Abstract
Purpose
The purpose of the study was to provide contemporary estimates for diabetic retinopathy (DR) prevalence in a well-defined UK cohort of patients with type 1 diabetes (T1DM) and investigate potential risk factors for proliferative diabetic retinopathy (PDR) and diabetic maculopathy.
Patients and Methods
Four hundred and sixty four T1DM patients in North Hampshire had T1DM duration, demographic and systemic risk factor data evaluated retrospectively alongside their DR status in 2010 using logistic regression analysis.
Results
Overall prevalence of any retinopathy, PDR, and maculopathy was 71.5%, 6.5%, and 10.8%, respectively. PDR and maculopathy prevalence were 0 and 0.7% for <10 years T1DM duration. PDR prevalence was 4%, 8%, and 16% for 10–19.9 years, 20–29.9, years and ≥30 years duration, respectively. Maculopathy prevalence was 15.6%, 18%, and 11% for 10–19.9 years, 20–29.9 years, and ≥30 years duration, respectively. In univariate analysis, PDR was associated with T1DM duration (odds ratio (OR) 1.07/year), age (OR 1.03/year), systolic blood pressure (OR 1.03/mmHg), and antihypertensive therapy (OR 10.63), while maculopathy was associated with duration (OR 1.03/year) and statin therapy (OR 2.83). In multivariate analysis, disease duration (OR 1.07/year) and antihypertensive therapy (OR 6.87) remained significantly associated with PDR, and maculopathy with statin therapy (OR 2.27).
Conclusion
This study confirms T1DM duration is a strong risk factor for sight-threatening DR. Maculopathy and PDR prevalence within 10 years of T1DM diagnosis is very low. PDR prevalence at 10–20 years was 4% and then doubled for every 10-year interval thereafter up to 16% with ≥30 years duration. Antihypertensive therapy and statin therapy were strongly associated with PDR and maculopathy, respectively.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is an important complication of diabetes and the second most common cause of certifiable blindness in the working age population.1 It is thought to develop following compromise of the retinal microvascular circulation and can ultimately threaten sight. Early detection through screening can help preserve vision.
The works of Klein et al2, 3 published in 1984 gave some of the first estimates for prevalence and natural progression of DR in a large screening population. Their study population were individuals diagnosed with diabetes in Wisconsin USA who were involved in their innovative screening programme. Patients were divided into those under 30 years of age at diagnosis of diabetes and on insulin (group 1) and those over 30 years of age at diagnosis either on insulin or on tablet treatment (group 2). Group 1 is likely to be predominantly, but perhaps not exclusively, type 1 diabetes mellitus (T1DM). The overall prevalence for DR and proliferative diabetic retinopathy (PDR) in group 1 were 70.7% and 25.7%, respectively. Disease duration was identified as a significant risk factor for severe disease with rates of PDR increasing from 1.2% in patients with T1DM for <10 years to 67% in those diagnosed with diabetes for 35 years or more.2
Although the treatment of diabetes has changed significantly since these seminal papers, current prevalence studies for DR in T1DM alone are scarce. There is a particular paucity of data from the UK in global systematic reviews.4, 5 In 2002, Younis et al6 published the first major UK study of DR prevalence in T1DM individuals at entry into a retinal screening programme. In 2015, Thomas et al7 also reported the prevalence of DR in a large community-based screening programme. While their studies also found a strong association between duration of disease and severe DR, the relationship between diabetes duration with diabetic maculopathy and PDR specifically were not investigated. Moreover data on modifiable systemic risk factors were not included.
This study aims to provide a contemporary estimate of the prevalence of DR of all grades, in a UK cohort of T1DM Caucasian patients using data collected by the Southampton Diabetic Eye Screening Programme. Rather than making any assumptions based on age at diagnosis, these patients were diagnosed with T1DM by a consultant diabetologist.8 A further aim of this study was to investigate the associations between PDR and maculopathy with potential risk factors: age, gender, duration of disease, blood pressure, cholesterol, urine albumin to creatinine ratio (ACR), glycaemic control, and smoking history.
Materials and methods
Study population
The Winchester Cohort comprises 750 Caucasian patients with T1DM of both sexes and all ages who attended regional secondary care diabetes clinics between 1983 and 2010. This represented 90–95% of all people with T1DM from 12 local postcodes. The full epidemiology of the Winchester Cohort has been described elsewhere.8 The clinical diagnosis of T1DM was made by consultant physicians specialising in diabetes. Clinical data were recorded on the secondary-care diabetes clinic database at each clinic visit. The Southampton Diabetic Eye Screening Programme (DESP) comprises of ~43 000 patients and covers the cohort in this study. It is part of the NHS DESP9 and therefore holds information regarding the DR status of these individuals either from screening visits or annual information provided from hospital eye units for those patients under hospital care for DR. Data including DR status and visual acuity were collected from the Southampton Diabetic Eye Screening service for patients from the Winchester Cohort between 1 January 2010 and 31 December 2010.
Methods
Best corrected visual acuity was measured using Bailey–Lovie LogMAR charts. Following mydriasis secondary to instillation of G. tropicamide 1%, two digital photographs of each eye were taken, one centred on the macula and one centred on the optic disc. The screening episodes including images are uploaded daily onto the screening software database (Optomize, EMIS Health, Leeds, UK) and graded. The average visual acuity of both eyes was calculated. Contemporaneous data on blood pressure, %HbA1c, urine ACR, total serum cholesterol, smoking history (previous or current), and antihypertensive or statin use were identified for the Winchester T1DM cohort from the secondary-care diabetes clinic database.
Grading
Grading of retinal photographs was performed according to the NHS DESP grading system.10 The diabetic retinopathy (R) and maculopathy (M) grading used by the DESP is based on a simplified version of the Early Treatment of Diabetic Retinopathy Study (ETDRS) clinical classification.11 ‘R0’ denotes no DR (ETDRS 10), ‘R1’ background DR (ETDRS 20–35), ‘R2’ pre-proliferative DR (ETDRS 43–53), and ‘R3’ proliferative DR (ETDRS ≥61). The absence or presence of referable maculopathy is denoted by ‘M0’ or ‘M1’, respectively. Grading was based on non-stereoscopic colour photographs, M1 grading indicating the presence of hard exudates within 1 disc diameter of the fovea and/or microaneurysms within 1 disc diameter of the fovea with a visual acuity of 0.3 LogMAR (6/12) or worse. M1 is therefore not necessarily always equivalent to oedema although these are surrogate markers suggestive of the presence of central macular oedema.
Grading is performed either by trained and accredited graders or ophthalmologists specialising in medical retina. Grading outcomes are recorded on the Optomize software database (Optomize, EMIS Health). Patients who are referred to hospital eye units are required to feed back the retinopathy (R and M) grades of each eye on at least an annual basis and this is recorded on Optomize. If this data is not provided, the patient is recalled to screening.
Where different levels of disease were present between two eyes from the same patient, those readings from the more severely affected eye were taken as the overall grade to enable analysis.
Statistics
The prevalence of retinopathy and maculopathy was calculated with 95% confidence intervals (CI). Associations between PDR (R3) and maculopathy (M1) with patient age, gender, duration of diabetes, systolic blood pressure, %HbA1c, urine ACR, serum cholesterol, smoking history, antihypertensive, and statin use were analysed using univariate logistic regression. Patient age, gender, and other factors showing a significant association with R3 or M1 were then incorporated into a multivariate logistic regression model. Adjusted odds ratios (OR) with 95% CI’s were calculated. Complete data were available for DR grade, patient age, gender, duration of diabetes, and visual acuity. Where some data were missing for other risk factors we used imputation to enable statistical analysis. All tests were two-sided and P<0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (Armonk, New York, NY, USA) and performed in conjunction with a statistician.
Results
Patient demographics and clinical characteristics
From the Winchester T1DM Cohort, 464 attended for DR screening in Southampton or had data recorded from the hospital eye units between January 2010 and December 2010. The baseline demographics and potential risk factor data for DR in T1DM are shown in Table 1.
The prevalence (95% CI’s) of any DR, PDR alone (R3), significant maculopathy alone (M1), or referable retinopathy (M1 or R3, or R2) for the whole cohort, as well as subdivided by disease duration, can be seen in Table 2. All patients with maculopathy concurrently had some degree of retinopathy (R1-R3).
Diabetes duration, age, and gender
Proliferative diabetic retinopathy
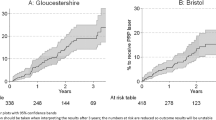
Increased duration of T1DM and older age, but not gender, were associated with PDR in univariate analysis (Table 3). Multivariate analysis however showed only diabetes duration to be a significantly associated risk factor for PDR. While no patients diagnosed with diabetes for <10 years had PDR, 4.1% of those with 10–19.9 years diabetes duration had PDR and this proportion doubled with every additional 10 years up to 15.7% for patients diagnosed with diabetes ≥30 years ago (Figure 1, Table 2). This was equivalent to an adjusted OR of 2.06 (95% CI 1.43–3.00; P<0.001) per 10 years of diabetes duration.
Diabetic maculopathy
Duration of T1DM was significantly associated with maculopathy in univariate analysis, however this did not remain significant in multivariate analysis (Table 3). Age and gender were not associated with maculopathy. The overall prevalence of referable maculopathy (M1) at screening was 10.8%. Only one patient with T1DM duration <10 years had M1. The prevalence of maculopathy rose to 15.6% by 10–19.9 years duration, increased further to 18.3% by 10–29.9 years, then declined to 11.3% for duration more than 30 years (Figure 1, Table 2).
Visual acuity
The average visual acuity was 0.1 LogMAR. Visual acuity slightly deteriorated with increasing duration of T1DM (Table 2) although this was not statistically significant. About 98.3% of all patients had visual acuity equal to or better than 0.3 LogMAR (6/12 Snellen) in their better-seeing eye.
Potential systemic risk factors
Proliferative diabetic retinopathy
Univariate analysis showed significant associations between PDR and systolic blood pressure and those on antihypertensive medication. There was no significant correlation between %HbA1c, urine ACR ratio, serum cholesterol, statin use, or smoking history (Table 3). In multivariate analysis, only antihypertensive medication use remained significantly associated with PDR.
PDR was also significantly associated with patients for whom data on antihypertensive medication were missing due to missed diabetic clinic appointments, both in univariate and multivariate analysis (n=81, OR 7.08, 95% CI 2.52–19.88; P<0.001).
Diabetic maculopathy
Of all the systemic risk factors investigated, only statin use was associated with diabetic maculopathy. This remained significant in both univariate and multivariate analysis (Table 3).
Discussion
This study provides prevalence rates for DR and maculopathy in a well-defined cohort of Caucasian T1DM patients, as graded by UK national screening programme criteria. Furthermore, this study also includes data on systemic modifiable risk factors and their correlation to DR. The overall prevalence in 2010 for any retinopathy, PDR, and maculopathy was 71.5%, 6.5%, and 10.8%, respectively. The average visual acuity remained good at all durations of T1DM and more than 98% of patients had visual acuity equal to or better than 0.3 LogMAR in their better-seeing eye. 0.3 LogMAR approximates to the legal visual acuity requirement for holding a UK driving license.
Prevalence estimates for DR vary considerably, ranging from 36.5 to 93.6% for any DR in Europe and the USA.12 A recent meta-analysis estimated the global prevalence of any DR and PDR in T1DM to be 77.3% and 32.4%, respectively.4 Overall, the prevalence of DR in our cohort was lower than the global average and closer to that found by previous UK studies (Table 4). A landmark UK report of DR prevalence was the Liverpool Diabetic Eye Study in 2002.6 For 831 T1DM patients, the baseline prevalence of any retinopathy, PDR and sight-threatening maculopathy was 45.7%, 3.7%, and 12.3%, respectively. More recently, Thomas et al7 investigated the prevalence of DR in 5003 T1DM patients at first screening in Wales. The prevalence of any retinopathy, PDR, and maculopathy was 56.2%, 2.6%, and 4.2%, respectively. The mean durations of disease for their studies were shorter than ours, which may partly account for the higher DR prevalence observed in our cohort. Furthermore, our sample differed by the inclusion of patients with referable disease under hospital eye services as well as those under the screening service, giving a truer picture of overall prevalence.
Consistent with previous studies, we found duration of diabetes to be strongly associated with PDR. Although univariate analysis showed both age and disease duration to be correlated with PDR, only disease duration remained significant in multivariate analysis. This implies that age in itself is not a risk factor. We also investigated the natural histories of PDR and maculopathy separately. The prevalence of both PDR and maculopathy was rare in the first 10 years of disease and subsequently increased. However, while PDR doubled in prevalence with every additional 10 years duration up to 15.7% for ≥30 years of T1DM, maculopathy prevalence rose to 15.6% for 10–19.9 years duration and remained relatively stable thereafter. This may explain why the correlation between disease duration and maculopathy did not remain statistically significant in multivariate analysis. It is also important to note that all patients with maculopathy also had some concurrent degree of retinopathy. Therefore while not completely independent of one another, these two forms of more advanced DR appear to have distinct natural histories.
A secondary aim of this study was to investigate associations between PDR and diabetic maculopathy with putative modifiable risk factors. Smoking history was not associated with severe DR, as previously shown by others.13, 14 Gender was also not associated, in keeping with a recent global meta-analysis, which found similar rates of DR in males and females.4 Although we did not find associations between DR with urine ACR and HbA1c, several other studies have shown these to be risk factors for DR.12 It is possible that our study may have been underpowered to detect these associations, that spot readings might not adequately reflect long-term control, or that they may be more strongly linked to DR progression than prevalence.15
The use of antihypertensive medications was significantly associated with PDR but not diabetic maculopathy. PDR and systolic blood pressure were significantly associated in univariate analysis, although this did not remain significant in multivariate analysis. Antihypertensive medication may more accurately represent hypertension status and suggests treated hypertension is still a significant risk factor for PDR. It is interesting that those patients for whom blood pressure readings were unavailable, due to missed appointments, had a significant higher prevalence of PDR. This small group of patients were likely to be poor attenders to medical follow-up and therefore at greater risk of suboptimal diabetes control. A number of previous epidemiological studies have identified hypertension as a risk factor for DR.4, 12 The evidence for treating hypertension to reduce DR risk is weaker however and unlike hyperglycaemia, any beneficial effect appears to diminish quickly after cessation of intensive treatment.16 A recent Cochrane review found no reduction in risk of DR progression with intensive blood pressure control, although there was a modest reduction in incidence.17
We found no correlation between total cholesterol levels and DR. However we did find the use of statins, implying a clinical diagnosis of hypercholesterolaemia, to be associated with diabetic maculopathy. Previous reports of dyslipidaemia in diabetes have not consistently identified a single lipid measure as a risk factor for DR.18 A recent meta-analysis found a strong association between lipid levels and diabetic macular oedema, although this was not confirmed when only including prospective randomised control trials.19 Although some studies have shown fenofibrate as having some benefit in diabetic macular oedema, statins remain first line as a lipid-lowering agent in T1DM and correspondingly fenofibrate was only used in one patient in the cohort.
There is ongoing national debate regarding diabetic retinal screening intervals, which are currently annual, varying according to risk of progression. In this study, those with a diagnosis of T1DM for <10 years and not on antihypertensive or statin treatment appear to be at lower risk of sight-threatening DR and may be suitable for less frequent screening. It may furthermore be safe to defer screening for some years following diagnosis in T1DM. The significant association between being on antihypertensive medication and PDR in our study suggests increasing the screening interval beyond the present annual standard might not be advisable in these patients. Likewise, those patients on a statin appear to have increased risk of maculopathy, suggesting screening intervals in this group should not be increased. However, it is vital that these findings are corroborated in larger studies before any recommendations for screening intervals can be made.
In summary, this study provides contemporary estimates of DR prevalence in the UK for T1DM. Disease duration is confirmed as a major risk factor for DR and the distinct natural histories of PDR and diabetic maculopathy are illustrated with relation to duration of T1DM. Antihypertensive treatment was significantly associated with PDR while statin therapy was associated with maculopathy, suggesting differences in pathophysiology underlying these two forms of potentially sight-threatening DR. Further T1DM studies of DR progression and larger current studies looking at T1DR prevalence in relation to systemic and other factors are needed to assist in categorising risk of sight-threatening DR, which may have important implications for redefining diabetic retinal screening intervals in the UK.

References
Liew G, Michaelides M, Bunce C . A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 with 2009-2010. BMJ Open 2014; 4: e004015-2013-004015.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL . The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 1984; 102: 520–526.
Klein R, Klein BK, Moss SE, Davis MD, DeMets DL . The Wisconsin epidemiologic study of diabetic retinopathy: iii. prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol 1984; 102: 527–532.
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012; 35: 556–564.
Echouffo-Tcheugui JB, Ali MK, Roglic G, Hayward RA, Narayan KM . Screening intervals for diabetic retinopathy and incidence of visual loss: a systematic review. Diabet Med 2013; 30: 1272–1292.
Younis N, Broadbent DM, Harding SP, Vora JR . Prevalence of diabetic eye disease in patients entering a systematic primary care-based eye screening programme. Diabet Med 2002; 19: 1014–1021.
Thomas RL, Dunstan FD, Luzio SD, Chowdhury SR, North RV, Hale SL et al. Prevalence of diabetic retinopathy within a national diabetic retinopathy screening service. Br J Ophthalmol 2015; 99: 64–68.
Brooks A, Li Voon Chong J . Observations on age at diagnosis of type 1 diabetes and family history in a small population: the Winchester cohort. Practical Diabetes 2014; 31: 331–335.
Scanlon PH . The English national screening programme for sight-threatening diabetic retinopathy. J Med Screen 2008; 15: 1–4.
NHS Diabetic Eye Screening Programme Grading definitions for referable disease. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/580329/Grading_definitions_for_referrable_disease_2017.pdf. first published in Nov 2012 and updated in Jan 2017.
Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991; 98: 823–833.
Lee R, Wong TY, Sabanayagam C . Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond) 2015; 2: 17-015-0026-2 eCollection 2015.
Klein R, Klein BE, Davis MD . Is cigarette smoking associated with diabetic retinopathy? Am J Epidemiol 1983; 118: 228–238.
Moss SE, Klein R, Klein BE . Cigarette smoking and ten-year progression of diabetic retinopathy. Ophthalmology 1996; 103: 1438–1442.
White NH, Sun W, Cleary PA, Danis RP, Davis MD, Hainsworth DP et al. Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the Diabetes Control and Complications Trial. Arch Ophthalmol 2008; 126: 1707–1715.
Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR . Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med 2008; 359: 1565–1576.
Do DV, Wang X, Vedula SS, Marrone M, Sleilati G, Hawkins BS et al. Blood pressure control for diabetic retinopathy. Cochrane Database Syst Rev 2015; 1: CD006127.
Ding J, Wong TY . Current epidemiology of diabetic retinopathy and diabetic macular edema. Curr Diab Rep 2012; 12: 346–354.
Das R, Kerr R, Chakravarthy U, Hogg RE . Dyslipidemia and diabetic macular edema: a systematic review and meta-analysis. Ophthalmology 2015; 122: 1820–1827.
Acknowledgements
We would like to thank the team at Southampton Diabetic Eye Screening Programme for providing assistance with access for data collection.
Author contributions
A Brooks created the list of patients comprising the Winchester Cohort, as described in the methods section, and also collected all data excluding diabetic retinopathy status and visual acuity. A Brooks and R Krishnan collaborated to design this study and A Warwick collected diabetic retinopathy status and visual acuity data for the cohort. A Warwick performed the data analysis with guidance from C Osmond. R Krishnan, A Brooks, and C Osmond reviewed and revised the manuscript drafted initially by A Warwick.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Warwick, A., Brooks, A., Osmond, C. et al. Prevalence of referable, sight-threatening retinopathy in type 1 diabetes and its relationship to diabetes duration and systemic risk factors. Eye 31, 333–341 (2017). https://doi.org/10.1038/eye.2016.294
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.294
This article is cited by
-
Surgical strategy and outcome in patients with bilateral proliferative diabetic retinopathy
International Ophthalmology (2023)
-
Visual outcomes of observation, macular laser and anti-VEGF in diabetic macular edema in type 1 diabetes: a real-world study
BMC Ophthalmology (2022)
-
How is the risk of being diagnosed with referable diabetic retinopathy affected by failure to attend diabetes eye screening appointments?
Eye (2021)
-
Prevalence, severity stages, and risk factors of diabetic retinopathy in 1464 adult patients with type 1 diabetes
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)