Abstract
Purpose
To determine the effect of oral acetazolamide on lowering the peak and duration of intraocular pressure (IOP) rise in glaucoma and glaucoma suspect patients, following intravitreal injection of ranibizumab for neovascular age-related macular degeneration.
Methods
The study was an open-label, parallel, randomised, controlled trial (EudraCT Number: 2010-023037-35). Twenty-four glaucoma or glaucoma suspect patients received either 500 mg acetazolamide or no treatment 60–90 min before 0.5 mg ranibizumab. The primary outcome measure was the difference in IOP immediately after injection (T0) and 5, 10, and 30 min following injection. ANCOVA was used to compare groups, adjusting for baseline IOP. The study was powered to detect a 9-mm Hg difference at T0.
Results
The IOP at T0 was 2.3 mm Hg higher in the non-treated group (mean 44.5 mm Hg, range (19–86 mm Hg)) compared with the treated group (mean 42.2 mm Hg, range (25–58 mm Hg)), but was not statistically significant after adjusting for baseline IOP (P=0.440). At 30 min, IOP was 4.9 mm Hg higher in the non-treated group (mean 20.6 mm Hg, range (11–46 mm Hg)) compared with the treated group (mean 15.7 mm Hg, range (8–21 mm Hg)). This was statistically significant after adjusting for baseline IOP (P=0.013).
Conclusions
Although the primary end points were not reached, 500 mg oral acetazolamide, 60–90 min before intravitreal injection, results in a statistically significant reduction in IOP at 3O min post injection. Prophylactic treatment may be considered as an option to minimise neuro-retinal rim damage in high-risk glaucoma patients who are most vulnerable to IOP spikes and undergoing repeated intravitreal injections of ranibizumab.
Similar content being viewed by others
Introduction
Neovascular age-related macular degeneration (nAMD) is characterised by the abnormal proliferation of blood vessels at the macula that leak and haemorrhage, often leading to severe loss of central vision. Vascular endothelial growth factor A (VEGF-A) is a key cytokine that promotes angiogenesis and vascular permeability, and treatment with anti-VEGF therapy leads to preservation of vision.1
Ranibizumab is a recombinant, humanized monoclonal antibody that is administered by intravitreal injection. It binds and neutralizes all active forms of VEGF-A but only has a short duration of clinical effect (of ∼30 days).1 Regular treatment is required to maintain disease stability, with treatment providing disease suppression rather than cure in the majority of patients.1, 2 In routine clinical practice the mean number of injections is ∼6.0 in year 1 and 3.5 in year 2.3 In the Seven-Up study, an observation of the 4 years following on from landmark clinical studies, a mean of approximately two anti-VEGF injections per year was reported.4
Several studies report the extent and duration of intraocular pressure (IOP) elevation following intravitreal injections and most conclude that there is an immediate pressure rise with a slow normalisation of IOP to <30 mm Hg within the subsequent 30 min.5, 6 Debate exists as to whether patients with glaucoma, a condition characterised by peripheral visual field loss and raised IOP, have a different pattern of pressure rise.5, 7, 8
IOP spikes and sustained IOP elevation cause progression of glaucoma. Frenkel et al9 studied prophylactic medication to prevent IOP rise in patients undergoing intravitreal therapy and concluded that they are essentially ineffective, but to the best of our knowledge no study has investigated prophylactic treatment in exclusively glaucoma or glaucoma suspect patients.
The aim of this study is to determine the effect of oral acetazolamide on lowering the peak and duration of IOP rise in glaucoma and glaucoma suspect patients, following an injection of ranibizumab for nAMD.
Materials and methods
Patients with a pre-existing diagnosis of glaucoma or glaucoma suspect undergoing routine ranibizumab intravitreal injections for nAMD in a dedicated treatment clinic were identified. Participants meeting the criteria outlined in Table 1 were randomised to receive, 60–90 min prior to injection, either 500 mg oral acetazolamide or no acetazolamide at a ratio of 1 : 1. The schedule was generated using randomisation software and the allocations were placed in opaque, sequentially numbered envelopes that were sealed. The sequence and envelopes were prepared by a member of staff with no involvement in the study. The randomisation envelopes were held in the Pharmacy department and opened by the trial pharmacist.
Ranibizumab (0.5 mg/0.05 ml) was administered using a 30-gauge needle following The Royal College of Ophthalmologists Guidelines for Intravitreal Injections Procedure 2009 (http://www.rcophth.ac.uk/page.asp?section=451§ionTitle=Clinical+Guidelines).
IOP was measured before treatment (Baseline, TB) immediately after injection (T0) with the patient supine, and at 5 min (T5), 10 min (T10) and 30 min (T30) with the patient upright. A calibrated handheld Tono-Pen (Medtronic Xomed Ophthalmics Inc., Minneapolis, MN, USA) was used for IOP measurements and the reading was validated by a second observer.
Statistical analysis plan
The primary end points were change in IOP from baseline to T0, T5, T10, and T30. Sample size calculation was based on a eye pressure difference of 9 mm Hg between the intervention and non-treated groups at T0. A total of 24 patients (12 in each arm) were required to provide 80% power at the 5% significance level.
Baseline observations of age, sex, race, existing ocular glaucoma and treatments were summarised using means (standard deviations), medians (inter-quartile ranges), and proportions (percentage). The study was analysed using Intention to Treat analysis (ITT). For the primary analysis, repeated-measure ANOVA was used to compare IOP over time, and ANCOVA was used to compare the IOP between the two groups at each time point. These analyses were adjusted for baseline IOP (TB). A P-value of <0.05 was considered to indicate statistical significance. All analyses were undertaken on SPSS version 18.0 (IBM, Portsmouth, UK).
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed in this research in accordance with the Declaration of Helsinki (EudraCT number: 2010-023037-35).
Results
Twenty-four participants gave consent to participate, were randomised, and completed the study. The two groups appeared to be well balanced for baseline characteristics (Table 2).
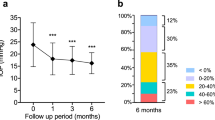
Repeated-ANOVA measurements showed a reduction in IOP from T0 to T30 (P<0.001). There was no difference in this reduction between the treated and untreated groups (P=0.459, Figure 1 and Table 3).
For ANCOVA analysis, no adjustments for co-variates were made. No significant differences between the groups were observed at T0, T5, or T10 (Table 4); however, at T30 a difference of 5.5 mm Hg was observed (SD 0.1, 95% CI 1.3–9.8, P=0.013). No adverse events were reported.
Discussion
This study demonstrates that transient IOP elevations in glaucoma and glaucoma suspect patients immediately after intravitreal injection of ranibizumab are common and can be substantial. This magnitude of elevation has been noticed in patients previously;5, 10, 11 however, glaucoma patients have not been specifically studied. This is the only study the authors are aware of that has a randomised control study design. The results of this study allow future planning of larger randomised controlled trials.
While randomisation determined which of the participants were assigned to the treatment vs control groups, it could be argued that the end baseline characteristic profile of the two groups was asymmetrical in terms of co-medications, glaucoma pathology subsets, and baseline IOP. The investigators appreciate that these factors may influence the results, mindful that the numbers in question are small and should be interpreted as such.
Although the baseline spread of different glaucoma pathologies is presented in Table 2, owing to the small numbers involved no subgroup analysis was carried out. The investigators acknowledge that the different glaucoma pathologies may well have individual influence on IOP trends following intravitreal injections. The inclusion of three patients with functioning trabeculectomies may also confound the results as these patients have ancillary drains and may no longer be as susceptible to IOP rises. The investigators concur that the grouping of patients controlled on different IOP-lowering regimes also does not make provision for differences in IOP responses following intravitreal injections, which may be a confounding factor in interpreting results. Further studies of all these subgroups are required to investigate this further. Now that a mean reduction in IOP has been established, in future, larger studies powered to this figure and using single pathologies can be performed.
Debate continues as to whether glaucoma patients behave differently. In a study of 213 consecutive injections, in 120 eyes of 112 patients, Kim et al5 noted a mean IOP immediately post injection of 44 mm Hg (range 4–87 mm Hg); however, by 30 min all patients had IOP <30 mm Hg. Twenty of these 112 patients had pre-existing glaucoma. They noted that these eyes took significantly longer to achieve an IOP of <30 mm Hg. In the non-treated arm of our study, we demonstrated an almost identical increase in IOP immediately post injections and that not all had an IOP of <30 mm Hg by 30 min. In contrast, a study of intravitreal pegatanib injections showed no statistical significance between the two groups at any time interval, but this study had only 9 glaucoma patients out of 22 and there was no clarity from the series as to which of the patients received prophylactic glaucoma medications.8
Many studies have looked at prevention of IOP spike in the non-glaucoma population. Frenkel et al9 report post-injection spikes, in glaucoma and non-glaucoma eyes, after intravitreal injection of pegatanib, ranibizumab, or bevacizumab. Prophylaxis included up to two topical medications or one topical combined with oral acetazolamide. Topical IOP-lowering medications administered 1 h before injection included timolol maleate, brimonidine tartrate, apraclonidine hydrochloride, and brinzolamide. Oral acetazolamide (500 mg) was administered 2 h before injection. They conclude that the routine use of IOP-lowering medications (topical and oral) is essentially ineffective and the immediate IOP spike after injection is more related to a sheer volume-mediated effect.9
A prospective double-blind placebo controlled study by Theoulakis et al12 concluded that use of Combigan (brimonidine 0.2% and timolol 0.5%) twice a day on the day before and on the day of the intravitreal injection of ranibizumab is a safe and effective prophylaxis to reduce acute IOP spikes in the post-injection period. In this series the IOP was measured before injection and again at 5, 10, 15, and 60 min, crucially missing the high IOP spike immediately after injection.12
We know that other factors can also contribute to acute IOP elevations. These include sheer volume increase inside the eye, which is in turn related to vitreous reflux and needle bore size,5 as well as the actual volume injected.5, 13 This study found no significant reduction in IOP immediately after injection between the control vs treatment group, which further supports the idea of a sheer volume-related pressure effect immediately after injection. Measurement of the IOP just before injection, although not done in this study, may have been useful to confirm the efficacy of pre-injection acetazolamide administered 60–90 min earlier in the treatment arm.
Shorter axial length can also contribute to acute IOP elevations.13 A positive correlation has been found between rigidity coefficient and age,14 which suggests that a similar volume injected into an older more rigid eye might induce a higher IOP.13
Although worth considering, the phakic status and status of vitreous/posterior hyaloid face were not evaluated in this study.
Conclusion
Intravitreal injections are now one of the commonest procedures performed in ophthalmology in a population with a mean age of 80 years with a significant prevalence of glaucomatous optic neuropathy. Protecting patients with pre-existing central visual loss due to nAMD from inadvertent acceleration of peripheral visual loss due to progression of glaucoma is an important consideration. This study has specifically addressed the prevention of IOP rise in glaucoma or glaucoma suspect patients. Although we demonstrate no statistically significant reduction in elevation of IOP at T0, T5, and T10 minutes, there was a reduction at T30 minutes (20.6 vs 15.8 mm Hg), when prophylactic acetazolamide was used 60–90 min before intravitreal ranibizumab injection. Although this is a statistically significant difference, the clinical significance requires further investigation and understanding of the influences of IOP elevations. The investigators advocate that further functional visual field and retinal nerve fibre layer studies are required. It can be argued that this modest reduction in IOP may not be clinically significant in all but those patients with the most vulnerable retinal nerve fibre layers. Equally, caution must be given to the use of acetazolamide because of its side effects such as renal impairment. Further studies of medication that have less chance of systemic side effects are required so as to better inform future practice as well as conserve limited resources in this ever-expanding treatment group.

References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355 (14): 1419–1431.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 2006; 355 (14): 1432–1444.
Ross AH, Donachie PH, Sallam A, Stratton IM, Mohamed Q, Scanlon PH et al. Which visual acuity measurements define high-quality care for patients with neovascular age-related macular degeneration treated with ranibizumab? Eye (Lond) 2013; 27 (1): 56–64.
Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K, SEVEN-UP study group. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology 2013; 120 (11): 2292–2299.
Kim JE, Mantravadi AV, Hur EY, Covert DJ . Short-term intraocular pressure changes immediately after intravitreal injections of anti-vascular endothelial growth factor agents. Am JOphthalmol 2008; 146 (6): 930–4 e1.
Falkenstein IA, Cheng L, Freeman WR . Changes of intraocular pressure after intravitreal injection of bevacizumab (avastin). Retina 2007; 27 (8): 1044–1047.
Hollands H, Wong J, Bruen R, Campbell RJ, Sharma S, Gale J . Short-term intraocular pressure changes after intravitreal injection of bevacizumab. Can J Ophthalmol 2007; 42 (6): 807–811.
Frenkel RE, Mani L, Toler AR, Frenkel MP . Intraocular pressure effects of pegaptanib (Macugen) injections in patients with and without glaucoma. Am J Ophthalmol 2007; 143 (6): 1034–1035.
Frenkel MP, Haji SA, Frenkel RE . Effect of prophylactic intraocular pressure-lowering medication on intraocular pressure spikes after intravitreal injections. Arch Ophthalmol 2010; 128 (12): 1523–1527.
Singer MA, Awh CC, Sadda S, Freeman WR, Antoszyk AN, Wong P et al. HORIZON: an open-label extension trial of ranibizumab for choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology 2012; 119 (6): 1175–1183.
Schmidt-Erfurth U . Clinical safety of ranibizumab in age-related macular degeneration. Expert Opin Drug Saf 2010; 9 (1): 149–165.
Theoulakis PE, Lepidas J, Petropoulos IK, Livieratou A, Brinkmann CK, Katsimpris JM . Effect of brimonidine/timolol fixed combination on preventing the short-term intraocular pressure increase after intravitreal injection of ranibizumab. Klin Monbl Augenheilkd 2010; 227 (4): 280–284.
Kotliar K, Maier M, Bauer S, Feucht N, Lohmann C, Lanzl I . Effect of intravitreal injections and volume changes on intraocular pressure: clinical results and biomechanical model. Acta Ophthalmol Scand 2007; 85 (7): 777–781.
Pallikaris IG, Kymionis GD, Ginis HS, Kounis GA, Tsilimbaris MK . Ocular rigidity in living human eyes. Invest Ophthalmol Vis Sci 2005; 46 (2): 409–414.
Acknowledgements
York Teaching Hospital NHS Foundation Trust was the sponsor for the study and charitable funding was granted from the Elsie May Sykes Trust Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Mr Richard P Gale and Mr Gavin Walters have worked as consultants for and received educational grants from Novartis Pharmaceuticals UK. Their institution has performed Novartis-sponsored clinical trials. The remaining authors declare no conflict of interest.
Additional information
This research was presented as a poster at the Annual Congress of The Royal College of Ophthalmologists, Liverpool, 2013.
Rights and permissions
About this article
Cite this article
Murray, C., Wood, D., Allgar, V. et al. Short-term intraocular pressure trends following intravitreal ranibizumab injections for neovascular age-related macular degeneration—the role of oral acetazolamide in protecting glaucoma patients. Eye 28, 1218–1222 (2014). https://doi.org/10.1038/eye.2014.180
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.180
This article is cited by
-
Acute and subacute intraocular pressure and macular microvascular structure changes after intravitreal ranibizumab injection in eyes with branch retinal vein occlusion
BMC Ophthalmology (2023)
-
Prophylactic effect of brinzolamide–brimonidine fixed combination on intraocular pressure spikes after intravitreal anti-VEGF injections
International Ophthalmology (2021)
-
Effect of antiglaucoma agents on short-term intraocular pressure fluctuations after intravitreal bevacizumab injections
International Ophthalmology (2021)
-
The effects of intravitreal injections on intraocular pressure and retinal nerve fiber layer: a systematic review and meta-analysis
Scientific Reports (2020)
-
Action on neovascular age-related macular degeneration (nAMD): recommendations for management and service provision in the UK hospital eye service
Eye (2019)