Abstract
Purpose
To determine the ability of the newly developed internet-based Spaeth/Richman Contrast Sensitivity (SPARCS) test to assess contrast sensitivity centrally and peripherally in cataract subjects and controls, in comparison with the Pelli–Robson (PR) test.
Methods
In this prospective cross-sectional study, cataract subjects and age-matched normal controls were evaluated using the SPARCS and PR tests. Contrast sensitivity testing was performed in each eye twice in a standardized testing environment in randomized order. SPARCS scores were obtained for central, right upper (RUQ), right lower (RLQ), left upper (LUQ), and left lower quadrants (LLQ). PR scores were obtained for central contrast sensitivity. PR and SPARCS scores in cataract subjects were compared with controls. Intraclass correlation coefficients (ICC) and Bland Altman analysis were used to determine test–retest reliability and correlation.
Results
A total of 162 eyes from 84 subjects were analyzed: 43 eyes from 23 cataract subjects, and 119 eyes from 61 controls. The mean scores for SPARCS centrally were 13.4 and 14.5 in the cataract and control groups, respectively (P=0.001). PR mean scores were 1.31 and 1.45 in cataract and control groups, respectively (P<0.001). ICC values for test–retest reliability for cataract subjects were 0.75 for PR and 0.61 for the SPARCS total. There was acceptable agreement between the ability of PR and SPARCS to detect the effect of cataract on central contrast sensitivity.
Conclusions
Both SPARCS and PR demonstrate a significant influence of cataract on contrast sensitivity. SPARCS offers the advantage of determining contrast sensitivity peripherally and centrally, without being influenced by literacy.
Similar content being viewed by others
Introduction
Visual acuity (VA) is commonly used to evaluate vision. Subjects with cataracts, however, may have good VA even though they report poor vision.1, 2 To more thoroughly assess vision in cataract subjects, VA can be supplemented with a test of contrast sensitivity (CS), the threshold to distinguish an object from its background.3 CS influences numerous aspects of people’s vision, including VA, visual field, motion detection, dark adaptation, and pattern recognition. CS is also a useful assessment of people’s functional vision,4 and decreased CS has been found to be responsible for the symptoms of poor vision in people with cataracts.2 Decreased CS may hinder people’s ability to discriminate traffic signs and faces and perform tasks such as walking, going up and down stairs, dialing a telephone, reading and driving.5, 6, 7 In fact, CS is better than VA in predicting many aspects of functional vision.7, 8
The Pelli–Robson (PR) test is a well-established, commonly used CS test. It is a chart showing letters of constant size but decreasing contrast. It is readily available, inexpensive, quick, consistent, and easy to administer; it evaluates CS centrally.3 It requires recognition of letters using pattern recognition and cognition, so its results may be influenced by the intelligence and literacy level of the subjects tested.
The Spaeth/Richman Contrast Sensitivity (SPARCS) test is a CS test that can be performed on a computer with access to the Internet. It evaluates CS centrally and in four peripheral quadrants and scores them separately. Because it contains contrast gratings instead of letters, low literacy level subjects may be tested as reliably as literate subjects. The five areas are presented in two irregular sequences, so even with retesting, memorizing the answer sequence is unlikely.
This study aimed to compare the SPARCS test to the PR test in the evaluation of subjects with cataracts.
Materials and methods
Subjects
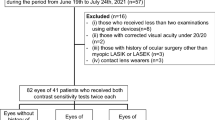
This prospective cross-sectional study was approved by the Institutional Review Board of Wills Eye Hospital and was conducted in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. The trial was registered on the ClinicalTrials.gov database (NCT01300949). Testing was carried out at the Wills Eye Hospital Glaucoma Research Center between January 2010 and August 2013. The control group included 119 eyes from 61 subjects while the cataract subject group included 43 eyes from 23 subjects. Groups of 23 and 61 subjects provided 80% power to detect a moderately large effect size of 0.7 or greater. Power was greater for this study’s sample since most subjects had data from both eyes.
Prior to participating, all subjects were given an explanation of the study. Written informed consent was obtained from all study participants. Inclusion criteria required subjects to be 18 years of age or older, able to provide fully informed consent, and either a cataract subject or healthy control. Those who could not speak or understand sufficient English or had cognitive impairment were excluded.
Cataract subjects were recruited from the Cataract and Primary Eye Care service of Wills Eye Hospital. Subjects’ lenses were graded according to the Lens Opacities Classification System II (LOCS II).9 Eyes with nuclear opacities 4+, anterior subcapsular, posterior subcapsular and cortical opacities affecting the visual axis were excluded due to the limited number of subjects in this population that could be recruited. The remaining subjects were divided into three groups: 1+ nuclear sclerosis; 2+ nuclear sclerosis; and 3+ nuclear sclerosis. Cataract subjects were excluded if their ocular history included optic nerve, cornea, or retinal diseases; previous surgeries; or ocular trauma.
The control group included volunteers and subjects recruited from unrelated studies conducted at the Wills Eye Hospital Glaucoma Research Center. Controls were required to have a best-corrected VA≤20/40 and no ocular or neurological pathology affecting their vision, which was confirmed during the clinical evaluation. The control group included some subjects who had previous cataract surgery.
Clinical evaluation
Demographic information and an ocular medical history were obtained and documented for each subject. All subjects were given a comprehensive ophthalmic clinical examination. Subjects were not routinely dilated. This examination included (1) Snellen VA, which was then converted to the logarithm of the minimum angle of resolution (logMAR), (2) refraction, (3) intraocular pressure via Goldmann Applanation tonometry, (4) a slit-lamp and fundus examination, (5) an optic nerve examination in which vertical cup-to-disc (C/D) ratio was assessed, (6) monocular Humphrey Visual field (24-2 Swedish Interactive Threshold Algorithm Standard Strategy; Carl Zeiss Meditec Inc., Dublin, CA, USA), and (7) monocular PR and SPARCS tests. Spherical and cylindrical refractions were obtained by averaging three consecutive readings with an autorefractor (Topcon KR-8000 auto keratorefractometer, Japan).
CS Assessment
Each subject was administered the PR test and the SPARCS test monocularly twice. The order of the tests was either PR, SPARCS, rest, then SPARCS, PR or SPARCS, PR, rest, then PR, SPARCS. A technician explained and administered each test. The second test was administered by a different technician to prevent testing bias. The results of one technician were hidden from the other. Testing order was randomized before subject enrollment using a randomization list generated from http://www.randomizer.org/. The non-tested eye was covered with an occluder. Both tests were performed in each eye with the subject’s habitual eyeglasses correction if needed. Testing was conducted in a room with fluorescent lighting and no windows to minimize glare and reflections and ensure uniform testing conditions.
PR test
The PR chart is a large wall-mounted chart, 59 cm wide and 84 cm high, with 16 triplets of Sloan letters of constant size.10 From top to bottom and left to right, each triplet decreases in contrast by 0.15 log units from 100% (0.00 log units) to 0.56% (2.25 log units). Each letter subtends 2.8° at the test distance of 1 meter. In this study, the chart was illuminated by multiple incandescent lamps. Testing ended when the subject failed to identify 2 of the 3 letters in a triplet correctly, and the log CS score was recorded. The test was performed twice and the scores averaged.
Spaeth/Richman contrast sensitivity test (SPARCS)
SPARCS is a novel internet-based assessment of CS, which can be accessed at https://www.sparcscontrastcenter.com. The website provides each subject with a unique ID and instructions to take the test. The test can be performed using a standard web-browser on a computer with a monitor set to 1024 × 768 resolution, 256 gray levels, and a monitor size at least 22 cm wide and 26.5 cm high. Two parallel horizontal lines and 2 parallel vertical lines divide the computer screen into 9 areas, with a rectangle in the center (Figure 1a). The online test has a screen standardization setting to rescale the screen such that the center rectangle is 4.4 cm wide. At the prescribed viewing distance of 50 cm, the test occupies 30° of vision horizontally and 23.5° of vision vertically, and, in the central test area, 5° of vision horizontally and 3.5° of vision vertically.
(a) Main screen of SPARCS test. Two vertical lines and two horizontal lines intersect to form nine rectangles. Contrast sensitivity is tested in the left upper quadrant, left lower quadrant, right upper quadrant, right lower quadrant, and central area. (b) A presentation of darkened vertical square wave gratings in the left upper quadrant during the SPARCS test. SPARCS=Spaeth/Richman Contrast Sensitivity Test.
SPARCS evaluates CS in five areas of the visual field: the left upper quadrant (LUQ), left lower quadrant (LLQ), right upper quadrant (RUQ), right lower quadrant (RLQ), and central area. During the test, an image is displayed in one of the 5 testing areas at random for 0.3 s, while the other 4 areas stay a similar color to the background (Figure 1b). This image consists of square wave gratings in the form of vertical dark bars on a constant light background at a fixed spatial frequency of 0.4 cycles per degree. During the test, the luminance of the gratings is gradually decreased. Seventeen potential levels of contrast can be tested. Contrast decreases by ~0.15 log units between levels and ranges from 100 to 0.45% (log CS 0.00 to 2.35).
The subject is instructed to maintain fixation on the central area throughout the test. In this study, central fixation was verified by the trained technician who observed the subject during the testing period. If fixation was not acceptable, the test was restarted. The subject indicates which area the vertical dark bars appeared (LUQ, LLQ, RUQ, RLQ, or center) and the technician makes the selection according the subject’s response. If the subject was unable to discern any contrast, the failed quadrant option was selected.
The testing strategy uses a staircase method with reversals as described by Richman et al11 In the beginning, correct responses allow the subject to advance 4 levels until an incorrect response is made. Then, the algorithm presents a contrast level that is 2 levels easier. The test then advances or regresses 1 level at a time until the subject makes 2 incorrect responses at a certain contrast level. This establishes the contrast threshold for the testing area. In areas where the threshold has been reached, contrast levels plus or minus one level of the threshold are presented at random until a threshold has been determined for all the remaining test areas, at which point the test is complete. Each of the 5 testing region’s log-based scores are scaled 0 to 20, making the highest possible SPARCS score to be 100. In this study, the scores were averaged between the two trials.
Statistical analysis
Data was analyzed using SAS software, version 9.2 and later (SAS Institute Inc, Cary, NC, USA). Demographic and clinical information was summarized using means and standard deviations or counts and percentages, as appropriate. Groups were compared with respect to eye-level data using mixed effects linear regression to account for correlation among eyes from the same subject. The 5 SPARCS position scores were modeled jointly using mixed effects linear regression. Fixed effects were included for position, group, test, and interactions between group and test and position and test. Random intercept and position effects were included for each subject to account for correlation between eyes from the same subjects. Within each eye, a direct product covariance structure for repeated multivariate measurements (un@cs) was assumed that allowed for an unstructured correlation among the 5 position scores at each test and a single parameter representing correlation among repeated test measurements. Within this model, least squares means were estimated for each group at each position and groups were compared at each position. Pairwise comparisons of means were conducted at each position and P-values for these comparisons were adjusted using the Bonferroni method.
Group differences in SPARCS total score and Pelli–Robson scores were assessed using mixed effects linear regression. Fixed effects were included for group and test. A random subject effect accounted for correlation among measurements from the same subject, while a random eye effect accounted for correlation among repeated measurements from the same eye. Least squares means were estimated by group and groups were compared. Subject-level data were compared using the Wilcoxon rank sum test for continuous variables and Fisher’s exact test for categorical variables.
Test–retest reliability for SPARCS and PR was evaluated using the Intraclass Correlation Coefficient (ICC) and Bland Altman analysis. Intraclass correlations were calculated from mixed effects models that accounted for correlation among eyes from the same subject and repeated measurements from the same eye. Through the Bland Altman analysis, test–retest reliability was evaluated by calculating the mean difference or bias between test and retest scores and the Coefficient of Repeatability (COR).12 The COR is a measure of the 95% limits of agreement, calculated as 1.96 times the SD of the difference between test and retest scores. Smaller ranges show greater agreement between test and retest. CORs were scaled based on the range of the measure (2.25 for PR, 20 for SPARCS region scores, 100 for SPARCS total score)`.
Results
Data were analyzed for 162 eyes from 84 subjects. The control group included 119 eyes from 61 subjects (27 males and 34 females) while the cataract subject group included 43 eyes from 23 subjects (9 males and 14 females). Within the cataract subject group, there were 16 eyes with 1+ nuclear sclerosis, 14 eyes with 2+ nuclear sclerosis, and 13 eyes with 3+ nuclear sclerosis. Analysis revealed statistically significant differences between the cataract group and control group with respect to age (P<0.001), VA (P<0.001), and cylindrical power (P<0.001). Spherical equivalence was noted to not have a statistically significant difference (P=0.072). The average age of subjects in the cataract group (69 years±9 s.d.) was higher than that of subjects in the control group (49 years±17 s.d.). The average VA in logMAR was 0.21 (0.17 s.d.) for the cataract group and 0.00 (0.14 s.d.) for the control group.
The test–retest reliability of SPARCS was acceptable and comparable to that of PR (ICC=0.71 for SPARCS, 0.73 for PR; Mean difference (as % of highest possible score)=−0.83% for SPARCS, −1.17% for PR; COR (as % of highest possible score)=9.58% for SPARCS, 9.28% for PR). Of the 5 SPARCS areas, the central region had the highest test–retest agreement (ICC=0.651). The total SPARCS score had better reproducibility than the individual areas of SPARCS. Among cataract subjects, the COR was ±11.7% for SPARCS and ±11.8% for PR.
Apart from the RLQ SPARCS score for cataract subjects, the mean difference values were negative for all subjects and all scores. Because differences were calculated by subtracting test scores from retest scores, this shows that retest scores were higher than the initial test scores, indicating a possible learning effect. Figure 2, which depicts scatterplots of the test–retest agreement for SPARCS and Pelli–Robson, also shows that results of the retest are higher than the initial test, particularly at the lower end of the measures. Subjects may have higher scores during the retest because they are more accustomed to the test during the second trial.
Scatterplots of the test–retest agreement of SPARCS central scores (a), SPARCS total scores (b), and Pelli–Robson (c). The x axis shows the result from Test 1. The y axis shows the result from Test 2. The blue line represents perfect agreement. The red line represents the least squares fit to the observed data. SPARCS=Spaeth/Richman Contrast Sensitivity Test. A full color version of this figure is available at the Eye journal online.
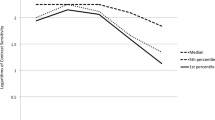
Table 1 shows model-estimated mean scores by cataract group and compares groups with respect to these measures. Cataract subjects scored significantly lower than controls with respect to all SPARCS test areas, the SPARCS total score, and the PR test (P≤0.001). Variability was slightly, but not significantly, greater in cataract patients than controls. Pairwise comparisons revealed significant differences in SPARCS results between 3+ nuclear sclerosis and controls (P<0.001) and 2+ nuclear sclerosis and controls (P<0.001), whereas the PR test showed a significant difference in results only between 3+ nuclear sclerosis and controls (P<0.001) (Table 2). CS decreased with increasing cataract severity (Figure 3). Subjects with 3+ nuclear sclerosis had significantly worse CS than subjects with 1+ nuclear sclerosis when measured by the SPARCS total score (P=0.041) and the PR score (P=0.021).
Boxplots depicting the mean scores for the SPARCS center (a), SPARCS total (b), and Pelli–Robson (c) for the controls and cataract groups. Cataract subjects scored significantly lower than controls (P<0.001). In addition, contrast sensitivity scores decreased with increased cataract severity. Data are shown for 119 control eyes, 16 eyes with 1+ nuclear sclerosis, 14 eyes with 2+ nuclear sclerosis, and 13 eyes with 3+ nuclear sclerosis. SPARCS=Spaeth/Richman Contrast Sensitivity Test.
Discussion
In this study, we compared a newly developed, internet-based test, SPARCS, with the traditionally used Pelli–Robson test in two populations, one with cataract and the other with apparently normal eyes.
We found that SPARCS better detects decreases in CS with worsening cataract severity. While the PR test was only able to detect statistically significant differences in CS between 3+ nuclear sclerosis and controls, the SPARCS test was able to detect a statistically significant reduction in CS for subjects with 2+ or 3+ nuclear sclerosis when compared to controls (Table 2, Figures 3b and c).
In addition, mean CS scores were lower for the cataract subject groups compared with the control group for the SPARCS central and peripheral areas, the SPARCS total, and the PR total scores. These scores declined significantly with increasing nuclear opacity. Therefore, our results confirmed earlier findings that CS is significantly impaired in subjects with cataract13, 14 and that central CS diminishes with worsening cataracts.15, 16 The finding that nuclear cataracts cause a reduction in CS for peripheral vision is a new observation that may be of clinical importance. This further highlights the value of the SPARCS test as it can assess both central and peripheral vision.
The importance of these findings is underscored by the value of contrast sensitivity as a measurement in subjects with cataracts. Although VA is often used as a conventional measurement of vision for these subjects, it is often considered an inadequate assessment.9, 17 In a study by Bernth–Petersen, 20% of the cataract subjects with relatively good VA reported high visual disability.2 This may be due to the fact that Snellen VA only assesses the higher spatial frequency aspect of vision.1 A reduction in low spatial frequency CS may explain the greater functional impairment perceived by these subjects. Low spatial frequency CS can better assess wide-angle scatter, including forward light-scattering, which can be caused by cataracts. It is also better correlated with visual disability than VA.1, 13 Therefore, a low spatial frequency CS test such as SPARCS can supplement a Snellen measurement of VA to provide a more comprehensive evaluation of cataract subjects.
The commonly used Pelli–Robson chart test assesses central CS10 and is quick, reliable, and easy to understand. However, it has disadvantages due to its bulky size, vulnerability to unevenness of illumination, fading of print, and reflections from the surface.3 Subjects performing this test are also required to distinguish letters, which necessitates pattern recognition and cognition. Like the PR test, SPARCS assesses low spatial frequency CS, is easy to perform, and has similar test–retest repeatability. However, SPARCS eliminates potential confounders such as literacy, intelligence, and pattern recognition.
As an internet-based CS test, SPARCS can be accessed in an increasing number of locations worldwide; it does not require specialized software, equipment, or operating procedures. It requires a computer with Internet access, one of several standard web browsers such as Chrome or Firefox, and a ruler to measure the distance between the monitor and the subject. Because it is computer-based, SPARCS does not have the same disadvantages of chart tests such as fading print. SPARCS also has multiple answer choices reducing the probability of guessing correctly. Other CS gratings tests (such as the Vistech and FACT) have few answer choices, decreasing reproducibility and reliability.18 SPARCS tests contrast levels between 100 and 0.45%, ruling out possible ceiling and floor effects. SPARCS has been found to distinguish between glaucoma patients, glaucoma-suspects, and controls and be correlated with the degree of damage to the visual field and optic nerve in these subjects.11 A recent study has found SPARCS to be useful for assessing CS in patients with age-related macular degeneration.19
SPARCS has certain limitations including subject fatigue. A full SPARCS assessment of both eyes typically takes 5-10 min. In this study, fatigue was negligible. If the technician identified subject fatigue, the subject was given rest time and the test was restarted. Another challenge is ensuring that the same amount of contrast is shown for low levels of contrast in a non-standardized testing environment. A gamma function assessment can be performed or noisy bits used to standardize low levels of contrast. However, making this a requirement for SPARCS would counteract the goal of having an easily accessible test. A future study may evaluate the effect of monitor luminance on SPARCS testing.
The significant difference in age between the two groups is a limitation of this study. This may have affected the results, as CS declines with age.20 In addition, the younger group may have had better scores because they were better able to understand the tasks; however, the test is relatively easy to understand and a technician was present to answer questions and ensure that the subject understood throughout testing. The test could also be restarted. The small sample size of the group of cataract subjects is also a limitation. Although an even larger group or more age-matched group would provide stronger data, we feel that the strength of the data offers useful insight that could be developed further in future studies.
The present study isolated subjects with varying degrees of nuclear sclerosis and excluded people with concurrent ocular diseases. In daily clinical practice, subjects often have more than one issue. For example, older subjects often have both cataracts and glaucoma, both of which can cause a decrease in CS. Looking at the SPARCS scores in Table 1 provides a rough idea of the effect of cataract severity on CS. However, care should be taken not to over-interpret these results as the 95% confidence intervals are wide.
The inclusion of pseudophakic subjects in the control group may also have introduced bias. However, Furuskog and Nilsson found no statistically significant difference in mean CS between pseudophakic subjects and age-matched controls.21 Rubin et al22 reported that after cataract surgery, CS improves.
In conclusion, our results represent useful findings with regard to a novel test of CS, an important parameter for visual impairment that has a significant correlation with visual function and quality of life. The SPARCS test should be considered a potential standard tool to assess CS and visual function in cataract subjects, especially those with relatively good VA but poor visual function. Advantages of SPARCS include that it is inexpensive, simple, and easily accessible. It is inherently less biased in terms of a subject’s literacy or ability to recognize letters and tests peripheral as well as central CS. Future studies should focus on the newly developed subject-administered version, which can be used more widely, and implementing this test in different countries and socioeconomic backgrounds.

References
Elliott DB . Evaluating visual function in cataract. Optom Vis Sci 1993; 70: 896–902.
Bernth-Petersen P . Visual functioning in cataract patients. Methods of measuring and results. Acta Ophthalmol (Copenh) 1981; 59: 198–205.
Richman J, Spaeth GL, Wirostko B . Contrast sensitivity basics and a critique of currently available tests. J Cataract Refract Surg 2013; 39: 1100–1106.
Ginsburg AP . Contrast sensitivity and functional vision. Int Ophthalmol Clin 2003; 43: 5–15.
Wood JM . Age and visual impairment decrease driving performance as measured on a closed-road circuit. Hum Factors 2002; 44: 482–494.
West SK, Rubin GS, Broman AT, Munoz B, Bandeen-Roche K, Turano K . How does visual impairment affect performance on tasks of everyday life? The SEE Project. Salisbury Eye Evaluation. Arch Ophthalmol 2002; 120: 774–780.
Owsley C, Sloane ME . Contrast sensitivity, acuity, and the perception of 'real-world' targets. Br J Ophthalmol 1987; 71: 791–796.
Rubin GS, Roche KB, Prasada-Rao P, Fried LP . Visual impairment and disability in older adults. Optom Vis Sci 1994; 71: 750–760.
Chylack LT Jr., Padhye N, Khu PM, Wehner C, Wolfe J, McCarthy D et al. Loss of contrast sensitivity in diabetic patients with LOCS II classified cataracts. Br J Ophthalmol 1993; 77: 7–11.
Pelli D, Robson J . The design of a new letter chart for measuring contrast sensitivity. Clin Vision Sci 1988; 187–199.
Richman J, Zangalli C, Lu L, Wizov SS, Spaeth E, Spaeth GL . The Spaeth/Richman contrast sensitivity test (SPARCS): design, reproducibility and ability to identify patients with glaucoma. Br J Ophthalmol 2015; 99 ((1)): 16–20.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Elliott DB, Hurst MA, Weatherill J . Comparing clinical tests of visual function in cataract with the patient's perceived visual disability. Eye (Lond) 1990; 4: 712–717.
Adamsons I, Rubin GS, Vitale S, Taylor HR, Stark WJ . The effect of early cataracts on glare and contrast sensitivity. A pilot study. Arch Ophthalmol 1992; 110: 1081–1086.
Shandiz JH, Derakhshan A, Daneshyar A, Azimi A, Moghaddam HO, Yekta AA et al. Effect of cataract type and severity on visual acuity and contrast sensitivity. J Ophthalmic Vis Res 2011; 6: 26–31.
Cheng Y, Shi X, Cao XG, Li XX, Bao YZ . Correlation between contrast sensitivity and the lens opacities classification system III in age-related nuclear and cortical cataracts. Chin Med J (Engl) 2013; 126: 1430–1435.
Elliott DB, Situ P . Visual acuity versus letter contrast sensitivity in early cataract. Vision Res 1998; 38: 2047–2052.
Pesudovs K, Hazel CA, Doran RM, Elliott DB . The usefulness of Vistech and FACT contrast sensitivity charts for cataract and refractive surgery outcomes research. Br J Ophthalmol 2004; 88: 11–16.
Faria BM, Duman F, Zheng CX, Waisbourd M, Gupta L, Ali M et al. Evaluating contrast sensitivity in age-related macular degeneration using a novel computer-based test, the Spaeth/Richman Contrast Sensitivity test. Retina 2015; 35 ((7)): 1465–1473.
Rubin GS, West SK, Munoz B, Bandeen-Roche K, Zeger S, Schein O et al. A comprehensive assessment of visual impairment in a population of older Americans. The SEE Study. Salisbury Eye Evaluation Project. Invest Ophthalmol Vis Sci 1997; 38: 557–568.
Furuskog P, Nilsson BY . Contrast sensitivity in patients with posterior chamber intraocular lens implants. Acta Ophthalmol (Copenh) 1988; 66: 438–444.
Rubin GS, Adamsons IA, Stark WJ . Comparison of acuity, contrast sensitivity, and disability glare before and after cataract surgery. Arch Ophthalmol 1993; 111: 56–61.
Acknowledgements
We thank Dr Ben Leiby, PhD for contributing to statistical analysis and Dr Michael Waisbourd, MD for his support in manuscript editing and preparation. Commercial Relationships Disclosure: George Spaeth: Consultant for Allergan and Merck. Financial support from Allergan and Merck. Financial support was provided by Pfizer, New York, NY, USA (Grant # WS698663). Glaucoma Service Foundation to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
George Spaeth, Eric Spaeth, and Jesse Richman developed and patented the Spaeth/Richman Contrast Sensitivity test (SPARCS). Eric Spaeth, Patent # 8.042,946; Jesse Richman, MD, Patent # 8.042,946; George L Spaeth, MD, Patent # 8.042,946.
Additional information
This study was presented as a poster at the Association for Research in Vision and Ophthalmology in Orlando, FL, USA on May 4, 2014.
Rights and permissions
About this article
Cite this article
Gupta, L., Cvintal, V., Delvadia, R. et al. SPARCS and Pelli–Robson contrast sensitivity testing in normal controls and patients with cataract. Eye 31, 753–761 (2017). https://doi.org/10.1038/eye.2016.319
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.319
This article is cited by
-
Test-retest repeatability and agreement of the quantitative contrast sensitivity function test: towards the validation of a new clinical endpoint
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Analysing the change in contrast sensitivity post-travoprost treatment in primary open-angle glaucoma patients using Spaeth Richman contrast sensitivity test
International Ophthalmology (2022)
-
Lighting conditions and perceived visual function in ophthalmic conditions
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
The effect of reduced contrast sensitivity on colour vision testing
Eye (2019)
-
Establishment of a normative database and evaluation of the test-retest repeatability of the Spaeth/Richman contrast sensitivity test
Japanese Journal of Ophthalmology (2019)