Abstract
Purpose
To compare the outcomes of phacoemulsification with either a 2.5-mm clear corneal incision and a foldable intraocular lens (IOL) or a 5-mm sclerocorneal tunnel incision and a rigid polymethyl methacrylate (PMMA) IOL.
Methods
In a prospective, randomised clinical trial of phacoemulsification cataract surgery, 1200 patients received either a foldable hydrophilic acrylic IOL through a 2.5-mm corneal incision or an inexpensive rigid PMMA IOL via a 5-mm sclerocorneal tunnel. Intra- and post-operative data and visual acuity at discharge, 6 weeks, and 1 year follow-up were analysed.
Results
At 1 year after surgery, 996 (83.0%) patients were followed up with an uncorrected visual acuity of 6/18 or better in 90.3% of the foldable and 94.3% in the rigid IOL group (risk ratio (RR) 0.96, 95% confidence intervals (CI) 0.92–0.99). Poor outcome (best-corrected acuity 6/60 or worse) occurred in 1.0% and 0.4%, respectively (RR 4.28, 95% CI 0.48–38.18). The surgical cost of consumables and overall surgical time were similar in both groups; however, the cost of the foldable IOL was eight times higher than the PMMA IOL. Posterior capsule opacification was more common in the rigid IOL group at 12 months (36.1% vs 23.3%); however, this did not affect post-operative vision.
Conclusion
In the hands of experienced cataract surgeons, phacoemulsification with implantation of a foldable or a rigid IOL gives excellent results. Using an inexpensive rigid PMMA IOL will make phacoemulsification more affordable for poor patients in low- and middle-income countries.
Similar content being viewed by others
Introduction
Cataract remains the leading cause of blindness worldwide.1 Although the number of cataract operations has increased as a result of the WHO/IAPB Vision 2020 initiative, poor visual outcome following surgery remains a major concern,2 and population-based studies in Asia, Africa, and Latin America have found that at least 20% of operated cataract patients have a presenting vision <6/60.3, 4, 5 Any surgical method that improves the visual outcome of cataract surgery would be an important contribution to Vision 2020.
Phacoemulsification followed by implantation of a foldable intraocular lens (IOL) is the procedure of choice in higher-income countries. The smaller incision leads to less astigmatism and better visual outcomes after surgery.6 In low- and middle-income countries (LMICs), trials of phacoemulsification vs small incision manual extracapsular cataract surgery (SICS) have had variable results, with two trials showing the superiority of phaco7, 8 and two showing little difference between the two methods.9, 10 However, a recent meta-analysis showed that phacoemulsification was more likely than SICS to give an uncorrected visual acuity of 6/18 or better soon after surgery.11 The equipment required for phacoemulsification is expensive and this technique has not been widely adopted in lower-income settings. However, ophthalmologists in LMICs are buying phacoemulsification machines to provide this service to wealthier patients paying high fees. Having bought the equipment, the main difference in cost between phacoemulsification and SICS is the price of the IOL.12
This study arose from the clinical observation that implanting an inexpensive rigid IOL after phacoemulsification appeared to give visual outcomes comparable to more expensive foldable IOLs.13 We designed this randomised controlled trial in order to make a fair comparison between the two types of IOL following phacoemulsification. The rationale for the study is that, if an inexpensive rigid IOL is as safe and effective as a foldable IOL, phaco could be accessible to patients in LMICs who currently cannot afford a foldable IOL.
The main aim of the trial was to compare the outcome of foldable and rigid IOLs in phacoemulsification cataract surgery.
In particular, the trial aimed to answer the following questions:
-
What is the visual outcome 1 year after surgery? How many patients achieve normal vision in the operated eye and how many patients are no longer visually impaired by WHO definitions?
-
How safe are the lenses? What are the complications during surgery, immediately after surgery and at 1 year after surgery? How many patients have severe visual loss 1 year after surgery that cannot be corrected by the use of spectacles?
-
What are the costs involved? This includes the cost of the lenses and also surgeon time.
Material and methods
The trial was registered with a publicly available database http://www.controlled-trials.com/ ISRCTN63984643. The protocol is available on request.
This was a parallel group randomised controlled trial. Participants were randomly allocated 1 : 1 to foldable or rigid lenses and were followed up for 1 year. For the 1-year follow-up, we specified that the follow-up should happen between 10 and 14 months after surgery; however, we extended this period to enable us to follow-up as many participants as possible. Otherwise there were no important changes to methods after the trial commenced.
Study participants were people aged 35–70 years, attending Sagarmatha Choudhary Eye Hospital, Lahan, Nepal, for cataract surgery, who had age-related cataract that reduced vision to at least 6/36 in the eye to be operated. Cataract patients, identified in cataract screening camps, were also eligible for inclusion. Only patients residing in three districts close to Lahan (Siraha, Saptari, Udayapur) were eligible to take part.
The following exclusion criteria were applied:
-
Corneal disease (Fuchs’ endothelial dystrophy; corneal stromal scarring)
-
Chronic anterior uveitis
-
Intraocular pressure>22 mm Hg
-
High ametropia (biometry for emmetropia: <17.0 dpt, >26.0 dpt)
-
Any other eye disease
-
Very advanced hard lens nuclei, where phacoemulsification was not considered to be suitable (grade III+)
-
Diabetes mellitus
This study complied with all local laws and the principles of the Declaration of Helsinki. Approval was obtained by the Research Ethical Review Board of Nepal Netra Jyoti Sangh, as well as by the Ethics Committee of the London School of Hygiene & Tropical Medicine. Informed written consent was obtained from every participant and a witness.
The randomisation sequence was computer generated using Microsoft Excel random function. Simple randomisation was used. The allocation was delivered in serially numbered, sealed opaque envelopes, each containing an adhesive label with the study number and allocation. The sequence was generated in the UK by JE and was sent to an administrative member of staff in Nepal who prepared the envelopes. The envelope was opened in the operating theatre, just before the operation, and the adhesive label stuck into the patient's study book. No one involved in recruiting and treating the patients in the trial was involved in any aspect of the production and concealment of the allocation sequence. Patients were not told which lens they had received.
The operation was performed by either one of the two surgeons (AH, LRP) in equal distribution. Both surgeons have experience of several thousands of phaco surgeries using foldable and polymethyl methacrylate (PMMA) IOLs.
For rigid IOL, a small fornix-based conjunctival flap was prepared. After cauterisation of blood vessels a sclerocorneal tunnel, 1.5 mm behind the limbus, with a 2.5-mm anterior chamber opening was performed. In the case of a foldable IOL, a 2.5-mm clear corneal incision was performed. These incisions were made superiorly in all patients, irrespective of pre-operative keratometry.
A continuous curvilinear capsulorhexis was performed with Utrata forceps. In case of poor capsule visibility, the capsule was stained with Trypan Blue. After hydrodissection and hydrodelineation, the nucleus was removed by phacoemulsification, using the phaco chop technique (phaco machines: OS-3 OERTLI Instruments, Berneck, Switzerland and Megatron Geuder AG, Heidelberg, Germany). The remaining cortex was removed with Simcoe cannula and/or bimanual irrigation/aspiration system. In the case of a rigid IOL, the sclerocorneal incision was enlarged to 5 mm and a 5-mm optic PMMA IOL (IOCare, India, Style: PH5, cost: USD 2.50) was inserted into the capsular bag. In the case of a foldable IOL, the 6-mm optic IOL (hydrophilic acrylic, IOCare, India, Style: RYCF-6, cost: USD 20.63) was inserted with an injector through the 2.5-mm corneal incision and placed in the capsular bag. Any residual viscoelastic solution was removed and intracameral cefuroxime 1 mg was injected. A subconjunctival injection of dexamethasone 4 mg was given in the upper fornix. An eye pad and a shield were applied.
In case of posterior capsule rupture, vitrectomy was performed and the IOL was placed either in the capsular bag or in the sulcus. If there was insufficient capsular support, an AC-IOL was implanted.
Post-operative corneal oedema was treated with steroid drops. All other complications such as hyphaema or iritis were treated in the usual way.
All patients were examined on the HS not involved in the surgery. HS was not masked to treatment status as the type of surgery was clear on examination.
Visual acuity was measured on the first post-operative day, using an E chart (illuminated vision drum) by an experienced ophthalmic assistant who was masked to treatment group. When measuring visual acuity these assistants could not tell which lens the patient had received. It is possible that they may have been able to identify the lens used from the patients’ notes; however, they were not informed of the hypothesis behind the study.
Each line was tested using four optotypes. Visual acuity was taken as the last line on which three or four optotypes were read correctly. Uncorrected visual acuity in the operated eye was recorded. In case of borderline or poor visual outcome (uncorrected acuity worse than 6/18), HS recorded the reason.
The patient was discharged on the second post-operative day with the patient identity card, which included the expected date of follow-up. Patients were encouraged to come to the hospital for follow-up after 6 weeks and 1 year. Financial compensation was available for any expenses that participants might incur while attending the follow-up.
When a patient returned to the hospital for the 6-week and 1-year appointment, it was confirmed that the correct person was examined by matching the name and photo on the record form and personal identity card. Uncorrected and best-corrected visual acuity were recorded. Keratometry was performed, astigmatism and axis, expressed in minus cylinder, were recorded. Slit-lamp biomicroscopic examination by an ophthalmologist (HS) was recorded, reasons for borderline and poor outcome were also recorded.
Follow-up was monitored with reference to the study diary. If a patient did not return for the follow-up, a motivator visited him/her and tried to bring him/her to the hospital for examination. If this failed, the patient was examined in the village, which included the same as in the hospital, except keratometry and auto-refractometry.
The primary outcome measure was visual acuity at 1 year after surgery in the operated eye. Vision was measured using a Snellen E chart at 6 m. We pre-defined the following cutpoints:
-
Uncorrected visual acuity of 6/9 or more (ie, very good functional vision)
-
Uncorrected visual acuity of 6/18 or more (ie, operated eye is no longer ‘visually impaired’ by WHO definitions)
-
Best-corrected visual acuity worse than 6/60 (ie, eye is effectively blind)
The secondary outcome measures were:
-
Visual acuity in the operated eye at other time points
-
Complications during surgery
-
Early post-operative complications
-
Long-term complications
-
Astigmatism
-
Cost
Poor outcomes were presumed to be due to refractive error if the uncorrected visual acuity was <6/18, but the corrected acuity was 6/18 or better. If the spherical equivalent was within 1 dpt of emmetropia, the poor outcome was assumed to be due to astigmatism. If the spherical equivalent exceeded 1 dpt of ametropia, the poor outcome was judged to be the result of inaccurate biometry.
There were no changes to the outcome measures after the trial commenced. We have reported all the outcomes for which we collected data.
The sample size was calculated assuming that the two lenses would give similar results and we have used the method of Bland.14 We estimated that a total sample size of 1200 would enable us to estimate the difference between the two proportions to within ∼5 percentage points. We anticipated that 35% of the group receiving foldable lenses would achieve visual acuity of 6/9 or better and 80% would achieve vision of 6/18 or better at 1 year.7, 8 We anticipated that 80% of the participants would be followed up at 1 year. We knew that the occurrence of many of the secondary outcomes would be too infrequent for this study to detect differences.
We did not plan any interim analyses because both lenses are in common use in our hospital and elsewhere, and we had previously published data on a large cohort of patients documenting the outcome of the procedure.13
A separate study book for each participant was prepared including a photo, detailed address and separate pages for data on recruitment, surgery, discharge, and 6-week and 1-year follow-up. Computer data entry was done by two different persons, then validated by a third person for corrections.
The majority of the analyses consisted of simple cross-tabulations of the outcomes by the intervention group accompanied by a χ2- or t-test, as appropriate. For the primary outcomes, our main effect measure was the risk ratio (RR) that we report with 95% confidence intervals (CIs). We did not plan any subgroup or adjusted analyses. All analyses were done with Stata version 12 (StataCorp, College Station, TX, USA).
Results
Recruitment took place between 24 September 2010 and 16 September 2011. A total of 1200 people were enrolled in the trial, 589 people were randomly allocated to receive a foldable lens and 611 to receive a rigid lens (Figure 1). There were no exclusions after randomisation. Table 1 shows the characteristics of the study population and surgery.
At 6 weeks after surgery, 977 (81.4%) participants were followed up with similar number of people in foldable group and rigid group (80.1% vs 82.7%). The median 6-week follow-up in the foldable group was 42 days (range 26–207) and in the rigid group 42 days (range 27–207). At 1 year after surgery, 996 (83.0%) participants were followed up with similar number of people in foldable group and rigid group followed up (81.7% vs 84.3%). The median 1-year follow-up in the foldable group was 395 days (range 135– 693) and in the rigid group 394 days (range 250–706). People with worse pre-operative visual acuity were less likely to be followed up at 6 weeks and 1 year.
Table 2 shows the visual acuity outcomes in the operated eye at discharge, 6 weeks, and 1 year after surgery.
People in the foldable group were less likely to achieve uncorrected visual acuity of 6/9 or better at discharge (RR 0.78, 95% CI 0.65–0.92), at 6 weeks (RR 0.80, 95% CI 0.67–0.96), and 1 year (RR 0.94, 95% CI 0.82–1.07). Note that the difference at 1 year was not statistically significant—the 95% confidence intervals for the estimate range from 0.82–1.07.
People in the foldable group were less likely to achieve uncorrected visual acuity of 6/18 or better at discharge (RR 0.96, 95% CI 0.93–0.98), 6 weeks (RR 0.97, 95% CI 0.93–1.002), and 1 year (RR 0.96, 95% CI 0.92–0.99).
More number of people in the foldable group had best-corrected visual acuity of <6/60, but the numbers of events were small, and the resulting wide confidence intervals are compatible with more or fewer cases of poor vision in either group at 6 weeks (RR 3.20, 95% CI 0.33–30.69) and 1 year after surgery (RR 4.28, 95% CI 0.48–38.18).
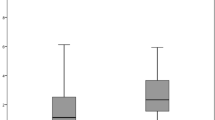
Table 3 shows the post-operative refractive errors in a more detailed manner. At 6 weeks, 116 eyes with foldable IOL had a spherical error of 1D or greater, compared with 68 rigid IOL (RR 2.09, 95% CI 1.5–2.91). By 1 year, this difference had disappeared. There was little difference in the astigmatic error between the two groups.
The assessor recorded the reasons for visual acuity worse than 6/60 at discharge. There were five cases, all in the foldable lens group. Three of these were thought be due to undetected pre-existing comorbidity that was unrelated to surgery, one was related to surgery, and one was due to refractive error.
Tables 4 and 5 summarise the complications recorded during surgery, at discharge, and at 6 weeks and 1 year, and the amount and type of posterior capsule opacification (PCO) at 1 year after surgery. PCO was significantly more common in the rigid PMMA IOL group. However, PCO reducing the vision to <6/9 was uncommon, and there was no significant difference between the two groups.
Table 6 shows the reasons for uncorrected visual acuity <6/18 at 6 weeks and 1 year. The majority of cases of uncorrected visual acuity were attributed to refractive error.
Discussion
Strictly speaking, this trial does not compare two different IOLs but two different surgical techniques—one using a low-cost rigid PMMA IOL inserted through a 5-mm sclerocorneal incision and the other using a more expensive foldable hydrophilic acrylic IOL inserted through a 2.5-mm corneal incision. However, this does not invalidate our main conclusion that the two techniques give comparable results. Indeed, the low-cost rigid IOL appears to be more likely to achieve early visual rehabilitation than the more expensive foldable IOL.
The inclusion criteria specified that patients should come from one of the three districts surrounding the hospital, in order to reduce loss in follow-up. During the 12-month recruitment period, ∼4000 patients from these districts had cataract surgery at Lahan, but only 1200 were included in the trial. This was because recruitment proceeded only if at least one of the two participating surgeons was available. We have no reason to believe that the sample included in the trial is unrepresentative of the population.
Although over 80% of patients were seen at the 1-year follow-up, the follow-up intervals were variable, and 17% of patients were not seen at 12 months. The wide variations in follow-up were evenly distributed between the two study groups and are unlikely to bias our results. Patients with worse vision at presentation were less likely to attend the 1-year follow-up, and it is possible that these patients may have had different outcomes. However, among patients who were blind at presentation, and who did attend for follow-up, there is no evidence that their outcomes were different compared with those who had a visual acuity of 3/60 or better.
Because of the differences in the physical appearance of the IOLs, it was impossible to mask the observers completely. However, primary outcome was visual acuity, and this was measured before examination, so it would not have been apparent as to which IOL had been used.
It has been shown that different IOL designs and materials significantly affect the incidence of PCO.15 Acrylic IOLs are associated with a lower rate of capsule opacity than rigid PMMA lenses. It is possible that a longer follow-up period would show an increased benefit from foldable acrylic IOL as the rigid PMMA IOL are more affected by capsule opacity. The increased risk of capsule opacification in rigid PMMA IOLs can be reduced by a square edge design of the optic. Only the foldable IOLs used in this trial had a square edge design. Central PCO was present at the time of surgery in 10.9% of the foldable and 8.8% of the rigid lens group. This is commonly found with advanced cataracts in LMICs.16
The better uncorrected visions at discharge and 6 weeks in the rigid PMMA IOL group were unexpected. We believe this is due to lower spherical equivalent refractive error in these eyes. We speculate that the foldable IOLs required some capsular contraction to move the optic to the correct AC depth, which would explain the difference at 6 weeks and its resolution by 1 year. At 1 year, 85.4% of patients had a spherical equivalent refractive error <1 dpt, and only 1.9% had a spherical equivalent error >2 dpt, which suggests that there is little that can be done to improve the accuracy of biometry, particularly, as over 80% of the operated eyes had a pre-operative vision <6/60.17
We did not calculate the surgical induced astigmatism, and no attempt was made to reduce post-operative astigmatism by the positioning of incisions. The numbers of patients with unaided VA <6/18 was similar in the two groups at 1 year, and in both groups uncorrected refractive error was the most common cause. There was no difference in the average astigmatism at 6 weeks or 1 year (Table 4). It is well known that moving the incision posteriorly reduces surgically induced astigmatism.18, 19 Although the 5-mm incision for the rigid IOL is wider than the incision for the foldable IOL, because it is further posterior, it appears to be astigmatically neutral. Some of the poor refractive outcomes were due to astigmatism, and this might be reduced by on-axis placement of incisions. However, this would increase the surgical time for many of the patients, and only 36 (3.6%) patients had an uncorrected vision <6/18 due to astigmatism at 1 year. As the leading cause of poor unaided vision was residual refractive error, this underlines the requirement for accurate post-operative refraction and provision of spectacles, following cataract surgery, whatever surgical technique is used.
This trial used two very experienced surgeons (AH and LRP), each of them has done thousands of phacoemulsifications and SICS. They are able to make scleral tunnel and corneal incisions equally swiftly and effectively. Surgeons with less breadth of experience may not achieve such excellent results.
The study assumes that surgeons will be equally at home with the scleral tunnel of SICS as they are with the standard corneal incision of phacoemulsification. This is likely to be true for most LMICs. Although a clear corneal incision is faster than a sclerocorneal tunnel, it takes longer to remove the lens cortex through a smaller incision. Ultimately, there was little difference in the total surgical time between the two groups. In developed countries, most surgeons are accustomed to a corneal wound, and a scleral tunnel incision would be more time-consuming.
In high-income countries, phacoemulsification equipment often uses large disposable packs, containing all the items needed for the surgery. Tubing and cassettes are also disposable. This means that the cost of the foldable IOL is a relatively small part of the cost of consumables, so a switch from a foldable IOL to a rigid PMMA IOL is less likely to result in significant reductions in the cost of surgery. In LMICs, disposables, including IOLs, are generally purchased separately, and the IOL is the major part of the additional cost. The foldable IOL used in our study is 8.3 times more expensive than the rigid PMMA IOL.
This study was carried out in Asia, but there is no reason to believe that the results would differ in Africa or Latin America. A randomised trial of phacoemulsification vs SICS in South Africa produced results that are very similar to trials carried out in South Asia.7, 8, 10
Provided surgeons are equally proficient at sclerocorneal tunnel and clear corneal incisions, the visual outcomes with rigid PMMA IOLs following phaco are at least as good as, if not better than, foldable IOLs at a much lower cost. As the greater expense of the foldable IOL accounts for a considerable portion of the additional cost of phacoemulsification in LMICs, this study demonstrates that the benefits of phacoemulsification can be made available to patients who are unable to afford a foldable IOL without any risk of worse short-term outcomes.
In the longer term, there may be an increased risk of PCO in eyes with a rigid PMMA IOL; however, this is not visually significant at 1 year.

References
Pascolini D, Mariotti SP . Global estimates of visual impairment: 2010. Br J Ophthalmol 2012; 96 (5): 614–618.
Lindfield R, Vishwanath K, Ngounou F, Khanna RC . The challenges in improving outcome of cataract surgery in low and middle income countries. Indian J Ophthalmol 2012; 60 (5): 464–469.
Polack S, Yorston D, Lopez-Ramos A, Lepe-Orta S, Baia RM, Alves L et al. Rapid assessment of avoidable blindness and diabetic retinopathy in Chiapas, Mexico. Ophthalmology 2012; 119 (5): 1033–1040.
Lindfield R, Griffiths U, Bozzani F, Mumba M, Munsanje J . A rapid assessment of avoidable blindness in Southern Zambia. PLoS One 2012; 7 (6): e38483.
Al Ghamdi AH, Rabiu M, Hajar S, Yorston D, Kuper H, Polack S . Rapid assessment of avoidable blindness and diabetic retinopathy in Taif, Saudi Arabia. Br J Ophthalmol 2012; 96 (9): 1168–1172.
Riaz Y, Mehta JS, Wormald R, Evans JR, Foster A, Ravilla T et al. Surgical interventions for age-related cataract. Cochrane Database Syst Rev 2006; (4): CD001323 doi:10.1002/14651858.CD001323.pub2.
Gogate PM, Kulkarni SR, Krishnaiah S, Deshpande RD, Joshi SA, Palimkar A et al. Safety and efficacy of phacoemulsification compared with manual small-incision cataract surgery by a randomized controlled clinical trial: six-week results. Ophthalmology 2005; 112 (5): 869–874.
Cook C, Carrara H, Myer L . Phaco-emulsification versus manual small-incision cataract surgery in South Africa. S Afr Med J 2012; 102 (6): 537–540.
Ruit S, Tabin G, Chang D, Bajracharya L, Kline DC, Richheimer W et al. A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular cataract surgery in Nepal. Am J Ophthalmol 2007; 143 (1): 32–38.
Venkatesh R, Tan CS, Sengupta S, Ravindran RD, Krishnan KT, Chang DF . Phacoemulsification versus manual small-incision cataract surgery for white cataract. J Cataract Refract Surg 2010; 36 (11): 1849–1854.
Riaz Y, de Silva SR, Evans JR . Manual small incision cataract surgery (MSICS) with posterior chamber intraocular lens versus phacoemulsification with posterior chamber intraocular lens for age-related cataract. Cochrane Database Syst Rev 2013; 10: CD008813.
Gogate P, Deshpande M, Nirmalan PK . Why do phacoemulsification? Manual small-incision cataract surgery is almost as effective, but less expensive. Ophthalmology 2007; 114 (5): 965–968.
Hennig A, Singh S, Winter I, Yorston D . Can phaco be a cost-effective solution to cataract blindness? Costs and outcomes in Nepal. Eye (Lond) 2010; 24 (6): 1104.
Bland JM . The tyranny of power: is there a better way to calculate sample size? BMJ 2009; 339, doi: 10.1136/bmj.b3985 b3985.
Cheng JW, Wei RL, Cai JP, Xi GL, Zhu H, Li Y et al. Efficacy of different intraocular lens materials and optic edge designs in preventing posterior capsular opacification: a meta-analysis. Am J Ophthalmol 2007; 143 (3): 428–436.
Peng Q, Hennig A, Vasavada AR, Apple DJ . Posterior capsular plaque: a common feature of cataract surgery in the developing world. Am J Ophthalmol 1998; 125 (5): 621–626.
Daniel C, Tuft S, Ionides A, Bunce C . Effect of visual acuity on biometry prediction error after cataract surgery. J Cataract Refract Surg 2003; 29 (7): 1365–1369.
Koch Paul S . Structural analysis of cataract incision construction. J Cataract Refract Surg 1991; 17 (Suppl): 661–667.
Fine IH, Hoffman RS, Packer M . Incision construction. In: Steinert RF (ed). Cataract Surgery. WB Saunders, Elsevier: Philadelphia, 2010 pp 141–162.
Acknowledgements
We thank the SCEH team, in particular Sudhir Thakur, for managing patient follow-up and data entry, and Ganesh Prasad Upadhyay, Chandra Narayan Choudhary, and Mahendra Mahato for assisting study patients during hospital stay.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hennig, A., Puri, L., Sharma, H. et al. Foldable vs rigid lenses after phacoemulsification for cataract surgery: a randomised controlled trial. Eye 28, 567–575 (2014). https://doi.org/10.1038/eye.2014.26
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.26
Keywords
This article is cited by
-
Phacoemulsification Cataract Surgery Affects the Discriminative Capacity of Iris Pattern Recognition
Scientific Reports (2019)