Abstract
Purpose
To compare axial length (AL) with vitreous cavity length (VCL) in patients with keratoconus and to ascertain whether graft size can be tailored to reduce myopic refractive error in patients with keratoconus undergoing penetrating keratoplasty (PK).
Patients and methods
The AL and VCL were measured prospectively in patients with keratoconus not undergoing PK (Group 1) and in normal phakic, emmetropic individuals (Group 2). A retrospective analysis of these measurements in patients with keratoconus who had undergone PK (Group 3) was also performed. The postoperative spherical equivalent (SE) was then correlated to size of donor buttons.
Results
Keratoconus patients tended to have a longer mean VCL than emmetropic normal individuals. The mean VCL of these patients (Group 1) was 16.49 mm±SD 1.13 compared to the mean VCL of 15.94 mm±SD 0.56 in normals (Group 2, P<0.0001). Patients with keratoconus who had an undersized graft showed reduced myopic refractive error compared to those with same size or oversized grafts.
Conclusion
VCL measurement is more accurate than AL measurement in deciding upon graft-host size disparity for corneal graft in patients with keratoconus. In patients with increased VCL, undersizing the donor button helps in reducing postoperative myopia. We recommend VCL measurement as part of the routine workup in all keratoconus patients undergoing corneal transplants.
Similar content being viewed by others
Introduction
Keratoconus (KC) is a non-inflammatory, usually bilateral but often asymmetric, ectasia of the cornea. Clinically, progressive corneal thinning results in a conical protrusion of the central cornea with the apex of the cone just inferior to the visual axis. A majority of patients with KC present with progressive myopic astigmatism. The myopia can be corneal, axial, or both. When the ectasia is significant, corneal curvature alterations result in irregular astigmatism.1 Optical correction of the refractive error in KC can be achieved with spectacles or contact lenses in a majority of patients. In some instances however, when the ectasia is excessive or the patient is intolerant of contact lenses, a corneal transplant procedure becomes necessary. Of the various surgical approaches available,1, 2, 3, 4 deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PK) are the procedures of choice for visual rehabilitation in advanced KC.1, 2 Though PK enjoys a high success rate for KC in terms of graft clarity and survival,5, 6, 7 the post keratoplasty refractive results maybe unsatisfactory.8, 9, 10, 11, 12, 13 The aim of keratoplasty is to reduce the high corneal refractive power (and astigmatism) to one that can be successfully managed with glasses or contact lenses. Various authors have advocated the use of same size or 0.25 mm smaller donor trephine to reduce postoperative refractive errors as oversized donor trephines, 0.5 mm larger, tend to increase myopia. However, there is usually residual high postoperative myopia or hypermetropia and high corneal astigmatism often resulting in anisometropia.14, 15, 16, 17, 18, 19, 20, 21 Attempts to improve refractive outcomes have suggested use of axial length (AL) measurements in KC patients in order to determine preoperatively the choice of graft-host disparity in button size.22, 23, 24 Doyle et al25 in a retrospective study showed a linear relationship between vitreous cavity length (VCL) and sphericalequivalent (SE) following PK for KC but unfortunately no details are provided on what constituted the ‘vitreous cavity’ in their measurements.
We analysed clinical parameters of our KC patients who had undergone PK and normal subjects with the following aims: (A) to determine the AL and VCL in patients with keratoconus not undergoing PK, (B) to determine the AL and VCL in normal phakic, emmetropic individuals, and (C) to determine the AL and VCL in patients with KC who had undergone PK. In the latter group, the ALs and VCLs were correlated with the donor button and host bed disparity in diameter, and its effect on the refractive outcome. DALK patients were excluded as it was not clear from the notes whether a type-1, type-2, mixed, or no big bubble was achieved during surgery and these variables could not be accounted for in the analysis.26
Patients and methods
A total of 136 eyes of 72 patients with KC (Group 1); 40 phakic, emmetropic eyes of 20 patients (control Group 2), and 31 eyes of 26 patients who had undergone PK for KC (Group 3) at least 2 years ago (range from 2 to 10 years) were included. Groups 1 and 2 were prospectively evaluated and Group 3 was retrospective. In Group 1 there were 43 males and 29 females ranging in age from 19 to 55 years. In Group 2 there were 6 males and 14 females ranging in age from 20 to 52 years. In Group 3 there were 8 females and 18 males, between the ages of 22 and 56 years.
Axial length measurement
AL was measured by A scan ultrasonography using the Alcon Biophysic OcuScan instrument, version 3.02 (Alcon, Forth Worth, Texas, USA). The probe was lightly applied to the surface of the cornea after instilling topical anaesthesia with tetracaine minims 1% w/v (Bausch & Lomb, Kingston, UK). Care was taken not to indent the corneal surface. Only traces showing well-defined peaks, to full height of the cornea, lens anterior and posterior capsules and chorioretina were selected. An average of ten readings were taken for both AL and VCL. The AL was measured from the anterior corneal peak to the chorioretinal peak. The anterior chamber was measured from the corneal peak to the first peak of the lens (anterior capsule) and the vitreous chamber was measured from the second peak of the lens (posterior capsule) to the chorioretinal peak. In the phakic mode, the anterior chamber depth was measured with a velocity of 1532 m/s. The lens was measured (first peak of lens to second peak of lens) with a velocity of 1641 m/s and the VCL with a velocity of 1532 m/s.
Refraction and keratometry
Optical keratometry using a Javal-Schiotz keratometer (Haag Streit UK, Harlow, Essex, UK) was carried out. Refraction was determined by streak retinoscopy by a trained optometrist. SE represented the spherical error plus half the astigmatic error measured in dioptres (D).
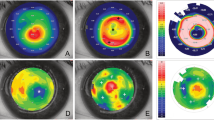
Penetrating keratoplasty
The indication for surgery in KC patients was intolerance to contact lenses, corrected visual acuity of less than 6/18 and the presence of central corneal scarring. All grafts were performed under general anaesthesia by the same experienced surgeon (HD). The Hessburg Barron recipient and donor trephines were used in all cases (Spectrum ophthalmics Ltd, Macclesfield, UK). The size of trephines was between 7.00 and 8.50 mm. All donor buttons were organ cultured and punched from the endothelial side. When the donor trephine was 0.25 mm larger than the host trephine the donor button was regarded as ‘Same size’. When the donor trephine was 0.5 mm larger than the host trephine the donor button was regarded as ‘Over sized’. When the donor trephine was the same size as the host trephine the donor button was regarded as ‘Under sized’. Postoperatively patients were treated with topical dexamethasone and chloramphenicol eye drops (Bausch & Lomb). All patients had all sutures removed at the time of assessment for the study.
Statistics
An unpaired t-test was used to analyse the correlation between the AL and VCL of the 136 keratoconus eyes with the control group respectively.
Results
The mean VCL of the 136 keratoconus eyes was 16.49 mm±SD 1.13 (range 15.01–20.11 mm) and the mean AL of these patients was 23.84 mm±SD 1.25 (range 21.40–27.95 mm). All eyes were further subdivided into three subgroups determined by the VCL (Table 1). Subgroup A (VCL≤15.50 mm); subgroup B (VCL between 15.51–16.50 mm) and subgroup C (VCL>16.50 mm). There were 20 eyes in subgroup A (range 14.21–15.40 mm); 59 eyes in subgroup B (range 15.51–16.43 mm) and 57 eyes in subgroup C (range 16.55–20.11 mm). The mean AL of the 40 emmetropic eyes used as a control group was 23.37 mm±SD 0.53 (range 22.26–24.3 mm) and the mean VCL was 15.94 mm±SD 0.56 (range 14.38–16.59 mm) with 9 in subgroup A, 25 in subgroup B and 6 in subgroup C (Table 1).
The VCL of the 136 keratoconus eyes (Group 1) was longer by a mean of 0.55 mm than the control group (Group 2). This was statistically significant (P<0.0001). Similarly, the anterior chamber depth and the AL in the KC eyes (Group 1) were significantly longer than in the control group (Group 2, P<0.05 for AC and P<0.001 for AL).
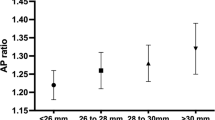
In the 31 eyes with PK, there were 8 eyes with VCL falling in subgroup A (range 14.21–15.40 mm), 14 eyes in subgroup B (range 15.51–16.43 mm) and 9 eyes in subgroup C (range 16.55–20.11 mm) (Table 1). Of the 31 eyes, 7 eyes that had under sized button (same sized trephine) had postoperative SE between +0.25 to –6.75 D. In the 20 eyes where donor button was same sized (trephine oversized by 0.25mm), 7 eyes had a hypermetropic SE between +0.25 to+4.00 D; 12 eyes had a myopic SE between −0.75 to –8.00 D and 1 eye had an emmetropic equivalent. All 4 eyes with oversized donor buttons (trephine oversized by 0.5mm) had a myopic SE between −0.75 to -17.50 D postoperatively.
The mean SE (MSE) for the same sized buttons (20 eyes) was −1.92 D±SD 3.56 (range −8.00 to +4.00 D). The MSE for the oversized buttons (four eyes) was –6.50 D±SD 7.84, (range –0.75 to −17.50 D). The MSE for undersized buttons (7 eyes) was −0.79 D±SD 3.74 (range −6.75 to +0.25 D). Overall 18 of the 31 eyes had a myopic SE between −0.75 and −17.50D.
We also analysed the correlation between VCL, AL, donor/host trephine size, and SE in 9 eyes that underwent PK for KC (subgroup C of group 3) (Table 2).
Discussion
Most patients with keratoconus have a myopic spherical error. When such patients come up for a corneal transplant procedure, often an attempt is made to address the myopia by undersizing the donor button. This is achieved by using a donor trephine of the same diameter as the host bed trephine, when the donor cornea is punched from the endothelial side. However, it is increasingly apparent that not all the myopia in keratoconus is due to increased AL.22, 23, 25 When the myopia is predominantly of corneal origin, undersizing the donor button would lead to unnecessary flattening of the cornea postoperatively with a resultant hyperopic shift. Furthermore, AL measurements would be an inaccurate indication of axial myopia because the ectatic cornea would add to the depth of the anterior chamber and the overall length of the eye. It would therefore be prudent to measure the VCL, as an indicator of the axial myopia in deciding whether the preoperative myopia is predominantly axial or corneal.
The data in this study and others22, 25 illustrates that though the AL in KC eyes is generally longer than normal, the VCL is not necessarily so. Even though both VCL and AL in KC were statistically significantly longer than in normals, individual patients may have normal VCL despite a longer AL. Clinically this is important because while deciding on graft size with a view to flatten the cornea or not, the VCL must be individually measured. In this study 20 of the 136 patients had a VCL of ≤15.5 mm who would not benefit from a ‘flat’ graft compared to the 59 patients who had a longer VCL and would benefit from a flat graft.
Furthermore, there can even be a difference in the two eyes of the same patient. Graft and host sizing therefore cannot be generalised to any group or even individual patient.
A case (Table 2, No. 7) in this study emphasises this point. The patient had AL of 26.08 mm and VCL of 18.84 mm in the right eye. In the unoperated left eye, the AL was 24.70 mm and the VCL was 18.84 mm. The right eye had a PK with a same sized donor button (0.25 mm oversized donor trephine) and the resultant postoperative SE was −8.00 D. Ideally this patient should have had an undersized graft, which would have resulted in a reduced amount of postoperative myopia. Another important case in point (Table 2 case numbers 6a, 6b) further illustrates the influence of graft-host size disparity on the resultant refractive outcome. Both eyes had approximately similar ALs and VCLs. In the right eye the donor button was oversized by 0.25 mm (trephine oversized by 0.5 mm) and in the left eye it was undersized by 0.25 mm (same size trephine for donor and host bed). The right eye had a postoperative myopia of –17.5 D and the left of –6.75 D. This case also illustrates the point that although significant reduction in myopia can be achieved by marginally undersizing the donor button, some residual myopia can remain. Attempts to reduce the size of the donor button further are not recommended as this could lead to other problems such as wound leaks and undue flattening of the graft with surface problems and difficulty in contact lens fitting.
Lanier et al23 considered the AL (not VCL) in KC patients in deciding graft size. They observed that there was a wide variability in the postoperative refractive errors related to the wide range of AL in KC eyes. They suggested that most preoperative KC eyes had their ALs in a relatively normal range of between 23.50 mm and 24.50 mm and should not be shortened surgically. The longer AL of more than 26.00 mm may benefit in reducing myopia by decreasing their AL. The mean AL of their KC eyes was 24.39 mm±SD 1.13 mm with a range of 21.82–28.69 mm. In our study the mean AL was similar, 23.84 mm±SD 1.25 mm but with a relative wide range 21.40–27.95 mm. Shimmura et al22 too, in a prospective study considered the AL in deciding graft size. They used same size trephines (undersized buttons) in patients with preoperative ALs of greater than 24.50 mm and 0.25 mm larger trephines (same size buttons) in eyes with AL <24.49 mm. In 11 eyes where this protocol was not adhered to and short eyes were grafted with buttons obtained with same size trephines (undersized buttons), a hyperopic postoperative refraction was noted.
Doyle et al25 and Tuft et al24 in retrospective studies compared VCL and AL measures to the graft-host size disparity and refractive outcome. Doyle et al25 concluded that for eyes with a VCL of <15.5 mm, a donor trephine of 0.25 mm larger should be used to punch from the endothelial side. Tuft et al24 reached the conclusion that increased AL makes a significant contribution to the myopia seen in KC eyes and that PK reduces the central corneal ectasia of KC but has little effect on reducing the AL of the globe.
In our retrospective study of 31 corneal grafts in KC eyes we observed that when AL, as a parameter was compared to the choice of graft-host size disparity, the refractive outcome was very variable. However when VCL was considered as the parameter, the results were more consistent. Based on these results we recommend the following:
(A) Measurement of vitreous length should be done routinely in the workup of patients undergoing corneal transplant for keratoconus. (B) Graft-host size disparity should be planned accordingly. (C) If the VCL is ≤15.50 mm, we recommend using a trephine of 0.5 mm diameter larger than the one used for cutting the host bed (oversize button by 0.25 mm). (D) If the VCL is between 15.50 mm and 16.50 mm, to use a 0.25 mm larger trephine for the donor (same sized button as host bed) and (E) if the VCL is≥16.50 mm to use a trephine of the same size as the host bed (undersized button by 0.25 mm diameter). These recommendations are summarised in Table 3.
We have not undersized the donor trephine by more than 0.25 mm in any case and it is not something that we recommend on the basis of the potential risks of wound leaks, irregular astigmatism and very flat graft topography. The following considerations also apply to all cases. The decision to undersize the button should take into account the refractive state of the other eye. With undersized buttons the risk of wound leakage is high and tight sutures need to be applied. Using a vacuum trephine on a very thin host bed could lead to a larger than intended or noncircular host bed. As vacuum trephines undermine the edge of the host bed while cutting, only a partial thickness cut should be made with the vacuum trephine and completed with a corneal scissors cutting vertically. The refractive outcome, particularly astigmatism, would also be affected by the disparity in graft and host thickness. Often the host beds are thinner than the donor buttons and do not support the buttons well. In such circumstances tailoring the graft size alone may not give the desired result.

References
Keane M, Coster D, Ziaei M, Williams K . Deep anterior lamellar keratoplasty versus penetrating keratoplasty for treating keratoconus. Cochrane Database Syst Rev 2014; 7: CD009700.
Söğütlü Sari E, Kubaloğlu A, Ünal M, Piñero Llorens D, Koytak A, Ofluoglu AN et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty: comparison of optical and visual quality outcomes. Br J Ophthalmol 2012; 96: 1063–1067.
Boxer Wachler BS, Christie JP, Chandra NS, Chou B, Korn T, Nepomuceno R . Intacs for Keratoconus. Ophthalmology 2003; 110: 1031–1040.
Parker JS, van Dijk K, Melles GR . Treatment options for advanced keratoconus: a review. Surv Ophthalmol 2015; 60: 459–480.
Choi JA, Lee MA, Kim MS . Long-term outcomes of penetrating keratoplasty in keratoconus: analysis of the factors associated with final visual acuities. Int J Ophthalmol 2014; 7: 517–521.
Huang T, Hu Y, Gui M, Hou C, Zhang H . Comparison of refractive outcomes in three corneal transplantation techniques for keratoconus. Graefes Arch Clin Exp Ophthalmol 2015; 253: 1947–1953.
Watson SL, Ramsay A, Dart JK, Bunce C, Craig E . Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology 2004; 111: 1676–1682.
Buzard KA, Fundingsland BR . Corneal transplant for keratoconus: results in early and late disease. J Cataract Refract Surg 1997; 23: 398–406.
Goble RR, Hardman Lea SJ, Falcon MG . The use of the same size host and donor trephine in penetrating keratoplasty for keratoconus. Eye 1994; 8: 311–314.
Wilson SE, Bourne WM . Effect of recipient-donor trephine size disparity on refractive error in keratoconus. Ophthalmology 1989; 96: 299–305.
Spadea L, Bianco G, Mastrofini MC, Balestrazzi E . Penetrating keratoplasty with donor and recipient corneas of the same diameter. Ophthalmic Surg Lasers 1996; 27: 425–430.
Girard LJ, Esnaola N, Rao R, Barnett L, Rand WJ . Use of grafts smaller than the opening for keratoconic myopia and astigmatism. A prospective study. J Cataract Refract Surg 1992; 18: 380–384.
Busin M, Zambianchi L, Franceschelli F, Lamberti G, al-Naweiseh I . Intraoperative cauterization of the cornea can reduce postkeratoplasty refractive error in patients with keratoconus. Ophthalmology 1998; 105: 1524–1529.
Javadi MA, Mohammadi MJ, Mirdehghan SA, Sajjadi SH . A comparison between donor-recipient corneal size and its effect on the ultimate refractive error induced in keratoconus. Cornea 1993; 12: 401–405.
Girard LJ, Eguez I, Esnaola N, Barnett L, Maghraby A . Effect of penetrating keratoplasty using grafts of various sizes on keratoconic myopia and astigmatism. J Cataract Refract Surg 1988; 14: 541–547.
Razmjoo H, Ghoreishi SM, Ashtari A, Ghafouri I, Mamousi B . Comparison the post operative refractive errors in same size corneal transplantation through deep lamellar keratoplasty and penetrating keratoplasty methods after sutures removing in keratoconus patients. Adv Biomed Res 2016; 5: 39.
Perry HD, Foulks GN . Oversize donor buttons in corneal transplantation surgery for keratoconus. Ophthalmic Surg 1987; 18: 751–752.
Olson RJ . Variation in corneal graft size related to trephine technique. Arch Ophthalmol 1979; 97: 1323–1325.
Oh BL, Kim MK, Wee WR . Comparison of clinical outcomes of same-size grafting between deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. Korean J Ophthalmol 2013; 27: 322–330.
Serdarevic ON, Renard GJ, Pouliquen Y . Penetrating keratoplasty for keratoconus: role of videokeratoscopy and trephine sizing. J Cataract Refract Surg 1996; 22: 1165–1174.
Seitz B, Langenbucher A, Küchle M, Naumann GO . Impact of graft diameter on corneal power and the regularity of postkeratoplasty astigmatism before and after suture removal. Ophthalmology 2003; 110: 2162–2167.
Shimmura S, Ando M, Ishioka M, Shimazaki J, Tsubota K . Same size donor corneas for myopic keratoconus. Cornea 2004; 23: 345–349.
Lanier JD, Bullington RH Jr, Prager TC . Axial length in keratoconus. Cornea 1992; 11: 250–254.
Tuft SJ, Fitzke FW, Buckley RJ . Myopia following penetrating keratoplasty for keratoconus. Br J Ophthalmol 1992; 76: 642–645.
Doyle SJ, Harper C, Marcyniuk B, Ridgway AE . Prediction of refractive outcome in penetrating keratoplasty for keratoconus. Cornea 1996; 15: 441–445.
Dua HS, Katamish T, Said DG, Faraj LA . Differentiating type 1 from type 2 big bubbles in deep anterior lamellar keratoplasty. Clin Ophthalmol 2015; 9: 1155–1157.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Messina, M., Umapathy, T., Avadhanam, V. et al. Vitreous cavity length in keratoconus: implications for keratoplasty. Eye 32, 359–363 (2018). https://doi.org/10.1038/eye.2017.184
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.184