Abstract
Purpose
To review the histopathological diagnoses, visual outcome, and complication rate of orbital biopsy in a UK tertiary referral centre.
Methods
This was a retrospective, clinical–pathological, interventional, consecutive case series. All orbital biopsies performed between July 2004 and June 2014 in Newcastle Eye Centre (Newcastle upon Tyne, UK) were included in this study. All relevant data collected from the local electronic database and medical records were analysed.
Results
A total of 166 orbital biopsies were identified during the study period: 86 patients (53.1%) were female and the mean age was 53.7±19.7 years. Of all the cases, orbital biopsies were performed unilaterally in 158 (97.5%) patients and bilaterally in 4 (2.5%) patients. The mean follow-up period was 2.2±2.3 years. The two most common histopathological diagnoses were non-specific inflammatory disease (62, 38.3%) and lymphoproliferative disease (40, 24.7%). None of the patients experienced ≥2-Snellen line visual loss. There were 7 (4.2%) postoperative complications noted: 1 (0.6%) orbital haemorrhage with no loss of vision, 4 (2.4%) diplopia, 1 (0.6%) short-term symblepharon, and 1 (0.6%) conjunctival granuloma. Postoperative diplopia was associated with lateral orbitotomy (P=0.044) and excisional biopsy (P=0.015).
Conclusions
Orbital biopsy serves as a safe diagnostic tool in managing orbital diseases. Patient should be made aware of the risk of postoperative diplopia. Our data provides useful guidance to clinicians when counselling patients for orbital biopsy.
Similar content being viewed by others
Introduction
Orbital diseases often present as serious ophthalmic emergencies which require immediate clinical attention. Permanent sight-threatening complications (eg, optic nerve compression and severe corneal exposure) may occur if the disease is not treated promptly.1, 2 The heterogeneity of orbital diseases frequently poses a diagnostic dilemma to the attending clinicians.3, 4, 5, 6, 7, 8, 9 When diagnosis cannot be made confidently on the ground of clinical and radiological findings, orbital biopsy is required to help achieve the definitive diagnosis before an appropriate management plan is formulated.
So far, there is limited data available in the literature specifically describing the histopathological diagnoses, visual outcome, and safety of orbital biopsy in UK.10, 11 The objectives of our study are twofold. First, we aim to examine the demographic factors and histopathological diagnoses of orbital biopsy in the Newcastle Eye Centre, which serves as a tertiary referral centre for orbital disease in the North East England, over the past 10 years. Second, we aim to report the visual outcome and the complication rate of orbital biopsy.
Materials and methods
This was a retrospective, clinical–pathological, interventional, consecutive case series. All orbital biopsies performed between July 2004 and June 2014 under the orbital service (LC, AJD, and CN) in Newcastle Eye Centre (Newcastle upon Tyne, UK) were included in this study. All the cases were identified from the electronic coding system using the term ‘orbital biopsy’, ‘lacrimal biopsy’, ‘orbitotomy’, and ‘eye/ocular muscle biopsy’. All identified cases were reviewed and only orbital biopsy cases were included in this study. Demographic factors, histopathological diagnoses, visual outcome, and complication of orbital biopsy collected from the local electronic database and medical records were analysed. Our study did not require any ethical approval but was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from all the patients prior to orbital biopsy.
Classification/terminology
The location of the lesion was defined by ‘anterior vs posterior’ and ‘intraconal vs extraconal’. The posterior limit of the globe was used as the cutoff point to distinguish between (predominantly) anterior and (predominantly) posterior lesions. The histopathological diagnoses were broadly divided into four groups: malignant tumours, benign tumours, inflammatory diseases, and others.
Statistical analysis
Visual outcome was defined by mild visual loss (loss of ≤2-Snellen line best-corrected visual acuity) and severe visual loss (loss of ≥6 Snellen line best-corrected visual acuity). Snellen visual acuity was also converted to LogMAR visual acuity for calculation of the mean difference between preoperative vision and postoperative vision. Two-tailed Fisher’s exact test was used to examine the significance of different variables predisposing to postoperative diplopia. P-value of <0.05 was considered statistically significant.
Results
A total of 166 orbital biopsies were identified during the study period: 86 patients (53.1%) were female and the mean age was 53.7±19.7 years. The demographic factors and clinical details of all orbital biopsies are summarised in Table 1. Of all the cases, orbital biopsies were performed unilaterally in 158 (97.5%) patients and bilaterally in 4 (2.5%) patients. The mean interval between first presentation to the orbital service and orbital biopsy was 7.2±11.6 weeks. The mean follow-up period was 2.2±2.3 years.
Histopathological diagnoses
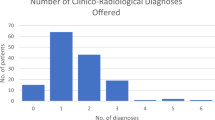
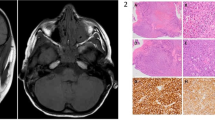
The distribution of histopathological diagnoses of all orbital biopsies is shown in Figure 1 and Table 2. Cases where bilateral orbital biopsies were performed were considered as a single case. Inflammatory orbital disease (71, 43.8%) was the most common group of histopathological diagnosis. In terms of specific diagnosis, non-specific inflammatory disease (62, 38.3%), lymphoproliferative disease (40, 24.7%), and normal biopsy (13, 8.0%) were the three main diagnoses. Of the 13 cases with normal biopsy result, 12 (92.3%) did not require any treatment and were either successfully discharged from the service or kept under observation; only 1 (7.7%) was treated with oral non-steroidal anti-inflammatory drug and oral steroid based on clinical findings.
Visual outcome
The mean preoperative and postoperative (within 1 month) best-corrected LogMAR visual acuity were 0.096±0.170 and 0.094±0.168, respectively (P=0.950). None (0, 0.0%) of the patients experienced ≥2-Snellen line visual loss.
Complication
There were 7 (4.2%) postoperative complications noted during the study period: 1 (0.6%) orbital haemorrhage with no loss of vision, 4 (2.4%) diplopia, 1 (0.6%) short-term symblepharon, and 1 (0.6%) conjunctival granuloma. The patient who developed postoperative orbital haemorrhage had an extensive orbital lesion secondary to arteriovenous malformation. The patient maintained good vision at 1-month postoperatively (visual acuity of 6/6) and 6-months postoperatively (visual acuity of 6/5) with no long-term sequelae. The case of symblepharon was related to wound-involved conjunctiva, which was released within 1 month with no further issue. In addition, the case of conjunctival granuloma settled without any complication following excision of the lesion.
Of the 4 cases of postoperative diplopia, 1 (25%) patient had full resolution of the symptoms within 6 months, 1 (25%) was coping with head posture and had a binocular field of single vision of 71% and 2 (50%) ultimately opted for occlusive intraocular lens to cope with the intractable diplopia. Postoperative diplopia was found to be significantly associated with lateral orbitotomy (P=0.044) and excisional biopsy (P=0.015; see Table 3).
Discussion
To our best knowledge, this study represents the largest case series specifically reporting the demographic factors, histopathological diagnoses, visual outcome, and complication of orbital biopsy in the North East of England. Visual outcome serves as one of the main measures in assessing the safety of orbital biopsy. However, the visual outcome can be influenced or confounded by various factors, including the types of orbital surgery (anterior vs lateral orbitotomy), the underlying disease process, the extent of the lesion, and the treatment effect. There are limited studies in the literature that specifically examined the visual outcome following orbital biopsy or orbital surgery.10, 11, 12 The reported rate of postoperative blindness following all types of orbital surgery ranged between 0.40% and 0.44%.11, 12 In terms of orbital biopsy specifically, the rate of postoperative blindness was 0–0.87%.10, 11
Our study did not observe any immediate visual loss following orbital biopsy despite a case of orbital haemorrhage, which settled with good visual acuity at 1-month and 6-months postoperatively. This suggested that orbital biopsy is a safe diagnostic procedure in managing patients with orbital disease. Similarly, Jamison et al10 reported no significant visual loss at 1-day postoperatively and 1-year postoperatively. Although they reported significant difference between the preoperative vision and the vision at final follow-up, the interpretation of the findings might be affected by the natural history of the orbital disease and the effect of the treatment (eg, orbital radiotherapy, steroid treatment). On the basis of these reasons, we therefore elected in our study to examine the initial postoperative visual acuity (<1 month) and not that during final follow-up. Various theories, including occlusion of the central retinal artery, traction on the optic nerve, and excessive postoperative bleeding or oedema leading to high intraorbital pressure, have been postulated for postoperative blindness following orbital surgery. The exact mechanism of postoperative blindness, however, remains elusive.12, 13 Rose proposed that the underlying mechanism of postoperative blindness is related to optic nerve ischaemia, which is most likely owing to postoperative vasospasm.11
Postoperative diplopia was shown to be one of the main complications (4, 2.5%) in our study. Although the rate of postoperative diplopia was low, two patients had intractable diplopia requiring occlusive intraocular lens. Therefore, careful counselling of the patient before undergoing orbital biopsy is of paramount importance. The risk of postoperative diplopia was shown to be significantly associated with lateral orbitotomy (P=0.044) and excisional biopsy (P=0.015). This was consistent with the studies conducted by Purgason and Hornblass,14 and Salem and Qahtani,15 who similarly reported a higher rate of complications following lateral orbitotomy as compared with anterior orbitotomy. They also observed that intraconal lesions carried a higher risk of complications in comparison with extraconal lesions.14, 15 Although our study observed a higher rate of postoperative diplopia in intraconal lesions, statistical significance was not achieved (P=0.078). In addition, excisional biopsy involves more extensive removal of diseased tissues with a greater risk of postoperative diplopia.
Large variation of orbital diseases has been reported in the literature.3, 4, 5, 6, 7, 8, 9, 10 Bonavolontà et al3 observed that dermoid cyst (14%) was the most common orbital disease noted in their study. On the other hand, Shields et al6 and Jamison et al10 reported idiopathic orbital inflammation and lymphoproliferative tumour as the two most common orbital diseases. Our study similarly showed that non-specific orbital inflammatory disease (62, 38.3%) and lymphoproliferative disease (40, 24.7%) were the two most common histopathological diagnoses during the 10-year study period. This highlights the importance of examining the incidence of the orbital diseases in each specific region as it may be subject to geographical variation. Also, the incidence of orbital disease may be influenced by the inclusion criteria of the research study. For instance, the findings in our study reflected the lesions that were likely to be biopsied; therefore, cases such as thyroid orbitopathy and infective lesions were excluded.
Out of the 71 cases of orbital inflammatory disease, 2 cases were found to have IgG4-related ophthalmic disease (ROD), which is a recently recognised as fibro-inflammatory disorder that can affect one or more organs. With the increasing understanding of the pathology, clinical–radiological features and clinical implications of IgG4 disease over the recent years,16, 17 we believe that this specific group of disease may represent a considerable proportion of the biopsied cases in the future. A recent Japanese report described, as many as, 21.4% of their presumed ‘lymphoproliferative disease’ cases were of IgG4-ROD.18 On the other hand Karamchandani et al from US found only 6 (3.6%) cases of IgG4-ROD out of the 164 presumed orbital lymphoma cases, underlining the large geographical variation of this disease among different countries.19
Our study also showed that 13 (8.0%) cases were of normal histology and 12 of those patients did not require any treatment following the biopsy. This emphasises the importance of performing biopsy in doubtful cases because it not only provides reassurance to the patient but also helps to obviate the need of unnecessary treatment—which may be potentially harmful. We did not perform any intraoperative frozen section as most biopsies were for diagnostic purpose. Our data demonstrated that only 2 (1.2%) cases were of inconclusive result, suggesting that our approach and surgical technique yielded satisfactory result without the need for intraoperative frozen section.
Although Newcastle Eye Centre serves as the tertiary referral centre for orbital diseases in the North East England (NEE), we acknowledge that our study did not capture all the orbital biopsies in NEE because some of the more straightforward cases were managed independently in other local ophthalmic units and some cases were managed by the other specialties such as ENT and maxillo-facial team. Nonetheless we believe that our study had captured the majority of cases to provide a good overview of the histopathological diagnosis, visual outcome, and safety of orbital biopsy in the NEE. From the perspective of patient safety, we recommend that easily accessible anterior orbital biopsies can be performed by appropriately trained non-orbital surgeons to facilitate prompt diagnosis, provided they have the skills and facilities to manage any complications. It is important to bear in mind that an abnormality may be more obvious on imaging than apparent intraoperatively; therefore caution and experience is require in assessing patient’s suitability. Deeper and less accessible orbital lesions are best approached by more experienced orbital surgeons under general anaesthesia.
In conclusion, our study demonstrated that orbital biopsy serves as a useful and safe diagnostic procedure in managing patients with orbital disease. Patients should, however, be made aware of the risk of postoperative diplopia. Our data provide useful guidance to the clinician when counselling the patients for orbital biopsy.

References
Hornbeak DM, Tamhankar MA, Eckstein LA . No light perception vision from compressive thyroid orbitopathy. Orbit 2014; 33 (1): 72–74.
Lima V, Burt B, Leibovitch I, Prabhakaran V, Goldberg RA, Selva D . Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol 2009; 54 (4): 441–449.
Bonavolontà G, Strianese D, Grassi P, Comune C, Tranfa F, Uccello G et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthal Plast Reconstr Surg 2013; 29 (2): 79–86.
Tailor TD, Gupta D, Dalley RW, Keene CD, Anzai Y . Orbital neoplasms in adults: clinical, radiologic, and pathologic review. Radiographics 2013; 33 (6): 1739–1758.
Teo L, Seah LL, Choo CT, Chee SP, Chee E, Looi A . A survey of the histopathology of lacrimal gland lesions in a tertiary referral centre. Orbit 2013; 32 (1): 1–7.
Shields JA, Shields CL, Scartozzi R . Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery lecture, part 1. Ophthalmology 2004; 111 (5): 997–1008.
Demirci H, Shields CL, Shields JA, Honavar SG, Mercado GJ, Tovilla JC . Orbital tumors in the older adult population. Ophthalmology 2002; 109 (2): 243–248.
Johansen S, Heegaard S, Bogeskov L, Prause JU . Orbital space-occupying lesions in Denmark 1974–1997. Acta Ophthalmol Scand 2000; 78 (5): 547–552.
Kodsi SR, Shetlar DJ, Campbell RJ, Garrity JA, Bartley GB . A review of 340 orbital tumors in children during a 60-year period. Am J Ophthalmol 1994; 117 (2): 177–182.
Jamison A, Gregory ME, Lyall DA, Kemp EG . Visual outcome following orbital biopsy. Orbit 2013; 32 (5): 304–308.
Rose GE . The "devil's touch"; visual loss and orbital surgery. A synopsis of the Mustardé lecture, 2006. Orbit 2007; 26 (3): 147–158.
Bonavolontà G . Postoperative blindness following orbital surgery. Orbit 2005; 24 (3): 195–200.
Kennerdell JS, Maroon JC, Malton ML . Surgical approaches to orbital tumors. Clin Plast Surg 1988; 15 (2): 273–282.
Purgason PA, Hornblass A . Complications of surgery for orbital tumors. Ophthal Plast Reconstr Surg 1992; 8 (2): 88–93.
Salem M, Qahtani F . Risk factors associated with complications of orbital surgery in children. J Pediatr Ophthalmol Strabismus 2001; 38 (6): 335–339.
McNab AA, McKelvie P . IgG4-related ophthalmic disease. Part I: background and pathology. Ophthal Plast Reconstr Surg 2015; 31 (2): 83–88.
Yamamoto M, Hashimoto M, Takahashi H, Shinomura Y . IgG4 disease. J Neuroophthalmol 2014; 34 (4): 393–399.
Japanese Study Group of IgG4-related ophthalmic disease. A prevalence study of IgG4-related ophthalmic disease in Japan. Jpn J Ophthalmol 2013; 57: 573–579.
Karamchandani JR, Younes SF, Warnke RA, Natkunam Y . IgG4-related systemic sclerosing disease of the ocular adnexa: a potential mimic of ocular lymphoma. Am J Clin Pathol 2012; 137: 699–711.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ting, D., Perez-Lopez, M., Chew, N. et al. A 10-year review of orbital biopsy: the Newcastle Eye Centre Study. Eye 29, 1162–1166 (2015). https://doi.org/10.1038/eye.2015.95
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.95
This article is cited by
-
Ocular lymphoma: overcoming a diagnostic challenge with an endoscopic sinus approach
Irish Journal of Medical Science (1971 -) (2024)
-
Clinical characteristics, diagnosis, and outcomes of orbital biopsies in a single Irish centre
Irish Journal of Medical Science (1971 -) (2023)