Abstract
Purpose
The objective of this study is to assess whether baseline optic nerve head (ONH) topography and retinal nerve fiber layer thickness (RNFLT) are predictive of glaucomatous visual-field progression in glaucoma suspect (GS) and glaucomatous eyes, and to calculate the level of risk associated with each of these parameters.
Methods
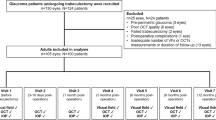
Participants with ≥28 months of follow-up were recruited from the longitudinal Advanced Imaging for Glaucoma Study. All eyes underwent standard automated perimetry (SAP), confocal scanning laser ophthalmoscopy (CSLO), time-domain optical coherence tomography (TDOCT), and scanning laser polarimetry using enhanced corneal compensation (SLPECC) every 6 months. Visual-field progression was assessed using pointwise linear-regression analysis of SAP sensitivity values (progressor) and defined as significant sensitivity loss of >1 dB/year at ≥2 adjacent test locations in the same hemifield at P<0.01. Cox proportional hazard ratios (HR) were calculated to determine the predictive ability of baseline ONH and RNFL parameters for SAP progression using univariate and multivariate models.
Results
Seventy-three eyes of 73 patients (43 GS and 30 glaucoma, mean age 63.2±9.5 years) were enrolled (mean follow-up 51.5±11.3 months). Four of 43 GS (9.3%) and 6 of 30 (20%) glaucomatous eyes demonstrated progression. Mean time to progression was 50.8±11.4 months. Using multivariate models, abnormal CSLO temporal-inferior Moorfields classification (HR=3.76, 95% confidence interval (CI): 1.02–6.80, P=0.04), SLPECC inferior RNFLT (per −1 μm, HR=1.38, 95% CI: 1.02–2.2, P=0.02), and TDOCT inferior RNFLT (per −1 μm, HR=1.11, 95% CI: 1.04–1.2, P=0.001) had significant HRs for SAP progression.
Conclusion
Abnormal baseline ONH topography and reduced inferior RNFL are predictive of SAP progression in GS and glaucomatous eyes.
Similar content being viewed by others
Introduction
Glaucoma is a multifactorial optic neuropathy characterized by a slowly progressive neurodegeneration of retinal ganglion cells and their axons characterized by a specific pattern of optic nerve head (ONH) and visual-field damage.1 Novel imaging technologies have been developed that are capable of detecting early glaucomatous damage using structural measures. Time-domain optical coherence tomography (TDOCT), scanning laser polarimetry using enhanced corneal compensation (SLPECC), and confocal scanning laser ophthalmoscopy (CSLO, Heidelberg Engineering) have been shown to discriminate between normal eyes and eyes with glaucomatous optic neuropathy, and are capable of identifying glaucomatous progression over time.2, 3, 4
Changes in the appearance of the optic nerve and RNFL thickness often precede the development of glaucomatous visual-field loss. Studies have demonstrated that abnormal baseline ONH topography and thin retinal nerve fiber layer thickness (RNFLT) measurements are predictive of future visual-field loss.5, 6, 7, 8, 9, 10, 11, 12, 13 Although structural risk factors associated with glaucoma progression have been studied in glaucoma suspect (GS) eyes, to our knowledge no studies have prospectively compared the predictive power of various posterior segment imaging technologies in a cohort of glaucomatous eyes.
The purpose of this study was to prospectively assess whether abnormal baseline ONH topography and reduced RNFLT measurements are predictive of glaucomatous visual-field progression in a cohort of eyes consisting of GS and glaucomatous eyes using TDOCT, SLPECC, and CSLO.
Materials and methods
Study population
This was a prospective, non-randomized, longitudinal cohort study. Participants consisted of GS and glaucoma patients with ≥28 months of follow-up, who were enrolled in the Advanced Imaging for Glaucoma Study (AIGS) conducted at Bascom Palmer Eye Institute, Palm Beach Gardens, FL, USA. Informed consent was obtained from all subjects using a consent form approved by the Institutional Review Board of the University Of Miami Miller School of Medicine, which was in agreement with the provisions of Declaration of Helsinki. The study was in accordance with the Health Insurance Portability and Accountability Act of 1996 privacy and security regulations. Inclusion criteria common to both groups consisted of spherical equivalent refractive error between −7 and +3 diopters sphere, best-corrected visual acuity of 20/40 or better, age between 40 and 80 years, and no prior history of intraocular surgery except for uncomplicated cataract extraction. Subjects with ocular disease other than glaucoma or cataract, parapapillary atrophy extending to 1.7 mm from the center of the optic disc, unreliable SAP, or poor-quality ONH or RNFL images were excluded. One eye of each eligible candidate was randomly selected for the analysis.
The GS eyes consisted of eyes with ocular hypertension characterized by intraocular pressure (IOP)≥24 mm Hg with normal optic discs and normal standard automated perimetry (SAP), patients with glaucomatous optic neuropathy on funduscopic examination, and review of stereoscopic optic disc photographs, but normal SAP. Glaucomatous optic neuropathy was defined as neuroretinal rim narrowing to the optic disc margin, notching, excavation, or RNFL defect. Glaucoma patients had glaucomatous optic nerve damage and corresponding abnormal SAP defined as glaucoma hemifield test outside normal limits, and pattern SD (PSD) outside 95% normal limits. Patients with SAP abnormalities had at least one confirmatory visual-field examination. All patients underwent a baseline examination consisting of a complete ophthalmic examination, including slit lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry, ultrasound pachymetry, dilated stereoscopic examination, and photography of the optic disc, SAP, and RNFL and ONH topography imaging. The RNFL imaging was performed using SLPECC (software version 6.1.0.4; Carl Zeiss Meditec Inc., Dublin, CA, USA), and TDOCT (Stratus OCT; software version 5.0.1; Carl Zeiss Meditec Inc.). The ONH topography imaging was performed with CSLO using Heidelberg Retina Tomograph 3 (HRT 3; software version 1.5.10.0; Heidelberg Engineering, Heidelberg, Germany). All patients underwent SAP and SLPECC, TDOCT, and CSLO imaging every 6 months. During the follow-up period, each patient was treated at the discretion of the attending physician.
Scanning laser polarimetry with enhanced corneal compensation
The SLPECC was performed in a standardized fashion through undilated pupils, considering the patient’s current refractive error to set the best focus for scanning the eye. The instrument uses a laser beam with a wavelength of 785 nm to scan the ocular fundus, within a field of 40° horizontally × 20° vertically, and a density of 256 × 128 pixels. In the ECC mode, the compensator is adjusted, so that combined with corneal birefringence, it produces a bias retardation of approximately 55 nm with the slow axis close to the vertical axis. The software then measures a higher total retardation than the RNFL retardation alone, resulting in an improved signal-to-noise ratio. The actual bias retardation and the axis in each image are measured from the macular region and mathematically removed from the final RNFL image to determine the actual RNFL retardation.14, 15, 16, 17, 18
Two sets of SLPECC images, each set consisting of three consecutive scans, were acquired at each visit by the same experience operator. The image with the highest quality was selected to be included in the analysis. A primary scan was obtained once before the baseline measurement to compensate for the corneal birefringence. A fixed concentric measurement band centered on the optic disc with a 3.2-mm outer and a 2.4-mm inner diameter was used to generate the peripapillary retardation measurements. Poor-quality SLPECC images (unfocused, poorly centered, obtained during eye movement, or quality score <8) were excluded. The SLPECC parameters investigated in this study included the superior average, inferior average, and temporal–superior–nasal–inferior–temporal average circumpapillary RNFL thickness measured using the automatically defined 3.2-mm diameter calculation circle. These parameters are provided on the standard SLPECC printout. We did not include the nerve fiber indicator parameter, because this parameter is generated by neural network technology using SLP with variable corneal compensation (SLPVCC) but not SLPECC. The VFI parameter does not appear on the SLPECC printouts for this reason.
The quality of the retardance image was also quantified using a support vector machine score called Typical Scan Score (TSS, ranging from 0 to 100). Abnormal retardation pattern (ARP) was defined as an SLP image with TSS <80. SLPECC images with ARP were excluded from the analysis.
Time-domain optical coherence tomography
The TDOCT was employed to measure the RNFL thickness. The software determines the RNFL thickness as the distance between the vitreoretinal interface and a posterior border, based on a predefined reflectivity signal level. The calibration was checked annually in accordance with the manufacturer’s guidelines by authorized technicians. At each visit, two images were acquired from each subject considering the patient’s current refractive correction to achieve the best focus. The image with the highest quality was selected for the analysis. Each image consisted of three sets of 256 A-scans along a 3.4-mm-diameter circumpapillary scan centered at the ONH. The fast-scanning mode was used, in which all scans are acquired and aligned automatically after initial positioning and acquisition by the operator. Peripapillary RNFL thickness parameters evaluated in this study were of average thickness (360°), superior quadrant thickness (46–135°), and inferior quadrant thickness (226–315°). These values were provided in the printout after averaging the results of three sequential circular scans captured during acquisition. Poor-quality scans were excluded, including images that were unfocused, poorly centered, obtained during eye movement, had a scan score <6, or those with failure to correctly segment the borders of the RNFL.
Confocal scanning laser ophthalmoscopy
CSLO images were acquired and analyzed using HRT 3 software. For optimum acquisition quality, the operator adjusted the focus using the patient’s current refractive error and added cylindrical lenses if needed, and fine-tuned the image of the video camera. For each patient, three topographical images were automatically acquired, aligned, and combined to make a single mean topography image. High-quality images required a focused reflectance image with an SD≤30. Outcome parameters selected consisted of cup volume, rim volume, global rim area, linear cup to disc ratio, and height variation contour. We also included Moorfields regression analysis (MRA) classification and glaucoma progression score (GPS) in temporal superior (45–90°), nasal superior (91–135°), nasal inferior (226–270°), and temporal inferior (271–315°) sectors. The GPS is automatically calculated and is independent of either contour line tracing or a reference plane. The software builds a three-dimensional model using five shape-based measures: cup size, cup depth, rim steepness, and vertical and horizontal parapapillary nerve fiber layer curvatures. Using a relevance vector machine, which is a machine-learning classifier, the HRT software compares the patient’s measurements with previously defined healthy and glaucomatous models.19 The final GPS is the probability of structural differences between the subject’s model and the normal model, consistent with glaucomatous damage. A higher GPS is indicative of a higher probability of glaucomatous damage. The GPS cutoff values proposed by the manufacturer for global and sectoral analyses, and for the final classification on the CSLO printout, indicate that GPS results between 0 and 0.27 are classified as within normal limits, between 0.28 and 0.64 as borderline, and between 0.65 and 1.0 as outside normal limits.
Progression definition using SAP
SAP was performed using the Swedish Interactive Threshold Algorithm (Humphrey Field Analyzer 750 II-i, 24-2 SITA Standard; Carl Zeiss Meditec Inc.). Reliable test results, based on the AIGS initial definition of ≤33% fixation losses, false-negative, and false-positive rates, were included. These reliability criteria were established 10 years ago at the time our NIH-sponsored AIG protocol was initiated, and were consistent with the literature. All patients were experienced with automated perimetry and had undergone a minimum of two visual-field tests before study enrolment. During the visual-field examination, the technician constantly monitored the position of the pupil compared with the trial lens rim. All visual fields were controlled to rule out the possibility of rim artifact and were repeated if the results were unsatisfactory.
SAP progression was evaluated using pointwise linear regression (PLR) analysis of sensitivity values of individual test locations over time, using the Progressor software (version 3.3; Medisoft Inc., Leeds, UK). The PLR analysis of serial visual fields allows the longitudinal evaluation of sensitivity values at each test location over time, and calculates the slope of change at each test location and provides individual, regional, and global rates of change and the associated levels of statistical significance.20 Progression was defined as the presence of a minimum of two adjacent test locations in the same hemifield, each losing>1 dB threshold sensitivity per year at P<0.01.20, 21 We required the confirmation of progression on at least one consecutive follow-up visual field.
Statistical analysis
Statistical analyses were performed using the JMP software version 8.0 (SAS Inc., Cary, NC, USA) to determine the predictive impact of baseline ONH topography and RNFLT on glaucomatous visual-field progression. All tests were two-sided and a P-value of <0.05 was considered significant. Analysis of variance was used for the continuous variables and χ2-test was used for the categorical variables, to compare the clinical characteristics of the two groups. Univariate and multivariate Cox proportional hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated. Univariate Cox proportional hazard regression models examined the HRs for the individual parameters and were not adjusted for the presence of other factors. Predictors with a P-value of 0.2 or less were considered for the multivariate models. Age, baseline IOP, central corneal thickness (CCT), and SAP PSD were identified as the clinical risk factors that had the highest predictive values. These variables have been identified to be significantly associated with the risk of development of glaucomatous visual-field progression.11, 22 Multivariate Cox proportional hazard models were constructed and were all adjusted for age, CCT, IOP, and SAP PSD. The Kendall’s τ-coefficient was calculated for different imaging procedures in non-progressing and progressing eyes separately. To construct the Kaplan–Meier curves, the RNFLT values were categorized into lowest quartile, median, and upper quartile. Positive predictive values, negative predictive values, and likelihood ratios were calculated. The α-level (type I error) was set at 0.05.
Results
Seventy-three eyes of 43 GS and 30 glaucoma patients, consisting 46 women and 27 men, were enrolled. Table 1 demonstrates the baseline characteristics of the visual-field and -imaging measures, along with the follow-up time and the number of examinations in GS and glaucomatous eyes. The mean age in the GS group was 60.9±9.4 years, and in the glaucoma group was 66.6±8.7 years (P=0.01). Only one eye of each subject was included. The mean follow-up time was 51.5±11.3 months (range, 28–73). The follow-up time was longer for the GS group compared with the glaucoma group (53.8±10.4 vs 48.3±11.8 months, respectively; P=0.04). The mean baseline IOP was higher in the GS group compared with the glaucoma group (19.0±3.4 vs 13.7±3.7 mm Hg, respectively; P<0.001). The visual-field MD and PSD indices were worse in glaucoma patients (−5.0±4.5 and 6.3±4.2 dB, respectively) compared with the GS patients (0.01±1.2 vs 1.6±0.5 dB, respectively; P<0.001). Four of 43 GS eyes (9.3%) and 6 of 30 (20%) glaucomatous eyes demonstrated SAP progression using PLR analysis. ‘Time to progression’ was defined as the visit that an eye was first deemed to be progressing, using the PLR definition of progression. Mean time to progression was 50.8±11.4 months (range, 28–73). Glaucoma patients showed progression significantly (P=0.02) earlier during the follow-up period (47.1±11.9 months) compared with GS patients (53.3±10.5 months).
The following clinical parameters were identified as having the greatest univariate Cox proportional HRs and were included in the multivariate models: age (1 year older, HR=1.11, 95% CI=1.03–1.24, P=0.008), SAP PSD (1 dB higher, HR=1.16, 95% CI=1.00–1.31, P=0.047), IOP (1 mm Hg higher, HR=0.89, 95% CI=0.78–1.02, P=0.08), and CCT (25 μm thinner, HR=1.28, 95% CI=0.83–2.09, P=0.2). Tables 2 and 3 demonstrate univariate and multivariate Cox proportional HRs for SLPECC, TDOCT, and CSLO parameters, respectively. Using multivariate models, the following parameters were significantly predictive (P=0.04, 0.02, and 0.001, respectively) of SAP progression: abnormal CSLO temporal inferior MRA classification (HR=3.76, 95% CI=1.02–6.80, P=0.04), SLPECC inferior RNFLT per 1 μm thinner (HR=1.38, 95% CI=1.02–2.2, P=0.02), and TDOCT inferior RNFLT per 1 μm thinner (HR=1.11, 95% CI=1.04–1.2, P=0.001).
The Kendall’s τ-coefficient, which demonstrates if a pair of observations is concordant, was calculated for different imaging procedures in non-progressing and progressing eyes separately. The highest Kendall’s τ-coefficient was between average RNFL thickness measure of TDOCT and SLPECC (τ=0.73, P<0.001), followed by inferior RNFL thickness measure of TDOCT and SLPECC (τ=0.56, P=0.03) in progressing eyes. In non-progressing eyes, the Kendall’s τ-coefficient between the average RNFL thickness values of TDOCT and SLPECC was τ=0.46, P<0.001, and between the inferior RNFL thickness values of TDOCT and SLPECC was τ=0.51, P<0.001.
Kaplan–Meier curves were constructed to compare the cumulative probability of SAP progression for various structural parameters. The lowest quartile RNFLT was compared with the combined median and upper quartile. Eyes with a CSLO Moorfields classification outside normal limits were compared with eyes classified as not outside normal limits. Figure 1 illustrates the survival analyses for each of three parameters using SLPECC, TDOCT, and CSLO, with significant HRs identified in multivariate Cox models. There was a higher probability of SAP progression in eyes categorized in the lowest quartile inferior RNFL thickness using SLPECC and TDOCT (Figures 1a and b), and eyes categorized as having a Moorfields classification outside normal limits (Figure 1c). Table 4 demonstrates the positive and negative predictive values and the likelihood ratios. In general, the negative predictive values were high, between 0.88 and 0.89.
(a) Cumulative probability of visual-field progression when inferior retinal nerve fiber layer thickness measured using SLPECC is within the lowest quartile vs combined median and upper quartile. (b) Cumulative probability of visual-field progression when inferior retinal nerve fiber layer measured using TDOCT is within the lowest quartile vs combined median and upper quartile. (c) Cumulative probability of visual-field progression when the CSLO temporal inferior Moorfields classification is outside normal limits (ONL) vs combined borderline (BL) and within normal limits (WNL).
Discussion
Previous studies have examined the ability of abnormal baseline structural measurements to predict progression among GS eyes. Lalezary et al12 found that reduced average, superior, and inferior RNFLT measured using TDOCT were significant risk factors for progression (HRs between 1.49 and 1.57). Mohammadi et al11 reported that abnormal baseline inferior ratio, ellipse modulation, and longitudinal discriminant function using SLPVCC were significant risk factors associated with SAP progression among GS eyes (highest HR 1.11 to 1.18). Zangwill et al6, Weinreb et al7, and Alencar et al19 identified various abnormal optic disc topographic using CSLO, which were significant risk factors for glaucomatous progression (maximum HR of 5.80).
In the present study, we prospectively compared the predictive abilities of three commonly employed posterior segment imaging technologies for the development of glaucomatous visual-field progression in a cohort of eyes consisting of GS and glaucomatous eyes. In contrast to prior studies, we evaluated functional progression using the trend-based PLR. The HRs in our study varied between 1.04 and 4.2, and were consistent with previous reports. Of interest was the observation that reduced inferior RNFL and optic disc topography had the greatest predictive value using all three technologies, which is in agreement with previous clinical findings.23
It should be noted that the mean follow-up duration (53.8±10.4 in GS and 48.3±11.8 in glaucoma) and the mean time to progression (53.3±10.5 in GS and 47.1±11.9 in glaucoma) were very close. This finding indicates that an average of 4 years of follow-up is required to observe visual-field progression using PLR in a treated glaucoma cohort, and we might have had found higher number of progressing eyes if these eyes were followed up for a longer period of time or if they were not treated. A recent study has confirmed that the rate of visual-field progression and the number of visual-field locations reaching a PLR endpoint decreased after therapy, based on the Ocular Hypertensive Treatment Study event-based endpoint among ocular hypertensive participants originally randomized to observation or treatment.24
Our results agree with a study conducted by Sung et al,25 who demonstrated that an abnormal inferior optic disc or RNFL sector were associated with future visual-field progression. We found that lower baseline measures in the inferior optic nerve and RNFL are more likely to influence progressive glaucomatous visual-field loss. Early glaucomatous optic nerve damage has been reported to occur more commonly at the inferior optic disc pole compared with the superior sector. In normal eyes, the neuroretinal rim is usually broadest in the inferior rim, followed by the superior and nasal rims, and thinnest in the temporal disc region. This pattern of rim width is known as the ISNT rule (inferior≥superior≥nasal≥temporal). The ISNT rule was originally described after assessment of optic disc photographs of 457 normal eyes26 and is often used in clinical practice to help detect early glaucomatous optic neuropathy.
The present study has several limitations. The sample size is relatively small. This was not a randomized clinical trial and patients were not washed out at the beginning of the study. Participants were treated at the discretion of the physician during the course of the study, and treatments were not standardized. Lastly, the functional outcome used in this study was defined using linear regression of individual sensitivity values generated using Progressor software, not widely utilized by clinicians. Therefore, risk factors for progression using this strategy may differ from those identified using event-based strategies for detecting SAP progression.
In conclusion, our results emphasize that if inferior RNFL or ONH is within normal limits in GS and glaucomatous eye, then there is a lower risk for visual-field progression. Baseline optic nerve and RNFLT abnormalities are useful adjuncts for prediction of subsequent SAP progression in GS and glaucomatous eyes, and finally structural factors associated with progression should be incorporated with established clinical and demographic risk factors in risk models.

References
Weinreb RN, Khaw PT . Primary open-angle glaucoma. Lancet 2004; 363: 1711–1720.
Zangwill LM, Bowd C, Berry CC, Williams J, Blumenthal EZ, Sanchez-Galeana CA et al. Discriminating between normal and glaucomatous eyes using the Heidelberg Retina Tomograph, GDx Nerve Fiber Analyzer, and Optical Coherence Tomograph. Arch Ophthalmol 2001; 119: 985–993.
Medeiros FA, Zangwill LM, Bowd C, Weinreb RN . Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol 2004; 122: 827–837.
Sehi M, Grewal DS, Sheets CW, Greenfield DS . Diagnostic ability of Fourier-domain vs time-domain optical coherence tomography for glaucoma detection. Am J Ophthalmol 2009; 148: 597–605.
Zangwill LM, Weinreb RN, Berry CC, Smith AR, Dirkes KA, Liebmann JM . The confocal scanning laser ophthalmoscopy ancillary study to the ocular hypertension treatment study: study design and baseline factors. Am J Ophthalmol 2004; 137: 219–227.
Zangwill LM, Weinreb RN, Beiser JA, Berry CC, Cioffi GA, Coleman AL et al. Baseline topographic optic disc measurements are associated with the development of primary open-angle glaucoma: the Confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment Study. Arch Ophthalmol 2005; 123: 1188–1197.
Weinreb RN, Zangwill LM, Jain S, Becerra LM, Dirkes K, Piltz-Seymour JR et al. Predicting the onset of glaucoma: the confocal scanning laser ophthalmoscopy ancillary study to theOcular Hypertension Treatment Study. Ophthalmology 2010; 117: 1674–1683.
Strouthidis NG, Gardiner SK, Owen VM, Zuniga C, Garway-Heath DF . Predicting progression to glaucoma in ocular hypertensive patients. J Glaucoma 2010; 19: 304–309.
Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN . Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol 2009; 127: 1250–1256.
Vizzeri G, Weinreb RN, Martinez de la Casa JM, Alencar LM, Bowd C, Balasubramanian M et al. Clinicians agreement in establishing glaucomatous progression using the Heidelberg retina tomograph. Ophthalmology 2009; 116: 14–24.
Mohammadi K, Bowd C, Weinreb RN, Medeiros FA, Sample PA, Zangwill LM . Retinal nerve fiber layer thickness measurements with scanning laser polarimetry predict glaucomatous visual field loss. Am J Ophthalmol 2004; 138: 592–601.
Lalezary M, Medeiros FA, Weinreb RN, Bowd C, Sample PA, Tavares IM et al. Baseline optical coherence tomography predicts the development of glaucomatous change in glaucoma suspects. Am J Ophthalmol 2006; 142: 576–582.
Gardiner SK, Johnson CA, Demirel S . Cup size predicts subsequent functional change in early glaucoma. Optom Vis Sci 2011; 88: 1470–1476.
Sehi M, Guaqueta DC, Greenfield DS . An enhancement module to improve the atypical birefringence pattern using scanning laser polarimetry with variable corneal compensation. Br J Ophthalmol 2006; 90: 749–753.
Lemij HG, Reus NJ . New developments in scanning laser polarimetry for glaucoma. Curr Opin Ophthalmol 2008; 19: 136–140.
Zhou Q . Retinal scanning laser polarimetry and methods to compensate for corneal birefringence. Bull Soc Belge Ophtalmol 2006; 302: 89–106.
Zhou Q, Weinreb RN . Individualized compensation of anterior segment birefringence during scanning laser polarimetry. Invest Ophthalmol Vis Sci 2002; 43: 2221–2228.
Greenfield DS, Knighton RW, Huang XR . Effect of corneal polarization axis on assessment of retinal nerve fiber layer thickness by scanning laser polarimetry. Am J Ophthalmol 2000; 129: 715–722.
Alencar LM, Bowd C, Weinreb RN, Zangwill LM, Sample PA, Medeiros FA . Comparison of HRT-3 glaucoma probability score and subjective stereophotograph assessment for prediction of progression in glaucoma. Invest Ophthalmol Vis Sci 2008; 49: 1898–1906.
Hitchings RA, Migdal CS, Wormald R, Poinooswamy D, Fitzke F . The primary treatment trial: changes in the visual field analysis by computer-assisted perimetry. Eye 1994; 8: 117–120.
De Moraes CG, Juthani VJ, Liebmann JM, Teng CC, Tello C, Susanna Jr R et al. Risk factors for visual field progression in treated glaucoma. Arch Ophthalmol 2011; 129: 562–568.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720.
Jonas JB, Dichtl A . Evaluation of the retinal nerve fiber layer. Surv Ophthalmol 1996; 40: 369–378.
De Moraes CG, Demirel S, Gardiner SK, Liebmann JM, Cioffi GA, Ritch R et al. Effect of treatment on the rate of visual field change in the ocular hypertension treatment study observation group. Invest Ophthalmol Vis Sci 2012; 53: 1704–1709.
Sung KR, Kim S, Lee Y, Yun SC, Na JH . Retinal nerve fiber layer normative classification by optical coherence tomography for prediction of future visual field loss. Invest Ophthalmol Vis Sci 2011; 52: 2634–2639.
Jonas JB, Gusek GC, Naumann GO . Optic disc, cup and neuroretinal rim size, configuration and correlations in normal eyes. Invest Ophthalmol Vis Sci 1988; 29: 1151–1158.
Acknowledgements
This study was supported by NIH Grant R01-EY013516, Bethesda, MD, USA; P30EY014801 University of Miami Core Grant; unrestricted grant from Research to Prevent Blindness, New York, NY, USA; and Department of Defense Grant to University of Miami (DOD-Grant number W81XWH-09-1-0675). Dr Greenfield has received research support from Carl Zeiss Meditec Inc.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented in part at the Annual Meeting of American Glaucoma Society, Dana Port, CA, USA, on 5 March 2011
Appendix A
Appendix A
Advanced Imaging for Glaucoma (AIG) Study Group: (1) Bascom Palmer Eye Institute, University of Miami, Palm Beach Gardens, FL, USA: DS Greenfield, M Sehi, CD Quinn, K Kishor; (2) University of Pittsburgh Medical Center, Pittsburgh, PA, USA: JS Schuman, G Wollstein, H Ishikawa, RJ Noecker, Larry Kagemann; (3) Doheny Eye Institute, University of Southern California, Los Angeles, CA, USA: R Varma, V Chopra, B Francis; (4) Casey Eye Institute, Oregon Health and Science University, Portland, OR, USA: D Huang, J Morrison, P Francis, B Edmunds, M Parikh, D Gatty, R Armour, L Lombardi, O Tan, Xinbo Zhang, Yimin Wang. See www.AIGStudy.net for the full list of authors.
Rights and permissions
About this article
Cite this article
Sehi, M., Bhardwaj, N., Chung, Y. et al. Evaluation of baseline structural factors for predicting glaucomatous visual-field progression using optical coherence tomography, scanning laser polarimetry and confocal scanning laser ophthalmoscopy. Eye 26, 1527–1535 (2012). https://doi.org/10.1038/eye.2012.203
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.203
Keywords
This article is cited by
-
Prediction of Visual Field Progression in Patients with Primary Open-Angle Glaucoma, Mainly Including Normal Tension Glaucoma
Scientific Reports (2017)
-
Baseline thickness of macular ganglion cell complex predicts progression of visual field loss
Graefe's Archive for Clinical and Experimental Ophthalmology (2014)