Abstract
Purpose
To assess the relationship between age, corneal astigmatism, and ocular dimensions with reference to astigmatism correction during cataract surgery.
Methods
In this cross-sectional study of right eyes of 2247 consecutive patients attending cataract surgery preassessment, data on patient demographics, axial length (AL), anterior chamber depth (ACD), and keratometric astigmatism were collected. Astigmatism was further analyzed as against-the-rule (ATR: steepest meridian 180±30°), with-the-rule (WTR: 90±30°), and oblique (OB: 30–60°or 120–150°).
Results
Mean age, AL, and ACD were 72.28±13.84 years, 23.99±1.85 mm and 3.08 ±0.52 mm, respectively. In all, 20.4% eyes had ≤0.50 diopters (D), 55.2% had 0.51–1.50 D, 7.9% had 2.01–3.00 D, and 3.7% eyes had >3.00 D of astigmatism. Overall, 44.2% of eyes had corneal astigmatism >1.00 D. Average astigmatism in age ranges 40–49, 50–59, 60–69, 70–79, 80–89, and 90+ years were 0.82, 1.04, 1.04, 1.02, 1.15 and 2.01 D, respectively. The magnitude of preoperative astigmatism positively correlated with age (P<0.0001), with increasing and decreasing prevalence of ATR and WTR astigmatism, respectively, with advancing age. The magnitude of ATR astigmatism inversely correlates to AL (P<0.0001). ATR astigmatism is more prevalent with increasing magnitude of astigmatism (P<0.0001).
Conclusions
A majority of patients for cataract surgery have astigmatism between 0.51 and 1.5 D. ATR astigmatism increases, whereas WTR decreases with age. ATR astigmatism inversely correlates to AL. With increasing age, the magnitude of astigmatism increases and ATR astigmatism becomes increasingly prevalent. The likelihood of a patient requiring astigmatic correction increases with age.
Similar content being viewed by others
Introduction
Cataract surgery aims to eliminate or reduce preexisting refractive error and is one of the most commonly performed operations globally. Patient demands and postoperative expectations are continuously increasing with advances in surgical technique and improvement in intraocular lens (IOL) design and calculations. To achieve best postoperative visual outcomes, spherical and astigmatic components of refractive error should be corrected during cataract surgery.1 The prevalence of corneal astigmatism has been widely reported in several parts of the world.
It is useful to assess the relationship of corneal astigmatism, age, and ocular dimensions to further understand and predict the necessity for offering astigmatism correction procedures such as peripheral corneal-relaxing incisions (PCRIs) and toric IOLs in publicly funded National Health Service (NHS) government hospitals, such as in the United Kingdom, as these procedures have to be cost-effective. PCRIs are proven to neutralize more astigmatism compared with on-axis incisions (on steep axis),2, 3 which are limited to approximately 1.0 dioptre (D).4 However, PCRIs are shown to have regression when performed for ≥3.5 D of astigmatism.5 Toric IOLs are effective for treating >1 D of corneal astigmatism at the time of cataract surgery.6
This study aims to identify any relationship between preexisting corneal astigmatism with age, axial length (AL), and anterior chamber depth (ACD) of the eyes undergoing preassessment for routine cataract surgery.
Patients and methods
This is a retrospective cross-sectional study of the right eyes of 2247 consecutive patients who attended the cataract surgery preassessment clinics between October 2012 and October 2014 at the Sussex Eye Hospital, Brighton, UK. This study was approved by the Hospital's Audit Committee and followed the tenets of the Declaration of Helsinki.
Inclusion criteria was eyes preassessed for cataract surgery and optical biometry performed using the principle of partial coherence tomography (IOLMaster 500, Carl Zeiss, Jena, Germany) with reliable scans. Reliable scans were defined as scans with SNR (signal-to-noise ratio) >3. Exclusion criteria included eyes where biometry was not possible with IOLMaster, eyes that had A-scan ultrasonographs, eyes with preexisting corneal pathology, any previous surgery, trauma, and left eyes. All eyes were examined before the cataract surgery procedure, including an uncorrected and best-corrected vision, slitlamp examination, tonometry, and ophthalmoscopy through dilated pupils. Data on patient age, AL, ACD, and keratometric astigmatism were collected. Astigmatism was further analyzed as against-the-rule (ATR: steepest meridian 180±30°), with-the-rule (WTR: 90±30°), and oblique (OB: 30–60° or 120–150°).
Patients were divided into seven distinct age groups (<40, 40–49, 50–59, 60–69, 70–79, 80–89, >90 years) for further analysis, and all patients were analyzed irrespective and with respect to the axis of corneal astigmatism (WTR/OB/ATR). In addition, the magnitude of corneal astigmatism was divided into three distinct groups (<1, 1–3, and >3 D). Kolmogorov–Smirnov test was used to check the normality of the data. Pearson's coefficient was used for calculating correlation coefficients. All statistical analyses were two-sided and P-values <0.01 were considered statistically significant.
Results
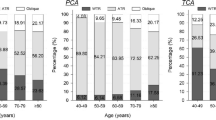
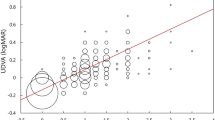
This study evaluated 2247 eyes from 2247 patients. Patient demographics are shown in Table 1. Figure 1a shows the distribution of corneal astigmatism in the entire sample in 0.25-D steps. Figure 1b shows the distribution of number of eyes with reference to age. In all, 22.4% eyes had ≤0.50 D, 55.2% had 0.51–1.50 D, 7.9% had 2.01–3.00 D, and 3.7% eyes had >3.00 D of astigmatism. The relationship between age and the magnitude of total corneal astigmatism is shown in Figures 1c and d. The magnitude of total corneal astigmatism was positively correlated with age (r=0.149, P<0.0001).
(a) Corneal astigmatism distribution in 0.25-D steps for the entire sample (2247 eyes). (b) Distribution of entire sample for each age subgroup. (c) Frequency distribution of corneal astigmatism in 0.50-D steps for the seven age groups. (d) Correlation between magnitude of total corneal astigmatism and age.
Further analysis indicates where the magnitude of corneal astigmatism was <1 D the prevalence decreased with increasing age (P<0.00001) and where the magnitude of corneal astigmatism was 1–3 D the prevalence increased with increasing age (P=0.0009). Furthermore where the magnitude of corneal stigmatism was >3 D the prevalence positively correlated with age (P<0.00001). This is illustrated in Figure 2.
There was a statistically significant linear relationship between the axis of astigmatism (WTR/OB/ATR) and age (r=0.301, P<0.00001); irrespective of the axis, there was a positive correlation between age and mean corneal astigmatism in the WTR/ATR/OB groups as illustrated in Figure 3a. Analysis of the WTR/ATR/OB prevalence by age showed that ATR astigmatism was increasingly prevalent with increasing age (r=0.256, P<0.00001), whereas WTR astigmatism was less prevalent with increasing age (r=−0.294, P<0.0001). However OB astigmatism did not clearly correlate to age (P=0.0415) as illustrated in Figure 3b.
(a) Correlation between mean corneal astigmatism in the WTR/ATR/OB groups and age. (b) The prevalence of WTR/ATR/OB astigmatism by age. (c) The prevalence of WTR/ATR/OB by different magnitudes of astigmatism. (d) Correlation between magnitude of preoperative astigmatism and ACD with reference to WTR/OB/ATR. (e) Correlation between magnitude of preoperative astigmatism and AL with reference to WTR/OB/ATR.
Prevalence of WTR/ATR/OB astigmatism in different magnitudes of astigmatism is shown in Figure 3c. This demonstrates that ATR astigmatism is increasingly prevalent with increasing magnitude of astigmatism (r=0.166, P<0.00001), whereas OB astigmatism is less prevalent with increasing magnitude of astigmatism (r=−0.166, P<0.00001). The prevalence of WTR astigmatism did not correlate to the magnitude of astigmatism (r=0.0384, P=0.124).
Figure 3d shows the correlation between ACD and the magnitude of astigmatism. ACD did not correlate to the magnitude of corneal astigmatism irrespective or with respect to the axis of astigmatism. Analysis of the correlation between AL and the magnitude of astigmatism is illustrated in Figure 3e. A WTR/OB magnitude of astigmatism did not significantly correlate to AL (P=0.775/0.0296, respectively); however, the magnitude of ATR astigmatism does significantly correlate to AL (r=−0.250, P<0.00001).
Discussion
A large proportion of patients with preexisting cataracts have some degree of corneal astigmatism. Correcting astigmatism improves quality of life, provides spectacle independence, and improvement in visual outcomes.7 In recent years, toric IOLs are increasingly used as first-line measures for correcting corneal astigmatism of >1.5 D at the time of phacoemulsification.6, 8 In this study, 44.2% of eyes had corneal astigmatism >1 D, which is higher than Chen et al9 (41.3%), Ferrer-Blasco et al10 (34.8%), Hoffman et al11 (36.0%), and Khan et al12(40.41%). The higher figure in this study is likely to be concurrent to higher mean age of 72.28 years. Similarly, the mean corneal astigmatism of 1.08 D was higher than the aforementioned studies as shown in Figure 2. Patients with >1 D of astigmatism should be considered for surgical correction of astigmatism at the time of surgery for improvement of visual outcomes postoperatively.
It is already known that the prevalence of corneal astigmatism increases relative to age, and our study is concordant with these findings (Table 2a). As such, the likelihood of a patient requiring astigmatic correction at the time of cataracts surgery increases with age. In this cohort, the prevalence of corneal astigmatism <1 D decreased with increasing age (P<0.00001), whereas reciprocally the prevalence of corneal astigmatism between 1–3 D (P=0.0009) and >3 D (P<0.00001) increased with increasing age. This further supports the positive correlation between the magnitude of corneal astigmatism and age.
Our data show that an ATR corneal astigmatism is increasingly prevalent with increasing age (r=0.256, P<0.00001), whereas WTR astigmatism is less prevalent (r=−0.294, P<0.0001). The shift from WTR to ATR astigmatism with increasing age is well documented in other studies,1, 9, 13, 14, 15, 16 although Hashemi et al17 identified no statistically significant correlation between the prevalence of WTR astigmatism and age. The reasons for the age-dependent change in axis remain unclear, but they are hypothesized to be due to changes to upper eyelid tension,18, 19 intraocular pressures,20 and possibly changes to corneal structure.13 The correlation between the axis of astigmatism and age is significant because residual postsurgical WTR astigmatism has been shown to result in better distance Snellen visual acuity than OB astigmatism,4 whereas residual ATR results in better unaided distance and near vision in some pseudophakics.21 This therefore poses the question as to whether corneal stigmatism should be treated more aggressively in younger patients where WTR astigmatism is most prevalent. However, with the increasing popularity of toric presbyopic (multifocal and depth-of-focus) IOLs this becomes less significant for patients who can afford to pay for premium IOLs with guaranteed multifocality and depth of focus.
To our knowledge, the relationship between the magnitude of preoperative corneal astigmatism and the type of astigmatism (WTR/ATR/OB) has not yet been reported. The degree of preoperative corneal astigmatism should be investigated at the time of cataract surgery. Data from this cohort demonstrated that ATR astigmatism is increasingly prevalent with increasing magnitude of astigmatism (Figure 3c). A large proportion of patients with ATR astigmatism may therefore benefit from toric IOLs at the time of cataract surgery to improve visual outcomes. While ATR and OB astigmatism may increase with age, our findings show that OB astigmatism decreases relative to the magnitude of astigmatism (Figure 3c). A summary of key findings from other papers relating to the population demographics, magnitude, and axis of corneal astigmatism can be seen in Tables 2a and b.
Finally, we also assessed the relationship between ocular dimensions and corneal astigmatism. AL is arguably one of the most important factors in preoperative assessment for IOL calculations, to ensure correct use of lenses and to reduce postoperative astigmatism. Analysis of this cohort showed that the magnitude of ATR astigmatism negatively correlated to AL (Figure 3e), meaning that smaller eyes have a larger degree of ATR astigmatism in patients undergoing cataract surgery. Conversely, ACD showed no significant correlation with corneal astigmatism (Figure 3d). AL is commonly regarded as the most significant determinant of refractive error.22 The key findings of other papers relating to AL and ACD can be seen in Table 2c; however, to our knowledge no paper has reported a significant correlation between AL and the magnitude of preoperative corneal astigmatism. In light of this, AL and corneal astigmatism should be assessed collectively preoperatively to decide the best method to correct astigmatism during cataract surgery with improved visual outcomes.
As the likelihood of a patient requiring astigmatic correction at the time of cataract surgery increases with age, it is useful to factor the cost of astigmatic corrective procedures when estimating expenses for cataract surgery in an ageing population. This is particularly relevant in countries where majority of cataract surgery is performed in the publicly funded government hospitals such as in the United Kingdom with National Health Service (NHS), compared with other countries. Furthermore, treatment should arguably be more aggressive during cataract surgery, because astigmatism will develop with age and increasing astigmatism is implicated with higher costs.23 As 44.2% of this cohort have >1 D of astigmatism and toric IOLs are affective for treating >1 D of astigmatism at the time of surgery, this data is also useful to assess the necessity for use of toric IOLs in this population.6 The data on prevalence of corneal astigmatism in our population is very useful for further design of local protocol and analysis of potential costs for the local NHS trust and NHS England. With reference to potential costs, an American study23 concluded toric IOLs (where astigmatism >1.5 D) reduce lifetime economic costs by reducing the need for glasses or contact lenses, following cataract removal.
The limitation of this study is that it is a retrospective cross-sectional study. Patient selection may account for some of the disparities between different international studies. Patient age ranged from 10 to 109 years in our study, compared with Chen et al9 (40–95), Ferrer-Blasco et al10 (32–87), Guan et al1 (16–98), Khan et al12 (30–104), Hashemi et al17 (40–65), and Nemeth et al24 (≥15). Nonetheless, our data has a very wide range capturing a real picture of astigmatism in the cataract surgery population.
In summary, our study supports an increasing trend from WTR to ATR preoperative corneal astigmatism with age. The magnitude of corneal astigmatism is also significantly more pronounced in ATR astigmatism. With respect to ocular dimensions, AL negatively correlates with the magnitude of ATR astigmatism. All of these findings should therefore be considered and used to estimate costs of astigmatic corrective procedures for cataract surgery in the ageing population.

References
Guan Z, Yuan F, Yuan YZ, Niu WR . Analysis of corneal astigmatism in cataract surgery candidates at a teaching hospital in Shanghai, China. J Cataract Refract Surg 2012; 38 (11): 1970–1977.
Budak K, Friedman NJ, Koch DD . Limbal relaxing incisions with cataract surgery. J Cataract Refract Surg 1998; 24 (4): 503–508.
Wang L, Misra M, Koch DD . Peripheral corneal relaxing incisions combined with cataract surgery. J Cataract Refract Surg 2003; 29 (4): 712–722.
Morlet N, Minassian D, Dart J . Astigmatism and the analysis of its surgical correction. Br J Ophthalmol 2001; 85 (9): 1127–1138.
Bayramlar H, Daglioglu MC, Borazan M . Limbal relaxing incisions for primary mixed astigmatism and mixed astigmatism after cataract surgery. J Cataract Refract Surg 2003; 29 (4): 723–728.
Amesbury EC, Miller KM . Correction of astigmatism at the time of cataract surgery. Curr Opin Ophthalmol 2009; 20 (1): 19–24.
Buckhurst PJ, Wolffsohn JS, Davies LN, Naroo SA . Surgical correction of astigmatism during cataract surgery. Clin Exp Optom 2010; 93 (6): 409–418.
Hasegawa Y, Okamoto F, Nakano S, Hiraoka T, Oshika T . Effect of preoperative corneal astigmatism orientation on results with a toric intraocular lens. J Cataract Refract Surg 2013; 39 (12): 1846–1851.
Chen W, Zuo C, Chen C, Su J, Luo L, Congdon N et al. Prevalence of corneal astigmatism before cataract surgery in Chinese patients. J Cataract Refract Surg 2013; 39 (2): 188–192.
Ferrer-Blasco T, Montes-Mico R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A . Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg 2009; 35 (1): 70–75.
Hoffmann PC, Hutz WW . Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg 2010; 36 (9): 1479–1485.
Khan MI, Muhtaseb M . Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg 2011; 37 (10): 1751–1755.
Hayashi K, Hayashi H, Hayashi F . Topographic analysis of the changes in corneal shape due to aging. Cornea 1995; 14 (5): 527–532.
Ho JD, Liou SW, Tsai RJ, Tsai CY . Effects of aging on anterior and posterior corneal astigmatism. Cornea 2010; 29 (6): 632–637.
Riley AF, Grupcheva CN, Malik TY, Craig JP, McGhee CN . The Auckland Cataract Study: demographic, corneal topographic and ocular biometric parameters. Clin Experiment Ophthalmol 2001; 29 (6): 381–386.
Ueno Y, Hiraoka T, Miyazaki M, Ito M, Oshika T . Corneal thickness profile and posterior corneal astigmatism in normal corneas. Ophthalmology 2015; 122 (6): 1072–1078.
Hashemi H, Khabazkhoob M, Yekta A, Jafarzadehpur E, Emamian MH, Shariati M . High prevalence of astigmatism in the 40- to 64-year-old population of Shahroud, Iran. Clin Experiment Ophthalmol 2012; 40 (3): 247–254.
Grosvenor T . Etiology of astigmatism. Am J Optom Physiol Opt 1978; 55 (3): 214–218.
Vihlen FS, Wilson G . The relation between eyelid tension, corneal toricity, and age. Invest Ophthalmol Vis Sci 1983; 24 (10): 1367–1373.
Howland HC, Sayles N . Photokeratometric and photorefractive measurements of astigmatism in infants and young children. Vision Res 1985; 25 (1): 73–81.
Nanavaty MA, Vasavada AR, Patel AS, Raj SM, Desai TH . Analysis of patients with good uncorrected distance and near vision after monofocal intraocular lens implantation. J Cataract Refract Surg 2006; 32 (7): 1091–1097.
Mallen EA, Gammoh Y, Al-Bdour M, Sayegh FN . Refractive error and ocular biometry in Jordanian adults. Ophthalmic Physiol Opt 2005; 25 (4): 302–309.
Pineda R, Denevich S, Lee WC, Waycaster C, Pashos C . Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol 2010; 128 (7): 834–840.
Nemeth G, Szalai E, Berta A, Modis L Jr . Astigmatism prevalence and biometric analysis in normal population. Eur J Ophthalmol 2013; 23 (6): 779–783.
Leighton DA, Tomlinson A . Changes in axial length and other dimensions of the eyeball with increasing age. Acta Ophthalmol (Copenh) 1972; 50 (6): 815–826.
Olsen T, Arnarsson A, Sasaki H, Sasaki K, Jonasson F . On the ocular refractive components: the Reykjavik Eye Study. Acta Ophthalmol Scand 2007; 85 (4): 361–366.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
A brief version of this paper has been presented at the Annual Meeting of the British Society of Refractive Surgery, Birmingham, UK, March 2015, as well as at the Annual Meeting of Students' Independent Research Project Conference, Brighton, UK.
Author contributions
OCW: Data collection, analysis, manuscript drafting, statistical analysis and interpretation. RA: Data collection, analysis, manuscript drafting. MAN: Concept and design, analysis, manuscript editing, drafting, and critical review.
Rights and permissions
About this article
Cite this article
Collier Wakefield, O., Annoh, R. & Nanavaty, M. Relationship between age, corneal astigmatism, and ocular dimensions with reference to astigmatism in eyes undergoing routine cataract surgery. Eye 30, 562–569 (2016). https://doi.org/10.1038/eye.2015.274
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.274
This article is cited by
-
Evaluation of an intraoperative marking technique using the body axis as a reference
Spektrum der Augenheilkunde (2022)
-
Central and mid-peripheral corneal astigmatism in an elderly population: a retrospective analysis of Scheimpflug topography results
Scientific Reports (2021)
-
Relationship between central and peripheral corneal astigmatism in elderly patients
Optical Review (2018)
-
Qualitative and quantitative evaluation of acute angle-closure mechanisms
BMC Ophthalmology (2017)