Abstract
Background
The use of adjunct antimetabolite therapy along with conjunctiva autograft has been shown to be effective in preventing pterygium recurrence. There has however been fewer reports on the effect of anti-vascular endothelial growth factor on pterygium recurrence.
Objective
To compare 5-fluorouracil with conjunctival autograft with bevacizumab (avastin) used along with autograft in the surgical treatment of pterygium.
Methods
A randomized controlled prospective study of outcome of pterygium treatment using 5-fluorouracil with conjunctiva autograft as adjuvant treatment compared avastin with conjunctiva autograft.
Results
A total of 70 eyes of 70 patients were recruited into the study with a mean age of 51.49 (±14.36) years. Thirty-five patients each were randomized into the 5-fluorouracil treatment group and into the avastin treatment group respectively. The mean follow-up was 18.35 months (18.44 for the 5-FU and 18.26 for the avastin group). Post operative, pterygium recurrence was observed in 1/27 (3.7%) eyes treated with 5-fluorouracil and 1/26 (3.9%) eyes of the avastin group. Both recurrences were observed at 1 year of follow-up and they were both female patients aged 46 and 52 years, respectively.
Conclusions
Both 5-fluorouracil and avastin are comparably effective as adjunct to conjunctival autograft. However, cost, availability, and convenience are other considerations with use of avastin.
Similar content being viewed by others
Introduction
Pterygium is an ocular surface degenerative lesion presenting as awing shaped fibrovascular conjunctival growth. It is located at the interpalpebral region of the conjunctiva, mostly nasal and extends unto the cornea. Its prevalence has been reported to range from 0.3 to 29% and mainly found in the tropical region.1, 2 The aetiopathogenesis of pterygium is not definite but various theories have been postulated. Exposure to ultraviolet light (mainly UVB) has been identified as a major risk factor for the development of pterygium.1, 3 Other risk factors include chronic irritation from dust and wind.3 An individual with pterygium may present with visual disturbance due to its induction of astigmatism or by its growth extending on the cornea to occlude the visual axis. It may also cause ocular irritation and recurrent inflammation as well as being unsightly, cosmetically.
Conservative treatment using topical eye medications can be employed as a temporal relief measure for mild symptoms, such as foreign body sensation and inflammation. They include artificial tears, eye ointments for foreign body sensation and anti-inflammatory eye-drops for inflamed pterygia. The main stay of treatment of pterygium, however, is by surgical excision. In 1948, the bare sclera surgical technique was first fully described by D’Ombrain4 and this became the classical standard of treatment for many years. The aim of this technique is to ensure the complete removal of the head, neck, and body of the pterygium. This bare sclera technique has been plagued with a high-reported rate of recurrence; rates of up to 90% have been reported.5 In a bid to reduce the rate of recurrence, numerous adjunctive therapies have been developed especially over the last few decades.
Adjuvant treatment modalities are numerous in the present day surgical management of pterygium. Adjuvant surgical technique being employed in a bit to reduce recurrence include; lamellar keratoplasty, amniotic membrane transplantation, and conjunctival autograft.6, 7 The lamellar keratoplasty is mainly indicated for recurrent pterygia with a scarred or thin cornea tissue. The conjunctival autograft treatment option is relatively popular and can be applied over the bare sclera either by a primary direct closure, a free conjunctival autograft8 or by a sliding conjunctival flap.9 Other adjuvant modalities include radiation therapy using beta-irradiation post-operatively, which is relatively safe, effective, and a satisfactory reduction of recurrence rate has been reported.10, 11 Chemotherapy agents such as antimetabolite are also commonly used as adjuvant therapy; such as mitomycin C (MMC) and 5-fluorouracil (5-FU). These two antimetabolite are mainly applied over the bare sclera intraoperative, but can also be used as a preoperative intra-lesion injection or as a post-operative eye drop. The MMC has a stronger anti-proliferative effect owing to its action on both fibroblasts and vascular endothelial cell as against 5-FU which effect is mainly on the fibroblasts.12 Alhough there is a significant reduction in the recurrence rate following these adjuvant therapies used separately or sometimes in combination, side effects from these treatment do occur. They include; punctate epitheliopathy, elevated intraocular pressure, and delayed onset sclera melting. These side effects has encouraged search for other safer modalities.
The use of alcohol (ethanol) and anti-vascular endothelial growth factors (anti-VEGF) has been recently introduced. Ethanol causes the denaturation of cytokines, growth factors, and enzymes involve in pterygium formation. A study comparing the use of ethanol and low-dose MMC as adjuvant therapy reported a lesser rate of recurrence and fewer post-operative complications in the ethanol group.13 The use of anti-VEGF has been encouraged by the demonstration of higher concentration of VEGF in pterygium tissue as compared with normal conjunctiva.14 Bevacizumab (avastin; Genentech Inc., San Francisco, CA, USA), an anti-VEGF, is a recombinant humanized murine monoclonal immunoglobulin G1. It inhibits the VEGF-A isoform, the main stimulant of angiogenesis. It is commonly used as an adjuvant for many neoplasms such as brain, lung, ovary, and breast cancers.15, 16, 17, 18 It recently got approval by the Food and Drug Administration of the United State of America for intraocular use and its been used extensively for posterior segment vascular diseases and for corneal neovascularisation.19, 20, 21, 22 A randomized clinical trial reported the use of subconjunctival bevacizumab injection in conjunction with primary surgery and conjunctival autograft to be safe, well-tolerated, and capable of preventing recurrence when compared with the control.23 Another randomized trial showed no statistically significant difference between the bevacizumab group and control, although recurrence rate was halved in the former.24
The purpose of this study is to compare 5-FU with conjunctival autograft and bevacizumab (avastin) used along with autograft in the surgical treatment of pterygium.
Materials and methods
Study site
The study was carried out at the Department of Ophthalmology, University of Ibadan/University College Hospital, Ibadan, between October 2009 and December 2013.
Design
A randomized controlled and prospective study of outcome of pterygium treatment using 5-FU with conjunctiva autograft as adjuvant treatment compared with bevacizumab with conjunctiva autograft.
Ethical clearance
ethical clearance was obtained from the institutional ethical committee of the UI/UCH.
Selection of patients (inclusion/exclusion criteria)
The full procedure for selection and recruitment of patients for the study has been described elsewhere25 but in brief, all patients seen with pterygium encroaching 2 mm or more into cornea (from the limbus) were selected and randomized into one of the two groups. Pterygia of size <2 mm into cornea as well as recurrent pterygium from previous surgery were excluded.
Sample size was calculated from estimation of proportions with assumption of success rate of about 80%26 for 5-FU with autograft and expected success rate of 100% for bevacizumab with conjunctival autograft, alpha error, 0.05% and a power of 90%.

Following adequate explanation and obtaining of consent, the subjects were randomized into their respective groups using a ‘lucky dip’ technique. Small-folded sheets of paper numbered 1–35 and 36–70 were kept in two separate envelopes (for male and female, respectively). Male and female patients who met the selection criteria were requested to pick one-folded sheet of paper from the appropriate envelope as they presented consecutively to the clinic. Those who picked odd numbers were assigned to the 5-FU with conjunctiva autograph group, whereas even numbers were assigned to the bevacizumab with conjunctiva autograph group. For any patient with bilateral pterygia, the worse eye was randomized and the other eye excluded from the study. Information obtained from subjects using a structured questionnaire included age, sex, occupation, eye affected, location, morphology, size of pterygium from limbus (measured with a slit lamp), vision of eye to be operated, and information on previous pterygium surgery done.
All patients received subconjunctival 2% lignocaine with adrenaline, for local anaesthesia. Pterygium tissue was excised from the cornea with Bard-Parker blade under microscope with subsequently bluntly dissected from over lying conjunctiva and underlying sclera. The Tenon was then gently excised without damage to the rectus muscle. The use of cautery was minimized.
5-FU with conjunctiva autograph group
The 5-FU group after an initial pterygium excision had the bare scleral area of the pterygium bed exposed to a section of a Weck-cel sponge soaked in 50 mg/ml of 5-FU for 5 min during which there was intermittent wetting of the sponge every minute with a drop of 5-FU, at the end of 5 min, the sponge was be removed and discarded and the eye copiously irrigated with 40–50 mls normal saline solution for about 1–2 min. A conjunctiva-free graft of a size equivalent to the scleral defect was excised from the pterygium-free superior 12:00 hours bulbar conjunctiva inclusive of limbal conjunctiva and 0.5 mm of clear cornea of the same eye. Thereafter the free graft was sutured to the recipient bed with 4–8 interrupted 8-0 vycril sutures taking care to ensure proper orientation of the ends of the graft (cornea end of the graft sutured to the recipient cornea).
Bevacizumab with conjunctiva graft procedure
This group had the bare scleral area of the pterygium bed covered with conjunctiva-free graft of a size equivalent to the scleral defect excised from the pterygium-free superior 12:00 hours bulbar conjunctiva inclusive of limbal conjunctiva and 0.5 mm of clear cornea of the same eye. The free graft was sutured to the recipient bed with 4–8 interrupted 8-0 vycril sutures taking care to ensure proper orientation of the ends of the graft (cornea end of the graft sutured to the recipient cornea). Thereafter a 0.05 ml of 0.5 mg bevacizumab subconjunctival injection was given adjacent to the graft.
Post operative, both groups had instillation of antibiotic ointment and dexamethasone (steroid) drops post-operatively for between 8 and 10 weeks, depending on duration of inflammation. Follow-up visits were at post-operative days 1, 7, and 21, monthly for 2 months and every 3 months for between 1 and 2 years.
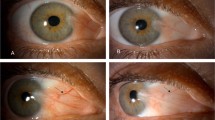
Recurrence of pterygium was defined as growth of fibrovascular tissue 1 mm or more into cornea as observed with a slit lamp.
Data analysis
All information was collected with the aid of a structured questionnaire and entered into a computer and analysed using Statistical Package for Social Sciences (IBM) for Windows, Version 19.0, IBM Corp (Armonk, NY, USA).
Seventeen (24.6%) of the patients comprising eight from 5-FU group and nine from the avastin group were lost to follow-up before the end of the study at 2 years and were excluded from the final analysis.
Results
A total of 70 eyes of 70 patients were recruited into the study with a mean age of 51.49 (±14.36) years. Thirty-five of the patients each were randomized into the 5-FU treatment group and avastin treatment group, respectively. Table 1 show the age and gender distribution in the two groups. There was no statistical difference between the mean ages of the two groups.
In both groups >80% were nasal in location and >90% were large and fleshy in morphology as depicted in Table 2. The mean size in length of the pterygia for the 5-FU treatment group was 3.94 mm and for the avastin treatment group was 3.36 mm. There was no statistically difference between the two groups with a P-value of 0.11.
The mean follow-up was 18.35 months (18.44 for the 5-FU and 18.26 for the avastin group, respectively). Twenty-seven of the 5-FU and 26 of the avastin patients were followed up to 2 years. Post-operatively pterygium recurrence was observed in 1/27 (3.7%) eyes treated with 5-FU and 1/26 (3.9%) eye of the avastin group with a P-value of 0.32. Both recurrences were observed at 1 year of follow-up and they were both female patients aged 46 and 52 years, respectively. They were also both of the fleshy morphologic type. In this study complications such as granuloma formation, surface infection or sclera necrosis were not observed. A total of 17 (eight of the 5-FU and nine of the avastin groups) were not analysed for recurrence because they were loss to follow-up in <1 year after surgery. Eleven of the 17 patients (64.7%) lost to follow-up were seen for at least 6 month post surgery.
Discussion
This study has observed the same successful rate of treatment (>96%) for the two groups which when compared, the rate of recurrence of pterygium in the avastin group of 3.9% is far less to a study conducted by Mohammad-Reza et al24 which was 18.18%. In their study pterygium excision with conjunctiva autograft was also the baseline surgery with subsequent randomization into two groups of either bevacizumab subconjunctival injection or balance salt solution (BSS) injection intraoperatively. The rate of recurrence in the bevacizumab group was half that of the BSS group in their study, but this failed to reach statistically significant difference. Another study by Nava-Castaneda et al23 reported no recurrence in the two groups that had subconjunctival bevacizumab injections after a 1 year follow-up period with recurrence only in the third group which had no injection given. This difference was statistically significant and they concluded that a single 2.5 mg/ml subconjunctival bevacizumab injection in conjunction with primary pterygium surgery accomplishing a conjunctival autograft procedure was safe, well-tolerated, and capable of preventing pterygium recurrences. Unlike the two studies mentioned above, our study compared bevacizumab and 5-FU with both having a baseline of pterygium excision with conjunctival autograft. The result showed a near 100% recurrence free rate in both studies comparable to the bevacizumab group of Nava-Castaneda et al23 study, though they used 2.5 mg/ml bevacizumab injection while we used 0.5 mg/ml bevacizumab injection.
This study also re-emphasized that combination of adjunct therapy is better than single adjunct therapy in reducing the rate of recurrence of pterygium. An earlier study by Bekibele et al25 reported a success rate of bare sclera technique with intraoperative 5-FU group as 88.6% and conjunctival autograft group as 87.9%, respectively. A latter study which compared 5-FU with Mitomycin C as adjunct to conjunctival autograft also by Bekibele et al27 reported recurrence rates of 8.7 and 11.8%, respectively. Whereas this current study which compared 5-FU and bevacizumab as adjuncts to conjunctival autograft reported a much higher success rate in preventing recurrence. 5-FU is relatively cheap and readily available while bevacizumab is more expensive and comes in higher concentrations that require dilution to desired concentrations with the possible risk of contamination and altered dosage. This, therefore, is the advantage 5-FU has over avastin in the management of pterygium in resource scarce settings.
A limitation of this study was that 17 (24.3%) of the subjects were lost to follow-up before the end of the study and were therefore not available for inclusion in the analysis of recurrence, their presence may have altered the success rate, however, they were evenly distributed between the groups and therefore not likely to bias the group comparison.
In conclusion, a single subconjunctival injection of 0.5 mg/ml bevacizumab intraoperatively with conjunctival autograft and 5-FU intraoperative use with conjunctival autograft have a very high success rate of prevention of pterygium recurrence close to 100%. Cost, convenience, and availability considered 5-FU would appear to have an advantage over bevacizumab. More studies are, however, needed to further explore the different effects between these drugs in preventing pterygium recurrence.

References
Moran DJ, Hollows FC . Pterygium and ultraviolet radiation: a positive correlation. Br J Ophthalmol 1984; 68: 343–346.
Taylor HR, West S, Munoz B . The long-term effects of visible light on the eye. Arch Ophthalmol 1992; 110: 99–104.
Cameron ME . Pterygium throughout the world. Charles C. Thomas: Springfield, Illinois, USA, 1965.
D’ Ombrain A . The surgical treatment of pterygium. Br J Ophthalmol 1948; 32: 65–71.
Youngson RM . Recurrence of pterygium after excision. Br J Ophthalmol 1972; 56: 120–125.
Kutbaab A, Ardekani HA, Khoshniyat H, Hosseini HJ . Amniotic membrane transplantation for primary pterygium surgery. J Ophthalmic Vis Res 2008; 3 (1): 23–27.
Figueira EC, Coroneo MT, Francis IC . Preventing conjunctival autograft inversion in pterygium surgery. Br J Ophthalmol 2007; 91: 83–84.
Kenyon KR, Wagoner MD, Hettinger ME . Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology 1985; 92: 1461–1470.
McCoombes JA, Hirst LW, Isbell GP . Sliding conjunctival flap for the treatment of primary pterygium. Ophthalmology 1994; 101: 169–173.
Ajayi BG, Bekibele CO . Evaluation of the effectiveness of postoperative beta irradiation in the management of pterygium. Afr J Med Med Sci 2002; 31: 9–11.
Jurgenliemk-Schulz IM, Hartman IJ, Roesink JM, Tersteeg RJ, Van der Tweel I, Kal HB et al. Prevention of pterygium recurrence by postoperative single dose beta irradiation: A prospective randomized clinical double blind trial. Int J Radiat Oncol Biol Phys 2004; 59: 1138–1147.
Smith S, D’Amore PA, Dreyer EB . Comparative toxicity of mitomycin C and 5-fluorouracil in vitro. Am J Ophthalmol 1994; 118: 332–337.
Chen KH, Hsu WM . Intraoperative ethanol treatment as an adjuvant therapy of pterygium excision. Int J Biomed Sci 2006; 2: 414–421.
Detorakis ET, Zaravinos A, Spandidos DA . Growth factor expression in ophthalmic pterygia and normal conjunctiva. Int J Mol Med 2010; 25: 513–516.
Lai A, Tran A, Nghiemphu PL, Pope WB, Solis OE, Selch M et al. Phase II study of bevacizumab plus temozolomide during and after radiation therapy for patients with newly diagnosed glioblastoma multiforme. J Clin Oncol 2011; 29: 142–148.
Stinchcombe TE, Socinski MA . Maintenance therapy in advanced non-small cell lung cancer: current status and future implications. J Thorac Oncol 2011; 6: 174–182.
Barrena Medel NI, Herzog TJ, Wright JD, Lewin SN . Neoadjuvant bevacizumab in a granulosa cell tumor of the ovary: a case report. Anticancer Res 2010; 30: 4767–4768.
Fojo T, Wilkerson J . Bevacizumab and breast cancer: the E2100 outlier. Lancet Oncol 2010; 11: 1117–1119.
Waisbourd M, Goldstein M, Loewenstein A . Treatment of diabetic retinopathy with anti-VEGF drugs. Acta Ophthalmol 2011; 89: 203–207.
Figueroa MS, Contreras I, Noval S, Arruabarrena C . Results of bevacizumab as the primary treatment for retinal vein occlusions. Br J Ophthalmol 2010; 94: 1052–1056.
Schouten JS, La Heij EC, Webers CA, Lundqvist IJ, Hendrikse F . A systematic review on the effect of bevacizumab in exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2009; 247: 1.
Habot-Wilner Z, Barequet IS, Ivanir Y, Moisseiev J, Rosner M . The inhibitory effect of different concentrations of topical bevacizumab on corneal neovascularization. Acta Ophthalmol 2010; 88: 862–867.
Nava-Castañeda A, Olvera-Morales O, Ramos-Castellon C, Garnica-Hayashi L, Garfias Y . Randomized, controlled trial of conjunctival autografting combined with subconjunctival bevacizumab for primary pterygium treatment: 1-year follow-up. Clin Experiment Ophthalmol 2014; 42: 235–241.
Mohammad-Reza R, Mohammad B . Subconjunctival bevacizumab for primary pterygium excision, a randomized clinical trial. J Ophthalmic Vis Res 2014; 9 (1): 22–30.
Bekibele CO, Baiyeroju AM, Olusanya BA, Ashaye AO, Oluleye TS . Pterygium treatment using 5-FU as adjunct treatment compared to conjunctiva autograft. Eye 2008; 22: 31–34.
Kareem AA, Farhood QK, Alhammami HA . The use of antimetabolites as adjunctive therapy in the surgical treatment of pterygium. Clin Ophthalmol 2012; 6: 1849–1854.
Bekibele CO, Ashaye A, Olusanya B, Baiyeroju AM, Fasina O, Ibrahim AO et al. 5-Fluorouracil versus mitomycin C as adjunct to conjunctival autograft in preventing pterygium recurrence. Int Ophthalmol 2012; 32 (1): 3–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bekibele, C., Sarimiye, T., Ogundipe, A. et al. 5-Fluorouracil vs avastin as adjunct to conjunctival autograft in the surgical treatment of pterygium. Eye 30, 515–521 (2016). https://doi.org/10.1038/eye.2016.29
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.29
This article is cited by
-
Effect of multiple subconjunctival conbercept injections as an adjuvant to the surgical treatment of pterygium: a prospective randomised comparative 6-month follow-up study
Eye (2020)
-
Anti-fibrotic, anti-VEGF or radiotherapy treatments as adjuvants for pterygium excision: a systematic review and network meta-analysis
BMC Ophthalmology (2017)