Abstract
Genome-wide association studies (GWAS) use high-throughput genotyping technologies to genotype thousands of single-nucleotide polymorphisms (SNPs) and relate them to the development of clinical and quantitative traits. Their use has been highly successful in the field of ophthalmology, and since the advent of GWAS in 2005, many genes not previously suspected of having a role in disease have been identified and the findings replicated. We conducted an extensive literature review and describe the concept, design, advantages, and limitations of GWAS and provide a detailed description of the applications and discoveries of GWAS in the field of eye disease to date. There have been many novel findings revealing previously unknown biological insights in a diverse range of common ocular conditions. GWAS have been a highly successful modality for investigating the pathogenesis of a wide variety of ophthalmic conditions. The insights gained into the pathogenesis of disease provide not only a better understanding of underlying disease mechanism but also offer a rationale for targeted treatment and preventative strategies. Expansive international collaboration and standardised phenotyping will permit the continued success of this investigative technique.
Similar content being viewed by others
Introduction
Many common diseases are complex or multi-factorial, meaning that they do not exhibit classic Mendelian inheritance attributable to a single gene locus but rather are determined by an intricate interplay of genetic and environmental factors. Unravelling these complexities to identify new biological insights and therapeutic possibilities presents an important challenge to clinicians, scientists, and geneticists. For several decades, investigative techniques such as linkage analysis and candidate gene studies have been highly successful in elucidating genetic defects responsible for thousands of Mendelian diseases. These methods, however, have provided limited insight into the pathogenesis of complex disease. Since the completion of the human genome sequence in the early part of this century and the cataloguing of millions of common single-nucleotide polymorphisms (SNPs), genome-wide association studies (GWAS) have led to unprecedented advances in revealing the genetic contributions underlying common complex disease. Here we focus on the new genetic insights into biological pathways that have been revealed from these studies in a diverse group of ocular conditions and characteristics.
GWAS
The fundamental principle of GWAS is that common diseases must be in part caused by common genetic variant. The most common such variant in the human genome is a SNP; a single base pair change between people occurring approximately every 1000 bases.1 A GWAS depends on the identification of genetic variants in the form of SNPs. This has been made possible by the International HapMap project and the development of rapid massive parallel genotyping. The International HapMap Project is a large international collaboration that began in 2002 and sought to determine the common patterns of DNA sequence variation in the human genome. It has done this by characterising sequence variants, their frequencies, and the correlations between them in DNA samples from populations with ancestry from parts of Africa, Asia, and Europe. Similar to the human genome project in scope, it was a huge and successful collaboration that made all data freely available in the public domain. This catalogue of genetic variation has provided the necessary ‘blueprint’ of human genetic variation making GWAS possible. GWAS seek to identify if the differences in common genetic variants between individuals can contribute to certain phenotypes. Since the year 2000, rapid advances have been made in genotyping technology permitting interrogation of the genome with a resolution that has not previously been possible, and several commercial companies now provide high-density SNP genotyping from 200 000 SNPs up to 1.2 million SNPs.
In GWAS, a large set of SNPs (>100 000) is genotyped across the human genome to determine the most common genetic variations that have a role in disease or to identify heritable quantitative traits. GWAS commonly use a case–control study design with a large number of unrelated participants, comparing the frequency of SNPs in a defined group of individuals with the phenotype in question and a similarly matched group without. If certain genetic variations are found to be significantly more frequent in people with the disease, these variants may either be causative or more commonly may be associated (in ‘linkage disequilibrium’) with the causative mutation.2 By careful population selection and stringently phenotyping cases and controls, this approach has been highly successful in identifying new genetic variants and biological pathways that predispose to medical disease.
GWAS issues and study design
The typical GWAS has four parts: (a) selection of a large number of individuals with the disease or trait of interest and, in a binary condition, a suitable comparison group; (b) DNA isolation, genotyping, and quality control; (c) statistical tests for associations between the SNPs that pass quality-control thresholds and the disease/trait; and (d) replication of identified associations in independent population samples or experimental examination of functional implications. By far, the most common design in published GWAS comprises a case–control study with a binary outcome. Other study designs include individuals with measured continuous phenotypic variables (eg, refractive error) analysed as a quantitative trait and family-based designs, such as trios (proband and parents) or other pedigrees of related individuals. It is ideal to recruit case subjects and control subjects systematically from the same population of single ancestry as case–control differences in ancestry (population stratification) can confound association test results. Experience has shown that large sample sizes (>2000) are needed to detect common genotypic variants likely to have a low relative risk (1.2–2) and to offset the large number of independent SNP association testing.3 Contemporary genotyping platforms have specific advantages and limitations; however, most provide a high level of genomic coverage estimated to capture between 67 and 90% of common SNP variation in Caucasian ethnicity.4 After genotyping, extensive data cleaning (quality control) is required to detect problems that can result in false-negative or false-positive findings, such as genotyping errors, duplicate samples, unexpected relatedness among subjects, and strong deviations from expected genetic (Hardy–Weinberg) equilibrium. Associations between the two alleles of each SNP are tested by comparing the frequency of each allele in cases and controls using a chi-squared test or Fisher’s exact test. However, because of the large number of multiple tests used, a correction factor is implemented to try and statistically distinguish true from false associations.3 Given the major challenge of separating the many false positives from the few true-positive associations, putative genetic variants that are identified and reach genome-wide significance need to be replicated in additional case–control cohorts, preferably of larger size, as the best method to verify a true association. Finding a true causal variant, however, only represents the beginning; genetic association does not imply causality but offers a genetic hypothesis of an underlying biological pathway that warrants further exploration.
GWAS
Age-related macular degeneration (AMD)
A genetic predisposition to AMD has been suggested for almost 30 years with familial aggregation studies, twin and linkage studies providing most of the evidence.
Initial investigative techniques focussed on assessing candidate genes which primarily comprised those associated with macular dystrophies and similar phenotypes to AMD. Over 45 such loci were investigated, with most failing to yield replicated associations. Linkage studies proved challenging because of the difficulty in recruiting large affected families and the late age of onset of the disease. Genome-wide linkage studies have suggested numerous loci, but only two (on chromosome 10q26 and 1q32) have been replicated convincingly. The former of these contains over 70 genes, including peroxiredoxin 3 (PRDX3) gene, which encodes a protein with antioxidant function. Interestingly, chromosome 1q contains the well-characterised gene complement factor H (CFH).
The first GWAS success story was the discovery of the association CFH with AMD that was independently described in three cohorts.5, 6, 7 A coding variant Y402H in exon 9 of CFH was significantly associated with AMD. This finding was replicated throughout the world in many ethnic groups. This mutation affects the binding properties of CFH, thus resulting in inappropriate complement activation.8
The discovery led to investigations of other complement factors in AMD, and the discovery of the association with complement factor B and complement component C2,9 further replicated across the world10, 11 adding to the understanding of this condition.
Previous linkage studies had long established 10q26 as a candidate locus for AMD.12 Age-related maculopathy 2 gene (ARMS2—previously known as LOC387715) was subsequently suggested as the candidate locus,13 in particular SNP rs10490924. However, the pathogenesis of this gene was not clarified. A GWAS undertaken by DeWan et al14 highlighted an alternative gene in the locus 10q26; high temperature requirement A1 (HTRA1), in 96 Oriental patients with neovascular AMD. The risk SNP rs11200638 (in complete linkage disequilibrium with rs10490924) was found to be highly associated with wet AMD. It encodes a heat-shock serum protease expressed in human retina that is activated by cellular stress.15 Meta-analysis has suggested that both ARMS2 and HTRA1 may contribute towards AMD independently with an augmented combined affect.16
Kopplin et al17 completed a GWAS on patients with late AMD in conjunction with a family-based GWAS. They not only confirmed previously associated risk genes but went further to suggest protective functions of genes MYRIP and SKIV2L. The former of these is involved in trafficking melanosomes in the RPE and thus may prevent or delay declines in RPE function. SKIV2l is involved in breakdown of RNA and may have a role in autophagy. Variations in SKIV2L have additionally been associated with a protective role in polypoidal choroidal vasculopathy.18
Risk factors associated with AMD have additionally been studied in relation to risk alleles. It has been shown that smoking and high BMI with at-risk alleles significantly increase the risk of developing AMD, adding considerations as to possible interactions.19 Further interactions of risk factors with CFH genotypes were explored by Seddon et al.20 They reported a risk profiling system which illustrated that established risk factors in combination with genotypes could predict progression to advanced AMD independent of demographic factors and ocular phenotype. Predictions of treatment outcomes with modern anti-VEGF agents have been suggested based on genotype variations of CFH and HTRA1.21 These steps toward a personalised risk profile, may provide for a more target approach to prevention and management of this condition.
The influence of the complement system in AMD has now even extended to novel treatments, aimed at modulation of this system. Available at: http://clinicaltrials.gov. The landmark GWAS in AMD have paved the way for almost 50% of the hereditability of this condition now being explained. This genetic understanding is unrivalled by any other complex diseases.
Glaucoma
Primary open angle glaucoma
The first gene implicated in the pathogenesis of primary open angle glaucoma (POAG) was Myocilin (MYOC)22 in which mutations may result in a breakdown of the extracelleular matrix structure in the trabecullar meshwork. Mutations in this gene are responsible for up to 4% of POAG cases. Mutations in optineurin (OPTN)23 and WD Repeat Domain 36 gene (WDR36)24 have also been shown to be causative. However, mutations in these genes have been shown to be infrequent and can explain only a small proportion of the genetic architecture of POAG.
Nakano et al25 published the first GWAS in POAG in a Japanese population, with meta-analysis revealing three associated loci with moderate but not genome-wide significance. Six polymorphisms were identified: near ZP4 gene, and PLXDC2 gene. The functionality of these associated genes and the markers were not discussed or replicated and were absent in an independent Indian population.26
Thorleifsson et al27 conducted a large multiethnic GWAS. They found two SNPs (rs 4236601, rs1052990), which were in the same linkage disequilibrium block as genes CAV1 and CAV2, which encode caveolin 1 and 2. Both these proteins are expressed throughout ocular tissue.28 Caveolin 1 is thought to have a regulatory role in the function of endothelial nitric oxide synthase and transforming growth factor-β (TGFβ) signalling, mechanisms that have been implicated in the pathogenesis of POAG.29 The most statistically significant variant (rs4236601), however, did not have an effect on IOP or central corneal thickness.
Thorleifsson et al27 found differences in rs4236601 within ethnicities. When compared with European populations, this variant was absent in a Japanese cohort but posed a greater risk with lower frequency in a Chinese population. Osman et al30 also showed significant association with CAV1 and CAV2, among other genes, in a GWAS on an Asian cohort. However, these findings were not replicated in a North American cohort.28
Most recently, Burdon et al31 analysed 590 patients with advanced open angle glaucoma. They found two regions of significance, near the TMCO1 gene and the CDKN2B-AS1 gene, both of which were shown to be expressed throughout ocular tissue. CDKN2B was shown to be upregulated in response to raised IOP. These genes have been suggested to have a role in apoptosis,32 with the link thus with glaucoma. Of further interest, CDKN2B was shown previously to be related to optic disc cupping33 (see later in ‘Quantitative traits’). The particular SNP in that study had a P-value=3.9 × 10−7, further implicating an association of this region with OAG. Interestingly, TMCO1 has subsequently been associated with intraocular pressure (see ‘Quantitative traits’), providing further evidence to its role in disease aetiology.
This paper raised interesting methodological and interpretational issues. First, they validated the efficacy of using extreme phenotypes in GWAS; the variants found in their discovery cohort of severe OAG were replicated in cases with less severe disease. Second, many of the cases in this study were used as a replication in the GWAS of Thorleifsson et al.27 Interestingly, although in the latter paper the analysis confirmed a role for CAV1 & CAV2, this was not found to be so in this full GWAS with the same cases. This is not a novel situation and highlights some of the challenges of interpreting GWAS and replication data. Conversely, this adds further credibility to those associations that are replicated in full independent GWAS.
More recent GWAS30, 34 and targeted genotyping35 have provided further evidence for the association with CDKN2B in numerous ethnicities. This gene has now been shown to be significant in multiple independent GWAS in both normal tension glaucoma (NTG; see later) and POAG. Some have suggested its role is therefore on optic nerve susceptibility,25 perhaps via effects on the TGF-beta pathway.34 Certainly its role in glaucoma is now established, and further understanding of its role and effect on phenotype is now warranted.
NTG
NTG is an important subset of primary open angle glaucoma, with a high prevalence in Japanese populations.36 Studies have implicated several genes, including optic atrophy 1,37 optineurin,38 p53,39 and apolipoprotein E.40, 41 The mechanism of these genes may involve abnormal regulation of apoptosis,42 but this remains controversial and represent a small proportion of NTG patients.
The first GWAS investigating NTG compared 305 Japanese NTG patients with 355 controls43 aged <60 years. The most significant SNP (rs3213787) along with the seven next SNPs they found lay in the gene for S1 RNA Binding Protein 1 (SRBD1). This group established expression of this gene in the brain, bone marrow, and retinal ganglion cells (RGCs) of neonatal mice and demonstrated that the at-risk allele resulted in enhanced SRBD1 expression. Although the function of this gene is unknown, they suggest that overexpression may result in apoptosis and inhibition of cell growth; leading to RGC and optic nerve axon loss. Also rs735860, a SNP of genome-wide significance, lies within the elongation of long-chain fatty acids family member 5 (ELOVL5) gene. This is one of a family of enzymes expressed in mammalian retina that is involved in long-chain polyunsaturated fatty acid synthesis (LCPUFA). Alteration in LCPUFA expression implies potential mechanism towards RGC apoptosis.
The same investigators have since replicated the significant SNPs in a separate population of NTG and high-tension open angle glaucoma (HTG) patients, with a wider age range than the original cohort.44 Although SRBD1 and ELOVL5 are thought to be non-IOP-related genetic factors, both SNPs (rs3213787 and rs735860) were found to be associated with NTG and HTG. There was no difference in the maximum IOP between the HTG patients with the at-risk alleles, leading to the suggestion that these SNPs act independent of IOP. Their findings also implied that these genes are associated in late-onset open angle glaucoma. Further replication of these results have yet to be done.
More recently, large independent GWAS and meta-analysis on GWAS cohorts45, 46 investigating >1500 NTG patients have suggested the role of CDKN2B in the aetiology of Japanese NTG. This gene is highly relevant to high-pressure open angle glaucoma (see previously). The importance of this gene on glaucomatous optic neuropathy47 suggests its role is likely to be IOP independent.48
Pseudoexfoliation (PXF)
Genetic factors contributing towards the development of PXF and PXF glaucoma (PXG) are established, with a demonstrated increased risk to relatives.49 Multiple modes of inheritance have been postulated.50 PXF has been associated with an increased production of microfibrillar material, such as fibrillin 1, latent transforming growth factor β binding proteins, and TGFβ. It has also been associated with a decreased level of clusterin (CLU), which may increase abnormal aggregation of microfibrillar material. Of these candidates, only polymorphisms encoding for CLU had been associated with PXF and PXG.51
Thorleifsson et al52 performed a GWAS initially on 195 patients with glaucoma. They found moderate significance of SNP rs2165241 in this group. However, significance was very high in the subgroup of 75 patients with PXG (OR=3.4). This SNP was sequenced in additional Swedish and Icelandic cohorts and confirmed to be associated with PXG. It is found in an intron of the lysyl oxidase–like protein 1 (LOXL1) gene. Although no mutations in the LOXL1 gene itself were determined to cause PXF, certain sequence variations were found more frequently in cases, suggesting an association with this gene. The association of LOXL1 with PXF has been replicated numerous times.53, 54, 55 The LOXL1 protein is part of a family of enzymes that catalyses deamination of tropoelastin resulting in the formation of elastin fibres and is essential in the homeostasis of elastic and connective tissue.56 Furthermore, it is suggested that PXF material consists of elastin microfibrillar components.57 Functional studies have demonstrated reduced expression of LOXL1 in ocular tissue of PXF and PXG patients and specifically in lens capsule of those with PXG.58 Krumbiegel et al59 performed a GWAS with DNA pooling and confirmed the association of the LOXL1 locus. Additionally, they highlighted a locus within the CNTNAP2 gene on chromosome 7, which did not reach genome-wide statistical significance. CNTNAP2 encodes contactin-associated protein-like 2 (CNTNAP2), a neuronal membrane protein the function of which is not yet clear. Krumbiegel et al59 demonstrated widespread expression of CNTNAP2 mRNA and protein throughout ocular tissue, including RGCs and trabecullar endothelial cells, although no difference was demonstrable between PXF and control tissue.
Primary angle closure glaucoma (PACG)
PACG is a separate condition aetiologically and genetically from the more common POAG. Vithana et al60 performed the only GWAS to date on 1854 cases from across Asia, replicated in 1917 cases from Asia and UK. They suggested two novel genes to be associated with PACG. First, PLEKHA7 on 11p15.1, which has a role in paracellular permeability. It is distributed widely in the eye, and the authors suggest that it may be involved in fluidic aspects related to PACG.
They also suggest an association with COL11A1, a gene which causes the monogenic conditions of Marshall syndrome (OMIM 154780), and Sticklers type 2 (STL2: OMIM 604841). They note the paradox that PACG is normally co-existent with hypermetropia, while Marshall and STL2 are normally associated with progressive axial myopia. The existence of COL11A1 in the trabecular meshwork suggests to the authors that alterations in this gene may influence numerous sites in eyes with PACG.
Finally, a third locus on 8q was suggested, although no definitive gene could be identified. The novel locus and the association of the known genes will help future investigations into PACG and perhaps ocular structural development.
Cornea
Fuchs endothelial dystrophy
Fuchs corneal endothelial dystrophy (FCED) is thought to occur in 38% of first-degree relatives of probands.61 Linkage studies first revealed a missense mutation in COL8A2 in a multigenerational-affected pedigree.62 However, some controversy exists over the reported findings. Additionally, rare autosomal dominant mutations in SLC4A11, ZEB1, and KCNJ13 have been reported.
The first GWAS in FCED was published in 2010.63 Baratz et al63 found numerous SNPs within the Transcription Factor 4 (TCF4) locus independently associated with FCED. The most strongly associated haplotypes spanned one exon, with the impact of the most significant variants increasing with disease severity. The authors, however, were unable to define a variation within the coding region and suggested that a non-coding regulatory region around the encoded protein E2-2 is important.
The protein encoded by TCF4 is a member of the family called E2-2. It is a member of the class I basic helix–loop–helix (bHLH) transcription factors that are involved in cellular growth and differentiation. E2-2 itself, found within the corneal endothelium, may influence FCED formation by altering the expression of ZEB1. If variants reduce the expression of E2-2, deficient proliferation or migration of endothelial cells may be causative. Alternatively, enhanced extracellular matrix deposition may be causative if variants result in increased expression of E2-2.
This original GWAS was replicated by Li et al64 in 450 cases with genome-wide linkage on 64 families with 215 affected members. They confirmed the significance of the SNP rs613872 with their former analysis (P=9.33 × 10−35). Linkage revealed the significant region was on chromosome 18—only 1.5 Mb from TCF4. Further evidence in other ethnicities has followed, with Thalamuthu et al65 confirming the association of TCF4 with FECD in a Chinese population.
Keratoconus (KC)
A genetic contribution towards the aetiology of KC has long been established with all modes of Mendelian inheritance66 and various loci suggested. The lack of consensus loci, suggests that the inheritance is likely to be complex. Two GWAS to date have investigated KC. Li et al67 completed a GWAS on 222 Caucasians with KC replicating in a further 611 cases and suggested an association with RAB3GAP1 on 2q21.3. This association was most significant, after a meta-analysis. Defects in this gene are known to cause Warburg Micro Syndrome (OMIM 600118) (which includes microcornea in the ocular phenotype). Simultaneously, this group performed a meta-analysis with a GWAS performed by Australian colleagues, suggesting the promoter region of HGF to be significantly associated with KC.68 HGF had previously been shown to be associated with myopia69and with narrow angle closure,70 suggesting that this gene may well have a role in structural development of the anterior segment. The encoded protein is also found in the cornea, particularly the stroma, and the authors suggest that this gene may have a role in KC pathogenesis via an inflammatory pathway.
The different genes suggested in these papers based on data from the same cohort may seem conflicting; however, they offer novel pathways in KC. Replication will be crucial for validation.
Diabetic retinopathy (DR)
DR is the leading cause of visual loss in the working ages of the developed world. There is growing evidence that the genetic contribution towards DR is significant, with suggestions of the heritability of severe retinopathy being between 25 and 50%.
Before the advent of GWAS, genome-wide linkage studies highlighted regions on chromosomes 1, 3, 9, and 12. Numerous candidate genes were also investigated (for a review, see Patel et al71). However, the era of GWAS further illuminated our understanding.
The two largest GWAS of DR in Type 1 (Grassi et al72) and Type 2 (Huang et al73) DM investigated 973 and 749 cases, respectively. Grassi et al72 performed GWA on two different platforms on two separate cohorts with PDR and macular oedema, imputing results to combine the data. They found a significant SNP between two genes (AKT3 and ZNF238) on chromosome 1. The former of these is known to be activated by insulin-like growth factor and platelet-derived growth factor—both of which are activated in PDR. They also analysed 281 patients with DR without nephropathy and demonstrated association with an intergenic SNP on chromosome 6. Furthermore, they also investigated SNPs tagging copy number variants (CNVs) and showed an association with CNVR6685.1 on chromosome 16. A number of genes involved in transcriptional regulation (CCDC101), posttranslational protein modification (SULT1A1 and SULT1A2) and apoptosis (NUPR1) are in within or in linkage disequilibrium to this region. However, this same group were unable to later replicate these findings in another cohort.74
Huang et al73 published in the same year on a cohort of 749 Taiwanese patients with T2D with proliferative and non-proliferative retinopathy. They demonstrated regions of interest on chromosomes 1, 5, 10, and 13, mapping to four known genes. Two of these genes (ARHGAP22 and PLXDC2) are involved in endothelial cell angiogenesis. They also confirmed the results of a previous genome-wide linkage study associating 1q32 with DR,75 re-iterating the importance of this region. It is particularly interesting that neither GWAS investigating the retinopathy in type 1 and 2 DM found overlapping regions.
Publications of GWAS into DR are novel, and more will be on the horizon. They are undoubtedly providing insights into the genetic architecture of these conditions and separating them from the genetics of diabetes. It is worth noting that the cohorts in both GWAS had diabetes for significantly longer than controls. It would be prudent to control for this in future studies to ensure findings are related to DR and not the age of onset of disease.
Rhegmatogenous retinal detachment (RD)
Beyond the well-documented Mendelian conditions associated with vitreoretinopathies and RD,76 a genetic predisposition towards the aetiology of complex RD has been known for >40 years. Recently, a sibling recurrence risk (λs) has been suggested as 2.1 and parent–offspring risk as 2.9.77
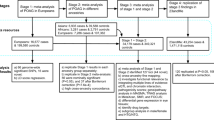
We performed the first GWAS into RD in 2013.78 We used a two-stage discovery stage followed by replication. Meta-analysis was undertaken on all the cases, totalling 2833 cases and 7871 controls. The most significant SNP rs267738 is a missense variant in an exon of Ceramide Synthase 2 (CERS2). This is the most abundant member of the Ceramide synthase family. Ceramides have a central role in sphingolipid metabolism and have a structural role in cell membranes and as a secondary messenger. There is ample evidence of a role of ceramides in retinal dysfunction,79 particularly with enhanced ceramide synthesis shown to induce RPE cell apoptosis. Furthermore, increased Cer levels have been shown not only in photoreceptors but also in other retinal layers in an in vivo model of RD, correlating with photoreceptor death.54
Other genes suggested as significant included SS18, TSTA3, and TIAM1. The former two modify integrins, which are transmembrane glycoproteins that bind extracellular matrix components, while the latter modulates changes in cytoskeleton. We undertook pathway analysis of the most significant genes highlighted and demonstrated significant pathways, which previously had only been associated with cell death and haematological systems.
We continue to investigate the genetic aetiology of RRD, with Exome-specific chips and in potentially alternative racial groups. An international collaboration has been established to help develop the required power for this endeavour.
GWAS in ophthalmic quantitative traits
Quantitative traits refer to continuous phenotype data (eg, blood pressure, blood glucose, height). When investigating complex diseases, there are many factors which may have influential roles (eg, total cholesterol, total low-density lipoproteins, total triglycerides, and the risk of cardiovascular disease). One way of further understanding the complexities of these conditions is to study these quantitative risk traits.
Refractive error
Much of the current information on human myopia molecular genetics can be drawn from familial studies of high myopia. To date, there are at least 16 loci listed on the OMIM database (http://www.ncbi.nlm.nih.gov/omim) (MYP2–MYP17) for non-syndromic high myopia, common myopia, or ocular refraction that are distributed among 13 chromosomes. At least seven loci for refractive phenotypes (MYP1, MYP3, MYP6, MYP11, MYP12, MYP14, and MYP17) have been successfully replicated in independent linkage data sets and identified as being associated with myopia.
Most of the biological information derived from these studies have implicated connective tissue growth and extracellular matrix reorganisation in the pathogenesis of myopia. This group includes genes that encode matrix metalloproteinases (MMP1, MMP2, MMP3, and MMP9), growth factors and growth factor receptors (HGF, TGFB1, TGFB2, and MET), collagens (COL1A1 and COL2A1), and proteoglycans (LUM) (see Wojciechowski80 for summary).
GWAS and linkage disequilibrium mapping have, for the first time, implicated mitochondrial and apoptotic pathways in the pathogenesis of myopia.81, 82 Andrew et al82 demonstrated an association of refractive error with MFN1, PSARL, and SOX2OT, while Nakanishi et al81 identified a polymorphism (rs577948) at 11q24.1 (near BLID) that was associated with an elevated risk of pathological myopia (OR=1.37). MFN1, PSARL, and BLID are expressed in mitochondria and are involved in mitochondrial-led cellular apoptosis.83 In addition, a further GWAS identified a polymorphism (rs9318086) at 13q12.12 significantly associated with an increased risk of high myopia in a Han Chinese population (OR=1.64).84 This region contains the genes MIPEP and C1QTNF9B-AS1. The former is expressed in the retina and is involved in oxidative phosphorylation and processing in the inner mitochondrial matrix. Given that the retina is the most energy-consuming tissue in the eye, these discoveries have led to an increasing interest in the role of the mitochondrial pathway in refractive error.84
In a large twin-based GWAS of refractive error in a European population, several polymorphisms at 15q25 near the RASGRF1 gene were found to be associated with ocular refraction.85 RASGRF1 was shown to be highly expressed in human retina and its expression is regulated by muscarinic receptors.86 This provides another intriguing biological mechanism as anti-muscarinic agents can prevent ocular elongation in animal myopia models87 and have been used to reduce myopia progression in human trials.88 In a companion paper, Solouki et al89 reported another European GWAS with a polymorphism (rs634990) at 15q14 significantly associated with refractive error. This polymorphism was found in a putative regulatory region near the genes GJD2 and ACTC1, both of which are expressed in the retina. GJD2 encodes a neuron-specific protein (connexin36) that is present in photoreceptors, amacrine, and bipolar cells and is thought to have an important role in the transmission process of the retinal circuitry by enabling intercellular transport of small molecules and ions.89 This novel finding suggests, for the first time, that modulators of retinal visual signals may have a role in susceptibility to refractive error. More recent reports have replicated loci at 15q14 that underscore a risk for high myopia, in particular an association with axial length,90 and a further GWAS for high myopia in a French population have refined a risk locus at MYP10, implicating a role for microRNA variation in predisposition to high myopia.91
There have now been eight GWAS investigating myopia or related endophenotypes. Most recently, two very large GWAS have been published, which have greatly furthered our understanding. The largest GWAS of refractive error (n=45 771) was published in early 2013.92 This group discovered 20 novel loci in a European cohort associated with myopia. These included the strongest association with an SNP in the intron of LAMA2. Laminins are structural proteins that are integral to the ECM. They also found an association 17 kb upstream from ANTXR2, which binds type IV collagen, thus further implicating ECM remodelling. Further pathways highlighted were by association with RDH5 and KCNQ5. Both have a significant role in the visual cycle. They also implicated genes involved in eye growth (PRSS56, BMP4, BMP3, ZBTB38, and DLX1). Associations with ZIC2 and ZMAT4 suggested a role of retinal ganglion outgrowth in development. Finally, the authors suggested a role of genes involved in neuronal development, which were not involved in the vision cycle (KCNMA1, RBFOX1, LRRC4C, DLG2, TfP2). Of further interest in this study was the method of recruitment. All of the cohort were paid members of 23andMe Inc. and self-reported their myopia. This may have resulted in misclassification. However, many of their findings were confirmed by the Consortium for Refractive Error and Myopia (CREAM) who conducted a meta-analysis on the well-defined and phenotyped cohort. They co-discovered93 16 of the 20 novel findings from the Kiefer et al92 and 23andI cohorts. Of the 22 novel loci discovered by CREAM, 14 were replicated by Kiefer et al.92 CREAM not only confirmed previous locus,94 but also confirmed roles in ECM remodelling, ion channel transportation, and eye development.93 Both these studies illustrate the importance of very large sample size in successful GWAS; and Kiefer and colleagues even demonstrate the possible dismissal of expensive phenotyping in conditions with early onset, such as myopia. It is likely that a combination of both will be required to demonstrate further success. Finally, further studies are likely to require incorporating measures of environmental exposure into the statistical analysis of GWAS.
Optic disc parameters
Optic disc area and vertical cup:disc (VCDR) are important parameters in the development of numerous ophthalmic conditions, including anterior ischaemic optic neuropathy, Leber’s hereditary optic neuropathy, and open angle glaucoma. The hereditability of optic disc area and VCDR are estimated as 52–58% and 48–80%, respectively. However, few studies before the advent of GWAS in quantitative traits attempted to analyse optic disc parameters in the normal population.
Ramdas et al33 investigated 7360 Caucasians (of whom 188 had POAG) from Rotterdam. They found three genetic loci associated with optic disc area, and six associated with VCDR that persisted when the 188 patients with POAG and the 115 with myopia were excluded. Their findings were replicated in 4455 Dutch and British Caucasians. Three SNPs within one locus (10q21.3-q22.1) were found to be significant in both traits, accounting for 2.7% of the variation within optic disc area and 2.2% of the VCDR variation. The most significant common related gene to these loci was atonal homolog 7 (ATOH7), more so in VCDR. Several genes were found to be associated with VCDR and included: CDKN2B (chromosome 9p21), which encodes a cyclin-dependent kinase thought to have a role in cell growth regulation; SIX1 (chromosome 14q22-23), which is involved in eye development and linked to anophthalmia; SCYL1 (chromosome 11q13), which is associated with optic atrophy in mice; CHEK2 (chromosome 22q12.1), which has no previous association with ocular conditions; DCLK1 (chromosome 13q13); and BCAS3 (chromosome 17q23). Additionally, for optic disc area, GFBR3 on chromosome 1p22 was shown to interact with with ATOH7 influencing VCDR parameters.
Macgregor et al95 subsequently performed a GWAS on two Australian twin cohorts and confirmed the association with ATOH7. This was further replicated in a UK cohort.
Optic disc parameters are known to vary between races. Khor et al,96 however, confirmed the association of ATOH7 and TGFBR3 through a further GWAS on 2132 Indians and 2313 Malays in Singapore. Additionally, they found most significance associated with a novel gene CARD10, on Chromosome 22q13.1, which encodes Caspase recruitment domain containing protein 10. This protein has a role in apoptosis via a transcription factor called NfkappaB.97 This pathway has been implicated in neurodegenerative disorders, such a Alzheimer’s disease.98
The most common condition related to optic disc parameters is of course glaucoma. Ramdas et al99 performed a meta-analysis, investigating SNPs found to be related to optic disc parameters in populations of POAG upon whom GWAS have been completed. Of particular interest, they confirmed three loci associated with optic disc parameters also having an association with POAG. These included ATOH7.
Most recently, Burdon et al31 discovered an association between CDKN2B-AS1 gene and primary open angle glaucoma, providing further evidence of the role of this locus 9p21 in OAG and optic disc morphology.
Central corneal thickness (CCT)
CCT is a normally distributed quantitative trait known to be associated with ocular hypertension and primary open angle glaucoma. Family and twin studies have suggested the hereditability of CCT range between 0.6 and 0.95,100 however, candidate gene analysis provided limited results.
Lu et al101 published a multi-staged GWAS in CCT. They initially performed GWAS on two population groups that individually provided weak associations. Meta-analysis revealed four associated SNPs—on chromosomes 16, 13, and 10. They performed replication GWAS on further population cohorts, and two SNPs were most significant. These were closest to the gene ZNF469 on chromosome 16q24 and FOX01 on chromosome 13q14.1.
The authors calculate that FOX01 may account for 1.2% of the variability of CCT. The exact role of FOX01 is unclear. Within the eye, FOXC1 is a transcription factor involved in the development of the anterior segment and involved in anterior segment dysgenesis. FOXC1 seems to regulate the expression of FOX01,102 thus perhaps suggesting a role for the latter in anterior segment formation.
Mutations in ZNF469 had already been described in a Brittle Cornea Syndome (OMIM 229200). However, the mutations in this condition are very rare, compared with the SNPs found in the GWAS with a minor allele frequency of 0.44. It has been suggested that linkage disequilibrium is unlikely between these two variants in this gene. This further suggests that although there may be similarity between the roles of these variants, there may also be significant differences.
A further GWAS on a Scottish and three Croatian populations further confirmed the association of ZNF469.103 Meta-analysis with the previously published GWAS confirmed the association of FOXC1. Additionally, three further SNPs reached genome-wide significance. The first was on chromosome 13q12.11, near the transcription factor gene AVGR8 (Autogenous Vein Graft Remodelling associated protein 8). The next SNP is on chromosome 15q25.3, the linkage block of which extends into the gene AKAP13. The encoded protein is thought to link cell surface receptors and transcription factors that may regulate collagen production in the extracellular matrix in the gastrointestinal tract via FOXF2;104 a similar role may be postulated within the cornea. The third SNP on 9q34.3 is near COL5A1. This is of interest particularly, as it initially appeared significant in the first GWAS. Functionally, this is an attractive candidate gene. Not only are collagen V present within the cornea, but mouse models have shown that heterozygote COL5A1 null mouse cornea is 25% thinner with fewer collagen fibrils than wild-type mice.105
More recently, a large GWAS on Caucasians from throughout Europe confirmed the association of ZNF469 and COL5A1.106 These genes therefore particularly appear to genuinely have a role in corneal thickness.
Corneal curvature (CC)
Hereditary influence for CC have been estimated between 60 and 92%. Previous investigations focussing on candidate genes and monogenic disorders affecting corneal morphology provided limited insight into the complex trait.
Han et al107 published the first GWAS into this trait. They found significant loci associated with FK506 binding protein rapamycin complex-associated protein 1 (FRAP1) gene and platelet-derived growth factor receptor alpha (PDGFRA) gene. These associations were corroborated in a cohort of Indian adults and Chinese children. Both these genes encode enzymes with kinase properties. The former has effects on cell growth and proliferation, while the latter induces intracellular kinase activity via enzymes such as MAP kinase, which are known to influence collagen fibres.108 Indeed, the role of PDGFRA in cell growth has implicated it in fibrotic diseases of the eye, such as proliferative vitreoretinopathy.109 The replication of the data within a young population reassures of the role these genes may have in corneal development. The ethnic variety within this cohort suggests that the role of these genes may be conserved throughout these populations.
Mishra et al29 performed meta-analysis on two GWAS Caucasian cohorts and suggest a further gene TRIM29, a gene shown to be expressed in patients with KC,110 to be associated with CC variation. More relevantly, they confirmed the association of PDGFRA in CC variation. This gene has also been demonstrated to be significantly associated with corneal astigmatism in a GWAS of >8000 Asian individuals.111 This gene, in particular, has become a very relevant candidate for the heritability of CC.
Intraocular pressure (IOP)
The greatest controllable determinant towards the aetiology of glaucoma is IOP and is thought to have a hereditability of up to 0.62. Van Koolwijk et al112 performed a GWAS including 11 972 affected Caucasians from 4 cohorts replicated in 7482 further patients. They found significant association with GAS7 and TMCO1. The former of these is thought to have a role in the outflow of the trabecular meshwork and has previously been shown through linkage studies to be associated with POAG.113 TMCO1, as mentioned previously, has been suggested to be associated with POAG.31 Van Koolwijk et al112 also investigated the effect of the minor alleles of these genes on POAG. The minor allele of GAS7, which decreased IOP by 0.19 mm Hg, reduced the glaucoma risk (OR=0.88, 95% CI=0.78–0.98). That of TMCO1, which increased IOP by 0.28 mm Hg, increased the risk of POAG (OR=1.31 (95% CI=1.12–1.53). The evidence of the importance of these genes in the aetiology of IOP and POAG is therefore growing.
A summary of the principal findings from the above studies is presented in Supplementary Table 1.
Future work
Independent replication of identified genetic variants remains the gold standard for validating reported risk alleles. In addition, larger studies and meta-analysis of conducted GWAS will allow identification of common genetic variants of very small effects, which may have an important role in disease pathogenesis. Many of the identified genetic variants described are not in the coding regions that alter the amino-acid sequence, but more frequently, they are involved in the regulation of one or more complex genetic processes. Thus, GWAS represent the first step in identifying novel regions and pathways that have a role in eye disease, with additional functional studies, animal models, and pharmacological studies needed to elaborate on the putative clinical application.
In the investigation of eye disease, it will be critical to conduct GWAS in populations of diverse ethnicity as different mechanisms may underlie the ethnic variations in disease prevalence seen in population studies. Such endeavours are being undertaken in common complex diseases, and such efforts may need to be established within ophthalmology. In addition, more complex study designs will be needed to examine the dynamic relationship between genomic variants and the environment in eye disease.
The concept of ‘missing hereditability’ is now well established.114 This describes the current situation whereby only a small fraction of the total hereditability of phenotypes has yet been discovered. Theories explaining this include suggestions that more rare variants, which may be missed by GWAS, may have a significant role to play in these conditions. Discovering these may be achieved by the development and utilisation of denser or even disease-specific SNP chips, or Exome-specific chips, which have been successful in other fields. Alternatively, sequencing at higher resolution than can be achieved with traditional tag-SNPs in GWAS may achieve similar aims. Next-generation sequencing can interrogate the genome at the resolution of a single base pair. Such sequencing of the exonic region or indeed the whole genome are likely to replace GWAS in the coming decade. However, these advances will present enormous hurdles for data storage, analysis, and interpretation.
Discussions
There is a compelling rationale for using GWAS methods in the investigation of common ophthalmic disease. The pathogenesis of many common ocular disorders remains unknown, and GWAS provide an unbiased, hypothesis-free method of examining the human genome. To date, GWAS have been highly successful in medical disease, but particularly in the remit of eye disease, with notable impacts of discovered genetic variants. Indeed, although large numbers of cases are generally required for adequate power for GWAS, the median number of cases in ophthalmic conditions here presented is 305. This is quite remarkable in view of the sizes of cases required for most GWAS. These ophthalmic studies have revealed many insights into the biological pathogenesis underlying common causes of visual morbidity, with perhaps one of the widely publicised findings in the field of GWAS relating to complement factor H in AMD, where pharmacological advances with real clinical application may be on the horizon.
Our review has highlighted notable advances in the understanding of the pathogenesis in a diverse group of ocular conditions responsible for significant visual morbidity. In POAG, the role of endothelial nitric oxide synthase and TGFβ signalling has been highlighted as an important pathway, and in PXG, the dramatic risk conferred by LOXL1 mandates further research into the exact mode of action and ways to modulate its effect. A lot remains to be discovered about the mode of RGC loss in NTG and POAG; however, studies have now highlighted new pathways such as ATOH7, a regulator of photoreceptor and RGC development that demonstrates significant ganglion cell loss in knock out mice. Refractive error is a complex quantitative trait with significant phenotypic and ethnic variability, but large multi-centre GWAS have pointed to a novel role of mitochondrial apoptosis, sparking new interest in this field. FCED is a common cause of significant visual morbidity, and genetic risk alleles conferring a fourfold increased risk have been identified where little was known previously.
Despite the overall success of GWAS with >1300 reported novel disease associations in medical literature, many challenges exist in conducting and analysing these studies. The need for large sample sizes, the potential for false-positive results, the lack of information on gene function, as well as potential biases due to genotyping errors and case and control selection are important obstacles and limitations of GWAS.
References
Altshuler D, Daly MJ, Lander ES . Genetic mapping in human disease. Science 2008; 322 (5903): 881–888.
Iles MM . What can genome-wide association studies tell us about the genetics of common disease? PLoS Genet 2008; 4 (2): e33.
Balding DJ . A tutorial on statistical methods for population association studies. Nat Rev Genet 2006; 7 (10): 781–791.
Frazer KA, Ballinger DG, Cox DR, Hinds DA, Stuve LL, Gibbs RA et al. A second generation human haplotype map of over 3.1 million SNPs. Nature 2007; 449 (7164): 851–861.
Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005; 308 (5720): 385–389.
Edwards AO, Ritter R 3rd, Abel KJ, Manning A, Panhuysen C, Farrer LA . Complement factor H polymorphism and age-related macular degeneration. Science 2005; 308 (5720): 421–424.
Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P et al. Complement factor H variant increases the risk of age-related macular degeneration. Science 2005; 308 (5720): 419–421.
Laine M, Jarva H, Seitsonen S, Haapasalo K, Lehtinen MJ, Lindeman N et al. Y402H polymorphism of complement factor H affects binding affinity to C-reactive protein. J Immunol 2007; 178 (6): 3831–3836.
Gold B, Merriam JE, Zernant J, Hancox LS, Taiber AJ, Gehrs K et al. Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat Genet 2006; 38 (4): 458–462.
McKay GJ, Silvestri G, Patterson CC, Hogg RE, Chakravarthy U, Hughes AE . Further assessment of the complement component 2 and factor B region associated with age-related macular degeneration. Invest Ophthalmol Vis Sci 2009; 50 (2): 533–539.
Richardson AJ, Islam FM, Guymer RH, Baird PN . Analysis of rare variants in the complement component 2 (C2) and factor B (BF) genes refine association for age-related macular degeneration (AMD). Invest Ophthalmol Vis Sci 2009; 50 (2): 540–543.
Weeks DE, Conley YP, Mah TS, Paul TO, Morse L, Ngo-Chang J et al. A full genome scan for age-related maculopathy. Hum Mol Genet 2000; 9 (9): 1329–1349.
Rivera A, Fisher SA, Fritsche LG, Keilhauer CN, Lichtner P, Meitinger T et al. Hypothetical LOC387715 is a second major susceptibility gene for age-related macular degeneration, contributing independently of complement factor H to disease risk. Hum Mol Genet 2005; 14 (21): 3227–3236.
DeWan A, Liu M, Hartman S, Zhang SS, Liu DT, Zhao C et al. HTRA1 promoter polymorphism in wet age-related macular degeneration. Science 2006; 314 (5801): 989–992.
Tocharus J, Tsuchiya A, Kajikawa M, Ueta Y, Oka C, Kawaichi M . Developmentally regulated expression of mouse HtrA3 and its role as an inhibitor of TGF-beta signaling. Dev Growth Differ 2004; 46 (3): 257–274.
Tong Y, Liao J, Zhang Y, Zhou J, Zhang H, Mao M . LOC387715/HTRA1 gene polymorphisms and susceptibility to age-related macular degeneration: a HuGE review and meta-analysis. Mol Vis 2010; 16: 1958–1981.
Kopplin LJ, Igo RP Jr., Wang Y, Sivakumaran TA, Hagstrom SA, Peachey NS et al. Genome-wide association identifies SKIV2L and MYRIP as protective factors for age-related macular degeneration. Genes Immun 2010; 11 (8): 609–621.
Kondo N, Honda S, Kuno S, Negi A . Role of RDBP and SKIV2L variants in the major histocompatibility complex class III region in polypoidal choroidal vasculopathy etiology. Ophthalmology 2009; 116 (8): 1502–1509.
Schaumberg DA, Hankinson SE, Guo Q, Rimm E, Hunter DJ . A prospective study of 2 major age-related macular degeneration susceptibility alleles and interactions with modifiable risk factors. Arch Ophthalmol 2007; 125 (1): 55–62.
Seddon JM, Reynolds R, Maller J, Fagerness JA, Daly MJ, Rosner B . Prediction model for prevalence and incidence of advanced age-related macular degeneration based on genetic, demographic, and environmental variables. Invest Ophthalmol Vis Sci 2009; 50 (5): 2044–2053.
McKibbin M, Ali M, Bansal S, Baxter PD, West K, Williams G et al. CFH, VEGF and HTRA1 promoter genotype may influence the response to intravitreal ranibizumab therapy for neovascular age-related macular degeneration. Br J Ophthalmol 2011; 96 (2): 208–212.
Stone EM, Fingert JH, Alward WL, Nguyen TD, Polansky JR, Sunden SL et al. Identification of a gene that causes primary open angle glaucoma. Science 1997; 275 (5300): 668–670.
Rezaie T, Child A, Hitchings R, Brice G, Miller L, Coca-Prados M et al. Adult-onset primary open-angle glaucoma caused by mutations in optineurin. Science 2002; 295 (5557): 1077–1079.
Footz TK, Johnson JL, Dubois S, Boivin N, Raymond V, Walter MA . Glaucoma-associated WDR36 variants encode functional defects in a yeast model system. Hum Mol Genet 2009; 18 (7): 1276–1287.
Nakano M, Ikeda Y, Taniguchi T, Yagi T, Fuwa M, Omi N et al. Three susceptible loci associated with primary open-angle glaucoma identified by genome-wide association study in a Japanese population. Proc Natl Acad Sci USA 2009; 106 (31): 12838–12842.
Rao KN, Kaur I, Chakrabarti S . Lack of association of three primary open-angle glaucoma-susceptible loci with primary glaucomas in an Indian population. Proc Natl Acad Sci USA 2009; 106 (44): E125–E126 author reply E127.
Thorleifsson G, Walters GB, Hewitt AW, Masson G, Helgason A, DeWan A et al. Common variants near CAV1 and CAV2 are associated with primary open-angle glaucoma. Nat Genet 2010; 42 (10): 906–909.
Kuehn MH, Wang K, Roos B, Stone EM, Kwon YH, Alward WL et al. Chromosome 7q31 POAG locus: ocular expression of caveolins and lack of association with POAG in a US cohort. Mol Vis 2011; 17: 430–435.
Mishra A, Yazar S, Hewitt AW, Mountain JA, Ang W, Pennell CE et al. Genetic variants near PDGFRA are associated with corneal curvature in Australians. Invest Ophthalmol Vis Sci 2012; 53 (11): 7131–7136.
Osman W, Low SK, Takahashi A, Kubo M, Nakamura Y . A genome-wide association study in the Japanese population confirms 9p21 and 14q23 as susceptibility loci for primary open angle glaucoma. Hum Mol Genet 2012; 21 (12): 2836–2842.
Burdon KP, Macgregor S, Hewitt AW, Sharma S, Chidlow G, Mills RA et al. Genome-wide association study identifies susceptibility loci for open angle glaucoma at TMCO1 and CDKN2B-AS1. Nat Genet 2011; 43 (6): 574–578.
Zhang Z, Mo D, Cong P, He Z, Ling F, Li A et al. Molecular cloning, expression patterns and subcellular localization of porcine TMCO1 gene. Mol Biol Rep 2010; 37 (3): 1611–1618.
Ramdas WD, van Koolwijk LM, Ikram MK, Jansonius NM, de Jong PT, Bergen AA et al. A genome-wide association study of optic disc parameters. PLoS Genet 2010; 6 (6): e1000978.
Wiggs JL, Yaspan BL, Hauser MA, Kang JH, Allingham RR, Olson LM et al. Common variants at 9p21 and 8q22 are associated with increased susceptibility to optic nerve degeneration in glaucoma. PLoS Genet 2012; 8 (4): e1002654.
Cao D, Jiao X, Liu X, Hennis A, Leske MC, Nemesure B et al. CDKN2B polymorphism is associated with primary open-angle glaucoma (POAG) in the Afro-Caribbean population of Barbados, West Indies. PLoS One 2012; 7 (6): e39278.
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology 2004; 111 (9): 1641–1648.
Yu-Wai-Man P, Stewart JD, Hudson G, Andrews RM, Griffiths PG, Birch MK et al. OPA1 increases the risk of normal but not high tension glaucoma. J Med Genet 2010; 47 (2): 120–125.
Toda Y, Tang S, Kashiwagi K, Mabuchi F, Iijima H, Tsukahara S et al. Mutations in the optineurin gene in Japanese patients with primary open-angle glaucoma and normal tension glaucoma. Am J Med Genet A 2004; 125A (1): 1–4.
Fan BJ, Liu K, Wang DY, Tham CC, Tam PO, Lam DS et al. Association of polymorphisms of tumor necrosis factor and tumor protein p53 with primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2010; 51 (8): 4110–4116.
Vickers JC, Craig JE, Stankovich J, McCormack GH, West AK, Dickinson JL et al. The apolipoprotein epsilon4 gene is associated with elevated risk of normal tension glaucoma. Mol Vis 2002; 8: 389–393.
Lam CY, Fan BJ, Wang DY, Tam PO, Yung Tham CC, Leung DY et al. Association of apolipoprotein E polymorphisms with normal tension glaucoma in a Chinese population. J Glaucoma 2006; 15 (3): 218–222.
Wiggs JL . Genetic etiologies of glaucoma. Arch Ophthalmol 2007; 125 (1): 30–37.
Meguro A, Inoko H, Ota M, Mizuki N, Bahram S . Genome-wide association study of normal tension glaucoma: common variants in SRBD1 and ELOVL5 contribute to disease susceptibility. Ophthalmology 2010; 117 (7): 1331–1338 e1335.
Mabuchi F, Sakurada Y, Kashiwagi K, Yamagata Z, Iijima H, Tsukahara S . Association between SRBD1 and ELOVL5 gene polymorphisms and primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2011; 52 (7): 4626–4629.
Nakano M, Ikeda Y, Tokuda Y, Fuwa M, Omi N, Ueno M et al. Common variants in CDKN2B-AS1 associated with optic-nerve vulnerability of glaucoma identified by genome-wide association studies in Japanese. PLoS One 2012; 7 (3): e33389.
Takamoto M, Kaburaki T, Mabuchi A, Araie M, Amano S, Aihara M et al. Common variants on chromosome 9p21 are associated with normal tension glaucoma. PLoS One 2012; 7 (7): e40107.
Pasquale LR, Loomis SJ, Kang JH, Yaspan BL, Abdrabou W, Budenz DL et al. CDKN2B-AS1 genotype-glaucoma feature correlations in primary open-angle glaucoma patients from the United States. Am J Ophthalmol 2012; 155 (2): 342–353.e5.
Mabuchi F, Sakurada Y, Kashiwagi K, Yamagata Z, Iijima H, Tsukahara S . Association between genetic variants associated with vertical cup-to-disc ratio and phenotypic features of primary open-angle glaucoma. Ophthalmology 2012; 119 (9): 1819–1825.
Gottfredsdottir MS, Sverrisson T, Musch DC, Stefansson E . Chronic open-angle glaucoma and associated ophthalmic findings in monozygotic twins and their spouses in Iceland. J Glaucoma 1999; 8 (2): 134–139.
Damji KF, Bains HS, Amjadi K, Dohadwala AA, Valberg JD, Chevrier R et al. Familial occurrence of pseudoexfoliation in Canada. Can J Ophthalmol 1999; 34 (5): 257–265.
Krumbiegel M, Pasutto F, Mardin CY, Weisschuh N, Paoli D, Gramer E et al. Exploring functional candidate genes for genetic association in german patients with pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Invest Ophthalmol Vis Sci 2009; 50 (6): 2796–2801.
Thorleifsson G, Magnusson KP, Sulem P, Walters GB, Gudbjartsson DF, Stefansson H et al. Common sequence variants in the LOXL1 gene confer susceptibility to exfoliation glaucoma. Science 2007; 317 (5843): 1397–1400.
Lemmela S, Forsman E, Onkamo P, Nurmi H, Laivuori H, Kivela T et al. Association of LOXL1 gene with Finnish exfoliation syndrome patients. J Hum Genet 2009; 54 (5): 289–297.
Ranty ML, Carpentier S, Cournot M, Rico-Lattes I, Malecaze F, Levade T et al. Ceramide production associated with retinal apoptosis after retinal detachment. Graefes Arch Clin Exp Ophthalmol 2009; 247 (2): 215–224.
Chen L, Jia L, Wang N, Tang G, Zhang C, Fan S et al. Evaluation of LOXL1 polymorphisms in exfoliation syndrome in a Chinese population. Mol Vis 2009; 15: 2349–2357.
Liu X, Zhao Y, Gao J, Pawlyk B, Starcher B, Spencer JA et al. Elastic fiber homeostasis requires lysyl oxidase-like 1 protein. Nat Genet 2004; 36 (2): 178–182.
Schlotzer-Schrehardt U, Naumann GO . Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol 2006; 141 (5): 921–937.
Khan TT, Li G, Navarro ID, Kastury RD, Zeil CJ, Semchyshyn TM et al. LOXL1 expression in lens capsule tissue specimens from individuals with pseudoexfoliation syndrome and glaucoma. Mol Vis 2010; 16: 2236–2241.
Krumbiegel M, Pasutto F, Schlotzer-Schrehardt U, Uebe S, Zenkel M, Mardin CY et al. Genome-wide association study with DNA pooling identifies variants at CNTNAP2 associated with pseudoexfoliation syndrome. Eur J Hum Genet 2011; 19 (2): 186–193.
Vithana EN, Khor CC, Qiao C, Nongpiur ME, George R, Chen LJ et al. Genome-wide association analyses identify three new susceptibility loci for primary angle closure glaucoma. Nat Genet 2012; 44 (10): 1142–1146.
Krachmer JH, Purcell JJ Jr., Young CW, Bucher KD . Corneal endothelial dystrophy. A study of 64 families. Arch Ophthalmol 1978; 96 (11): 2036–2039.
Biswas S, Munier FL, Yardley J, Hart-Holden N, Perveen R, Cousin P et al. Missense mutations in COL8A2, the gene encoding the alpha2 chain of type VIII collagen, cause two forms of corneal endothelial dystrophy. Hum Mol Genet 2001; 10 (21): 2415–2423.
Baratz KH, Tosakulwong N, Ryu E, Brown WL, Branham K, Chen W et al. E2-2 protein and Fuchs's corneal dystrophy. N Engl J Med 2010; 363 (11): 1016–1024.
Li YJ, Minear MA, Rimmler J, Zhao B, Balajonda E, Hauser MA et al. Replication of TCF4 through association and linkage studies in late-onset Fuchs endothelial corneal dystrophy. PLoS One 2011; 6 (4): e18044.
Thalamuthu A, Khor CC, Venkataraman D, Koh LW, Tan DT, Aung T et al. Association of TCF4 gene polymorphisms with fuchs corneal dystrophy in the Chinese. Invest Ophthalmol Vis Sci 2011.
Edwards M, McGhee CN, Dean S . The genetics of keratoconus. Clin Experiment Ophthalmol 2001; 29 (6): 345–351.
Li X, Bykhovskaya Y, Haritunians T, Siscovick D, Aldave A, Szczotka-Flynn L et al. A genome-wide association study identifies a potential novel gene locus for keratoconus, one of the commonest causes for corneal transplantation in developed countries. Hum Mol Genet 2012; 21 (2): 421–429.
Burdon KP, Macgregor S, Bykhovskaya Y, Javadiyan S, Li X, Laurie KJ et al. Association of polymorphisms in the hepatocyte growth factor gene promoter with keratoconus. Invest Ophthalmol Vis Sci 2011; 52 (11): 8514–8519.
Han W, Yap MK, Wang J, Yip SP . Family-based association analysis of hepatocyte growth factor (HGF) gene polymorphisms in high myopia. Invest Ophthalmol Vis Sci 2006; 47 (6): 2291–2299.
Awadalla MS, Thapa SS, Burdon KP, Hewitt AW, Craig JE . The association of hepatocyte growth factor (HGF) gene with primary angle closure glaucoma in the Nepalese population. Mol Vis 2011; 17: 2248–2254.
Patel S, Chen H, Tinkham NH, Zhang K . Genetic susceptibility of diabetic retinopathy. Curr Diab Rep 2008; 8 (4): 257–262.
Grassi MA, Tikhomirov A, Ramalingam S, Below JE, Cox NJ, Nicolae DL . Genome-wide meta-analysis for severe diabetic retinopathy. Hum Mol Genet 2011; 20 (12): 2472–2481.
Huang YC, Lin JM, Lin HJ, Chen CC, Chen SY, Tsai CH et al. Genome-wide association study of diabetic retinopathy in a Taiwanese population. Ophthalmology 2011; 118 (4): 642–648.
Grassi MA, Tikhomirov A, Ramalingam S, Lee KE, Hosseini SM, Klein BE et al. Replication analysis for severe diabetic retinopathy. Invest Ophthalmol Vis Sci 2012; 53 (4): 2377–2381.
Looker HC, Nelson RG, Chew E, Klein R, Klein BE, Knowler WC et al. Genome-wide linkage analyses to identify Loci for diabetic retinopathy. Diabetes 2007; 56 (4): 1160–1166.
Edwards AO . Clinical features of the congenital vitreoretinopathies. Eye (Lond) 2008; 22 (10): 1233–1242.
Mitry D, Williams L, Charteris DG, Fleck BW, Wright AF, Campbell H . Population based estimate of the sibling recurrence risk ratio for rhegmatogenous retinal detachment. Invest Ophthalmol Vis Sci 2011; 52 (5): 2551–2555.
Kirin M, Chandra A, Charteris DG, Hayward C, Campbell S, Celap I et al. Genome-wide association study identifies genetic risk underlying primary rhegmatogenous retinal detachment. Hum Mol Genet 2013; 22 (15): 3174–3185.
Rotstein NP, Miranda GE, Abrahan CE, German OL . Regulating survival and development in the retina: key roles for simple sphingolipids. J Lipid Res 2010; 51 (6): 1247–1262.
Wojciechowski R . Nature and nurture: the complex genetics of myopia and refractive error. Clin Genet 2011; 79 (4): 301–320.
Nakanishi H, Yamada R, Gotoh N, Hayashi H, Yamashiro K, Shimada N et al. A genome-wide association analysis identified a novel susceptible locus for pathological myopia at 11q24.1. PLoS Genet 2009; 5 (9): e1000660.
Andrew T, Maniatis N, Carbonaro F, Liew SH, Lau W, Spector TD et al. Identification and replication of three novel myopia common susceptibility gene loci on chromosome 3q26 using linkage and linkage disequilibrium mapping. PLoS Genet 2008; 4 (10): e1000220.
Nakanishi H, Yamada R, Gotoh N, Hayashi H, Yamashiro K, Shimada N et al. A genome-wide association analysis identified a novel susceptible locus for pathological myopia at 11q24.1. PLoS Genet 2009; 5 (9): e1000660.
Shi Y, Qu J, Zhang D, Zhao P, Zhang Q, Tam PO et al. Genetic variants at 13q12.12 are associated with high myopia in the Han Chinese population. Am J Hum Genet 2011; 88 (6): 805–813.
Hysi PG, Young TL, Mackey DA, Andrew T, Fernandez-Medarde A, Solouki AM et al. A genome-wide association study for myopia and refractive error identifies a susceptibility locus at 15q25. Nat Genet 2010; 42 (10): 902–905.
Mattingly RR, Macara IG . Phosphorylation-dependent activation of the Ras-GRF/CDC25Mm exchange factor by muscarinic receptors and G-protein beta gamma subunits. Nature 1996; 382 (6588): 268–272.
McBrien NA, Moghaddam HO, Reeder AP . Atropine reduces experimental myopia and eye enlargement via a nonaccommodative mechanism. Invest Ophthalmol Vis Sci 1993; 34 (1): 205–215.
Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL et al. Atropine for the treatment of childhood myopia. Ophthalmology 2006; 113 (12): 2285–2291.
Solouki AM, Verhoeven VJ, Van Duijn CM, Verkerk AJ, Ikram MK, Hysi PG et al. A genome-wide association study identifies a susceptibility locus for refractive errors and myopia at 15q14. Nat Genet 2010; 42 (10): 897–901.
Schache M, Richardson AJ, Mitchell P, Wang JJ, Rochtchina E, Viswanathan AC et al. Genetic association of refractive error and axial length with 15q14 but not 15q25 in the Blue Mountains Eye Study cohort. Ophthalmology 2012; 120 (2): 292–297.
Meng W, Butterworth J, Bradley DT, Hughes AE, Soler V, Calvas P et al. A genome-wide association study provides evidence for association of chromosome 8p23 (MYP10) and 10q21.1 (MYP15) with high myopia in the French population. Invest Ophthalmol Vis Sci 2012; 53 (13): 7983–7988.
Kiefer AK, Tung JY, Do CB, Hinds DA, Mountain JL, Francke U et al. Genome-wide analysis points to roles for extracellular matrix remodeling, the visual cycle, and neuronal development in myopia. PLoS Genet 2013; 9 (2): e1003299.
Verhoeven VJ, Hysi PG, Wojciechowski R, Fan Q, Guggenheim JA, Hohn R et al. Genome-wide meta-analyses of multiancestry cohorts identify multiple new susceptibility loci for refractive error and myopia. Nat Genet 2013; 45 (3): 314–318.
Verhoeven VJ, Hysi PG, Saw SM, Vitart V, Mirshahi A, Guggenheim JA et al. Large scale international replication and meta-analysis study confirms association of the 15q14 locus with myopia. The CREAM consortium. Hum Genet 2012; 131 (9): 1467–1480.
Macgregor S, Hewitt AW, Hysi PG, Ruddle JB, Medland SE, Henders AK et al. Genome-wide association identifies ATOH7 as a major gene determining human optic disc size. Hum Mol Genet 2010; 19 (13): 2716–2724.
Khor CC, Ramdas WD, Vithana EN, Cornes BK, Sim X, Tay WT et al. Genome-wide association studies in Asians confirm the involvement of ATOH7 and TGFBR3, and further identify CARD10 as a novel locus influencing optic disc area. Hum Mol Genet 2011; 20 (9): 1864–1872.
Wang L, Guo Y, Huang WJ, Ke X, Poyet JL, Manji GA et al. Card10 is a novel caspase recruitment domain/membrane-associated guanylate kinase family member that interacts with BCL10 and activates NF-kappa B. J Biol Chem 2001; 276 (24): 21405–21409.
Tan L, Schedl P, Song HJ, Garza D, Konsolaki M . The Toll—>NFkappaB signaling pathway mediates the neuropathological effects of the human Alzheimer's Abeta42 polypeptide in Drosophila. PLoS One 2008; 3 (12): e3966.
Ramdas WD, van Koolwijk LM, Lemij HG, Pasutto F, Cree AJ, Thorleifsson G et al. Common genetic variants associated with open-angle glaucoma. Hum Mol Genet 2011; 20 (12): 2464–2471.
Toh T, Liew SH, MacKinnon JR, Hewitt AW, Poulsen JL, Spector TD et al. Central corneal thickness is highly heritable: the twin eye studies. Invest Ophthalmol Vis Sci 2005; 46 (10): 3718–3722.
Lu Y, Dimasi DP, Hysi PG, Hewitt AW, Burdon KP, Toh T et al. Common genetic variants near the Brittle Cornea Syndrome locus ZNF469 influence the blinding disease risk factor central corneal thickness. PLoS Genet 2010; 6 (5): e1000947.
Berry FB, Skarie JM, Mirzayans F, Fortin Y, Hudson TJ, Raymond V et al. FOXC1 is required for cell viability and resistance to oxidative stress in the eye through the transcriptional regulation of FOXO1A. Hum Mol Genet 2008; 17 (4): 490–505.
Vitart V, Bencic G, Hayward C, Skunca Herman J, Huffman J, Campbell S et al. New loci associated with central cornea thickness include COL5A1, AKAP13 and AVGR8. Hum Mol Genet 2010; 19 (21): 4304–4311.
Ormestad M, Astorga J, Landgren H, Wang T, Johansson BR, Miura N et al. Foxf1 and Foxf2 control murine gut development by limiting mesenchymal Wnt signaling and promoting extracellular matrix production. Development 2006; 133 (5): 833–843.
Wenstrup RJ, Florer JB, Davidson JM, Phillips CL, Pfeiffer BJ, Menezes DW et al. Murine model of the Ehlers-Danlos syndrome. col5a1 haploinsufficiency disrupts collagen fibril assembly at multiple stages. J Biol Chem 2006; 281 (18): 12888–12895.
Hoehn R, Zeller T, Verhoeven VJ, Grus F, Adler M, Wolfs RC et al. Population-based meta-analysis in Caucasians confirms association with COL5A1 and ZNF469 but not COL8A2 with central corneal thickness. Hum Genet 2012; 131 (11): 1783–1793.
Han S, Chen P, Fan Q, Khor CC, Sim X, Tay WT et al. Association of variants in FRAP1 and PDGFRA with corneal curvature in Asian populations from Singapore. Hum Mol Genet 2011; 20 (18): 3693–3698.
Lassarre C, Ricort JM . Growth factor-specific regulation of insulin receptor substrate-1 expression in MCF-7 breast carcinoma cells: effects on the insulin-like growth factor signaling pathway. Endocrinology 2003; 144 (11): 4811–4819.
Lei H, Rheaume MA, Velez G, Mukai S, Kazlauskas A . Expression of PDGFR{alpha} is a determinant of the PVR potential of ARPE19 cells. Invest Ophthalmol Vis Sci 2011; 52 (9): 5016–5021.
Rabinowitz YS, Dong L, Wistow G . Gene expression profile studies of human keratoconus cornea for NEIBank: a novel cornea-expressed gene and the absence of transcripts for aquaporin 5. Invest Ophthalmol Vis Sci 2005; 46 (4): 1239–1246.
Fan Q, Zhou X, Khor CC, Cheng CY, Goh LK, Sim X et al. Genome-wide meta-analysis of five Asian cohorts identifies PDGFRA as a susceptibility locus for corneal astigmatism. PLoS Genet 2011; 7 (12): e1002402.
van Koolwijk LM, Ramdas WD, Ikram MK, Jansonius NM, Pasutto F, Hysi PG et al. Common genetic determinants of intraocular pressure and primary open-angle glaucoma. PLoS Genet 2012; 8 (5): e1002611.
Wiggs JL, Allingham RR, Hossain A, Kern J, Auguste J, DelBono EA et al. Genome-wide scan for adult onset primary open angle glaucoma. Hum Mol Genet 2000; 9 (7): 1109–1117.
Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ et al. Finding the missing heritability of complex diseases. Nature 2009; 461 (7265): 747–753.
Acknowledgements
We acknowledge a proportion of their support by the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. We also acknowledge support from the Royal College of Surgeons of Edinburgh, Fight for Sight UK and the Special Trustees of Moorfields Eye Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Chandra, A., Mitry, D., Wright, A. et al. Genome-wide association studies: applications and insights gained in Ophthalmology. Eye 28, 1066–1079 (2014). https://doi.org/10.1038/eye.2014.145
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.145
This article is cited by
-
Screening of single nucleotide polymorphisms among fuchs’ endothelial corneal dystrophy subjects in Malaysia
Egyptian Journal of Medical Human Genetics (2021)
-
Corneal cell therapy: with iPSCs, it is no more a far-sight
Stem Cell Research & Therapy (2018)