Abstract
Purpose
To evaluate the functional and morphological outcomes of postoperative systemic steroid therapy after successful macular surgery in eyes with macular edema due to idiopathic macular epiretinal membranes (ERMs).
Design
Prospective, randomized, investigator-masked, controlled clinical study.
Methods
Twenty-eight patients scheduled for 23-gauge vitrectomy combined with ERM and inner limiting membrane (ILM) peeling for macular edema due to ERM were included in this single center trial. Patients were randomized to receive oral steroid therapy (Prednisolone, 100 mg per day for 5 days) or no oral steroid (control group) after surgery. Main outcome measures included best corrected visual acuity (BCVA; Early Treatment Diabetic Retinopathy Study), central retinal thickness (CRT), retinal volume (RV), and macular morphology as determined by spectral domain optical coherence tomography (SD-OCT, Cirrus). Examinations were carried out preoperatively and at week 1, at months 1 and 3, postoperatively.
Results
At month 3, mean BCVA improved to a eight-letter gain in each study group (P<0.01 compared with baseline for both groups), showing no statistically significant difference between both the groups (P=0.19). Morphologically, retinal surface folds resolved within 1 month after surgery in both treatment groups, followed by a progressive recovery of retinal layer integrity and a statistical significant (P<0.01) decrease in CRT and RV without significant differences between both groups (P=0.62, P=0.13, respectively, ANOVA between the groups).
Conclusion
The early postoperative use of systemic steroid treatment after successful vitrectomy combined with ERM and ILM peeling does not seem to improve significantly the anatomic and functional outcomes in eyes with ERM.
Similar content being viewed by others
Introduction
Vitreomacular traction syndrome by epiretinal membranes (ERMs) is a common macular pathology leading to morphological distortion of the retinal surface because of the proliferation of myofibroblasts, the contractile element of the ERM, followed by functional changes such as metamorphopsia and visual deterioration.1 The current standard of care for this epimacular pathology is vitrectomy and membrane peeling, a procedure that is thought to relieve epiretinal traction and macular edema, followed by regeneration of the intraretinal architecture and recovery of visual function.2 Despite the successful removal of the ERM, it is known that retinal morphology in the macula does not completely return to normal structure after macular surgery, and the functional results are not always satisfactory, probably due to some irreversible damage of photoreceptors as well as postoperative inflammation and scarring. The most significant prognostic factors for the clinical outcome of ERM surgery have been identified as being preoperative visual acuity (VA), duration of symptoms, and macular edema.3,4
The postoperative reduction of inflammation, fibrosis, and macular edema may significantly influence the prognosis of a successful postoperative treatment after macular surgery. It is well known that glucocorticoids reduce early inflammatory reactions such as increased permeability of capillaries, capillary dilatation, leukocyte extravasation, and fibrin deposition, as well as late inflammatory reactions such as proliferation of fibroblasts and collagen deposition.5 Steroid treatment may, therefore, lead to accelerated reduction of macular edema and less severe scarring after macular surgery, resulting in faster recovery of visual outcome.
Although studies could demonstrate the undisputed anti-inflammatory and anti-proliferative effect of steroids in different macular diseases such as diabetic macular edema6 or exudative age-related macular degeneration (AMD),7 there is no standardized scheme regarding the application, duration, and dosage as a postoperative therapy. Overall, looking at the currently available literature, the widespread use of steroids after intravitreal surgery in clinical practice lacks any scientific basis in terms of evidence-based medicine. Moreover, steroid treatment was combined with other medications or with additional surgical procedures in most of the published studies, therefore, the results cannot be attributed to the steroid effects alone.8,9 As steroids also have a number of unwanted systemic side effects such as diabetes mellitus, increased infection risk, wound healing disorders, osteoporosis, psychiatric disorders,10 as well as increase in intraocular pressure (IOP) and cataract formation in the eye,11,12 the uncritical use of a systemic steroid therapy should be put into question until its effectiveness has been proven.
The aim of the present study was to evaluate short-term outcomes of patients who received standardized postoperative systemic steroid treatment after successful 23-gauge vitrectomy combined with ERM and inner limiting membrane (ILM) peeling for macular edema due to ERM compared with patients without postoperative steroid treatment.
Patients and methods
Patients and examination procedures
This prospective, randomized, controlled, investigator-masked single center clinical trial was conducted at the Department of Ophthalmology at the Medical University of Vienna. The study and data accumulation were approved by the local institutional review board (Ethics Committee of the Medical University of Vienna), were registered within the EudraCT database for clinical trials (No. 2006-006871-19), and followed the tenets of the Declaration of Helsinki. Informed consent for the research was obtained from all participants.
Patients scheduled for ERM surgery without any prior treatment and a VA of 20/40 to 20/400 were enrolled. After inclusion into the study, the participants were randomly assigned 1 : 1 to either the treatment group or to the control group using a computer-generated randomization list. Patients with any changes in the central retina (eg, diabetic retinopathy or neovascular AMD), with high myopia (<−6 spheres), any history of intraocular surgery, aphakia, uveitis, glaucoma, significant cataract, or eye trauma were excluded from this study.
All patients underwent a complete ophthalmological examination 3 days before surgery, including best corrected VA (BCVA) using early treatment diabetic retinopathy study (4-m distance) charts, IOP measurements using applanation (Goldmann) tonometry, slit-lamp biomicroscopy, fundus examination with dilated pupils and spectral-domain optical coherence tomography (SD-OCT) imaging using the Cirrus OCT (Carl Zeiss Meditec AG, Jena, Germany). Follow-up examinations were performed at week 1, months 1 and 3 including BCVA, SD-OCT, and laser cell flare meter (LFCM) measurements.
Surgery and postoperative management
Vitrectomy was performed in all cases by two experienced surgeons (SS and CP) using the OS3 vitreoretinal system (Oertli, Berneck, Switzerland). Oblique-angled incisions were made in the conjunctiva and in the sclera through the pars plana with a 23-gauge blade in the inferotemporal, superonasal, and superotemporal quadrants. Trocars were inserted through these wounds and the infusion cannula was placed in the inferotemporal quadrant, whereas the superonasal and superotemporal quadrants were used for the retinal instrumentation. A core vitrectomy was performed and the posterior hyaloid membrane was separated from the retina. A plano–concave contact lens was used for the visualization of the macula during peeling. The ERM as well as the ILM were peeled in the macular area using end-gripping forceps with the additional use of 0.15% Membrane-blue (Dutch Ophthalmic USA, Exeter, NH, USA). Thereafter, peripheral retina was examined under indentation and air–fluid exchange was performed. Finally the inserts were removed and when necessary the sclerotomies were closed using 7/0 Vicryl suture (Ethicon, Brussels, Belgium). The treatment group received four Prednisolone (25 mg) tablets (100 mg) (Aprednislon, Merck, Darmstadt, Germany) combined with daily one Pantoprazole (40 mg) tablet (Pantoloc, Altana Pharma, Konstanz, Germany) to prevent gastric side effects, for 5 days. The control group did not receive systemic steroids. All patients received a combination of dexamethasone/gentamicin ointment (Dexagenta ointment; Croma Pharma, Leobendorf, Austria) immediately after surgery. The eye was then covered overnight. At day 1 postoperatively, the eyes were treated with dexamethasone/gentamicin eyedrops (Dexagenta eyedrops) and ketorolac-trometamol eyedrops (Acular eyedrops, Pharm Allergan, Ettlingen Germany) four times a day for 4 weeks.
Morphological imaging using SD-OCT
OCT images were obtained using SD, high-definition OCT. The Cirrus SD-OCT produces high-resolution B-scan images by a raster scanning technique with an axial resolution of 5 μm within a 6 × 6-mm (20° × 20°) area. The 512 × 128 × 1024 scan was used to document the course of central retina thickness (CRT) and retinal volume (RV). For morphological analysis, a high-resolution B-scan was performed. The presence or absence of intraretinal cysts and foveal depression, as well as the appearance of retinal layer integrity and the severity of epiretinal surface folding was graded. Retinal layer pathology was characterized by three different grades: grade 1 with an intact layer structure; grade 2 when the retinal layer structure was recognized but disturbed; and grade 3 when no layer pattern could be distinguished. Retinal surface folds (RSFs) were characterized as no detectable retinal folding (grade 1), mild (grade 2), or severe (grade 3). All morphological gradings were performed by a certified OCT reader of the Vienna Reading Center, Austria (MR).
Flare measurements
Anterior chamber flare measurements were performed 30 min after pupil dilation with one drop of 1% tropicamide (Mydriatikum Agepha; Agepha, Soeding, Austria) and 2.5% phenylephrine (sterile solution produced by the hospital's dispensary), using a Kowa FC-1000 LFCM (Kowa Co. Ltd, Tokyo, Japan), before the OCT examinations were carried out. Two trained doctors (GM and RD) took all measurements. Calibration of the LFCM was performed according to the manual. Seven readings were taken with a background scatter of <10%. The highest and lowest readings were discarded and the remaining five values were averaged to obtain the flare value documented (expressed in photons per millisecond).
Statistical analyses
All calculations were performed using SPSS for Windows Version 17.0 (SPSS Inc., Chicago, IL, USA). The repeated ANOVA test and the repeated measures t-test was used for statistical analysis of changes in BCVA, CRT, RV, IOP, and LFCM values compared with baseline. For analysis of changes in retinal morphology, the χ2-test was used. A value of P≤0.05 was considered as statistically significant after Bonferroni–Holm's multiple test correction.
Results
Twenty-eight eyes of 28 consecutive patients (mean age 71 years, range 63–87, 22 women, 6 men) were included in this study; 14 patients were randomly enrolled into each study group. One patient was excluded from the study because of the additional use of Indocyanin green dye (ICG-Pulsion, Medical AG, Munich, Germany) for ILM visualization during macular surgery. Baseline characteristics were well balanced between the two groups. There was no statistically significant difference with regard to BCVA, CRT, RV, or IOP at baseline (Table 1).
At the time of surgery, in the steroid group, 3 eyes (21%) were pseudophakic and 11 eyes (79%) were phakic, and in the control group, 1 eye (7%) was pseudophakic and 13 eyes were phakic. None of the phakic eyes had significant clinical worsening of cataract during the follow-up period, and none underwent cataract extraction and intraocular lens implantation.
Visual acuity outcomes
Mean BCVA of eyes enrolled into the control group showed an increase from 29±10 letters at baseline to 36±12 letters at week 1, 40±13 letters at month 1, and then a decrease to 37±12 letters at month 3. Compared with baseline, changes in BCVA were statistically significant (P<0.01) at month 1 (Table 1, Figure 1).
Mean BCVA of eyes enrolled into the steroid group improved from 34±8 letters at baseline to 38±8 letters at week 1, 41±5 letters at month 1, and 42±4 at month 3. Compared with baseline, changes in BCVA were statistically significant (P<0.01) at month 1 (Table 1, Figure 1). Comparing the mean BCVA of both groups showed no statistically significant difference between the groups (P=0.19, ANOVA between groups).
Central retinal thickness, retinal volume, and retinal morphology outcomes
Mean CRT and RV values showed similar changes for both groups up to month 3 follow-up. In the control group, CRT decreased from 470±107 μm at baseline to 418±62 μm at week 1, 404±66 μm at month 1, and 370±51 μm at month 3. RV decreased from 12.0±1.3 mm3 at baseline to 11.6±1.1 mm3 at week 1, 11.1±1.1 mm3 at month 1, and 10.7±0.6 mm3 at month 3 (Table 1, Figure 2). Compared with baseline, the decrease in mean CRT and RV became statistically significant as early as week 1 (P<0.01). In the steroid group, mean CRT decreased from 496±57 μm at baseline continuously to 431±45 μm at week 1, 406±47 μm at month 1, and to 380±55 μm at month 3 (P<0.01). Mean RV values decreased from 12.5±1.2 mm3 at baseline to 12.1±1.0 mm3 at week 1, 11.7±0.7 mm3 at month 1, and 11.3±1.1 mm3 at month 3 (P<0.01, Table 1, Figure 2). Compared with baseline, the decrease in CRT and RV became statistically significant as early as week 1 (P<0.05). There was no statistically significant difference between the groups with regard to CRT and RV (P=0.62, P=0.13, respectively, ANOVA between the groups).
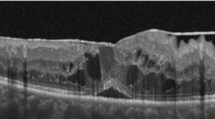
Retinal morphology, as documented by high-resolution B-scans of SD-OCT, recovered substantially after macular surgery with complete removal of the ERM and ILM in all eyes of both treatment groups. SD-OCT images allowed for identification of intraretinal cysts, presence of a foveal contour, and the varying degree of distortion of the neurosensory layers from the ILM to retinal pigment epithelium. The presence and severity of such intraretinal disturbances vary at baseline presentation and demonstrate a characteristic recovery process over time. The grading system described above was used to quantify the intensity of RSF and retinal layer integrity, as well as the presence of intraretinal cysts and a foveal contour.
RSFs resolve most rapidly as early as 1 week after surgery, representing the fastest postoperative morphological improvement, showing no significant difference between the two treatment groups (P>0.05). The restoration of retinal layer integrity proceeds more slowly and incompletely in both the groups with no significant difference between the groups (P>0.05). The resolution of intraretinal cysts and recovery of the foveal contour proceeds similarly in both the groups, most intensively during the first postoperative month. Absolute and relative values of the morphological grading are presented in Table 2.
Figure 3 shows representative cases from each study group.
Macular morphology. Cirrus SD-OCT B-scans (left column) and retinal thickness maps (right column) of a representative case from each treatment group during follow-up. Panels (a–c) show scans of a patient from the steroid group: 3a=baseline, 3b=month 1, and 3c=month 3. Panels (d–f) show scans of a patient from the control group: 3d=baseline, 3e=month 1, and 3f=month 3. In both the cases, the mild preoperative retinal wrinkling similarly resolved, the retinal thickness decreased, and the retinal layer integrity was restored.
Flare measurements
During the study period, there was no significant difference between the treatment groups regarding changes in anterior chamber flare measurements. The values within the two groups showed no significant difference between the three postoperative visits (Table 1).
Safety
Within the follow-up of 3 months, none of the participants showed any local or systemic adverse event related to steroid therapy. No cataract development or retinal detachment was observed during the follow-up time. Mean preoperative IOP was 14±3.3 in the steroid and 15±1.7 in the control group (P=0.20). During the study period, there was no statistically significant difference between the follow-up visits within and between the groups (Table 1); none of the patients needed anti-glaucoma treatment.
Discussion
The overall results of this prospective, randomized, controlled study show that 23-gauge vitrectomy, ERM and ILM peeling for idiopathic ERMs is an effective and safe technique for the treatment of macular edema due to idiopathic ERM. The results of both treatment groups compare favorably with previous studies. Fine et al13 reported that VA improved from a mean of 0.16 to 0.22 (decimal equivalent), after 23-gauge vitrectomy in 20 patients with idiopathic ERMs. Gupta et al14 investigated the short-term outcomes and reported VA improvement from a mean of 0.23 to 0.36 (decimal equivalent) after ERM peeling in 36 eyes. Tewari et al15 also described favorable visual outcomes in 20 eyes with a mean VA improvement from 0.3 to 0.4 (decimal equivalent). However, all of these studies were performed purely by peeling the ERM mechanically and the associated macular edema disappeared spontaneously over several months during the postoperative phase.
Corticosteroids have been used in ophthalmology since the early 1950s to suppress intraocular inflammation by reducing inflammatory exudation and inhibiting proliferation of fibroblasts and formation of granulation tissue.16,17,18,19 They have been applied topically as eyedrops, locally by subconjunctival, peribulbar, or by intravitreal injections, or systemically as oral medications or by intravenous or intramuscular injections. Besides their use in conditions such as proliferative diabetic retinopathy,20 diabetic macular edema,6 exudative AMD,7 or central retinal vein occlusion,21 steroids have also been applied in combination with intraocular surgery. Körner et al22 reported a trend to a reduction of postoperative fibrosis after systemic cortisone therapy. Valone et al23 report in their study about 134 patients with complete retinal detachment. They found a reduction of inflammatory signs and the rate of postoperative choroid detachment after combined systemic therapy with cortisone and antibiotics.
The aim of the present study was to investigate a potential advantage of combining macular surgery for idiopathic ERM with postoperative short-term treatment with systemic steroid. It is widely assumed that adjuvant pharmacological therapy of steroid treatment, administered locally or systemically in association with vitreomacular surgery, may have a beneficial effect on the progress of visual recovery. Although macular edema, secondary to ERM, is likely to be of more mechanical than of primarily inflammatory nature, it has been shown that the initial mechanical traction of the retinal surface is associated with secondary biochemical pathways involving different cytokines, which may contribute to the development of macular edema. Therefore, it is considered that steroids may function to combat the secondary inflammatory effects triggered by the mechanical distortion and thus accelerate the resolution of macular edema. A previous report on concomitant administration of intravitreal triamcinolon (IVTA) with macular surgery for ERM described the short-term visual recovery after use of IVTA.24 It was noted that the level of achieved vision within 1 week is almost identical to the final VA data after 6 months. On the basis of these data, the authors suggest that the use of IVTA gives an important benefit by accelerating visual recovery. However, these observations are based on a retrospective uncontrolled case series.
Our study was designed as a prospective, controlled, investigator-masked single center trial, using systemic Prednisolone instead of IVTA, providing the most reliable setting for the assessment of a potential advantage of steroid treatment after macular surgery. Short-term results of this investigation show no treatment benefit of macular surgery combined with oral Prednisolone compared with macular surgery alone. BCVA significantly improved, and CRT as well as RV significantly decreased in both groups compared with baseline. No statistically significant difference was observed between both treatment groups during the entire study duration. Even analysis of retinal morphology, being the most sensitive parameter for assessment of any difference in postoperative restoration of the retinal surface and recovery of neurosensory layer integrity, showed no significant difference between the groups. One reason for this might be that the concentration of 100 mg Prednisolone per day for 5 days was not high enough to show a significant effect. In addition, a possible effect of the topical treatment with ketorolac-trometamol eyedrops in both groups for 4 weeks postoperatively should be considered.
Some potential complications of steroid treatment include cataract formation and increase in IOP. The incidence of cataract progression after steroid treatment appears to differ considerably between reports (7–24%).25,26 No clinical cataract progression was observed and none of the patients required cataract surgery with intraocular lens implantation during the follow-up period. This result indicates that the present study is able to show the influence of systemic steroid on the functional outcome without any additional vision disturbing pathology of the eyes. There is limited knowledge regarding IOP changes after intravitreal injection or short-term systemic application of steroids in vitrectomized eyes. Tsujikawa et al27 reported an IOP increase of >21 mm Hg in 9 of 17 (53%) vitrectomized eyes after IVTA injection of 10 mg. In our study, no statistically significant elevation of the IOP after vitrectomy was seen in both groups.
In summary, the present study shows that 23-gauge vitrectomy combined with ERM and ILM peeling is a safe and effective technique for the treatment of macular edema in eyes with idiopathic macular ERM. The postoperative administration of systemic steroid treatment does not seem to significantly improve the anatomic and functional outcomes. Further randomized clinical studies should be conducted to investigate the effect of local steroids (s.a., intravitreal Osurdex, IVTA, or subconjuctival dexamethasone) on different vitreoretinal surgeries.

References
Gandorfer A, Rohleder M, Kampik A . Epiretinal pathology of vitreomacular traction syndrome. Br J Ophthalmol 2002; 86: 902–909.
Massin P, Allouch C, Haouchine B, Yoshimura N . Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol 2000; 130: 732–739.
Michalewski J, Michalewska Z, Cisiecki S, Nawrocki J . Morphologically functional correlations of macular pathology connected with epiretinal membrane formation in spectral optical coherence tomography (SOCT). Graefes Arch Clin Exp Ophthalmol 2007; 245: 1623–1631.
Pesin SR, Olk RJ, Grand MG, Boniuk I, Arribas NP, Thomas MA et al. Vitrectomy for premacular fibroplasia. Prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology 1991; 98: 1109–1114.
Schwab F . Cortison und Auge. Wr Med Wochenschrift 1958; 108: 839–842.
Jonas JB, Söfker A . Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular oedema. Am J Ophthalmol 2001; 132: 425–427.
Challa JK, Gillies MC, Penfold PL, Gyory JF, Hunyor AB, Billson FA . Exudative macular degeneration and intravitreal triamcinolone: 18-month follow-up. Aust NZJ Ophthalmol 1998; 26: 277–281.
Weller M, Wiedemann P, Heimann K . Proliferative vitreoretinopathy—is it anything more than wound healing at a wrong place? Int Ophthalmol 1990; 14: 105–117.
Wiedemann P . Drug treatment of proliferative vitreoretinopathy. Fortschr Ophthalmol 1989; 86: 115–120.
Stanbury RM, Graham EM . Systemic corticosteroid therapy—side effects and their management. Br J Ophthalmol 1998; 82: 704–708.
Gillies MC, Simpson JM, Luo W, Penfold P, Hunyor AB, Chua W et al. A randomized clinical trial of a single dose of intravitreal triamcinolone acetonide for neovascular age-related macular degeneration: one-year results. Arch Ophthalmol 2003; 12: 667–673.
Jonas JB, Degenring RF, Kreissig I, Akkoyun I, Kamppeter BA . Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Ophthalmology 2005; 112: 593–598.
Fine HF, Iranmanesh R, Iturralde D, Spaide RF . Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology 2007; 114: 1197–1200.
Gupta OP, Ho AC, Kaiser PK, Regillo CD, Chen S, Dyer DS et al. Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol 2008; 146: 193–197.
Tewari A, Shah GK, Fang A . Visual outcomes with 23-gauge transconjunctival sutureless vitrectomy. Retina 2008; 28: 258–262.
Gordon DM, McLean JM . Effects of pituitary adrenocorticotropin hormone (ACTH) therapy in ophthalmic conditions. JAMA 1950; 142: 1271–1276.
Olson JA, Steffensen EN, Margulis RR, Smith RW, Whitney EL . Effect of ACTH on certain inflammatory diseases of the eye: a preliminary report. JAMA 1950; 142: 1276–1278.
Woods AC . Clinical and experimental observations on the use of ACTH and cortisone in ocular inflammatory disease. Am J Ophthalmol 1950; 33: 1325–1349.
Ruhmann AG, Berliner DL . Influence of steroids on fibroblasts. II. The fibroblast as an assay system for topical antiinflammatory potency of corticosteroids. J Invest Dermatol 1967; 49: 123–130.
Jonas JB, Hayler JK, Söfker A, Panda-Jonas S . Intravitreal injection of crystalline cortisone as adjunctive treatment of proliferative diabetic retinopathy. Am J Ophthalmol 2001; 131: 468–471.
Bynoe LA, Weiss JN . Retinal endovascular surgery and intravitreal triamcinolone acetonide for central vein occlusion in young adults. Am J Ophthalmol 2003; 135: 382–384.
Koerner F, Merz A, Gloor B, Wagner E . Postoperative retinal fibrosis—a controlled clinical study of systemic steroid therapy. Graefes Arch Clin Exp Ophthalmol 1982; 219: 268–271.
Valone Jr J, Moser D . Management of rhegmatogenous retinal detachment with macula detached. Steroids, choroidal detachment, and acuity. Ophthalmology 1986; 93: 1413–1417.
Konstantinidis L, Berguiga M, Beknazar E, Wolfensberger TJ . Anatomic and functional outcome after 23-gauge vitrectomy, peeling, and intravitreal triamcinolone for idiopathic macular epiretinal membrane. Retina 2009; 29: 1119–1127.
Gillies MC, Simpson JM, Billson FA, Luo W, Penfold P, Chua W et al. Safety of an intravitreal injection of triamcinolone: results from a randomized clinical trial. Arch Ophthalmol 2004; 122: 336–340.
Zkiris A, Erkilic K . Complications of intravitreal injection of triamcinolone acetonide. Can J Ophthalmol 2005; 40: 63–68.
Tsujikawa A, Fujihara M, Iwawaki T, Yamamoto K, Kurimoto Y . Triamcinolone acetonide with vitrectomy for treatment of macular edema associated with branch retinal vein occlusion. Retina 2005; 25: 861–867.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ritter, M., Sacu, S., Matt, G. et al. Use of systemic steroid after successful macular surgery in eyes with epiretinal membrane: a randomized, controlled clinical study. Eye 25, 1284–1293 (2011). https://doi.org/10.1038/eye.2011.190
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.190