Abstract
Purpose
The purpose of this study is to evaluate the efficacy of preoperative intravitreal bevacizumab (IVB) for improving outcomes in vitrectomy for diabetic retinopathy-related non-clearing vitreous haemorrhage and/or tractional retinal detachment.
Methods
Medical record from patients undergoing vitrectomy for proliferative diabetic retinopathy (PDR) were retrospectively analysed (2003–2011). From 2007, IVB (1.25 mg 2–4 days before operating) was used on all eyes. Eyes receiving IVB were compared with those that did not receive IVB. Intraoperative complications, reoperation rates, and final visual acuity were the core outcome measures.
Results
Data were analysed for 88 patients (101 eyes). In all, 41 (41%) patients had received IVB, whereas 60 (59%) patients had not. Significant intraoperative haemorrhage occurred in six eyes (10%) in the non-IVB group and in one (2.4%) IVB eyes (P=0.24). Silicon oil was used in 29 (48%) non-IVB eyes and in 11 (27%) IVB eyes (P=0.03). The non-IVB eyes underwent significantly more vitreoretinal reoperations (P=0.01) and were significantly more likely to lose two or more lines of vision at the final follow-up (P=0.03). The numbers needed to treat (NNT) blindness (<3/60) was four for non-IVB eyes and two for the IVB group.
Conclusions
IVB reduces surgical complications, the use of silicon oil, and the need for further retinal surgery. The NNT to restore useful vision (≥3/60) to a blind eye were significantly lower in the IVB group. Vitreoretinal surgery for the complications of PDR is effective in an East African context, and IVB should be considered a valuable adjunct.
Similar content being viewed by others
Introduction
The WHO estimates that there are 12 million type 2 diabetics in sub-Saharan Africa and that the prevalence of this condition will double in the region within 20 years. This will result in a corresponding increase in the burden of diabetes-associated eye disease.1 Tractional retinal detachment (TRD) and non-clearing vitreous haemorrhage (VH) are two potentially blinding complications associated with diabetic eye disease. Ideally, primary preventative measures or early laser treatment would reduce the incidence of advanced diabetic eye disease, making surgery unnecessary. However, access to primary prevention and ophthalmic care in developing nations is limited; typically, patients present late with advanced disease.2
In recent years, several studies have assessed the efficacy of preoperative intravitreal bevacizumab (IVB) on surgical outcomes for diabetic vitrectomy. Bevacizumab, a vascular endothelial growth factor antibody, induces regression of the vascular component of the fibrovascular membranes (FVMs).3, 4, 5 This facilitates segmentation and delamination of membranes, as they are less adhesive to the underlying retina and are more readily separated.6 IVB has also been shown to decrease intraoperative haemorrhage.7, 8 This study investigated the outcomes of diabetic vitrectomy surgery in the Kilimanjaro Christian Medical Centre Eye Department in Tanzania, East Africa, before and after the introduction of previtrectomy IVB use. It is the first to examine the effectiveness of preoperative IVB in the region.
Patients and methods
This is a retrospective, comparative, and consecutive record review conducted in the Kilimanjaro Christian Medical Centre, Moshi, Tanzania. The medical records of all diabetic patients who underwent vitreoretinal surgery between May 2003 and May 2011 were identified from theatre records and were reviewed. Data were gathered solely from hand-written records. Only eyes that underwent vitreoretinal surgery as a consequence of proliferative diabetic retinopathy (PDR) were included in the study. Indication for surgery included non-clearing VH, TRD threatening or detaching the macula, and combined TRD and rhegmatogenous retinal detachment (RRD).
All of the included eyes were operated upon by the same surgeon and had a minimum follow-up of 60 days. Eyes that had previously undergone vitreoretinal surgery, except laser surgery, or intraocular surgery of any type within the prior 4 months were excluded.
In October 2007, it became a standard practice for all eyes undergoing diabetic vitrectomy to receive 1.25 mg of IVB 2–4 days before surgery. This dosing regimen had been noted to effectively reduce neovascularization by Avery et al.3 The untreated control group included all those patients who received surgery for diabetic eye disease before the regular use of IVB. Patients did not universally receive preoperative panretinal photocoagulation (PRP). PRP was performed if there was no VH obscuring the view or no urgent indication for surgery, such as a combined tractional/rhegmatogenous detachment or fresh tractional detachment of the macula.
The following baseline data were recorded from medical records: patient demographics, type and duration of diabetes, HbA1c, blood pressure, intraocular pressure, preoperative laser, and best-corrected visual acuity (BCVA) and primary indication for surgery (Table 1). Postoperatively, the following data were recorded: intraoperative complications, tamponade use, postoperative complications, vitreoretinal reoperations, and BCVA (Table 2). Primary outcomes of this study were BCVA at 6 months, incidence of intra- and postoperative complications, incidence of additional vitreoretinal surgery (including the removal of silicon oil), and the restoration of useful vision (≥3/60) to previously blind eyes.
Surgeries were performed by one surgeon using a 20-gauge, 3-port pars plana vitrectomy (PPV) by using the Alcon Accurus Surgical System (Alcon, Hemel Hempstead, UK). In all cases, the surgical approach was the clearance of core vitreous and blood, identification and incision of the posterior hyaloid face followed by removal with delamination, or segmentation, where not possible, of preretinal FVMs using scissors and the vitrectomy cutter as needed. The surgical endpoint was the relief of traction on the macula and areas of TRD and a clear vitreous cavity. Endodiathermy was used to achieve haemostasis as required. Low systemic blood pressures and high intraocular pressures were avoided ensuring that intraocular perfusion was not compromised. A careful internal search was performed to locate retinal breaks, which were then treated with the indirect laser. Cryotherapy was rarely used, and only in situations where blood on the retinal surface around a break made the uptake of laser impossible. All retinal breaks were recorded in the operation notes and PRP was completed with the indirect laser. Significant haemorrhage were recorded and defined as bleeds that obscured tears, hindered the dissection of membranes, and prevented the application of laser. The use of intraocular retinal tamponade was determined by the final appearance and status of the retina using the following criteria.
Criteria for silicone oil:
-
Significant intraoperative haemorrhage obscuring tears and preventing the application of laser.
-
Large retinal breaks with increased potential for postoperative proliferative vitreoretinopathy.
-
Incomplete removal of FVM in the vicinity of retinal tears (often a result of significant haemorrhage).
-
Extensive preoperative TRD or combined rhegmatogenous TRD. In these cases, the underlying retinal pigment epithelium was often atrophic and the neurosensory retina oedematous. Uptake of laser in these cases was poor. Silicone oil gave the option of postoperatively applied laser top up at a later date.
Criteria for gas:
-
Retinal tears in eyes with superior breaks or entry site breaks.
-
Membranes completely removed.
-
Laser easily applied to breaks.
-
Previous laser resulting in adequate pre-existing retinal scarring in the retina around a tear with localised subretinal fluid only.
-
Inferior breaks fulfilling all the above criteria received gas rather than oil.
The bevacizumab group were compared with the non-bevacizumab group using Minitab 16 (Minitab Ltd, Coventry, UK) for statistical analysis. The numbers needed to treat (NNT) was calculated by dividing the initially blind eyes (<3/60), as defined by the WHO, by the number of initially blind eyes that regained sight postoperatively (≥3/60). Case characteristics were calculated using descriptive statistics, including mean and SD. Categorical variables were compared using Pearson’s χ2-test, wherein all values within the table were >5. If any values were <5, then Fisher’s exact test was employed. Means were compared using Student’s t-test for unequal variance. P-values of <0.05 were considered statistically significant. Snellen chart measurements were converted to logarithmic minimum angle of resolution, LogMAR, for statistical analysis. Acuity values were assigned to counting fingers, hand motion, and no perception of light as recommended by Schulze-Bonsel et al.9
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. A board review was not required by the institution, as this was considered a retrospective clinical audit.
Results
For the 8 years covered by the study, 120 records of PPV performed on diabetic patients were retrieved. One hundred and one eyes met the inclusion criteria, 60 had not received IVB, and 41 had received IVB. The most common reason for exclusion was because of <60 days follow-up (17 eyes). One eye was excluded because of recent intraocular surgery. The average follow-up in the non-IVB group was 403 days with a range of 67–1864 days. The IVB group’s average was 345 days with a range of 62–1269 days. Baseline demographics data are shown in Table 1.
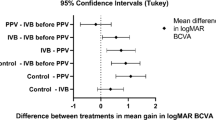
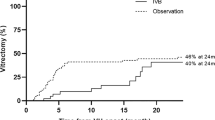
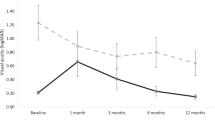
Intraoperative complications were more common in the non-IVB group (Table 2). Significant intraoperative haemorrhage occurred in six eyes (10%) in the non-IVB group and in one (2%) IVB eyes (P=0.24). Iatrogenic breaks occurred in 23 non-IVB eyes (38%) and in 11 (27%) IVB eyes (P=0.24). Significantly more silicon oil was injected into non-IVB eyes, ie, 29 (48%) eyes in the non-IVB group compared with 11 (27%) eyes in the IVB group (P=0.03). The non-IVB eyes underwent significantly more vitreoretinal reoperations (P=0.01) and were significantly more likely to lose two or more lines of vision at the final follow-up (P=0.03). The NNT, a blind eye, (<3/60) was four for non-IVB eyes and two for those who received IVB. The 95% confidence interval for NNT is significant (1.7–23.6). No preoperative injection-related complications were recorded. No IVB eye developed obvious RRD between the IVB injection and PPV. No clinically significant increase in TRD was noted in the short interval between injection and surgery.
Discussion
This study examined outcomes from a cohort of patients who presented with advanced diabetic eye disease. Two groups were compared: the first group had not received preoperative IVB before undergoing vitrectomy for complications of PDR and the second group had received IVB. Injections were given at 2–4 days before operating; this is now considered to be the optimum time to give IVB, as it provides time for vascular regression, but is not enough to allow the development or progression of TRD.7
The IVB group had a reduced rate of significant intraoperative haemorrhages, six in the non-IVB group and one in the IVB group (P=0.24). This non-significant finding mirrors the reductions in intraoperative bleeding reported in other studies.7, 10 Patients in Africa commonly present late with advanced disease.2 Africans have also been noted to form more extensive FVMs than those found in Caucasian populations.11 The combination of late presentation and extensive FVMs makes this patient group challenging to operate upon. Subjectively, the surgeon reported that IVB greatly reduced the extent of intraoperative bleeding, enabling clear visualization of extensive membranes. Surgery was consequently less technically demanding due to the decrease in vascularity of membranes and easier separation of the posterior hyaloid face from the underlying retina. Unfortunately, operative times and the use of diathermy were not consistently recorded for this period; hence, these cannot be demonstrated numerically.
The increased use of silicone oil in the non-IVB group (P=0.03) reflects the surgical difficulties encountered by surgeons before the introduction on IVB. Before IVB, dissection of FVMs off the surface of an unlasered detached retina was difficult and was usually incomplete. Furthermore, the increased frequency of haemorrhage in the non-IVB group may have led to more oil being used to facilitate laser at a later date. The number of surgeries using silicone oil tamponade was greater than the number of iatrogenic breaks in this group. This was partly due to the higher number of combined tractional and rhegmatogenous detachments in this group. Vitreoretinal reoperation rates in the IVB group were significantly lower than that in the non-IVB group (P=0.01). The majority of these reoperations were undertaken to remove silicon oil, which had been used during the initial operation because of extensive haemorrhage, iatrogenic breaks, and poor retinal flattening. If silicon oil removal is not considered to be a reoperation, then there is no statistical difference in the vitreoretinal reoperation rates between the two groups.
Silicon oil was used frequently in both groups because of the challenging nature of the surgery; patients had advanced disease and, commonly, had not received adequate laser preoperatively. Inferior retinal breaks occurred frequently and would generally receive a silicon oil tamponade. Furthermore, patients regularly came from far-off places to receive surgery, and it was felt that SF6/C3F8 would be unsuitable for patients who would fly back home or who would travel for days by road.
There was no statistically significant difference between the groups for postoperative BCVA (P=0.16). However, significantly less people lost two or more lines of vision postoperatively in the IVB group (P=0.04) and a greater proportion of blind eyes (<3/60) regained vision (≥3/60), 60% IVB vs 28% non-IVB. One in four operations in the non-IVB group restored vision to a blind eye. This reduced to one in two operations in the IVB group. This means a gain of vision in one extra eye for every four patients when IVB was administered.
Similar studies conducted in developed nations have reported better visual outcomes. The mean visual acuity change at 6 months follow-up found by di Lauro et al7 was 0.4 LogMAR units in the non-IVB group and 0.62 in the intervention group. The average LogMAR unit improvement in this study was 0.17 for the non-IVB group and 0.39 for the IVB group. The late presentation of patients, the difficulty of operating on African retinas, and the limited follow-up could account for the poorer visual outcomes found by this study. Cataract is a frequent sequel of vitrectomy and many patients had not yet had cataract surgery at their final review. There was no record of adverse reactions, nor was there any record of worsened TRD resulting from IVB.
Over 80% of those operated upon were male. Currently, the ratio of female to male patients with diabetes, who are registered in diabetic clinics in the Kilimanjaro region, is 1.6 : 1. This difference reflects a higher incidence of advanced diabetic eye disease in male diabetics and gender inequalities with regard to access to healthcare in the region.12, 13 Many of the patients came from other countries in sub-Saharan Africa, from as far afield as Ghana and Zimbabwe. Male patients from these countries were more likely to be able to access the resources to fly to Tanzania. Patients in this study presented at a similar mean age to their counterparts in the United Kingdom, but they reported to have had diabetes for a shorter duration before undergoing surgery. Type 2 diabetics underwent surgery on an average of 4.7 years earlier and type 1 diabetics on an average of 7.4 years earlier.11 This could result from the late diagnosis of the condition and/or poor diabetic control, resulting in earlier onset of diabetic retinopathy.
This retrospective study has several limitations. First, the use of diathermy and the operation duration was not regularly recorded. This information would have provided insight into the effect of IVB on surgical procedure and operating time. Second, operations were conducted across an 8-year period. It could be argued that surgical outcomes will improve during the 8-year period, as greater surgical experience is gained, favouring the IVB group. The surgeon, however, had nearly 10 years of experience before 2003 and had spent 3 years dealing with difficult African proliferative retinopathy surgery before the start of the study. The learning curve is therefore unlikely to have influenced the surgical outcomes. Lastly, because of the inherent difficulty with patient follow-up in sub-Saharan Africa, it was not possible to obtain BCVA for all patients at 6 months. Consequently, the closest recorded BCVA to 6 months was used.
This study has several strengths. It is the first to examine the efficacy of preoperative IVB in an African population with advanced diabetic retinopathy. The examined population was relatively large and homogenous (Table 1). The surgery was conducted by a single surgeon with years of prior experience of operating in sub-Saharan Africa. All operations were carried out using standardized equipment and surgical technique.
In conclusion, IVB facilitates surgery in an exclusively Black, African population by limiting intraoperative bleeding and reducing posterior hyaloid adherence to the underlying retina. This expedites FVM dissection, improves laser uptake, and decreases silicon oil use. Reduced use of silicon oil results in a significantly fall in reoperation rates. Ultimately, visual outcomes were superior when IVB was used in this population, with the NNT blind eyes (<3/60) falling from four to two. For every four operations carried out on blind eyes, one extra eye will regain vision if IVB was used.

References
International Diabetes Federation. Diabetes Atlas 5th edn. International Diabetes Federation: Brussels, 2012.
Lewallen S, Courtright P . Blindness in Africa: present situation and future needs. Br J Ophthalmol 2001; 85: 897–903.
Avery R, Pearlman J, Pieramici D, Rabena MD, Castellarin AA, Nasir MA et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology 2006; 113: 1695–1705.
Mason JI, Nixon P, White M . Intravitreal injection of bevacizumab (Avastin) as adjunctive treatment of proliferative diabetic retinopathy. Ophthalmology 2006; 142: 685–688.
Zhao L-Q, Zhu H, Zhao P, Hu Y . A systematic review and meta-analysis of clinical outcomes of vitrectomy with or without intravitreal bevacizumab pretreatment for severe diabetic retinopathy. Br J Ophthalmol 2011; 95: 1216–1222.
Yeh P, Yang C, Lin Y, Chen MS, Yang CH . Bevacizumab pretreatment in vitrectomy with silicone oil for severe diabetic retinopathy. Retina 2009; 29: 768–774.
di Lauro R, De Ruggiero P, di Lauro R, di Lauro MT, Romano MR . Intravitreal bevacizumab for surgical treatment of severe proliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 2010; 248: 785–791.
Pokroy R, Desai UR, Du E, Li Y, Edwards P . Bevacizumab prior to vitrectomy for diabetic traction retinal detachment. Eye 2011; 25: 989–997.
Schulze-Bonsel K, Feltgen F, Burau H, Hansen L, Bach M . Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg Visual Acuity Test. Invest Ophthalmol Vis Sci 2006; 47: 1236–1240.
da R, Lucena D, Ribeiro JA, Costa RA, Barbosa JC, Scott IU, de Figueiredo-Pontes LL et al. Intraoperative bleeding during vitrectomy for diabetic tractional retinal detachment with versus without preoperative intravitreal bevacizumab (IBeTra Study). Br J Ophthalmol 2009; 93: 688–691.
Yorston D, Wickham L, Benson S, Bunce C, Sheard R, Charteris D . Predictive clinical features and outcomes of vitrectomy for proliferative dic retinopathy. Br J Ophthalmol 2008; 92: 365–368.
Zhang X, Saaddine JB, Chou CF, Cotch MF, Cheng YJ, Geiss LS et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA 2010; 304: 649–656.
Lewallen S, Mousa A, Bassett K, Courtright P . Cataract surgical coverage remains lower in women. Br J Ophthalmol 2009; 93: 295–298.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Guthrie, G., Hall, A., Dhalla, K. et al. Bevacizumab as an adjunct to vitreoretinal surgery for diabetic retinopathy in East Africa. Eye 27, 1263–1268 (2013). https://doi.org/10.1038/eye.2013.182
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.182
Keywords
This article is cited by
-
Beneficial visual outcome of vitrectomy and delamination surgery for tractional complications of diabetic retinopathy in a cohort of black patients
Eye (2019)
-
Sickle cell retinopathy. A focused review
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
Black patients sustain vision loss while White and South Asian patients gain vision following delamination or segmentation surgery for tractional complications associated with proliferative diabetic retinopathy
Eye (2017)