Abstract
Purpose
To determine the influence of diabetes and diabetes type on ocular outcomes following central retinal vein occlusion (CRVO).
Methods
Retrospective chart review of all patients evaluated over a 4-year period in a tertiary diabetes eye care center. Ophthalmic findings were recorded including visual acuity and the presence of retinal neovascularization at presentation, after 3–6 months, and at last follow-up.
Results
The records of 19 648 patients (13 571 diabetic; 6077 nondiabetic) were reviewed. The prevalence of CRVO in diabetic patients (N=72) and nondiabetic patients (N=27) were 0.5 and 0.4%, respectively. Disc neovascularization (21.3 vs 0.0%, P=0.05) and panretinal photocoagulation (PRP) (48.7 vs 21.4%, P=0.01) were more common in diabetic patients compared with nondiabetic patients. Compared with type 2 diabetic patients, retinal neovascularization (28.6 vs 3.7%, P=0.004) and subsequent PRP (78.6 vs 41.9%, P=0.01) were more likely in type 1 patients. Optic nerve head collateral vessels (CVs) were observed less than half as often (21.4 vs 56.5%, P=0.04) in patients with type 1 diabetes. Presence of optic nerve head CVs at baseline was associated with less likelihood of PRP (14.3 vs 46.1%, P=0.03).
Conclusions
In this cohort, the rates of CRVO in diabetic and nondiabetic patients were similar to previously published population-based studies. Following CRVO, diabetic patients had higher rates of disc neovascularization and were more likely to require subsequent PRP than nondiabetic patients. As compared with CRVO patients with type 2 diabetes, patients with type 1 diabetes and CRVO had worse anatomic outcomes with substantially increased risks of retinal neovascularization and PRP; however, final visual acuity outcomes were similar.
Similar content being viewed by others
Introduction
Central retinal vein occlusion (CRVO) is a retinal vascular disease that frequently results in significant visual loss.1, 2, 3 Population-based studies estimate that the prevalence ranges from 0.1%4 to 0.8%5 and that the 15-year cumulative incidence is 0.5%.6 CRVO is observed in all age groups, with increasing incidence with advancing age.6, 7 CRVO is classified into two distinct groups with different visual outcomes: nonischemic and ischemic.8 The ischemic CRVO generally presents with poorer visual acuity at baseline, worse visual prognosis and higher risk of developing neovascularization as compared with the nonischemic group.8, 9 Visual decline in patients with CRVO may occur from ischemic injury to the retina, macular edema, vitreous hemorrhage, retinal neovascularization, and/or neovascular glaucoma.10 There is an associated vision-related decline in quality of life.11
Multiple systemic and ocular conditions are associated with CRVO.7, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 Many studies have confirmed higher prevalence of diabetes mellitus (DM) in patients with CRVO.16, 21, 22, 23, 24 Co-existing DM is reported in 10–34% of patients with CRVO and may affect the natural history in this subgroup of patients.25, 26 Patients with DM have a higher risk of subsequently developing ischemic CRVO and neovascular complications.14, 27 A higher prevalence of DM has been noted among those patients developing CRVO. However, detailed assessment of risk factors in DM patients that may predict the development of retinal ischemia and neovascularization following CRVO is lacking. The influence of DM type on the natural course of CRVO is also unknown. In the current study, we compared nondiabetic and diabetic patients with CRVO and evaluated the effect of diabetes type and systemic and ocular risk factors on ophthalmic outcomes in an academic tertiary care diabetes center.
Materials and methods
A structured, retrospective medical record review of all patients seen at the Beetham Eye Institute of the Joslin Diabetes Center from 1 January 2004 to 15 November 2008 was performed. The study was approved by the Joslin Diabetes Center Institutional Review Board prior to the review of the patients’ records. A structured electronic search query from the electronic medical record was used to identify all CRVO patients with ICD-9 coded diagnosis of 362.35 (CRVO). The individual medical records of all identified patients were retrieved and all pertinent information was recorded on a standardized form. The diagnoses of CRVO and DM were confirmed based on the systemic and clinical characteristics documented at the initial visit. Diabetes type was determined based on the physician coded ICD-9 diagnosis in the patient’s electronic medical records.
Baseline demographic factors including age, gender, ethnicity, and pertinent systemic medical risk factors associated with progression of diabetic retinopathy (DR) or increased risk of CRVO were noted at the initial visit. The systemic medical and ophthalmic risk factors evaluated included those published in previous studies: hypertension, DM, hyperlipidemia, cardiovascular disease, smoking history, open-angle glaucoma, and elevated intraocular pressure (IOP).7, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 The ophthalmic findings from all patients at the initial (visit I), 4-month (visit M; window=3–6 months), and final follow-up (visit F) were recorded. Data from the visit prior to development of CRVO were also recorded when available (visit P). If a patient was diagnosed with bilateral CRVO, ophthalmic findings were recorded individually for each eye at each of the three specified visits.
Recorded visual and anatomic outcomes included best-corrected Early Treatment Diabetic Retinopathy Study (ETDRS) protocol visual acuity; IOP measured by Goldman applanation tonometry; presence of neovascularization of the iris and/or angle, optic disc, or elsewhere on the retina; presence of neovascular glaucoma; clinical DR severity; presence of macular edema; and presence of optic nerve head collateral vessels (CVs). All refractionists, visual acuity examiners, and visual examination rooms were clinical trial certified. Standardized templates were used to record the presence of neovascularization, CV, DR severity, and macular edema. Consistency of ophthalmologists’ grading of DR at the Beetham Eye Institute has been established as comparable to the inter-reader results of the ETDRS study and masked evaluation of ETDRS standardized photographs.28 Fundus photography and fluorescein angiography were reviewed when the images were available. Retinal ischemia was established based on capillary nonperfusion observed on fluorescein angiography. The dates of all ophthalmic procedures after onset of CRVO were recorded, including those for cataract surgery, glaucoma surgery, intravitreal injection, panretinal laser photocoagulation, vitrectomy, and radial optic neurotomy.
We certify that all applicable institutional and governmental regulations were followed during this research.
Statistical analysis
All analyses were performed using Statistical Analyses System software V9.2 (SAS Institute, Cary, NC, USA). For patients with fewer than three visits, the ‘last observation carried forward’ method was used. If the last visit (visit F) was within 3–6 months of baseline, data from this visit were also used for analyses pertaining to the visit M 3–6-month follow-up. Nonparametric analyses (Wilcoxon rank sums) were used to compare distributions of continuous variables between groups. The χ2-test was used to compare frequencies of categorical variables. For these exploratory analyses, P<0.05 was defined as statistically significant.
Results
A total of 104 eyes of 99 patients with CRVO were identified from the 5-year cohort of 19 648 patients. The overall prevalence was 0.5%. The right eye only was affected in 46 patients (44.2%) and 5 patients (5.1%) had bilateral CRVO. Of the 13 571 DM patients, 76 eyes of 72 patients developed CRVO (0.5%). Among the 6077 nondiabetic patients, 28 eyes of 27 patients developed CRVO (0.4%). Individual eye involvement and bilateral CRVO prevalence did not differ significantly between DM and nondiabetic patients. The mean age for the entire CRVO cohort was 65.3±14.2 (range: 30.1–95.1) years. CRVO patients with DM tended to be younger compared with CRVO patients without DM but this difference was not statistically significant (63.9 vs 69.0 years, P=0.22). The epidemiological characteristics of the study population are presented in Table 1.
Comorbidities in diabetic vs nondiabetic CRVO patients
Among CRVO patients, the prevalence of systemic hypertension, hyperlipidemia, and cardiovascular disease was 78.8, 56.6 and 34.3%, respectively. Less prevalent was the presence of anemia (9.1%) and renal disease (7.1%). The prevalence of systemic hypertension (84.7 vs 63.0%, P=0.02), use of antihypertensive medications (80.6 vs 51.9%, P<0.01), cardiovascular disease (40.3 vs 18.5%, P=0.04), hyperlipidemia (66.7 vs 29.6%, P<0.001), and hyperlipidemia treatment (61.1 vs 25.9%, P=0.003) were significantly higher in DM patients than in nondiabetic patients (Table 2). In contrast, systolic and diastolic blood pressures (BPs) were not significantly different in DM patients (mean BP: 136/75 mmHg) compared with nondiabetic patients (mean BP: 131/75 mmHg). DM patients had a higher prevalence of renal disease (9.7 vs 0.0%, P=0.93), anemia (9.7 vs 7.4%, P=0.72), smoking history (23.6 vs 22.2%, P=0.80), and use of anticoagulation medications (41.7 vs 37.0%, P=0.78) such as aspirin, clopidogrel, and/or warfarin as compared with nondiabetic patients; however, these differences were not statistically significant.
DR was present at baseline exam in 66.7% of CRVO eyes of DM patients. Among these eyes with DR, 64.6% had mild nonproliferative DR (NPDR), 12.5% had moderate–severe NPDR, and 22.9% had proliferative DR (PDR). At the first visit following CRVO (3–6 months), there was an increase in the percentage of patients with PDR (from 15.3 to 23.9%) as well as moderate NPDR (from 4.2 to 7.5%) and a decrease in the percentage of patients with mild NPDR (from 43.1 to 28.4%).
CRVO outcomes in diabetic vs nondiabetic patients
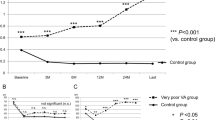
In the subgroup of eyes with visits prior to the onset of the CRVO (N=88), the mean logMAR visual acuity was 0.17 (Snellen equivalent 20/30) prior to developing CRVO. Mean visual acuity at the initial visit after CRVO declined to 0.79 (Snellen equivalent 20/123) and the mean logMAR at last follow-up was 1.16 (Snellen equivalent 20/290). Patients with DM tended to have slightly worse logMAR visual acuity at the initial visit after CRVO (0.8316 vs 0.6653; P=0.89) and final visit (1.1771 vs 1.1206; P=0.95); however, these differences were not statistically significant.
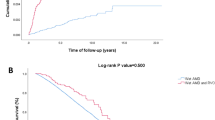
Ophthalmic procedure frequencies are shown in Table 3. Panretinal photocoagulation (PRP) after CRVO was more than twice as common in eyes of patients with DM (48.7%) than in eyes of patients without DM (21.4%, P=0.01). The presence of optic nerve head CVs at initial visit was associated with more than threefold lower rates of PRP (14.3 vs 46.1%, P=0.03). Cataract extraction rates were similar in CRVO eyes with DM compared with CRVO eyes without DM (15.8 vs 10.7%, P=0.20). Similarly, there were no statistical differences noted for intravitreal injection, pars plana vitrectomy, glaucoma surgery, or radial optic neurotomy.
Ischemic vs nonischemic CRVO outcomes in diabetic and nondiabetic patients
Fluorescein angiography was available and reviewed according to Standard of Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study criteria in 54 eyes (52%). Baseline parameters of eyes with angiograms did not differ significantly from eyes where angiograms were not available. As shown in Table 1, 6 (11%) of the 54 evaluated eyes had ischemic CRVO by fluorescein angiography, and 5 (83.3%) of these eyes were from diabetic patients (1 eye type 1 DM, 4 eyes type 2 DM). In this partial cohort, trends were evident, but none reached statistical significance. Ischemic CRVO tended to be more common in eyes of subjects with DM than in those without DM (13.9 vs 5.6%, P=0.36). Ischemic CRVO tended to be slightly more common in eyes with type 2 DM than in eyes with type 1 DM (15.4 vs 10%, P=0.68). However, owing to the small number of ischemic CRVO in this cohort overall, comparisons of risks for ischemic vs nonischemic CRVO could not be analyzed.
CRVO and glaucoma
Primary open-angle glaucoma and use of glaucoma medications were more common in nondiabetic patients. Nondiabetic subjects with CRVO were over four times more likely to be using glaucoma medications prior to CRVO diagnosis (62.5 vs 13.2%, P=0.002) and had a lower mean IOP (14.0 vs 16.1 mmHg, P=0.02) than diabetic subjects who developed CRVO. All eyes with diabetes and ischemic CRVO were on glaucoma medications on follow-up (100 vs 26,9%, P=0.03) and on the final visit (100 vs 46.4%, P=0.05).
CRVO outcomes by diabetes type
Among diabetes patients with CRVO, 19.4% (n=14) had type 1 DM and 80.6% (n=58) had type 2 DM. The mean duration of DM was 16.0±10.4 (1.5–45.0) years, with a shorter duration observed among type 1 DM patients (12.1±6.7 years) than for type 2 DM patients (27.1±10.0 years, P<0.0001). The mean HbA1c in DM patients was 7.7±1.3% (5.0–11.3). The mean HbA1c was higher in type 1 DM (8.4±1.2%) than in type 2 DM (7.6±1.2%, P=0.02) (Table 4).
Neovascularization of all types tended to be more common in DM patients with CRVO than in nondiabetic patients with CRVO. This finding was particularly true for neovascularization of the disc (NVD) after CRVO, which was much more likely in eyes of DM patients as compared with nondiabetic patients (21.3 vs 0.0%, P=0.05, Table 5). Compared with type 2 DM, retinal neovascularization from CRVO was eight times more likely (28.6 vs 3.7%, P=0.004) and optic nerve head CVs were observed less than half as often (21.4 vs 56.5%, P=0.04) in patients with type 1 DM. CRVO patients with type 1 DM were nearly twice as likely to undergo subsequent PRP as compared with patients with type 2 DM (78.6 vs 41.9%, P=0.01). However, visual outcomes between type 1 and type 2 DM patients with CRVO were not significantly different (initial visit, P=0.11; follow-up visit, P=0.36; final visit, P=0.68).
Discussion
DR and retinal vein occlusions are among the most common vascular disorders affecting the retina.29 There are many factors common to both these disorders: older age, hypertension, hyperlipidemia, and coagulation disorders. Both have similar treatment options including PRP and intravitreal injections of vascular endothelial growth factor inhibitors. Studies focusing on vitreous factors mediating these disorders have shown increased expression of similar proteins30, 31 and it is likely that both CRVO and DR share similar pathogenic mechanisms in relation to the final pathways resulting in retinal neovascularization.
Previously reported prevalence of CRVO overall ranges from 0.1%4 to 0.8%.5 In the current study, the prevalence of 0.5% is consistent with prior reports. Although patients with CRVO have a higher prevalence of DM than the general population,16, 21, 22, 23, 24 in the current study the prevalence of CRVO in DM patients was 0.5%, and was not statistically different than the prevalence of 0.4% observed in the nondiabetic patients. The similarity between these two groups may reflect the academic diabetes-specific tertiary care medical center referral setting in which this study was conducted. Older age has been associated with increasing prevalence of CRVO6, 7 as well as more ischemic CRVO in the general population.32 Potentially, diabetes itself does not increase the risk of developing CRVO.33 In this study, there was no statistical difference in the mean age of CRVO patients with DM as compared with nondiabetic patients with CRVO. However, patients with DM and CRVO were significantly older compared with the overall cohort of DM patients reviewed in the study, consistent with increasing age being a risk factor for CRVO. Consistent with previous studies,25, 34 we observed that DM patients with CRVO developed retinal neovascularization (particularly NVD) more frequently than nondiabetic patients with CRVO. Increased risk of neovascularization would be consistent with the generally increased state of retinal ischemia in the diabetic patient.
Interestingly, DM type had a substantial impact on CRVO anatomic outcomes. There was more than an eightfold increased risk of developing neovascularization and a twofold greater rate of receiving PRP in type 1 DM patients as compared with type 2 DM patients. This finding is consistent with the generally greater risk of neovascular complications observed in type 1 compared with type 2 DM patients in population- and clinic-based reports.35 Optic nerve head CVs were observed less than half as often in patients with type 1 DM and the presence of these CVs at baseline was associated with a more than threefold reduction in PRP. However, visual outcomes between type 1 and type 2 DM patients with CRVO were not significantly different, likely as a result of the effectiveness of current treatment regimens and limited number of events in specific subgroups.
The role of retinochoroidal CVs on the natural history of CRVO is unclear. Some studies report that the development of CVs may be associated with a better visual prognosis in patients with CRVO. However, Hayreh et al suggested that CVs formation may be associated with a delay in resolution of macular edema and worse prognosis.9 Recent data from the SCORE study may indicate that the development of venous collaterals does not demonstrate an independent association with visual acuity in eyes with CRVO.36 Although limited to only 15 instances of CV formation, our data did not demonstrate a significant difference in the incidence of collateral formation following CRVO in patients with or without DM.
Although the number of eyes identified in this study that developed CRVO was relatively small (104 eyes of 99 patients), a total of 19 648 patients (13 571 with DM) were evaluated over nearly a 5-year period. Thus, this study represents one of the largest reports of DM patients with CRVO (76 eyes) and one of the only studies to specifically report on diabetes type. Comparatively, the Central Vein Occlusion Study (CVOS), which established the guidelines for panretinal laser photocoagulation in patients with CRVO, enrolled only five patients with diabetes in each study arm.27 The Beaver Dam population-based study evaluated 4068 patients over a 15-year period and reported only 62 incident CRVO cases.6 The more recent SCORE study enrolled 62 diabetes CRVO patients.37 In none of these reports was diabetes type specifically evaluated.
The retrospective nature of the current study is a limitation; however, the drawbacks inherent in this study design are mitigated in this particular case by evaluation of the entire patient population over the period, use of standardized diabetes-specific electronic medical record with comprehensive diabetes and systemic history, standardized refraction and visual acuity measurement, study-certified data acquisition personnel, and uniform retinopathy grading. Fluorescein angiograms were only obtained in a subset of patients, which is a limitation of the study; however, the baseline demographic did not significantly differ in eyes that had an angiogram performed at baseline as compared with eyes that did not have an angiogram. Furthermore, the available angiograms were evaluated based on SCORE study criteria that was previously demonstrated to be a reproducible assessment of retinal vascular leakage severity and capillary nonperfusion.38
In conclusion, this study suggests not only that DM increases the likelihood of retinal neovascularization and the need for PRP in patients with CRVO, but also that diabetes type is an important indicator of key ocular outcomes. Patients with type 1 DM were at eightfold higher risk for developing neovascularization following CRVO as compared with patients with type 2 DM, and twice as likely to receive PRP and half as likely to develop optic nerve head CVs. These data suggest that following CRVO, patients with type 1 DM should be followed especially carefully for development of retinal complications and need for treatment. However, given current care approaches, visual acuity outcomes are similar following CRVO for type 1 DM, type 2 DM, and nondiabetic patients.

References
Scott IU, VanVeldhuisen PC, Oden NL, Ip M, Blodi BA, Jumper JM et al. SCORE Study Investigator Group. SCORE Study report 1: baseline associations between central retinal thickness and visual acuity in patients with retinal vein occlusion. Ophthalmology 2009; 116: 504–512.
Chen JC, Klein ML, Watzke RC, Handelman IL, Robertson JE . Natural course of perfused central retinal vein occlusion. Can J Ophthalmol 1995; 30: 21–24.
Klein R, Klein BE, Lee KE, Cruickshanks KJ, Gangnon RE . Changes in visual acuity in a population over a 15-year period: the Beaver Dam Eye Study. Am J Ophthalmol 2006; 142: 539–549.
Klein R, Klein BE, Moss SE, Meuer SM . The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 2000; 98: 133–141.
Rogers S, McIntosh RL, Cheung N, Wang JJ, Mitchell P, Kowalski JW et al. International Eye Disease Consortium. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe. Asia, and Australia. Ophthalmology 2010; 117: 313–319.
Klein R, Moss SE, Meuer SM, Klein BE . The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol 2008; 126: 513–518.
Shahsuvaryan ML, Melkonyan AK . Central retinal vein occlusion risk profile: a case-control study. Eur J Ophthalmol 2003; 13: 445–452.
Hayreh SS . Classification of central retinal vein occlusion. Ophthalmology 1983; 90: 458–474.
Hayreh SS, Podhajsky PA, Zimmerman MB . Natural history of visual outcome in central retinal vein occlusion. Ophthalmology 2011; 118: 119–133.
Hayreh SS . Retinal vein occlusion. Indian J Ophthalmol 1994; 42: 109–132.
Deramo VA, Cox TA, Syed AB, Lee PP, Fekrat S . Vision-related quality of life in people with central retinal vein occlusion using the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 2003; 121: 1297–1302.
David R, Zangwill L, Badarna M, Yassur Y . Epidemiology of retinal vein occlusion and its association with glaucoma and increased intraocular pressure. Ophthalmologica 1988; 197: 69–74.
O'Mahoney PR, Wong DT, Ray JG . Retinal vein occlusion and traditional risk factors for atherosclerosis. Arch Ophthalmol 2008; 126: 692–699.
Hayreh SS, Zimmerman B, McCarthy MJ, Podhajsky P . Systemic diseases associated with various types of retinal vein occlusion. Am J Ophthalmol 2001; 131: 61–77.
Turello M, Pasca S, Daminato R, Dello Russo P, Giacomello R, Venturelli U et al. Retinal vein occlusion: evaluation of ‘classic’ and ‘emerging’ risk factors and treatment. J Thromb Thrombolysis 2010; 29: 459–464.
The Eye Disease Case-Control Study Group. Risk factors for central retinal vein occlusion. Arch Ophthalmol 1996; 114: 545–554.
Elman MJ, Bhatt AK, Quinlan PM, Enger C . The risk for systemic vascular diseases and mortality in patients with central retinal vein occlusion. Ophthalmology 1990; 97: 1543–1548.
Appiah AP, Trempe CL . Risk factors associated with branch vs central retinal vein occlusion. Ann Ophthalmol 1989; 21: 153–155 157.
Saatci OA, Ferliel ST, Ferliel M, Kaynak S, Ergin MH . Pseudoexfoliation and glaucoma in eyes with retinal vein occlusion. Int Ophthalmol 1999; 23: 75–78.
Hayreh SS, Zimmerman MB, Beri M, Podhajsky P . Intraocular pressure abnormalities associated with central and hemicentral retinal vein occlusion. Ophthalmology 2004; 111: 133–141.
Shrestha RK, Shrestha JK, Koirala S, Shah DN . Association of systemic diseases with retinal vein occlusive disease. JNMA J Nepal Med Assoc 2006; 45: 244–248.
Koizumi H, Ferrara DC, Bruè C, Spaide RF . Central retinal vein occlusion case-control study. Am J Ophthalmol 2007; 144: 858–863.
Dodson PM, Kritzinger EE, Clough CG . Diabetes mellitus and retinal vein occlusion in patients of Asian, west Indian and white European origin. Eye (Lond) 1992; 6: 66–68.
Dodson PM, Clough CG, Downes SM, Kritzinger EE . Does type II diabetes predispose to retinal vein occlusion? Eur J Ophthalmol 1993; 3: 109–113.
Mansour AM, Walsh JB, Goldberger S, Henkind P . Role of diabetes mellitus on the natural history of central retinal vein occlusion. Ophthalmologica 1992; 204: 57–62.
Fong AC, Schatz H . Central retinal vein occlusion in young adults. Surv Ophthalmol 1992; 37: 393–417.
The Central Vein Occlusion Study Group. Natural history and clinical management of central retinal vein occlusion. Arch Ophthalmol 1997; 115: 486–491.
Bursell SE, Cavallerano JD, Cavallerano AA, Clermont AC, Birkmire-Peters D, Aiello LP et al. Joslin Vision Network Research Team. Stereo nonmydriatic digital-video color retinal imaging compared with Early Treatment Diabetic Retinopathy Study seven standard field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology 2001; 108: 572–585.
Laouri M, Chen E, Looman M, Gallagher M . The burden of disease of retinal vein occlusion: review of the literature. Eye (Lond) 2011; 25: 981–988.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 1994; 331: 1480–1487.
Yoshimura T, Sonoda KH, Sugahara M, Mochizuki Y, Enaida H, Oshima Y et al. Comprehensive analysis of inflammatory immune mediators in vitreoretinal diseases. PLoS One 2009; 4: e8158.
Glacet-Bernard A, Coscas G, Chabanel A, Zourdani A, Lelong F, Samama MM . Prognostic factors for retinal vein occlusion: prospective study of 175 cases. Ophthalmology 1996; 103: 551–560.
Luntz MH, Schenker HI . Retinal vascular accidents in glaucoma and ocular hypertension. Surv Ophthalmol 1980; 25: 163–167.
Funderburk RL, Feinberg EB . Diabetes as a risk factor for retinal neovascularization in retinal vein occlusion. Ann Ophthalmol 1989; 21: 65–66.
Klein R, Klein BE, Moss SE . Epidemiology of proliferative diabetic retinopathy. Diabetes Care 1992; 15: 1875–1891.
Weinberg DV, Wahle AE, Ip MS, Scott IU, Vanveldhuisen PC, Blodi BA . SCORE study report 12: development of venous collaterals in the SCORE study. Retina 2013; 33 (2): 287–295.
Scott IU, Vanveldhuisen PC, Oden NL, Ip MS, Domalpally A, Doft BH et al. SCORE Study Investigator Group. Baseline characteristics and response to treatment of participants with hemiretinal compared with branch retinal or central retinal vein occlusion in the Standard Care vs COrticosteroid for REtinal Vein Occlusion (SCORE) Study: SCORE Study Report 14. Arch Ophthalmol 2012; 130 (12): 1517–1524.
Blodi BA, Domalpally A, Scott IU, Ip MS, Oden NL, Elledge J et al. SCORE Study Research Group. Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) Study System for Evaluation of Stereoscopic Color Fundus Photographs and Fluorescein Angiograms. SCORE Study Report 9. Arch Ophthalmol 2010; 128: 1140–1145.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Santiago, J., Walia, S., Sun, J. et al. Influence of diabetes and diabetes type on anatomic and visual outcomes following central rein vein occlusion. Eye 28, 259–268 (2014). https://doi.org/10.1038/eye.2014.1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.1
Keywords
This article is cited by
-
Baseline clinical features predict visual outcome in young patients with central retinal vein occlusion
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)