Abstract
Purpose
To evaluate short- and long-term success rates on isolated subtotal Muller resection in over 300 cases of ptosis over a 10-year period.
Methods
Clinical records were retrospectively evaluated for aetiology and severity of ptosis, levator function, response to phenylephrine, pre- and postoperative margin reflex distance of the upper lid (MRD1), postoperative lid contour and symmetry, complications and follow-up duration. Main outcome measures: change in MRD1 and eyelid contour. Surgical success: postoperative MRD1 ≥2 and ≤4.5 mm, symmetry to within 1.0 mm and satisfactory contour. All patients were also sent patient satisfaction questionnaires, and invited to attend for a longer-term assessment of their surgical outcome.
Results
In total, 92 and 95% of 309 eyelids met all three criteria for success after an average follow-up of 4 and 47 months, respectively. Mean improvement in MRD1 was 2.56 mm. In all, 97% had postoperative MRD1 of ≥2 and ≤4.5 mm and over 99% had an excellent contour. Altogether, 95 and 89% were within 1.0 and 0.5 mm symmetry of the fellow eye, respectively. In total, 51% of eyelids continued to rise, 17% maintained the same initial postoperative height, and 32% dropped by 1 mm or less. In all, 92% felt that their initial postoperative eyelid height had been maintained. Only 2% required repeat surgery and minor complications occurred in 4%.
Conclusions
Isolated subtotal Muller’s resection is safe and effective for the repair of the majority of ptosis with moderate-to-good levator function. It results in a more predictable height, which is maintained over time, less frequent contour abnormalities, and lower re-operation rates compared with anterior levator advancement.
Similar content being viewed by others
Introduction
Conventional ptosis surgery in the presence of a functioning levator muscle is predominately on the aponeurosis of the levator complex via an anterior approach. Although reported success rates range from 57 to 95%,1, 2, 3, 4 there are some concerns regarding unpredictability of lid height and perhaps more so, the postoperative contour with this procedure.
Posterior approach blepharoptosis surgery, via the transconjunctival route, was probably the first method of surgery used to shorten the levator palpebrae superioris muscle.5, 6, 7 Posterior approach surgery was further popularised utilising Muller’s muscle and tarsoconjunctival resection.8 Resection of Muller’s muscle together with overlying conjunctiva (MMCR) was first reported by Putterman, where he dissected Muller’s blindly off its bed on the aponeurosis with the aid of a special clamp.9 This technique has been shown to be safe and effective with 90% of eyelids achieving within 1.5 mm symmetry of the fellow eye.10 However, because of the blind capture of tissues with the clamp, the amount of Muller’s muscle that is resected is variable and limited, and hence it has been predominantly popularised for patients with good levator function and a positive response to the phenylephrine test. Modifications have since been described in order to better address Muller’s muscle, including our open-sky technique, which engages Muller’s muscle in a more direct approach,11 and more recently, an isolated Muller resection to avoid sacrificing healthy conjunctiva.12 We have also recently demonstrated its efficacy in patients with a negative phenylephrine response.13 We herein report our results on isolated subtotal Muller resection in over 300 cases of both phenylephrine-positive and -negative ptosis repair over a 10-year period, including long-term data on 83 eyelids.
Materials and methods
This was a retrospective audit in which the notes of all patients undergoing surgical repair for ptosis by posterior approach Muller resection between December 2000 and June 2011 at Stoke Mandeville and Wycombe Hospitals, Buckinghamshire, UK, were reviewed.
The following data were collected: patient age, sex, the aetiology of ptosis, side of surgery, levator function, margin reflex distance of the upper lid (MRD1), response to phenylephrine 2.5%, and the presence of an occult ptosis. Both phenylephrine test-positive and -negative patients were included. Ptosis was recorded as mild, moderate, and severe if MRD1 was ≥2, 1–2, and <1 mm, respectively. Levator function was considered good if >10 mm and moderate if between 5 and 10 mm.
Intra-operatively, the grade of surgeon, which tissues were resected (eg, conjunctiva, Muller, and/or any tarsus), and any simultaneous procedures (blepharoplasty) were recorded. In bilateral cases, the worse eyelid was always operated on first. Postoperative data collected included final MRD1, symmetry and contour at discharge, follow-up duration, and any complications. The need for further surgery was also noted. The main outcome measures were change in MRD1 and eyelid contour, which were recorded in each case. Surgical success was defined as a postoperative MRD1 of ≥2 and ≤4.5 mm, symmetry to within 1.0 mm of the fellow eye, and a satisfactory eyelid contour. Cases with poor levator function (4 mm or less), a history of previous ptosis surgery, inadequate data, including postoperative follow-up of <1 month, and those who underwent conjunctival-Muller resection or anterior approach surgery were excluded. Our surgical technique and the phenylephrine test has been described in detail elsewhere.12, 13
All patients were sent patient satisfaction questionnaires regarding their perception of the long-term outcome of their surgery, and their patient experience. They were also invited to attend for photography and a final longer-term postoperative assessment. At this visit, patients were asked to grade their satisfaction with their postoperative outcome at initial discharge and present time, and whether they felt there had been any change in their outcome over time. Informed consent was obtained according to regional hospital protocol. All data analyses were completed using SPSS version 16 (SPSS, Inc., Chicago, IL, USA) statistical software.
Results
Data were collected on 584 eyelids in 510 patients undergoing posterior approach Muller resection over the study period. A total of 309 eyes in 232 patients met the inclusion criteria, with an average follow-up of 4 months (range 1–32). In all, 55% underwent simultaneous bilateral surgery. The aetiology was involutional in 70%, contact-lens related in 15%, post intra-ocular surgery in 5%, spastic (aberrant regeneration ptosis following facial palsy) in 4%, congenital in 3%, secondary to lymphoedema in 2%, and neurogenic or anopthalmic in 1%. The mean levator function was 12.90 mm (range 6–17 mm). Ptosis was classified as severe in 41%, moderate in 28%, and mild in 31%. In total, 88% had a positive response to phenylephrine.
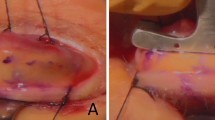
The majority (81%) of all surgery was performed by the senior author (RK) with the remainder by her fellow or associate specialist trained in the above technique, and often under supervision. The mean preoperative MRD1 was 0.98 mm (range −2 to 3 mm). The mean postoperative MRD1 was 3.55 mm (range 3–5 mm), giving a mean improvement in MRD1 (see Figure 1) of 2.56 mm (range 0.5–6 mm). Blepharoplasty was simultaneously performed in 26% of procedures. Nineteen eyelids (6%) required intra-operative augmentation of a subtotal Muller resection by either a small tarsectomy or posterior approach levator resection and all but one achieved a very good postoperative outcome. A significantly greater number of phenylephrine-negative eyelids required such intra-operative augmentation (27 compared with only 3% of phenylephrine-positive eyelids).
Overall, 92% of patients met all three of our criteria for success. In all, 97% had postoperative MRD of ≥2 and ≤4.5 mm. There was no significant correlation between severity of ptosis and postoperative height (99% of mild ptosis and 96% of severe ptosis achieving target height). Similarly, 94% of the phenylephrine-positive group vs 88% of the phenylephrine-negative group had a successful postoperative height. Nine eyelids (3%) were overcorrected with a postoperative MRD1 of 5, however, none required further surgery. There was a trend towards the degree of levator function being a predictor of increased risk of overcorrection, with all those overcorrected having a levator function of 11 mm or more.
Over 99% had an excellent contour postoperatively, with a persistent medial droop in only two eyelids—one had redo surgery with a good postoperative result. No patients had a peak postoperatively.
In total, 95% were within 1.0 mm symmetry of the fellow eye, with 89% being within 0.5 mm of symmetry. In all, 5% had a final MRD1 between 1 and 3 mm of the fellow eye—the vast majority of these were due to an increase in occult ptosis in the fellow eye postoperatively, for which the patients declined surgery.
Six eyelids (1.9%) had repeat surgery—one for a medial droop and five for asymmetry. If the patients with occult ptosis causing asymmetry were excluded from the failures, our overall success rates increased to 95%.
There was a greater degree of final symmetry between simultaneous bilateral compared with unilateral or sequential surgery, with 100% of bilateral cases reaching within 1 mm of symmetry, and 94% achieving within 0.5 mm of symmetry, compared with 89 and 83% for unilateral cases, respectively.
In all, 4% of eyelids developed complications: five corneal abrasions (pattern consistent with peroperative surface drying rather than problems with the conjunctival sutures), two suture abscesses, four prolonged postoperative pain, and one blood cyst.
Long-term data
Patient satisfaction questionnaires were returned on 191 eyelids with an average postoperative duration of 40 months (range 1–132 months). In all, 97% of cases remained happy with their surgery and felt that it had been a success. The subjective improvement was categorised as significant in 82%, moderate in 15%, and minimal or none in 3%. In total, 94% were happy with their eyelid shape and 87% were happy with the final symmetry.
Additional data were collected on 83 eyelids in 51 patients who attended for a longer-term assessment after an average follow-up of 47 months (range 15–138). Overall, 95% of patients met all three of our criteria for success (96% had a final postoperative MRD of ≥2 and ≤4.5 mm and 99% had an excellent long-term contour and symmetry postoperatively). Two eyelids (2.4%) had repeat surgery, both for an undercorrection, and achieved excellent final height and postoperative outcome.
Since discharge, 51% of eyelids had continued to rise (by an average of 0.9 mm), 17% maintained the same initial postoperative height and 32% dropped by 1 mm or less (average by 0.7 mm). No eyelids dropped by >1 mm. There was no significant association between the change in eyelid height over time and aetiology of ptosis, levator function and response to phenylephrine. A greater number of patients who had simultaneous blepharoplasty had continued increase in eyelid height postoperatively compared with those who had Muller resection alone (70 vs 40%).
Overall, 96% of patients felt that their final eyelid height was 80% or more of their target height—83% felt that they had achieved an ideal height, 11% felt they were within 90% of their target, and 2% felt they were within 80%. In all, 92% felt that their initial postoperative eyelid height had been maintained over time, whereas 4% felt that it had dropped, and 4% felt it had continued to rise.
Conclusion
Conventional ptosis surgery is based on the traditional theory that the aponeurosis is the main transmitter of contraction of the levator to the tarsus. Levator aponeurosis surgery was first advocated by Jones et al14 for the treatment of involutional ptosis, and since then, reported success rates in the literature have varied, ranging from 57 to over 90%.1, 2, 3, 4 In a large series of anterior levator advancement, McCulley et al2 found that 77% of eyelids were symmetrical to within 1 mm of the fellow eye, with 8.8% of eyelids requiring re-operation. More recently, a BOPSS national survey reported that only 57% of patients undergoing primary aponeurotic surgery in the United Kingdom had a successful outcome with 65% of patients completely satisfied with the results.1 There is only one comparative study of anterior levator advancement vs MMCR for the correction of involutional ptosis, which reported a 22% lower revision rate for MMCR vs anterior levator advancement and a statistically better cosmetic outcome.15 This is consistent with other reports of Muller’s muscle resection, which suggest a generally higher success rate (85–98%) compared with that for anterior approach levator advancement.10, 11, 12, 16
To our knowledge, the current series is the largest to date assessing the success of isolated Muller resection. In this study of over 300 cases, we have shown that our previously described surgical technique consistently achieves a high success rate, with 95–99% of eyelids achieving any one of target height, symmetry, or contour, and 92 and 95% achieving all three over short-term and long-term follow-up, respectively. We have also demonstrated that the majority of patients maintain or have continued increase in eyelid height with this surgical approach, and have shown an extremely high subjective patient satisfaction rate, with 97% of almost 200 cases remaining happy with their surgery after an average follow-up of 40 months, and 92% feeling that their initial postoperative eyelid height had been maintained over time.
The anatomical reasons for the success of MMCR have been a matter of debate for some time. Several mechanisms have been suggested for the success of this technique, which include vertical posterior lamellar shortening and secondary contractile cicatrisation of the wound. However, as we have previously postulated, it has been increasingly felt that the success of the procedure is due to advancement of the levator muscle itself, along with the aponeurosis. The mechanism by which Muller’s muscle resection alleviates ptosis would therefore be by transmitting the contraction force of the levator muscle directly to the tarsal plate instead of through its aponeurotic attachment. By passing the sutures through the stump of Muller’s muscle (which originates at the distal edge of the inferior surface of the levator muscle) and then through the tarsus, one is in effect advancing the levator and attaching it to the tarsal plate and skin crease, irrespective of any potential aponeurosis defects, high or low.
This theory is further supported by our high success rate (88%) of the procedure in phenylephrine-negative patients. However, we feel that the phenylephrine test is still an integral part of the preoperative assessment for Muller resection. We believe it serves as a predictor of the viability of the adrenergic receptors of Muller’s muscle, giving a negative response in situations where there is gross fatty degeneration of Muller’s muscle and its neuroreceptors. In these cases, as we have shown, while not precluding patients achieving a high success rate, as resection of even a degenerate Muller’s muscle will advance the levator with excellent results, a negative result can alert the surgeon to an increased probability of requiring intra-operative augmentation of surgery. This is only possible through an open-sky technique where the surgery can be easily converted to a posterior levator resection. In addition, the phenylephrine test is invaluable in unmasking a coexisting occult ptosis and is very useful in demonstrating the outcome of surgery to the patient.
We have also noted that in contrast to anterior aponeurosis surgery, when initial eyelid height tends to drop over time,3 with Muller resection, the eyelid height can often continue to rise postoperatively, for up to 6 months or longer, as found in 51% of our cases. This can be explained by the highly vasculature nature of the scar that forms in Muller surgery, resulting in a stronger wound. Although 32% of eyelids were found to have dropped, the degree of lowering was minimal, measuring 1 mm or less in all, and subjectively noticed by only 4% of patients. In all, 92% felt that their initial postoperative eyelid height had been maintained over time. Therefore, it would seem that if the desired postoperative height is achieved after surgery, it is very likely to be maintained over the long term. This would also explain the very low revision rates we have consistently demonstrated, with only 2.4% over an average of almost 4 years undergoing further corrective surgery in this study. This contrasts to anterior approach surgery, with re-operation rates as high as 8.7% over 1 year.2
Our open-sky technique allows intra- as well as postoperative adjustment, thus offering several advantages over anterior aponeurosis advancement surgery. One of the main criticisms of anterior levator surgery is its unpredictability, particularly as there is no opportunity for postoperative adjustment unless adjustable sutures are used. In contrast, the use of ‘pull-out’ silk sutures in Muller resection allows some postoperative manipulation of lid height through their timely removal. As these sutures are not absorbed, stimulate minimal inflammatory reaction and can be left in place for up to 3 weeks to maximise the effect, the eyelid height is far more predictable for any given degree of ptosis. Although there is similar opportunity for intra-operative adjustment of lid height, this is much simpler to perform in Muller resection compared with aponeurosis advancement, with simple selective tightening or loosening of sutures. We have rarely found the need to replace sutures intra-operatively through the tarsus, making this a much more predictable and quicker procedure. Furthermore, if adequate height is not achieved, this open-sky approach can easily be augmented with a small tarsectomy or conversion to posterior approach levator resection through the same incision, although this has rarely been necessary in our clinical experience, occurring in only 6% of over 300 cases.
In anterior approach surgery, a persistent medial droop is a problem observed by many, possibly due to thinner and structurally less dynamic medial attachments of the levator.17 In contrast, we had only two cases of this occurring in our large series. A good contour is more consistently achieved than from the anterior approach as the force of the levator muscle is passed to the upper border of the tarsal plate, rather than lower down. Care is also required to exclude high apo-defects to avoid surgical failure with levator advancement. Resection of Muller’s muscle, however, advances the levator muscle toward the tarsal plate through shortening Muller muscle, making even a high aponeurosis defect irrelevant. The nine patients with congenital ptosis in this paper had good levator function, with a minimum of 11 mm, and achieved excellent results. Only one needed peroperative augmentation with a posterior levator resection. These cases were most likely to be of a high aponeurosis type of congenital ptosis. The role of surgery on Muller’s muscle to correct congenital dystrophic ptosis is less clear.
In contrast to other types of posterior approach surgery, our technique transmits the pull of Muller’s muscle through orbicularis muscle and skin, resulting in a more predictable skin crease as well as a degree of lash eversion.
Reported disadvantages of Muller resection have included a limited degree of lid elevation. However, we have clearly demonstrated in this large series that even in severe cases of ptosis, excellent height is achieved—96% of eyelids with MRD <1 mm achieved their target lid height, and we found no significant relationship between our success rates and ptosis severity. Furthermore, <2% of our cases required redo surgery (mostly for asymmetry), despite 41% of our series having a severe ptosis. This contrasts very favourably with anterior approaches with reported success rates of 64% for similarly severe ptosis of MRD≤1 mm.18
In our isolated Muller resection, conjunctiva is also preserved, thus avoiding the theoretical possibility of compromising tear production. This may be of benefit to patients as they get older and may also extend the role of this technique in anophthalmic patients with ptosis, in whom fornix shallowing is a concern.
One potential disadvantage of posterior approach Muller’s muscle resection relates to wound closure and presence of suture material on the palpebral conjunctiva. Complications may arise from this, including keratopathy, suture granulomas, infection, and the need for suture removal. However, our rate of such complications was low, occurring in <4% of patients.
The potential of increased postoperative ptosis in the contralateral eyelid is well documented, explicable by Hering’s law of equal innervation. Some surgeons advocate that the contralateral eyelid should be corrected at the same time using the same technique to avoid an unpredictable outcome.19 This is supported by our results, which showed a greater degree of final symmetry between simultaneous bilateral compared with unilateral or sequential surgery. However, others have found an increased rate of complications, including asymmetry, in bilateral surgery.20 This remains an area of interest for oculoplastic surgeons and will be a topic studied well into the future. Ocular dominance has an undetermined, potentially significant role.
We acknowledge the limitations of this retrospective audit, including potential confounding factors, such as the presence of multiple surgeons in the study (although the vast majority, over 80%, were performed by a single surgeon) and the performance of additional procedures at the time of ptosis repair, which could theoretically affect final eyelid height. Nevertheless, our study evaluating over 300 cases, to the best of our knowledge the largest series of isolated subtotal Muller’s resections, demonstrates excellent success rates with this procedure. Its main advantages are that it allows both intra- and postoperative adjustment, thus giving a more predictable result with less frequent contour abnormalities and lower re-operation rates compared with anterior levator advancement. We believe that our open-sky technique addresses and resects the main terminal layers of levator, that is, the smooth muscle of Muller along with the thinner smooth muscle of the more posterior layer of the aponeurosis, 21 leaving the anterior fibrotic layer of the aponeurosis (the ‘white line’ ) intact (author’s histological study in progress). These two smooth layers have strong attachments to the upper and anterior tarsal surface, hence the strength of correction that can be achieved, as we have demonstrated, even in severe ptosis. We conclude that isolated subtotal resection of Muller’s muscle is a safe and effective procedure with excellent long-term success rates and can be used in the majority of ptosis patients with moderate-to-good levator function.

References
Scoppettulol E, Chadha V, Bunce C, Olver JM, Wright M . British Oculoplastic Surgery Society (BOPSS) National Ptosis Survery. Br J Ophthalmol 2008; 92: 1134–1138.
McCulley T, Kersten R, Kulwin D, Feuer W . Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthalmic Plast Reconst Surg 2003; 19: 388–393.
Berlin A, Vestal K . Levator aponeurosis surgery: a retrospective review. Ophthalmology 1989; 96: 1033–1037.
Liu D . Ptosis repair by single suture aponeurotic tuck. Surgical technique and long-term results. Ophthalmology 1993; 100 (2): 251–259.
Blaskovicz L . A new operation for ptosis with shortening of the levator and tarsus. Arch Ophthalmol 1923; 52: 563–573.
Dortzbach RK . Superior tarsal muscle resection to correct blepharoptosis. Ophthalmology 1979; 86 (10): 1883–1891.
Werb A . Ptosis. Trans Ophthalmol Soc N Z. 1976; 28: 29–32.
Buckman G, Jakobiec FA, Hyde K, Lisman RD, Hornblass A, Harrison W . Success of the Fasanella-Servat operation independent of Müller’s smooth muscle excision. Ophthalmology 1989; 96: 413–418.
Putterman AM, Urist MJ . Muller muscle-conjunctiva resection. Arch Ophthalmol 1975; 93: 619–623.
Putterman AM, Fett DR . Müller’s muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg 1986; 17: 354–360.
Lake S, Mohammad-Ali FH, Khooshabeh R . Open sky Müller’s muscle-conjunctiva resection for ptosis surgery. Eye (Lond) 2003; 17 (9): 1008–1012.
Khooshabeh R, Baldwin HC . Isolated Muller’s muscle resection for the correction of blepharoptosis. Eye (Lond) 2008; 22 (2): 267–272.
Baldwin HC, Bhagey J, Khooshabeh R . Open sky Müller muscle-conjunctival resection in phenylephrine test-negative blepharoptosis patients. Ophthal Plast Reconstr Surg 2005; 21 (4): 276–280.
Jones LT, Quickert MH, Wobig JL . The cure of ptosis by aponeurotic repair. Arch Ophthalmol 1975; 93: 629–634.
Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA . External levator advancement vs. Muller’s muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol 2005; 140: 426–432.
Dresner SC . Further modifications of the Müller’s muscleconjunctival resection procedure for blepharoptosis. Ophthal Plast Reconstr Surg 1991; 7: 114–122.
Kakizaki H, Zako M, Ide A, Mito H, Nakano T, Iwaki M . Causes of undercorrection of medial palpebral fissures in blepharoptosis surgery. Ophthal Plast Reconstr Surg 2004; 20 (3): 198–201.
Malhotra R, Salam A, Then SY, Grieve AP . Visible iris sign as a predictor of problems during and following anterior approach ptosis surgery. Eye (Lond) 2011; 25 (2): 185–191.
Carraway JH . The impact of Herring’s Law on blepharoplasty and ptosis surgery. Aesthet Surg J 2004; 24: 275–276.
Park DH, Baik BS . Advancement of the Müller muscle-levator aponeurosis composite flap for correction of blepharoptosis. Plast Reconstr Surg 2008; 122 (1): 140–142.
Kakizaki H, Zako M, Nakano T, Asamoto K, Miyaishi O, Iwaki M . The levator aponeurosis consists of two layers that include smooth muscle. Ophthal Plast Reconstr Surg 2005; 21 (4): 281–284.
Acknowledgements
We are indebted to Anna Williams who was involved in this study and assisted in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Peter, N., Khooshabeh, R. Open-sky isolated subtotal Muller’s muscle resection for ptosis surgery: a review of over 300 cases and assessment of long-term outcome. Eye 27, 519–524 (2013). https://doi.org/10.1038/eye.2012.303
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.303
Keywords
This article is cited by
-
Upper lid ptosis surgery: what is the optimal interval for the postoperative review? A retrospective review of 300 cases
Eye (2018)
-
Minimal incision posterior approach levator plication for aponeurotic ptosis
Eye (2015)
-
Aktuelle Aspekte der Ptosischirurgie
Journal für Ästhetische Chirurgie (2014)