Abstract
Purpose
The purpose of the study was to determine what proportion of new certifications between 1 April 2007 and 31 March 2008 could be attributed to age-related macular degeneration (AMD) and to describe the AMD-certified population in England and Wales.
Methods
An electronic version of the Certificate of Vision Impairment form (CVI), the ECVI, was used at the certifications office to transfer information from the paper-based certificates into a database. The electronic certifications data set was queried for all certificates completed between 1 April 2007 and 31 March 2008 with the main cause of certifiable visual loss being AMD or with the main cause of certifiable visual loss being multiple pathology but a contributory cause being AMD. The electronic data set was adapted so that a distinction could be made between geographic atrophy (GA) and neovascular AMD (nAMD).
Results
The Certifications Office received 23 185 CVIs between April 2007 and March 2008, of whom 9823 (42%) were people registered severely sight impaired (SSI) and 12 607 (52%) were certified as sight impaired (SI). AMD contributed to 13 000 causes of registration on the CVI forms during this period and was the main cause in 11 015 people. In these 11 015 people, GA accounted for 49.3%, nAMD 35.1%, and AMD not specified 15.7%.
Conclusions
The data in this report provide detailed information on CVI registration due to AMD before the widespread adoption of ranibizumab therapy in NHS practice and provide an insight into the burden of vision loss due to AMD at a time of great change in the management of nAMD.
Similar content being viewed by others
Introduction
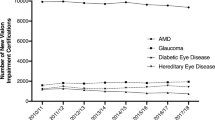
The number of blind people has been recorded in Britain since 1851, and documentation of the causes of low vision began in 1950.1, 2, 3, 4, 5, 6 Sight-impairment certification figures are used by the Department of Health in England and Wales to derive an indicator for preventable vision loss that is included in the Public Health Outcomes Framework. To be registered as sight impaired in England and Wales, an individual must be certified as visually impaired by a consultant ophthalmologist who certifies them vision impaired by completing a form provided by the Department of Health (the Certificate of Vision Impairment form (CVI)). A copy of this certificate is sent to the Certifications Office in London for anonymized epidemiological analysis. In the past, every 3 years, the Department of Health has released figures on the numbers of people newly registered sight impaired and the total number on the register for blindness and partial sight in England and Wales. These figures are compiled from information sent by local councils to the Information Centre for Health and Social Care (IC). The figures released by the IC do not contain any information on causes of vision loss.
The most recent complete analysis conducted on cause of visual loss leading to sight impairment registration was for certifications made between 1 April 2007 and 31 March 2008. This analysis reported the main cause of certifiable visual impairment and reported the proportion of patients with different causes of sight impairment.7 The main cause of certifiable visual loss was degeneration of the macula and posterior pole, mostly age-related macular degeneration (AMD), accounting for 58.6% for severe sight impairment and 57.2% of cases of sight impairment.7 Since then, new therapies for the treatment of neovascular AMD have been brought to market. The first therapy approved by the National Institute of Health and Clinical Excellence (NICE) was ranibizumab (Lucentis, Novartis, Basel, Switzerland) in August 2008. Given by intravitreous injection to the affected eye, results from phase III trials reported between 30 and 40% of patients gaining 3 lines or more of visual acuity with over 90% of patients remaining stable with less than 3 lines of vision loss over 2 years of treatment. The introduction of this therapy into the NHS during 2008 could potentially affect future numbers of patients being registered as sight impaired.8
This paper explores the sight-impairment certification data set further to provide detailed figures of the numbers of people certified with different types of AMD by age, sex, and ethnicity made between 1 April 2007 and 31 March 2008. The results provide a baseline measure of sight-impartment certification because of AMD at the time of introduction of ranibizumab therapy into the NHS.
Materials and methods
An electronic version of the CVI, the ECVI, was used at the certifications office to transfer information from the paper-based certificates into a database. Part C of the CVI form collects information on the visual loss. It contains a list of common diagnoses and instructs the individual completing the form to select the main cause of vision loss in each eye using an asterisk or a circle. Guidelines are provided in the ‘explanatory notes for Consultant ophthalmologists’ as to how to select a single main cause of visual loss where this is not evident.
The electronic certifications data set was queried for all certificates completed between 1 April 2007 and 31 March 2008 with the main cause of certifiable visual loss being AMD or with the main cause of certifiable visual loss being multiple pathology but a contributory cause being AMD.
Multiple pathology features where the consultant ophthalmologist who completed the CVI has not indicated a single cause of visual loss is where there may be differing causes in the two eyes or more than one cause within one eye and the ophthalmologist is unable to decide what contributes most to the certifiable visual loss. This paper’s analysis is based on the same data set previously published, except that this is a more detailed analysis of the e-data to allow dissection of the data on types of AMD.7
The CVI presents ICD-10 codes, but the code for ‘age related macular degeneration - subretinal neovascularisation’ is the same as that for ‘age-related macular/geographic macular atrophy’ (H35.3), and hence the electronic data set was adapted so that that a distinction could be made between the two.
The certifications could then be grouped into one of the four categories:
-
1)
Geographic (GA) AMD;
-
2)
Neovascular (nAMD) AMD;
-
3)
AMD (not otherwise specified (NOS)); and
-
4)
Multiple causes (with a contributory cause being AMD of any type). The certifications data set allows up to two diagnoses to be recorded for each eye in the data set, so that a single patient can have two causes for their right eye and two causes for their left eye.
Category 4, where the main cause of certification was classed as ‘multiple pathology’, was then classified into one of the four categories:
-
1)
GA AMD (only GA AMD was recorded on the CVI for that person);
-
2)
nAMD AMD (only nAMD was recorded on the CVI for that person);
-
3)
Mixed AMD (both GA AMD and nAMD were recorded on the CVI); and
-
4)
AMD (NOS) (AMD was recorded but not in detail).
Information from both classifications (ie, the main cause or the reclassified multiple pathology) was then used to derive a single classification for each subject:
-
1
GA AMD: (main cause was geographic atrophy AMD or main cause was multiple pathology and this had been categorized as dry AMD);
-
2
nAMD;
-
3
mixed AMD; and
-
4
AMD NOS.
These classifications were then cross-tabulated against each of
-
1)
Visual status: severe sight impairment, sight impairment, or not recorded.
-
2)
Sex: male, female, not recorded.
-
3)
Age group (age banded in 5-year age groups from 50 years of age onwards).
-
4)
Ethnic origin (where stated on the form): using the Office of National Statistics Level 1 categories.
To assess prevalence per 100 000 of AMD certification in the >50-year-old group, census data from 2001 were used to predict population estimates of the >50-year-old group from the government statistics office.9 The same was done for ethnicity population estimates.10
Results
The Certifications Office received 23 185 CVIs between April 2007 and March 2008, of whom 9823 (42%) were people registered as severely sight impaired (SSI) and 12 607 (52%) were certified as sight impaired (SI). The remaining 755 forms did not state the certification status.7
AMD contributed to sight-impairment registration on the CVI forms for 13 000 patients during this period, and was the main cause in 11 015 patients. In these 11 015 patients, GA accounted for 49.3%, nAMD 35.1%, and AMD not specified 15.7%. Table 1 shows the classifications of AMD CVIs.
The AMD CVIs listed as multiple pathology including AMD were also analysed. GA AMD was still the dominant cause of AMD CVI registration in this subgroup, accounting for 64% of the 1985 patients. nAMD was still second with 28.6%, with mixed AMD and AMD NOS 7.3% and 0.2%, respectively.
The final diagnostic classification of AMD CVIs with over half of patients with vision impairment because of GA AMD is seen in Table 2. A specific classification was not recorded for 1729 (13.3%) of the forms.
It is shown in Table 3 that there were more AMD CVIs for SI than for SSI (6972 (53.6%) vs 5674 (43.6%)). However, when looked by type of AMD, it can be seen that a different pattern is seen for nAMD than for other types of AMD, with there being more SSI certifications than SI certifications (2367 (53.5%) vs 1958 (44.2%)).
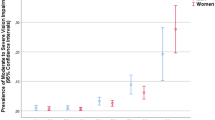
There were more women certified with SI because of AMD than men. This was true both in total and also by type of AMD—in all categories, over 60% of subjects were female.
Table 4 shows that overall there were more AMD certifications for individuals aged between 85 and 89 years. The age group most likely to be newly certified with nAMD was 80–84 years, and this is slightly earlier than the age group most likely to be newly certified with GA.
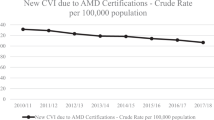
The population >50 years old in 2007–2008 was 21 million from the national census figures, giving a prevalence of blind registration of 0.06% (60 per 100 000 population). The population >85 years old was 1.3 million during that time period, giving a prevalence of 0.5% (500 per 100 000 population).9
When we cross-tabulated age against sex (Table 5), there was an increased number of women newly certified with vision impairment because of AMD compared with men. This was not explained by differences in age, just as there were more women than men in each age band examined.
The majority of AMD CVIs were for white subjects 88.2% (n=11 473), with GA AMD accounting for 5909 CVIs, nAMD accounting for 3901 CVIs, and mixed AMD and AMD (NOS) accounting for 134 and 1533 CVIs, respectively. The next largest group was Asian or Asian British with 122 CVIs, with GA accounting for 65 CVIs, nAMD accounting for 43 CVIs, and mixed AMD and AMD (NOS) accounting for 1 and 13 CVIs, respectively. The other ethnic groups had very small numbers of CVIs—mixed 9, Black or Black British 14, and Chinese or other ethnic groups 19. If we look at the population of these groups, the prevalence of AMD per 100 000 population for Asians is 20, Black 6, mixed 10, and Chinese 30.10 However, it is to be noted that data on ethnicity were missing for 10.5% of the CVIs. If the ethnic origin distribution is examined only from forms where ethnicity was recorded, 98.5% of forms were for white subjects.
Discussion
Sight-impairment certification provides a measure of the burden of vision loss in England and Wales. This is important to health-care commissioners, health-care providers, and to patients as it provides one way of measuring trends in vision loss across England and Wales. Indeed, the Department of Health uses these data to derive an indicator for preventable vision loss that is included in the Public Health Outcomes Framework.
A previous report described the different causes of vision loss in patients registered as sight impaired in England and Wales in 2007–2008. This confirmed that AMD was the single largest cause of sight-impairment certification. This information is particularly important in view of the recent paradigm shift in the management of nAMD with the introduction of anti-VEGF agents into clinical practice. In this report, we describe the relative contributions of nAMD and GA to cases of sight-impairment certification.
The results in this report provide more details on the cases of sight-impairment registration due to AMD. It shows that in 2007–2008, there were more patients with GA registered as SI or SSI. The numbers of patients certified as SSI were similar for both nAMD and GA; however, there were more patients with GA who were certified as SI. In patients registered as sight impaired because of nAMD, SSI was more common than SI registration. However, sending a copy of the CVI to the certifications office is not a statutory requirement for hospitals, and it is therefore possible that certifications do not correlate exactly to registrations. A comparison of certification data with registration data for England in 2007–2008 suggested that certifications were received for 92% of SSIs and 91.5% of SIs. There were 3% of certificates that did not state whether the patient was a SI or SSI.6
The analysis of sight impairment certification because of AMD by age bands showed a very similar pattern to that found by Owen et al11 in a large meta-analysis looking at the burden of visual loss caused by AMD in the United Kingdom.4 What is striking about this is that <4% of AMD certifications were for subjects aged <70 years, and the peak for nAMD appears to occur slightly earlier at 80–84 years of age than for GA at 85–89 years of age. In 2010, 10 million people in the United Kingdom were >65 years old. The latest projections are for 5½ million more elderly people in 20 years time and the number will nearly double to ∼19 million by 2050.
Within this total, the number of very old people grows even faster. There are currently 3 million people aged >80 years, and this is projected to almost double by 2030 and reach 8 million by 2050. Although 1 in 6 of the UK population is currently aged ≥65 years, by 2050 this proportion will rise to one-quarter. This means that the number of certifiable patients with AMD will also increase and with it the burden on NHS services.12
In 2007–2008, as stated in the results, the prevalence of blind registration was 60 per 100 000 population in >50-year olds with AMD, and this is similar to the prevalence stated in other papers before the start of injections in the anti-VEGF era.13
It is important to note that all these figures describe certifications. In order to be certified, an individual needs to be examined by a consultant ophthalmologist. Clearly, there may be many individuals in the United Kingdom who never seek support for their sight loss. They may assume that sight loss is simply an inexorable and irreversible part of ageing and may also have other systemic comorbidities that may make it difficult for them to see an ophthalmologist in the hospital setting. It is therefore possible that these figures are underestimates of AMD visual impairment; however, this should not detract from the value of these data. There were still 13 000 people who were offered and accepted certification as a result of AMD in England and Wales in 2007–2008. Capturing this number should allow better planning of appropriate health-care resources and hopefully better services for those in need.
There were more AMD sight-impairment certification cases in women than men, and this was true for each age band and for both nAMD and GA subtypes. This may suggest that vision loss because of AMD is more common in women than in men, but similar findings would also be seen if women with AMD were more likely than men to be offered and/or to accept certification. This may also suggest that women live longer than men and hence are more likely to develop AMD that is more common in individuals who are >80 years old. Other studies have reported more AMD blindness in women than men but this area needs further research.5
Of those in whom ethnic origin was stated, over 98.5% of forms were for subjects of white origin. In 2007, the ethnic minority population was 15.7%.10 This may reflect a lower incidence of disease in subjects of non-white origin that could be genetic14 or dietary, but may also suggest unequal access to health care.15
Considering the subtype of AMD, surprisingly there were more cases of GA accounting for sight-impairment registration than cases of nAMD. This may reflect the greater prevalence of GA but may also be because of underdetection of nAMD coexisting with GA in longstanding cases.
Ranibizumab was approved by NICE as a cost-effective therapy for nAMD with publication of the Final Appraisal Determination in August 2008 after the period of data collection for this report. This has led to a dramatic change in management for patients with nAMD, and results from clinical trials show that novel pharmacotherapies are able to improve vision in over 40% of patients with nAMD over 1–2 years;16, 17, 18, 19, 20 however, outcomes in clinical practice and with long-term follow-up are more uncertain.21, 22 Effective pharmacotherapies have the potential to positively affect the burden of vision loss because of AMD, but the availability of a potentially effective treatment may lead to changes in attitudes toward sight-impairment registration among both ophthalmologists and patients. This may cause delay in sight-impairment registration in the hope of the therapy leading to improvement in vision. Bunce and colleagues23 found that patients who require treatment for their sight impairment are almost 3 times less likely to be certified than those in whom treatment is not indicated.
The data in this report therefore provide detailed information on CVI registration because of AMD before the widespread adoption of ranibizumab therapy in NHS practice and provide an insight into the burden of vision loss because of AMD at a time of great change in the management of nAMD. More work is needed to understand the impact of the introduction of pharmacotherapy on the burden of sight loss because of AMD and the incidence of sight-impairment registration. Further research is also needed on the impact of therapies on attitudes to sight-impairment registration in both patients and ophthalmologists in an effort to ensure that AMD patients with vision loss seek support promptly to help minimize the impact of vision loss on everyday life.

References
Sorsby A . The Causes of Blindness in England 1948–50. HMSO: London, 1953.
Sorsby A . Blindness in England 1951–54. HMSO: London, 1956.
Sorsby A . The Incidence and Causes of Blindness in England and Wales 1948–62. Reports of Public Health and Medical Subjects Vol 114. HMSO: London, 1966.
Sorsby A . The Incidence and Causes of Blindness in England and Wales 1963–8. Reports of Public Health and Medical Subjects Vol 128. HMSO: London, 1972.
Department of Health and Social Security. Blindness and Partial Sight in England 1969–76. Reports of Public Health and Medical Subjects Vol 129. HMSO: London, 1979.
Government Statistical Service. Causes of Blindness and Partial Sight among Adults in 1976–77 and 1980/81. HMSO: London, 1988.
Bunce C, Xing W, Wormald R . Causes of blind and partial sight certifications in England and Wales April 2007–March 2008. Eye 2010; 24: 1692–1699.
Rostron E, McKibbin M . Visual impairment certification secondary to ARMD in Leeds, 2005–2010: is the incidence falling? Eye (Lond) 2012; 26: 933–936.
Government Statistical Service. Population estimates for UK, England and Wales 2007–2008. www.statistics.gov.uk.
Lievesley N The future ageing of the ethnic population of England and Wales. www.cpa.org.uk.
Owen CG, Fletcher AE, Donoghue M, Rudnicka AR . How big is the burden of visual loss caused by age related macular degeneration in the United Kingdom. Br J Ophthalmol 2003; 87: 312–317.
Parliament UK. The aging population. http://www.parliament.uk/business/publications/research/key-issues-for-the-new-parliament/value-for-money-in-public-services/the-ageing-population/.
Bloch SB, Larsen M, Munch IC . Incidence of legal blindness from age-related macular degeneration in Denmark: year 2000 to 2010. Am J Ophthalmol 153 (2): 209–213.
Klein R, Li X, Kuo JZ, Klein BE, Cotch MF, Wong TY et al. Associations of candidate genes to age-related macular degeneration among racial/ethnic groups in the multi-ethnic study of atherosclerosis. Am J Ophthalmol 2013; 156 (5): 1010–1020.e1.
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O 2nd . Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep 2003; 118 (4): 293–302.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et alfor the MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T . Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology 2009; 116: 57–65.
ABC Trial Investigators Tufail A, Patel PJ, Egan C, Hykin P, da Cruz L, Gregor Z et al. Bevacizumab for neovascular age related macular degeneration (ABC Trial): multicentre randomised double masked study. BMJ 2010; 340: c2459.
IVAN Study Investigators Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S et al. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. [published erratum appears in Ophthalmology 2012;119(8):1508] Ophthalmology 2012; 119 (7): 1399–1411.
Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012; 119 (7): 1388–1398.
Cohen SY, Mimoun G, Oubraham H, Zourdani A, Malbrel C, Queré S et alfor the LUMIERE Study Group. Changes in visual acuity in patients with wet age-related macular degeneration treated with intravitreal ranibizumab in daily clinical practice: The Lumiere Study. Retina 2013; 33 (3): 474–481.
Cohen SY, Dubois L, Tadayoni R, Fajnkuchen F, Nghiem-Buffet S, Delahaye-Mazza C et al. Results of one-year’s treatment with ranibizumab for exudative age-related macular degeneration in a clinical setting. Am J Ophthalmol 2009; 148 (3): 409–413.
Leamon S, Simkiss P, Zekite A, Seeberan R, Bunce C Numbers of people newly certified and registered with sight loss in England 2010–2011. Vision UK Conference 2012.
Acknowledgements
This study was supported by a grant from Guide Dogs, the Macular Disease Society, and NIHR support. The views expressed in this paper are those of the author and not necessarily any funding body or the Department of Health. The data captured by the CVI are DH copyright and this work was made possible by collaboration with the Royal College of Ophthalmologists.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rees, A., Zekite, A., Bunce, C. et al. How many people in England and Wales are registered partially sighted or blind because of age-related macular degeneration?. Eye 28, 832–837 (2014). https://doi.org/10.1038/eye.2014.103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.103
This article is cited by
-
Piloting a forced-choice task to elicit treatment preferences in geographic atrophy
BMC Research Notes (2023)
-
Intravitreal treatment for geographic atrophy: coming soon to a patient near you?
Eye (2022)
-
Agreement between ophthalmologists and optometrists in the certification of vision impairment
Eye (2021)
-
Metformin, A Potential Role in Age-Related Macular Degeneration: A Systematic Review and Meta-Analysis
Ophthalmology and Therapy (2021)
-
Comment on: ‘You’ve got dry macular degeneration, end of story: a qualitative study into the experience of living with non-neovascular age-related macular degeneration’
Eye (2020)