related to the systemic effects of MR antagonists. Finally, both half-fluence PDT and oral eplerenone do not permanently damage choriocapillaris or other choroidal layers as evaluated by OCT-A.

References
Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burke JP . The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980–2002. Ophthalmology 2008; 115 (1): 169–173.
Wang M, Munch IC, Hasler PW, Prunte C, Larsen M . Central serous chorioretinopathy. Acta Ophthalmol 2008; 86 (2): 126–145.
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res 2015; 48: 82–118.
Rabiolo A, Carnevali A, Bandello F, Querques G . Optical coherence tomography angiography: evolution or revolution? Exp Rev Ophthalmol 2016; 11 (4): 243–245.
Bonini Filho MA, de Carlo TE, Ferrara D, Adhi M, Baumal CR, Witkin AJ et al. Association of choroidal neovascularization and central serous chorioretinopathy with optical coherence tomography angiography. JAMA Ophthalmol 2015; 133 (8): 899–906.
Costanzo E, Cohen SY, Miere A, Querques G, Capuano V, Semoun O et al. Optical coherence tomography angiography in central serous chorioretinopathy. J Ophthalmol 2015; 2015: 134783.
Quaranta-El Maftouhi M, El Maftouhi A, Eandi CM . Chronic central serous chorioretinopathy imaged by optical coherence tomographic angiography. Am J Ophthalmol 2015; 160 (3): 581–587 e581.
Teussink MM, Breukink MB, van Grinsven MJ, Hoyng CB, Klevering BJ, Boon CJ et al. OCT angiography compared to fluorescein and indocyanine green angiography in chronic central serous chorioretinopathy. Invest Ophthalmol Vis Sci 2015; 56 (9): 5229–5237.
Kuroda Y, Ooto S, Yamashiro K, Oishi A, Nakanishi H, Tamura H et al. Increased choroidal vascularity in central serous chorioretinopathy quantified using swept-source optical coherence tomography. Am J Ophthalmol 2016; 169: 199–207.
Casalino G, Del Turco C, Corvi F, Rafaeli O, Bandello F, Querques G . Short-term retinal sensitivity and metamorphopsia changes following half-fluence photodynamic therapy in central serous chorioretinopathy. Ophthalmic Res 2016; 56 (1): 23–29.
Samara WA, Say EA, Khoo CT, Higgins TP, Magrath G, Ferenczy S et al. Correlation of foveal avascular zone size with foveal morphology in normal eyes using optical coherence tomography angiography. Retina 2015; 35 (11): 2188–2195.
Shahlaee A, Pefkianaki M, Hsu J, Ho AC . Measurement of foveal avascular zone dimensions and its reliability in healthy eyes using optical coherence tomography angiography. Am J Ophthalmol 2016; 161: 50–55 e51.
Battaglia Parodi M, Cicinelli MV, Rabiolo A, Pierro L, Bolognesi G, Bandello F . Vascular abnormalities in patients with Stargardt disease assessed with optical coherence tomography angiography. Br J Ophthalmol 2016; 101 (6): 780–785.
Chidambara L, Gadde SG, Yadav NK, Jayadev C, Bhanushali D, Appaji AM et al. Characteristics and quantification of vascular changes in macular telangiectasia type 2 on optical coherence tomography angiography. Br J Ophthalmol 2016; 100 (11): 1482–1488.
Goktas A . Correlation of subretinal fluid volume with choroidal thickness and macular volume in acute central serous chorioretinopathy. Eye (Lond) 2014; 28 (12): 1431–1436.
Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T . Subfoveal choroidal thickness in fellow eyes of patients with central serous chorioretinopathy. Retina 2011; 31 (8): 1603–1608.
Lee WJ, Lee JH, Lee BR . Fundus autofluorescence imaging patterns in central serous chorioretinopathy according to chronicity. Eye (Lond) 2016; 30 (10): 1336–1342.
Hayashi K, Hasegawa Y, Tokoro T . Indocyanine green angiography of central serous chorioretinopathy. Int Ophthalmol 1986; 9 (1): 37–41.
Menchini U, Virgili G, Lanzetta P, Ferrari E . Indocyanine green angiography in central serous chorioretinopathy. ICG angiography in CSC. Int Ophthalmol 1997; 21 (2): 57–69.
Tsujikawa A, Ojima Y, Yamashiro K, Ooto S, Tamura H, Nakagawa S et al. Punctate hyperfluorescent spots associated with central serous chorioretinopathy as seen on indocyanine green angiography. Retina 2010; 30 (5): 801–809.
Yannuzzi LA . Indocyanine green angiography: a perspective on use in the clinical setting. Am J Ophthalmol 2011; 151 (5): 745–751 e741.
Tomasso L, Benatti L, Rabiolo A, Carnevali A, Zucchiatti I, Querques L et al. Retinal vessels functionality in eyes with central serous chorioretinopathy. Br J Ophthalmol 2017; e-pub ahead of print 9 June 2017; doi: 10.1136/bjophthalmol-2017-310398.
Cicinelli MV, Carnevali A, Rabiolo A, Querques L, Zucchiatti I, Scorcia V et al. Clinical spectrum of macular-foveal capillaries evaluated with optical coherence tomography angiography. Retina 2017; 37 (3): 436–443.
La Spina C, Carnevali A, Marchese A, Querques G, Bandello F . Reproducibility and reliability of optical coherence tomography angiography for foveal avascular zone evaluation and measurement in different settings. Retina 2016; 37 (9): 1636–1641.
Yanik Odabas O, Demirel S, Ozmert E, Batioglu F . Repeatability of automated vessel density and superficial and deep foveal avascular zone area measurements using optical coherence tomography angiography: diurnal findings. Retina 2017; e-pub ahead of print 2 May 2017; doi: 10.1097/IAE.0000000000001671.
Venugopal JP, Rao HL, Weinreb RN, Pradhan ZS, Dasari S, Riyazuddin M et al. Repeatability of vessel density measurements of optical coherence tomography angiography in normal and glaucoma eyes. Br J Ophthalmol 2017; e-pub ahead of print 24 July 2017; doi: 10.1136/bjophthalmol-2017-310637.
Yalcinbayir O, Gelisken O, Akova-Budak B, Ozkaya G, Gorkem Cevik S, Yucel AA . Correlation of spectral domain optical coherence tomography findings and visual acuity in central serous chorioretinopathy. Retina 2014; 34 (4): 705–712.
Salehi M, Wenick AS, Law H, Evans JR, Gehlbach P . Interventions for central serous chorioretinopathy: a network meta-analysis. Cochrane Database Syst Rev 2015; (12): CD011841.
Mehta PH, Meyerle C, Sivaprasad S, Boon C, Chhablani J . Preferred practice pattern in central serous chorioretinopathy. Br J Ophthalmol 2016; 101 (5): 587–590.
Chan WM, Lam DS, Lai TY, Tam BS, Liu DT, Chan CK . Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol 2003; 87 (12): 1453–1458.
Lim JI, Glassman AR, Aiello LP, Chakravarthy U, Flaxel CJ, Spaide RF et al. Collaborative retrospective macula society study of photodynamic therapy for chronic central serous chorioretinopathy. Ophthalmology 2014; 121 (5): 1073–1078.
Reibaldi M, Cardascia N, Longo A, Furino C, Avitabile T, Faro S et al. Standard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trial. Am J Ophthalmol 2010; 149 (2): 307–315 e302.
Ma J, Meng N, Xu X, Zhou F, Qu Y . System review and meta-analysis on photodynamic therapy in central serous chorioretinopathy. Acta Ophthalmol 2014; 92 (8): e594–e601.
Zhao M, Celerier I, Bousquet E, Jeanny JC, Jonet L, Savoldelli M et al. Mineralocorticoid receptor is involved in rat and human ocular chorioretinopathy. J Clin Invest 2012; 122 (7): 2672–2679.
Delyani JA . Mineralocorticoid receptor antagonists: the evolution of utility and pharmacology. Kidney Int 2000; 57 (4): 1408–1411.
Chung YR, Kim JW, Kim SW, Lee K . Choroidal thickness in patients with central serous chorioretinopathy: assessment of Haller and Sattler layers. Retina 2016; 36 (9): 1652–1657.
Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF . Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology 2010; 117 (9): 1792–1799.
Gergely R, Kovacs I, Schneider M, Resch M, Papp A, Recsan Z et al. Mineralocorticoid receptor antagonist treatment in bilateral chronic central serous chorioretinopathy: a comparative study of exudative and nonexudative fellow eyes. Retina 2016; 37 (6): 1084–1091.
Oh BL, Yu HG . Choroidal thickness after full-fluence and half-fluence photodynamic therapy in chronic central serous chorioretinopathy. Retina 2015; 35 (8): 1555–1560.
Kinoshita T, Mitamura Y, Mori T, Akaiwa K, Semba K, Egawa M et al. Changes in choroidal structures in eyes with chronic central serous chorioretinopathy after half-dose photodynamic therapy. PLoS One 2016; 11 (9): e0163104.
Schmidt-Erfurth U, Laqua H, Schlotzer-Schrehard U, Viestenz A, Naumann GO . Histopathological changes following photodynamic therapy in human eyes. Arch Ophthalmol 2002; 120 (6): 835–844.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rabiolo, A., Zucchiatti, I., Marchese, A. et al. Multimodal retinal imaging in central serous chorioretinopathy treated with oral eplerenone or photodynamic therapy. Eye 32, 55–66 (2018). https://doi.org/10.1038/eye.2017.290
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.290
This article is cited by
-
Evaluation of the choriocapillaris after photodynamic therapy for chronic central serous chorioretinopathy. A review of optical coherence tomography angiography (OCT-A) studies
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Efficacy of mineralocorticoid receptor antagonist for central serous chorioretinopathy: a meta-analysis
International Ophthalmology (2020)
-
Vascular and structural alterations of the choroid evaluated by optical coherence tomography angiography and optical coherence tomography after half-fluence photodynamic therapy in chronic central serous chorioretinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
Eplerenone Versus Observation in the Treatment of Acute Central Serous Chorioretinopathy: A Retrospective Controlled Study
Ophthalmology and Therapy (2018)