Abstract
Purpose
To determine the association of hydroxymethylglutarylcoenzyme A (HMG Co-A) reductase inhibitor (statin) use with the prevalence of age-related macular degeneration (AMD).
Methods
This cross-sectional study included 5604 participants in the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2008, ≥40 years of age, who were ascertained with regard to the diagnosis of AMD, the use of statins, and comorbidities and health-related behaviors such as smoking.
Results
The mean age of participants denying or confirming a history of AMD was 68 (SEM 0.90) and 55 (SEM 0.36) years, respectively. Individuals 68 years of age or older who were classified as long-term users of statins had statistically significant less self-reported AMD (odds ratio (OR) 0.64, 95% confidence interval (CI) 0.49–0.84; P=0.002), after adjusting for potential confounding variables. No significant association was found between the prevalence of AMD and statin consumption among subjects between 40 and 67 years of age (OR 1.61, 95% CI 0.85–3.03; P=0.137).
Conclusions
Our results suggest a possible beneficial effect of statin intake for the prevention of AMD in individuals 68 years of age or older.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is a progressive eye disorder and the leading cause of legal blindness in individuals aged 65 years and older in developed countries.1, 2, 3, 4 AMD becomes clinically evident typically after 50 years of age,5 and is classified based upon disease severity.6 Early AMD is characterized by the presence of drusen and pigmentary abnormalities in the retinal pigment epithelium (RPE) and late AMD is characterized by degenerative changes in the RPE, Bruch’s membrane, and choriocapillaris, resulting in geographic atrophy and/or neovascular AMD.6, 7
The prevalence of AMD in the United States was described by Klein et al4 in 2011. The highest prevalence was found in individuals aged 60 years or older, with approximately 7.2 million individuals having AMD and 0.89 million having late AMD. In the United States, there is a 50% increased projection of advanced AMD cases by 2020, reaching 3 million individuals, approximately 40% of AMD cases.6
Although a number of agents are available to treat exudative (‘wet’) AMD, prevention of the disease continues to be more challenging.8, 9 The pathogenesis of AMD remains indeterminate and is likely to be multifactorial.10 The disease is related to well-known risk factors, such as cigarette smoking, elevated serum cholesterol levels, and hypertension, that are shared with atherosclerosis and consequently with increased risk of cardiovascular disease (CVD).1, 6, 11 Genetic studies have reported similar susceptibility genes for CVD and AMD, such as complement factor H loci.9, 12, 13 Therefore, a modification in atherosclerotic changes with lipid-lowering medications may exert a preventive effect in AMD development by prevention of lipid deposits at the level of Bruch’s membrane.3, 9, 10
Statins are hydroxymethylglutarylcoenzyme A (HMG Co-A) reductase inhibitors, which are capable of reducing serum lipoprotein levels and are primarily used to treat dyslipidemia and reduce cardiovascular mortality.14 This class of drugs includes atorvastatin, simvastatin, lovastatin, fluvastatin, cerivastatin, rosuvastatin, and pravastatin. Since 1987, these drugs have been widely used to reduce LDL cholesterol and plasma triglycerides.15 However, other effects including anti-inflammatory, anti-endothelial dysfunction, anti-angiogenic, and antioxidant activities of statins have been reported in relation to various conditions such as cancer, osteoporosis, Alzheimer’s dementia, and AMD.10, 14, 16, 17
Evidence in the published medical literature relating to the association of statin intake and AMD remains controversial.18 Since 1991, multiple studies with different designs have evaluated statin use and AMD development or progression. Some studies support a protective effect and others have been inconclusive with regard to a protective effect. The National Health and Nutrition Examination Survey (NHANES) is a nationwide, population-based sample of individuals aged 40 years of age or older. It is designed to assess the health status of the US population. The survey provides essential data on AMD, using high-resolution color photographs of the macula that were graded by an objective system.4 We have used the NHANES’ extensive representative sample to study the potential protective effect of statin intake and AMD.
Materials and methods
Data source
In this study, we used data from years 2005 to 2008 of the NHANES, a national program of studies designed to assess the health and nutritional status of adults and children. NHANES is conducted annually by the Centers for Disease Control and Prevention and designed to provide statistics for the US population via a cross-sectional series of interviews, medical exams, and laboratory tests of approximately 5000 civilians, non-institutionalized persons per year who are chosen by a stratified multistage sampling design. It was reviewed and approved by a human subjects board, and informed consent was obtained from all participants. A detailed description of the design and data collection can be found online.19 The data were analyzed to assess the relationship between statin intake and presence of AMD.
Sample and population
Using data from 2005 to 2008, we initially included the 6797 participants of NHANES who were 40 years and older and underwent both interview and examination portions of the study. Of this total, 1193 participants were excluded, including 969 that did not have complete ophthalmological examinations with retinal photographs and 224 that had unreadable photographs. For better understanding of the influence of age in the relationship between statin use and presence of AMD, we used subgroups of the population sample, comparing younger (40–67 years) and older individuals (68 years and older), taking into account that the mean age of AMD participants was 68 years.
Measures
Our main predictor variable for this study was the self-reported use of a statin drug. NHANES has information regarding the use of prescription medication 30 days before the questionnaires. Patients were considered to be under statin therapy when they reported the use of any type of statin agents such as lovastatin, pravastatin, simvastatin, fluvastatin, atorvastatin, cerivastatin, and rosuvastatin, during this period, and were included in the analysis.
The questionnaire also provides information on the number of days each participant was using the statins. This was converted to month and years of use, for an easier interpretation.
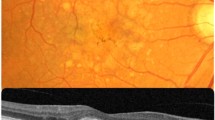
Retinal images were captured using a Canon CR6 (Canon Inc., Tokyo, Japan), nonmydriatic, camera with a Canon 10D camera back. Two 45° digital images were taken, providing photographic documentation of the optic disc, macula, and portions of the superior temporal arcades. A complete explanation on the grading system is available elsewhere.20
The presence of AMD was determined through gradable retinal photographs of the macula from the participants as part of the ophthalmology examination. Early AMD was defined as presence of either soft drusen with a grid area of greater than a 500 μ circle and a pigmentary abnormality (increased pigmentation or depigmentation) or soft drusen and a pigmentary abnormality in the center circle without signs of advanced AMD. Advanced or late AMD was defined as the presence of any late lesions, such as geographic atrophy, RPE detachments, subretinal hemorrhage, fibrous scar, or neovascularization. When retinal photos were considered unreadable or confounded by other findings in the retina, they were excluded from the evaluation of AMD lesions. Any AMD as defined in this study included both early and late AMD. When the eyes of a participant had different grading for AMD, the worse eye was used to assign the participant a grade. The main outcome for this study was the presence of any AMD in the worse eye.
The interview portion of the NHANES survey provides data on demographic variables such as age, race, sex, education level, and household income. Individual health-related behaviors (smoking and alcohol use); general health condition (self-rated as excellent or very good, fair, poor or very poor); body mass index (BMI); medical comorbidities (diabetes mellitus, systemic hypertension, history of stroke, and coronary heart disease); and ocular comorbidities (history of cataract extraction, diabetic retinopathy, and macular degeneration), were also collected through self-reported questionnaire.
Data analysis
All data analysis was performed using Stata software, version 12.1 (College Station, TX, USA). Using multivariate logistic regression models, we analyzed the association between statin intake and AMD by adjusting for potential confounding variables.
Confounding comorbidities that did not present significant values in the multivariate models at the P<0.1 level were excluded from the final analysis. As history of alcohol use and BMI did not reach significance, they were excluded from the model. Taylor linearization was used to extrapolate the values to the US national population. We calculated odds ratios (ORs) with corresponding 95% confidence intervals (CIs). A value of P<0.05 was determined as significant for all the analyses.
We used design-adjusted Rao–Scott χ2 for categorical values and Wald tests for continuous variables when evaluating the distribution of these variables between participants receiving and not receiving statins. Additional models were performed to assess whether or not a potential association between variables was influenced by the duration of statin therapy in different age groups.
Results
Population characteristics
The 2005–2008 NHANES data yielded 5604 participants aged 40 years and older, who participated in both the interview and examination portions of the study and had gradable retinal photographs. Of these participants, 1231 were receiving statin therapy representing 19.48% (SEM 0.74%) of the study population, 620 were in the younger group (40–67 years) and 611 in the older group (68 years and older); and 441 were diagnosed with AMD, representing 6.58% (SEM 0.49%) of the same population. The mean ages of those without AMD was 55.6 years (SEM 0.36 years) and those with AMD was 68.0 (SEM 0.90 years; P<0.0001).
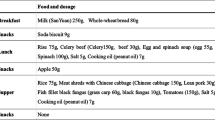
Table 1 shows demographic information, health-related behaviors, and comorbidities of the study population, comparing those receiving and not receiving statins. Among the population enrolled in the study, several differences in baseline characteristics were found to be statistically significant. Racial distribution (P=0.0009) and annual household income (P=0.0005) differed significantly between the two groups. Whites and individuals with greater income were more likely to use statins; in addition, they also had higher odds for developing AMD. Those using statins also had a greater chance of reporting higher smoking status (P<0.0001), having poor general health condition (P<0.0001), and prior cataract extraction (P<0.0001). There was also a higher prevalence of cardiovascular-related events (self-reported stroke) among statin users when compared with the other group (P<0.0001).
Statin therapy and AMD
Out of the 441 participants that presented with AMD, 126 (28.6%) were using a statin medication, and from these, 90 participants were older than 68 years; and 315 (71.4%) were not receiving such therapy, of which 206 participants were older than 68 years. Among statin users, the mean length of time on the medication was 57.8 months with a median of 48 month (IQR: 24–96). Those who had early AMD accounted for 386 cases (87.5%), 139 cases in the younger sub-population and 247 in the older; and those with late AMD for 55 cases (12.5%), 6 in the younger sub-population and 49 in the older.
We constructed multivariate logistic regression models to assess the association between statin intake and presence of AMD (Table 2), which adjusted for age, gender, other demographic characteristics, health-related behaviors, comorbidities. and self-reported general health condition. All medical and ocular comorbidities that did not reach statistical significance at the P<0.1 level were excluded from consideration as confounders in the final model. The only medical comorbidity that showed significance was history of stroke. History of prior cataract surgery was the only visual comorbidity retained in the multivariate model.
The initial unadjusted model, using the 40 years or older population from NHANES, showed that statins intake was significantly associated with increased odds of AMD (OR 1.77, 95% CI 1.32–2.38). However, after adjusting for age this previously positive association became a statistically insignificant negative association (OR 0.92, 95% CI 0.68–1.24; P=0.565). Adjusting for demographic characteristics, health-related behaviors such as smoking and alcohol use, and self-reported general health condition and comorbidities, did not change the association or the significance (OR 0.91, 95% CI 0.67–1.24; P=0.539), suggesting that statin therapy was not independently associated with AMD.
A second analysis was performed looking at the association between statins intake and early and late AMD cases, separately. After adjusting for potential confounding factors, early AMD was not significantly associated with the use of statins (OR 0.95, 95% CI 0.67–1.33; P=0.745). Although late AMD also did not show such a significant association, the OR was lower than that found for early AMD (OR 0.78, 95% CI 0.34–1.80; P=0.556).
When looking at the younger sub-population (40–67 years), the results from the multivariate regression model were similar to our initial analysis with increased OR and a significant association in the unadjusted model (OR 2.15, 95% CI 1.26–3.66; P=0.006). After adjusting for age, gender, demographic characteristics, health-related behaviors, comorbidities, and general health condition the association was no longer significant (P=0.154; Table 3). Similarly, early AMD was not independently associated with statin intake for this subgroup (OR 1.61, 95% CI 0.85–3.03; P=0.137). The analysis to assess the relation between late AMD and statins could not be adequately performed, because there were not enough cases of late AMD in this sub-population as only six participants (0.15%) were diagnosed with late AMD of whom only one was receiving statin therapy.
After analyzing the participants who were 68 years of age or older, we found that statin intake was significantly associated with lower odds of AMD compared with no statin use in the unadjusted model (OR 0.64, 95% CI 0.49–0.84; P=0.002). Even after adjusting for all confounding factors and comorbidities this correlation remained significant (OR 0.69, 95% CI 0.51–0.94; P=0.018), indicating a possible protective effect of statins over AMD in this older subgroup. The same significant association was found for early AMD in this sub-population (OR 0.69, 95% CI 0.49–0.97; P=0.032). The odds for having late AMD were also low but did not reach statistical significance in the regression analysis (P=0.623).
Finally, we analyzed the duration of treatment in these two age groups. First looking at the mean duration of treatment, we found that for those younger than 68 years the mean duration of treatment was shorter (43.8 months with a median of 24 months, IQR: 12–60) than for those 68 years and older (61.1 months with a median of 60 months, IQR: 12–96). Second, we did another analysis using the duration of statin use as our predictor and found a trend toward a protective effect with significant lower OR in the older population (P=0.039; Table 4).
Conclusion
The greatest risk factor for AMD is advanced age, with lipid accumulation in the Bruch’s membrane increasing over time. That deposition can inhibit exchange of nutrients at the RPE level leading to the development of AMD lesions.6, 21 Most of the published population-based studies that evaluate AMD and statin use as a protective parameter against this process have evaluated individuals 40 years of age or older. In this cross-sectional study of a US-based, we sought to assess if age could be a determinant in the association using a sample of adults older than 40 years of age in whom the mean age of subjects with AMD was 68 years old, we compared the older subjects (68+years) to the younger participants (40–67 years) to evaluate potential differences in the effect of statins in these subgroups.
In our analysis, among those individuals aged 68 years and older, statin use was associated with significantly lower odds for AMD compared with non-users; however, this protective effect was not observed in the group of participants who were 40–67 years old. One hypothesis that may explain these findings is that the benefit of statin use in the prevention of AMD increases with long-term use.
The risk factors for the development of AMD, which are common to atherosclerotic disease, such as cigarette smoking, high serum cholesterol, and hypertension, suggest analogous etiologies for both conditions.17 In vivo and in vitro studies have reported that statins inhibit the expression of vascular endothelial growth factor, Cc1-2 macrophage recruiting molecules and intercellular adhesion molecule-1, which are well-known factors related to AMD pathogenesis.17 Evidence has been presented that the RPE produces apolipoprotein-B-containing lipoprotein particles that can accumulate and deposit with age, thus creating a barrier to the exchange of essential nutrients, perhaps leading to AMD development.6 In animal experimental studies, high cholesterol levels lead to retinal changes similar to dry AMD, supporting this theory of lipid deposits causing a barrier in the RPE level and subsequent development of AMD lipid-containing lesions.6, 21 Therefore, modification of atherosclerotic processes with lipid-lowering drugs may have a role in the prevention of AMD development or progress.22
Although statins have been widely used to lower lipids in the treatment of atherosclerotic diseases and hyperlipidemia, it is noteworthy that anti-inflammatory and anti-angiogenic effects have also been attributed to this class of drugs.14, 17 These properties can be important to other vascular pathologies and also to AMD.
Sagara et al17 performed an animal study with pitavastatin in 2007 in which the effects of statin therapy on choroidal neovascularization (CNV) in rats was assessed, using doses considered therapeutic for human hypocholesterolemia. Their results showed less fluorescein angiogram leakage, decreased area, and thickness of CNV measured by both angiography and histopathological studies, supporting the anti-angiogenic effect of statins.
In the current literature, the association of statin intake and clinical AMD is a matter of controversy (see Table 5). Most of studies are case–control and population-based cohorts.9, 10, 14, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 There are four randomized clinical trials (RCTs), which evaluated the use of statins and AMD.27, 34, 35, 36 The first RCT by Martini et al36 and two other recent RCTs27, 34 that evaluated statin use and AMD did not find a significant protective association with AMD development. However, Klein et al37 found an inverse association of statin intake and soft drusen.
In terms of population-based evaluations of the association of statins and AMD, the Blue Mountains Eye Study,10 an Australian population-based longitudinal study of 3654 participants aged 49+ years, reported a reduced risk of developing soft drusen in statin users (hazard ratio of 0.33; 95% CI 0.13–0.84). Also, Friedman38 in 2004 and Wilson et al39 in 2004 reported a protective effect of statins intake and AMD development.
Furthermore, a meta-analysis of observational studies was performed in 2007 by Chuo et al14 to examine the effect of lipid-lowering agents in the development of AMD. The authors identified eight studies10, 24, 26, 29, 30, 31, 32, 33 and the pooled relative risk was 0.74 (95% CI 0.55–1.00). The study did not show an association between the use of lipid-lowering medications and the incidence of AMD.
In the 2012 Cochrane Study, Gehlbach et al3 postulate that there is insufficient data to support statins as a preventive or risk factor for AMD. But their results were based on a literature review that selected only two RCTs that met the study criteria with a small number of participants (n=72). In 2011, Shalev et al40 evaluated a larger population of 108 973 individuals aged 55 or older and reported no association between persistent use of statins and reduced risk of AMD among 2732 incident AMD cases in individuals.
The possible disparate findings in the previous studies may be related to the composition of the groups in terms of age and duration of statin use. It is likely that one explanation for the difference in protective effect between our two age groups is due to duration of statin use, which was statistically different. Recently, Tan et al10 found that statin use may reduce the long-term risk of developing AMD after a 10-year follow-up of the initial baseline population, which could be a result of the longer duration of treatment in that population. In support of this finding, in the older age group of our study, greater duration of statin use was associated with less likelihood of AMD.
Our results show that the mean duration of statin use in participants 68 years of age or older is associated with lower risk for AMD, suggesting a possible protective effect of statins against AMD in elderly individuals (ie, ≥68 years old), but this can be a result of a relatively small sample effect (N=441 AMD cases). Although there are many strengths of this study such as a nationwide, multiracial population-based sample, and AMD detection by an objective system for grading fundus digital photographs, the study is subject to several limitations. It may underestimate the number of persons with AMD, because some fundus photos were excluded in the survey, due to poor image quality (n=224) or non-existent photos (n=969). Moreover, only 0.15% of the population studied had late AMD. Such small numbers of late AMD cases can lead to low statistical power to detect an association between statin intake and late AMD. Yet, the prevalence rates of both late and early AMD were similar to other population-based studies.24
In summary, we found that after adjustment for confounding factors statin intake has significantly lower odds for AMD in individuals 68 years of age or older. This association, if confirmed in other independent data sets, may be due to anti-inflammatory and/or lipid-lowering properties of statin drugs. Additional prospective research elucidating the potential protective effect of statin intake and development of AMD is required. As dry AMD is the most common form of the disease including in this study, our findings may enhance therapeutic interest in dry AMD.

References
Fernandez AB, Wong TY, Klein R, Collins D, Burke G, Cotch MF et al. Age-related macular degeneration and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Ophthalmology 2012; 119 (4): 765–770.
Garcia Lozano I, Lopez Garcia S, Elosua de Juan I . [Management of age-related macular degeneration. An update]. Revista Espanola de Geriatria y Gerontologia 2012; 47 (5): 214–219.
Gehlbach P, Li T, Hatef E . Statins for age-related macular degeneration. Cochrane Database Syst Rev 2012; 3: CD006927.
Klein R, Chou CF, Klein BE, Zhang X, Meuer SM, Saaddine JB . Prevalence of age-related macular degeneration in the US population. Arch Ophthalmol 2011; 129 (1): 75–80.
Choudhury F, Varma R, McKean-Cowdin R, Klein R, Azen SP . Risk factors for four-year incidence and progression of age-related macular degeneration: the Los Angeles Latino Eye Study. Am J Ophthalmol 2011; 152 (3): 385–395.
Kishan AU, Modjtahedi BS, Martins EN, Modjtahedi SP, Morse LS . Lipids and age-related macular degeneration. Surv Ophthalmol 2011; 56 (3): 195–213.
Delcourt C, Michel F, Colvez A, Lacroux A, Delage M, Vernet MH . Associations of cardiovascular disease and its risk factors with age-related macular degeneration: the POLA study. Ophthalmic Epidemiol 2001; 8 (4): 237–249.
Damico FM, Gasparin F, Scolari MR, Pedral LS, Takahashi BS . New approaches and potential treatments for dry age-related macular degeneration. Arquivos Brasileiros de Oftalmologia 2012; 75 (1): 71–76.
Fong DS, Contreras R . Recent statin use and 1-year incidence of exudative age-related macular degeneration. Am J Ophthalmol 2010; 149 (6): 955–958 e951.
Tan JS, Mitchell P, Rochtchina E, Wang JJ . Statins and the long-term risk of incident age-related macular degeneration: the Blue Mountains Eye Study. Am J Ophthalmol 2007; 143 (4): 685–687.
Vingerling JR, Dielemans I, Bots ML, Hofman A, Grobbee DE, de Jong PT . Age-related macular degeneration is associated with atherosclerosis. The Rotterdam Study. Am J Epidemiol 1995; 142 (4): 404–409.
Machalinska A, Kawa MP, Marlicz W, Machalinski B . Complement system activation and endothelial dysfunction in patients with age-related macular degeneration (AMD): possible relationship between AMD and atherosclerosis. Acta Ophthalmologica 2012; 90 (8): 695–703.
Peponis V, Chalkiadakis SE, Bonovas S, Sitaras NM . The controversy over the association between statins use and progression of age-related macular degeneration: a mini review. Clin Ophthalmol 2010; 4: 865–869.
Chuo JY, Wiens M, Etminan M, Maberley DA . Use of lipid-lowering agents for the prevention of age-related macular degeneration: a meta-analysis of observational studies. Ophthalmic Epidemiol 2007; 14 (6): 367–374.
Tobert JA . Lovastatin and beyond: the history of the HMG-CoA reductase inhibitors. Nat Rev Drug Discovery 2003; 2 (7): 517–526.
Beri A, Sural N, Mahajan SB . Non-atheroprotective effects of statins: a systematic review. Am J Cardiovasc Drugs 2009; 9 (6): 361–370.
Sagara N, Kawaji T, Takano A, Inomata Y, Inatani M, Fukushima M et al. Effect of pitavastatin on experimental choroidal neovascularization in rats. Exp Eye Res 2007; 84 (6): 1074–1080.
Wong IY, Koo SC, Chan CW . Prevention of age-related macular degeneration. Int Ophthalmol 2011; 31 (1): 73–82.
National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: survey questionnaires, examination components and laboratory components 2007-2008, http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/questexam07_08.htm. Accessed 29 May 2012.
National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: survey operations manuals, brochures, consent documents. NHANES 2007-2008, http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/current_nhanes_07_08.htm. Accessed 29 May 2012.
Curcio CA, Johnson M, Huang JD, Rudolf M . Aging, age-related macular degeneration, and the response-to-retention of apolipoprotein B-containing lipoproteins. Prog Retinal Eye Res 2009; 28 (6): 393–422.
Hall NF, Gale CR, Syddall H, Phillips DI, Martyn CN . Risk of macular degeneration in users of statins: cross sectional study. BMJ 2001; 323 (7309): 375–376.
Drobek-Slowik M, Karczewicz D, Safranow K, Jakubowska K, Chlubek D . [Use of statins as a form of protection against age-related macular degeneration (AMD)]. Klinika Oczna 2008; 110 (1-3): 50–54.
Friedman E . The role of the atherosclerotic process in the pathogenesis of age-related macular degeneration. Am J Ophthalmol 2000; 130 (5): 658–663.
Kaiserman N, Vinker S, Kaiserman I . Statins do not decrease the risk for wet age-related macular degeneration. Curr Eye Res 2009; 34 (4): 304–310.
Klein R, Klein BE, Tomany SC, Danforth LG, Cruickshanks KJ . Relation of statin use to the 5-year incidence and progression of age-related maculopathy. Arch Ophthalmol 2003; 121 (8): 1151–1155.
Klein R, Knudtson MD, Klein BE . Statin use and the five-year incidence and progression of age-related macular degeneration. Am J Ophthalmol 2007; 144 (1): 1–6.
McCarty CA, Mukesh BN, Guymer RH, Baird PN, Taylor HR . Cholesterol-lowering medications reduce the risk of age-related maculopathy progression. Med J Australia 2001; 175 (6): 340.
McGwin Jr G, Modjarrad K, Hall TA, Xie A, Owsley C . 3-Hydroxy-3-methylglutaryl coenzyme a reductase inhibitors and the presence of age-related macular degeneration in the Cardiovascular Health Study. Arch Ophthalmol 2006; 124 (1): 33–37.
McGwin Jr G, Owsley C, Curcio CA, Crain RJ . The association between statin use and age related maculopathy. Br J Ophthalmol 2003; 87 (9): 1121–1125.
McGwin Jr G, Xie A, Owsley C . The use of cholesterol-lowering medications and age-related macular degeneration. Ophthalmology 2005; 112 (3): 488–494.
Smeeth L, Cook C, Chakravarthy U, Hubbard R, Fletcher AE . A case control study of age related macular degeneration and use of statins. Br J Ophthalmol 2005; 89 (9): 1171–1175.
van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT . The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Arch Ophthalmol 2003; 121 (4): 519–526.
Maguire MG, Ying GS, McCannel CA, Liu C, Dai Y . Statin use and the incidence of advanced age-related macular degeneration in the Complications of Age-related Macular Degeneration Prevention Trial. Ophthalmology 2009; 116 (12): 2381–2385.
Guymer RH, Dimitrov PN, Varsamidis M, Lim LL, Baird PN, Vingrys AJ et al. Can HMG Co-A reductase inhibitors (‘statins’) slow the progression of age-related macular degeneration? The age-related maculopathy statin study (ARMSS). Clin Interventions Aging 2008; 3 (3): 581–593.
Martini E, Scorolli L, Burgagni MS, Fessehaie S . Valutazione degli effetti retinici della somministrazione di simvastatina in pazienti affetti da degenerazione maculare senile. Annali Di Ottalmologia e Clinica Oculistica 1991; 117 (11): 1121–1126.
Klein R, Cruickshanks KJ, Nash SD, Krantz EM, Nieto FJ, Huang GH et al. The prevalence of age-related macular degeneration and associated risk factors. Arch Ophthalmol 2010; 128 (6): 750–758.
Friedman E . Update of the vascular model of AMD. Br J Ophthalmol 2004; 88 (2): 161–163.
Wilson HL, Schwartz DM, Bhatt HR, McCulloch CE, Duncan JL . Statin and aspirin therapy are associated with decreased rates of choroidal neovascularization among patients with age-related macular degeneration. Am J Ophthalmol 2004; 137 (4): 615–624.
Shalev V, Sror M, Goldshtein I, Kokia E, Chodick G . Statin use and the risk of age related macular degeneration in a large health organization in Israel. Ophthalmic Epidemiol 2011; 18 (2): 83–90.
Acknowledgements
This study was supported by NIH-NEI EY002162—Core Grant for Vision Research, That Man May See, Inc., Research to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Barbosa, D., Mendes, T., Cíntron-Colon, H. et al. Age-related macular degeneration and protective effect of HMG Co-A reductase inhibitors (statins): results from the National Health and Nutrition Examination Survey 2005–2008. Eye 28, 472–480 (2014). https://doi.org/10.1038/eye.2014.8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.8
Keywords
This article is cited by
-
‘Statins in retinal disease’
Eye (2018)
-
The association between statin use and risk of age-related macular degeneration
Scientific Reports (2015)