Abstract
Purpose
To investigate the association of the severity of obstructive sleep apnea syndrome (OSAS) with peripapillary retinal nerve fiber layer (RNFL) and macular ganglion cell-inner plexiform layer (GC-IPL).
Materials and methods
In this cross-sectional study, 145 patients with OSAS and 40 healthy subjects were enrolled. OSAS patients were further divided into mild (n=50), moderate (n=36), and severe (n=59) OSAS groups according to their apnea–hypopnea index (AHI) values. Spectral-domain optical coherence tomography was used to measure the peripapillary RNFL and GC-IPL thicknesses.
Results
There was no statistical difference between the RNFL thickness in OSAS and control groups (P>0.05). Both average GC-IPL and minimum GC-IPL thicknesses were significantly lower in severe OSAS group than in healthy controls (P<0.05 for both). There was a significant negative correlation between AHI and both average GC-IPL (r=−0.232, P=0.005) and minimum GC-IPL (r=−0.233, P=0.005) thicknesses.
Conclusions
Our study results suggest that although RNFL thickness did not differ significantly between OSAS and control groups, ganglion cell layer thickness in OSAS patients is much lower than in healthy population. Ganglion cell thickness showed a significant correlation with the severity of OSAS.
Similar content being viewed by others
Introduction
Obstructive sleep apnea syndrome (OSAS) is defined as repetitive complete or partial obstruction of upper airway during sleep that results in reduction in oxygen saturation and intermittent hypoxia. This, in turn, induces oxidative stress, inflammation, and endothelial dysfunction, and consequently leads to impaired vascular autoregulation. OSAS has been associated with numerous ophthalmic disorders, including floppy eyelid syndrome, non-arteritic anterior ischemic optic neuropathy, glaucoma, papilledema, central serous choroido-retinopathy, and retinal vein occlusion.1, 2, 3, 4, 5, 6, 7, 8
Glaucoma is the most investigated ocular conditions in patients with OSAS. Although numerous previous studies have reported high glaucoma prevalence in patients with OSAS, only few investigators have indicated any association between OSAS and glaucoma.5, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Additionally, it has been suggested that OSAS may also influence the retina nerve fiber layer (RNFL) and macular ganglion cell complex (GCC).9, 14, 15, 19
Nowadays optical coherence tomography (OCT) is commonly used for qualitative and quantitative assessment of retina. Structural alterations in peripapillary RNFL and macular GCC thickness are often detected with OCT. Although several studies have investigated the impact on RNFL thickness in patients with OSAS, there is limited information regarding the effect of OSAS on GCC thickness. The aim of our study is to evaluate the association of the severity of OSAS with peripapillary RNFL and macular ganglion cell-inner plexiform layer (GC-IPL)
Materials and methods
Study population and design
This prospective comparative study was performed in the Department of Ophthalmology, Kanuni Sultan Suleyman Education and Research Hospital and Chest Diseases and Sleep Center, Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and Research Hospital, Istanbul, Turkey. The study followed the tenets of the Declaration of Helsinki and was approved by the local ethics committee. All participants received oral and written study-related information, and each participant provided written informed consent.
Eligibility criteria
Both study and control groups were recruited in Chest Diseases and Sleep Center, Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and Research Hospital. Patients presenting to the sleep center with complaints of snoring, witnessed apnea, and excessive daytime sleepiness underwent polysomnographic investigation. Obstructive sleep apnea syndrome was diagnosed and graded according to the following apnea–hypopnea index (AHI) values: mild (>5 to ≤15), moderate (>15 to <30), and severe (≥30). Newly diagnosed, treatment-naïve OSAS patients were enrolled in this study. Control subjects had an AHI value <5 and were age and sex matched with the OSAS group participants. The subjects who had a myopia or hyperopia (>+3 or −3 D of spherical equivalent), glaucoma, intraocular pressure >21 mm Hg, posterior pole pathology such as macular degeneration or diabetic retinopathy, a history of intraocular surgery, ocular trauma, uveitis, and poor image due to cataract or unstable fixation were excluded.
Sleep study (polysomnography)
A standard overnight polysomnography was performed at the Chest Diseases and Sleep Center, Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and Research Hospital. All patients underwent an overnight polysomnography in a quiet room, which included the following variables: electroencephalography, submental electromyography, electro-oculography, airflow (nasal and oral) by thermistors, and pulse oximetry measurements. The AHI (times/h) was calculated by calculating the average number of episodes of apnea plus hypopnea per hour of sleep or recording time. An apneic event was defined as the cessation of airflow for at least 10 s with an effort to breathe. A hypoapneic event was described as a minimum of 30% fall in airflow for at least 10 s with 3% or greater oxygen desaturation compared with baseline.
Ocular examination protocol and measurements
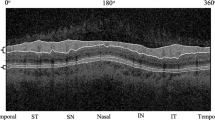
All ocular examination and measurements were performed at the Department of Ophthalmology, Kanuni Sultan Suleyman Education and Research Hospital. All subjects underwent detailed ophthalmic examinations, including slit-lamp biomicroscopy, tonometry, and fundus examination. All participants were examined with Cirrus HD-OCT 4000 (Carl Zeiss Meditec Inc., Dublin, CA, USA). A single well-trained examiner blinded to the study groups took the ocular images. All measurements were performed between 0900 and 1200 hours. OCT scans with signal strength >6 were included for analysis. The GCC mapping was conducted based on macular protocol centered on fovea with a cube of 512 × 128 with automated measurement of the GC-IPL thickness. Data for RNFL thickness were acquired using the ‘Optic Disc Cube 200 × 200' protocol. One eye of each participant was randomly selected for statistical analysis.
Outcome measures
Outcomes measures were the ganglion cell thickness including average and minimum GC-IPL thicknesses, and RNFL thickness parameters including average, temporal, superior, nasal, and inferior thicknesses.
Statistical analysis
All statistical analyzes were performed using SPSS 16.0 (SPSS, Chicago, IL, USA). The normality of all data samples was checked using the Shapiro–Wilk test. Comparisons among the groups were performed using one-way analysis of variance test, followed by the Bonferroni–Dunn post hoc test. χ2 tests were used for categorical variables. The Pearson's correlation coefficient was used to determine the relationship between the AHI and OCT parameters. Differences were considered statistically significant for P-values <0.05.
Results
A total of 185 subjects met the study criteria, including 40 eyes in the control group, 50 eyes in the mild OSAS group, 36 eyes in the moderate OSAS group, and 59 eyes in the severe OSAS group. The demographic and clinical characteristics of the groups are shown in Table 1. There was no difference between OSAS and control groups with respect to age, gender, intraocular pressure, axial length, refractive values, and existence of systemic diseases, including diabetes and hypertension.
Table 2 shows RNFL and GC-IPL thickness between the patients with OSAS and control subjects. Although RNFL thickness was not significantly different between the groups, the average GC-IPL thickness and minimum GC-IPL thickness were significantly lower in the OSAS group (P<0.05 for both).
The GC-IPL thickness measurements of the groups are shown in Table 3. A pairwise comparison between the groups revealed that severe OSAS group has statistically significant thinner average GC-IPL thickness and minimum GC-IPL thickness than the control group and mild OSAS group (P<0.05 for all). Table 4 shows the results of Pearson's correlation analysis between the AHI and OCT parameters. The AHI index was significantly negatively correlated with average GC-IPL (r=−0.232, P=0.005) and minimum GC-IPL (r=−0.233, P=0.005) thicknesses.
RNFL thickness measurements are shown in Table 5. No significant differences were found between the groups (P>0.05 for all). The results of Pearson's correlation analysis showed that the RNFL thickness measurements were not correlated with the AHI (P>0.05 for all) (Table 4)
Discussion
In this prospective cross-sectional study, we investigated the RNFL thickness and ganglion cell thickness in patients with OSAS and compared the results with a control group. To our knowledge, this study included one of the largest number of subjects with OSAS in the published literature. Our results suggested that the GC-IPL thickness in patients with severe OSAS was significantly lower than that of normal subjects; also, there was a significant negative correlation between the AHI and both average and minimum GC-IPL thicknesses.
Several previous studies have indicated an association between OSAS and glaucoma.5, 9, 10, 11, 12, 13, 14 Previous studies have reported that patients with OSAS had a high incidence and prevalence of glaucoma.4, 5, 20 Moreover, patients with primary open-angle glaucoma or normal-tension glaucoma constitute a high-risk population for OSAS.11, 12, 21 Conversely, a few studies have reported that the prevalence of glaucoma in patients with OSAS was similar to that in the general Caucasian population.15, 17
Glaucomatous optic neuropathy is characterized by degeneration of retinal ganglion cells (RGCs) and resulting changes in the optic nerve head such as reduction in RNFL thickness. Numerous studies have shown that early detection of decreased peripapillary RNFL thickness has a diagnostic ability to detect early glaucoma.22, 23 It has also been reported that 40% of RGC axon loss may have already occurred before a visual field defect is detected on a standard automated perimetry.24, 25 Several previous studies have investigated RNFL parameters in OSAS patients.5, 14, 20, 26 While most studies have reported decreased RNFL thickness in patients with OSAS,10, 14, 27, 28, 29, 30, 31, 32 some other studies found no reduction33, 34 or relationship between the RNFL thickness and disease severity.28, 29 In our study, RNFL thickness was not significantly different between the OSAS groups and control group in all quadrants. Moreover, no significant correlation was observed between AHI and RNFL thicknesses. Similarly, a study performed in Turkish population reported that RNFL thickness did not differ between healthy and OSAS subjects.35 Another study by Ferrandez et al36 reported that RNFL thickness measured with OCT did not differ significantly between groups.
There may be several factors responsible for the varying results among the studies. First factor, which may lead to differences among the studies, is difference in mean age of the study participants. Two previous studies and this study found that AHI was not correlated with RNFL thickness. The mean age in these studies was under 52 years.27, 29 A study by Shiba et al31 found a significant correlation between the AHI and RNFL thickness and the mean age in that study was 61.9 years old. It may be postulated that if the patients were older we would see a thinner RNFL thickness. Moreover, we do not know exactly how long the patients suffered from OSAS before diagnosis. RNFL thickness may decrease gradually over long periods of time with the OSAS. A second possible factor can be ethnical differences among the studies. Similar to our study, a study by Adam et al35 investigated RNFL thickness in Turkish patients with OSAS and did not find any difference between OSAS and control groups.
Recently, in addition to the evaluation of peripapillary RNFL thickness, measurement of the macular ganglion cell thickness by OCT has been used in several ocular and neurological conditions, particularly glaucoma. There are limited studies on ganglion cell thickness in patients with OSAS, which may lead to glaucoma and reduction in RNFL thickness. Ferrandez et al37 showed that neither GC-IPL nor GCL thickness were reduced in OSAS patients compared with healthy controls.37 Conversely, Huseyinoglu et al30 found lower ganglion cell thickness in patients with severe OSAS compared to the control group. In addition, there was a significant negative correlation between AHI and GC thickness. In our study, both average and minimum GC-IPL thicknesses were significantly reduced in patients with severe OSAS in comparison with healthy controls. Also, both average and minimum GC-IPL thicknesses showed a significant correlation with OSAS severity (AHI). The thinner ganglion cell layer thickness without a decrease in RNFL thickness in our patients with OSAS may suggest that measurement of the GC-IPL thickness may be a more effective method to detect early structural progression than measurement of RNFL thickness. Some recent studies have reported that the measurement of ganglion cell layer thickness may have an advantage over measurement of RNFL thickness in detecting the early glaucomatous structural changes.38, 39 It may be expected that RNFL thickness may gradually decrease over time in patients with OSAS even if this hypothesis remains to be demonstrated.
The underlying pathophysiology of ocular complications in OSAS has not been clearly elucidated; however, it appears to be multifactorial and is closely linked to hypoxia.40, 41 In patients with OSAS, hypoxia caused by repetitive episodes of upper airway obstruction results in a subsequent of increase in PaCO2 and decrease in PaO2.42 Long-term abnormal blood flow and hypoxia can lead to retinal layer cell damage. RGCs have been reported to be particularly sensitive to acute, transient, and mild systemic hypoxic stress.43 It has also been indicated that RGCs are more sensitive to ischemia than the more distal retinal cells.44, 45 Retinal hypoxia leads to increase in some mediators including vascular endothelial growth factor, nitric oxide, glutamate, inflammatory cytokines, and reactive oxygen species. Enhanced expression of these mediators causes RGCs loss by disruption of blood retinal barrier, excitotoxicity, and increased accumulation of intracellular Ca2+.36
The current study had some limitations. First, we evaluated the only retinal structural changes with OCT. The functional evaluation of retina should be analyzed in future studies using visual field testing with 10-2 program and pattern electroretinography in these subjects. Also, we do not know how long our patients suffered from OSAS before their diagnosis; peripapillary RNFL and GC-IPL thickness may alter gradually over long periods of time with the disease. A prospective longitudinal study is required for a better understanding of the peripapillary RNFL and GC-IPL thickness changes in OSAS patients.
In conclusion, we observed that severe OSAS patients had lower GCC thickness compared to mild OSAS patient or control group. We also found significant correlations between the severity of apnea (AHI) and GCC thickness. Future studies including monitoring of these participants with RNFL thickness and visual field measurements may indicate the role of this study in detection of early glaucomatous changes in patient with OSAS.

References
Muniesa M, Sánchez-de-la-Torre M, Huerva V, Lumbierres M, Barbé F . Floppy eyelid syndrome as an indicator of the presence of glaucoma in patients with obstructive sleep apnea. J Glaucoma 2014; 23: e81–e85.
Li J, McGwin G Jr, Vaphiades MS, Owsley C . Non-arteritic anterior ischaemic optic neuropathy and presumed sleep apnoea syndrome screened by the Sleep Apnea scale of the Sleep Disorders Questionnaire (SA-SDQ). Br J Ophthalmol 2007; 91: 1524–1527.
Mojon DS, Hedges TR 3rd, Ehrenberg B, Karam EZ, Goldblum D, Abou-Chebl A et al. Association between sleep apnea syndrome and nonarteritic anterior ischemic optic neuropathy. Arch Ophthalmol 2002; 120: 601–605.
Mojon DS, Hess CW, Goldblum D, Fleischhauer J, Koerner F, Bassetti C et al. High prevalence of glaucoma in patients with sleep apnea syndrome. Ophthalmology 1999; 106: 1009–1012.
Sergi M, Salerno DE, Rizzi M, Blini M, Andreoli A, Messenio D et al. Prevalence of normal tension glaucoma in obstructive sleep apnea syndrome patients. J Glaucoma 2007; 16: 42–46.
Purvin VA, Kawasaki A, Yee RD . Papilledema and obstructive sleep apnea syndrome. Arch Ophthalmol 2000; 118: 1626–1630.
Kloos P, Laube I, Thoelen A . Obstructive sleep apnea in patients with central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol 2008; 246: 1225–1228.
Leroux les Jardins G, Glacet-Bernard A, Lasry S, Housset B, Coscas G, Soubrane G . Retinal vein occlusion and obstructive sleep apnea syndrome. J Fr Ophtalmol 2009; 32: 420–424.
Marcus DM, Costarides AP, Gokhale P, Papastergiou G, Miller JJ, Johnson MH et al. Sleep disorders: a risk factor for normal-tension glaucoma? J Glaucoma 2001; 10: 177–183.
Kargi SH, Altin R, Koksal M, Kart L, Cinar F, Ugurbas SH et al. Retinal nerve fibre layer measurements are reduced in patients with obstructive sleep apnoea syndrome. Eye (Lond) 2005; 19: 575–579.
Mojon DS, Hess CW, Goldblum D, Böhnke M, Körner F, Mathis J . Primssary open-angle glaucoma is associated with sleep apnea syndrome. Ophthalmologica 2000; 214: 115–118.
Mojon DS, Hess CW, Goldblum D, Boehnke M, Koerner F, Gugger M et al. Normal-tension glaucoma is associated with sleep apnea syndrome. Ophthalmologica 2002; 216: 180–184.
Bendel RE, Kaplan J, Heckman M, Fredrickson PA, Lin SC . Prevalence of glaucoma in patients with obstructive sleep apnoea —a cross-sectional case-series. Eye (Lond) 2008; 22: 1105–1109.
Lin PW, Friedman M, Lin HC, Chang HW, Pulver TM, Chin CH . Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea/hypopnea syndrome. Graefes Arch Clin Exp Ophthalmol 2011; 249: 585–593.
Geyer O, Cohen N, Segev E, Rath EZ, Melamud L, Peled R et al. The prevalence of glaucoma in patients with sleep apneasyndrome: same as in the general population. Am J Ophthalmol 2003; 136: 1093–1096.
Girkin CA, McGwin G Jr, McNeal SF, Owsley C . Is there an association between pre-existing sleep apnoea and the development of glaucoma? Br J Ophthalmol 2006; 90: 679–681.
Kadyan A, Asghar J, Dowson L, Sandramouli S . Ocular findings in sleep apnoea patients using continuous positive airway pressure. Eye (Lond) 2010; 24: 843–850.
Pearson J . Glaucoma in patients with sleep apnea. Ophthalmology 2000; 107: 816–817.
Chervin RD, Guilleminault C . Obstructive sleep apnea and related disorders. Neurol Clin 1996; 14: 583–609.
Lin PW, Friedman M, Lin HC, Chang HW, Wilson M, Lin MC . Normal tension glaucoma in patients with obstructive sleep apnea/hypopnea syndrome. J Glaucoma 2011; 20: 553–558.
Goldblum D, Mathis J, Böhnke M, Bassetti C, Hess CW, Gugger M et al. Nocturnal measurements of intraocular pressure in patients with normal-tension glaucoma and sleep apnea syndrome. Klin Monatsbl Augenheilkd 2000; 216: 246–249.
Lee VW, Mok KH . Retinal nerve fiber layer measurement by nerve fiber analyzer in normal subjects and patients with glaucoma. Ophthalmology 1999; 106: 1006–1008.
Kwon YH, Hong S, Honkanen RA, Alward WL . Correlation of automated visual field parameters and peripapillary nerve fiber layer thickness as measured by scanning laser polarimetry. J Glaucoma 2000; 9: 281–288.
Quigley HA, Dunkelberger GR, Green WR . Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol 1989; 107: 453–464.
Kerrigan-Baumrind LA, Quigley HA, Pease ME, Kerrigan DF, Mitchell RS . Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci 2000; 41: 741–748.
Tjon-Fo-Sang MJ, Lemij HG . The sensitivity and specificity of nerve fibre layer measurements in glaucoma as determined with scanning laser polarimetry. Am J Ophthalmol 1997; 123: 62–69.
Casas P, Ascaso FJ, Vicente E, Tejero-Garcés G, Adiego MI, Cristóbal JA . Retinal and optic nerve evaluation by optical coherence tomography in adults with obstructive sleep apnea-hypopnea syndrome (OSAHS). Graefes Arch Clin Exp Ophthalmol 2013; 251: 1625–1634.
Moghimi S, Ahmadraji A, Sotoodeh H, Sadeghniat K, Maghsoudipour M, Fakhraie G et al. Retinal nerve fiber thickness is reduced in sleep apnea syndrome. Sleep Med 2013; 14: 53–57.
Sagiv O, Fishelson-Arev T, Buckman G, Mathalone N, Wolfson J, Segev E et al. Retinal nerve fiber layer thickness measurements by optical coherence tomography in patients with sleep apnea syndrome. Clin Experiment Ophthalmol 2014; 42: 132–138.
Huseyinoglu N, Ekinci M, Ozben S, Buyukuysal C, Kale MY, Sanivar HS . Optic disc and retinal nerve fiber layer parameters as indicators of neurodegenerative brain changes in patients with obstructive sleep apnea syndrome. Sleep Breath 2014; 18: 95–102.
Shiba T, Takahashi M, Sato Y, Onoda Y, Hori Y, Sugiyama T et al. Relationship between severity of obstructive sleep apnea syndrome and retinal nerve fiber layer thickness. Am J Ophthalmol 2014; 157: 1202–1208.
Calvo P, Ferrandez B, Ferreras A, Marín JM . Retinal nerve fiber layer thickness alterations in patients with obstructive sleep apnea. Arch Soc Esp Oftalmol 2012; 87: 1–2.
Ferrandez B, Ferreras A, Calvo P, Abadia B, Fogagnolo P, Wang Y et al. Retinal sensitivity is reduced in patients with obstructive sleep apnea. Invest Ophthalmol Vis Sci 2014; 55: 7119–7125.
Salzgeber R, Iliev ME, Mathis J . Do optic nerve head and visual field parameters in patients with obstructive sleep apnea syndrome differ from those in control individuals? Klin Monbl Augenheilkd 2014; 231: 340–343.
Adam M, Okka M, Yosunkaya S, Bozkurt B, Kerimoğlu H, Turan M . The Evaluation of Retinal Nerve Fiber Layer Thickness in Patients with Obstructive Sleep Apnea Syndrome. J Ophthalmol 2013; 2013: 292158.
Ferrandez B, Ferreras A, Calvo P, Abadia B, Pajarin AB, Marin JM et al. Assessment of the retinal nerve fiber layer in individuals with obstructive sleep apnea. BMC Ophthalmology 2016; 16: 40.
Ferrandez B, Ferreras A, Calvo P, Abadia B, Pajarin AB, Marin JM et al. Macular Retinal Ganglion Cell Layer Thickness Is Not Reduced in Patients with Obstructive Sleep Apnea. Ophthalmic Res 2016; 56: 85–91.
Anraku A, Enomoto N, Takeyama A, Ito H, Tomita G . Baseline thickness of macular ganglion cell complex predicts progression of visual field loss. Graefes Arch Clin Exp Ophthalmol 2014; 252: 109–115.
Lee J, Hangai M, Kimura Y, Takayama K, Kee C, Yoshimura N . Measurement of macular ganglion cell layer and circumpapillary retinal nerve fiber layer to detect paracentral scotoma in early glaucoma. Graefes Arch Clin Exp Ophthalmol 2013; 251: 2003–2012.
Abdal H, Pizzimenti JJ, Purvis CC . The eye in sleep apnea syndrome. Sleep Med 2006; 7: 107–115.
Dhillon S, Shapiro CM, Flanagan J . Sleep-disordered breathing and effects on ocular health. Can J Ophthalmol 2007; 42: 238–243.
Bilgin G . Normal-tension glaucoma and obstructive sleep apnea syndrome: a prospective study. BMC Ophthalmol 2014; 14: 27.
Kergoat H, Hérard ME, Lemay M . RGC sensitivity to mild systemic hypoxia. Invest Ophthalmol Vis Sci 2006; 47: 5423–5427.
Cinici E, Tatar A . Thickness alterations of retinal nerve fiber layer in children with sleep-disordered breathing due to adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 2015; 79: 1218–1223.
Simsek A, Bayraktar C, Dogan S, Uckardes F, Reyhan AH, Sarikaya Y et al. Retinal nerve fiber layer thickness alteration in apneic children. Optom Vis Sci 2016; 93: 63–69.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kara, N., Sayin, N., Bayramoglu, S. et al. Peripapillary retina nerve fiber layer thickness and macular ganglion cell layer thickness in patients with obstructive sleep apnea syndrome. Eye 32, 701–706 (2018). https://doi.org/10.1038/eye.2017.279
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.279
This article is cited by
-
Plasma homocysteine and macular thickness in older adults—the Rugao Longevity and Aging Study
Eye (2022)
-
Ganglion cell layer thickening in patients suffering from Obstructive Sleep Apnea–Hypopnea syndrome with long Mean Apnea–Hypopnea Duration during sleep
International Ophthalmology (2021)
-
Thinning of the inner and outer retinal layers, including the ganglion cell layer and photoreceptor layers, in obstructive sleep apnea and hypopnea syndrome unrelated to the disease severity
International Ophthalmology (2021)
-
Evaluation of effects of positive airway pressure treatment on retinal fiber thickness and visual pathways using optic coherence tomography and visual evoked potentials in the patients with severe obstructive sleep apnea syndrome
International Ophthalmology (2020)