Abstract
Purpose
To validate a table of amounts of three horizontal muscle surgery in patients with large-angle infantile esotropia (≥60 prism dioptres, PD).
Methods
A prospective interventional case series reporting the postoperative alignment of 51 patients (27 male, 24 female) over a 15-year period was conducted. Surgery amounts were according to a published table developed on a previous patient cohort (n=49), using bilateral medial rectus recession with graded unilateral lateral rectus resection. Kaplan–Meier life-table survival curves were formulated for success to orthotropia (±10 PD) after one and subsequent horizontal muscle surgeries for up to 8 years follow-up.
Results
The median preoperative deviation was 65 PD (range 60–80 PD) and median age at surgery was 11.8 months (range 5.1 months–3.6 years). Surgical success to orthotropia (±10 PD) after one surgery was 100% at 2 months, 95.7% at 6 months, 91.3% at 12 months, 77.8% at 4 years, and 73.6% at 8 years. Postoperative failure requiring further horizontal surgery occurred in 17.6% (residual esotropia 4, consecutive exotropia 5).
Conclusions
Our second cohort has reproduced the success rate of the previous cohort (77.8% vs 77.1% at 4 years). If the published table of surgical amounts is used, three horizontal muscle surgery in large-angle infantile esotropia (≥60 PD) appears to have a good long-term success rate, and does not lead to the high rates of either residual esotropia or consecutive exotropia reported by others in the literature.
Similar content being viewed by others
Introduction
There has been ongoing debate about surgical management approaches for infantile esotropia. The various surgical interventions for infantile esotropia have included performing a unilateral medial rectus recession and lateral rectus resection, a ‘uniform’ approach with bilateral medial rectus recession, or a ‘selected’ approach for larger preoperative angles by performing three (or four) horizontal muscle surgery that involves bilateral medial rectus recessions and unilateral (or bilateral) lateral rectus resections.1 Despite the widespread use of these different surgical approaches, there are few published tables to guide surgery amounts, no prospective validation studies of surgery amounts, and no randomized controlled trials.2, 3, 4
The majority of published cohort studies are retrospective with widely variable success rates on children aged from 3 months to 11 years old at the time of surgery and with preoperative angles ranging from 20 to 100 prism dioptres (PD). Few studies have reported subgroup analysis and instead the results of success to orthotropia were on the groups as a whole making their results difficult to apply to clinical practice. Although it has become more widely accepted that early surgery results in better binocular vision in infantile esotropia,5, 6, 7, 8, 9, 10 there is no agreed consensus on the amount of surgery to perform for different preoperative angles, particularly in large-angle infantile esotropia, which has been defined as ≥60 PD in this study, alongside previously published definitions.11
All long-term studies of postoperative alignment to orthotropia (±10 PD) in patients with infantile esotropia have demonstrated progressive failure over time.12, 13 Prieto Diaz and Prieto Diaz12 demonstrated Kaplan–Meier (KM) survival curves for infantile esotropia, with success to orthotropia of approximately 70% at 10 years and 50% at 20 years follow-up.12 Louwagie et al13 reported that further surgery was required in 51% of cases by 10 years and 66% by 20 years for a large cohort following unspecified type or amount of surgery.
To date, the literature has reported variable success to orthotropia when two muscle surgery was performed for large-angle infantile esotropia (≥60 PD). Since the late 1970s the success rates of large bilateral medial rectus recession (eg, 6–8 mm recession from muscle insertion or 10.5 mm from the limbus) for infantile esotropia >50 PD has been reported to be between 60 and 91%.5, 11, 14, 15, 16, 17 Similarly, the success rates of three horizontal muscle surgeries have been reported between 61 and 82%.4, 18, 19, 20
It has been proposed that the undercorrection rates (residual esotropia) after bilateral medial rectus recession may be due to inadequate surgery amounts and/or due to the variability of the medial rectus insertion, which can range from 3.0 to 6.0 mm from the limbus.21 Unreliable results may occur when planning surgical recession from the muscle insertion rather than the limbus.3, 14 The supporters of two muscle surgery argue that it is a simpler, quicker procedure with lower rates of overcorrection, which also leaves the lateral rectus untouched for future surgery if required. However, we have found bilateral medial rectus recessions frequently result in residual esotropia when used for angles of greater than 55 PD.
In a previous study, the senior author (GAG) defined a table of amounts of surgery20 that was formulated to improve the results of surgery in large-angle infantile esotropia and reduce the need for subsequent surgeries. The aim of this study was to validate the table of numbers in a separate prospective cohort of patients.
Materials and methods
This study was a prospective interventional cohort of 51 children from a single paediatric ophthalmology practice. We used the table of numbers20 (Table 1) to guide surgery for all patients with large-angle infantile esotropia ≥60 PD. The term large-angle infantile esotropia was defined by Costenbader10 in 1961 as angles greater than 30 PD, but for this paper we used the term for angles ≥60 PD in keeping with previous authors' and common current clinical usage.11 All surgeries were performed by one surgeon (GAG) over 15 years (August 1993 to April 2009) and no patients in this validation study were reported on in the previous study.
The following parameters were recorded for each patient: preoperative deviation (in PD), preoperative binocular spherical equivalent refraction (dioptres, D), need for preoperative patching, age at the time of surgery, bilateral medial rectus recession, lateral rectus resection, vertical component, postoperative assessment, duration of follow-up, prevalence of inferior oblique overaction, dissociated strabismus complex, postoperative patching, and amblyopia. The need for further surgery and time intervals for under- and overcorrection were recorded.
All preoperative and postoperative measurements were performed using two loose plastic isosceles prisms (Gulden, Elkins Park, PA, USA) held in one hand (separately over each eye, that is, not stacked) with the bases facing out in the position suggested by O'Flynn,22 which in practice is more or less in the sagittal plane. We acknowledge the potential errors inherent in measuring large angles of strabismus with prisms.23 Measurement techniques included the alternate cover test and Krimsky light reflex using an accommodative target for distance and near if possible. The senior author recently described a test useful in very young patients, where difficulties in measurement may occur,24 that utilizes the principles of both Krimsky light reflex and the Bruckner reflex. Vertical muscle imbalance (A or V pattern associated with superior oblique or inferior oblique overaction) and dissociated vertical deviation were assessed preoperatively with appropriate surgical correction incorporated into the surgical plan as required. Cycloplegic retinoscopy was performed at least 30 min following instillation of two drops of 0.5% cyclopentolate (Bausch & Lomb, Chauvin Pharmaceuticals Ltd, London, UK) for patients less than 1 year of age, or 1% cyclopentolate for patients older than 1 year.
The surgical technique for both recession and resection was as described by Wright et al,25 but all recessions were measured from the limbus (as per Kushner and Helveston),3, 20, 21 rather than the muscle insertion. The Castroviejo squint caliper was used to check these measurements (Figure 1). We chose the amount of recession based on Helveston's numbers for bilateral medial rectus recession, with two modifications as described in the author's original paper: 20
-
1)
The amount of recession performed was 0.5 mm less than the amounts used by Helveston owing to concerns about the possibility of consecutive exotropia resulting from large bilateral medial rectus recession when combined with a lateral rectus resection.20
-
2)
The limbus-based measurements were made with a radial chord dropped back the required amount to mark the centre of the new insertion; further scleral marks were then made superiorly or inferiorly to intersect with a chord dropped radially from the old insertion (to mark the entry point of the suture needle immediately behind the original insertion). Using this technique, the reinserted muscle has a linear insertion parallel to the original insertion and tangential to the limbus. The measurement from the limbus to the centre of the new insertion is confirmed with the Castroviejo caliper before final suture tying.20
Postoperative surgical success was defined as alignment to orthotropia (±10 PD). A surgical failure (residual esotropia or consecutive exotropia) was defined as alignment >10 PD (esotropia or exotropia) after the 1-week postoperative visit, and that required further surgery. Postoperative over- or undercorrection was aggressively treated with appropriate use of miotics, spectacles, or prisms. Tabulation of the postoperative alignments was performed for the following postoperative intervals: 1 week, 2 months, 6 months, 12 months, 18 months, 2 years, and annually thereafter. KM life-table analysis was used to formulate curves to demonstrate surgical success over time after one three-horizontal muscle surgery and overall after subsequent surgeries were performed in the event of a surgical failure.
The maximum follow-up interval and corresponding alignment was taken as that occurring at the most recent postoperative visit, date of second operation for residual esotropia or consecutive exotropia, or date of last examination before loss to follow-up. Data analysis was ceased after 8 years owing to the author's (GAG) practice to discharge at 8/9 years of age if the uncorrected alignment was orthotropic.
We certify that all applicable institutional and governmental regulations concerning the ethical treatment of humans were followed and all patients underwent surgery with full informed consent from their parents/guardians.
Statistical analysis
The distribution of non-Gaussian variables is described as a median (range). Statistical significance was taken at the 95% confidence interval and all statistical analysis was performed using STATA IC 10.1 (StataCorp, College Station, TX, USA).
Results
In all, 51 patients (27 boys, 24 girls) underwent bilateral medial rectus recession and unilateral lateral rectus resection according to the senior author's table of amounts of surgery (Table 1). The median preoperative deviation was 65 PD (range 60–80 PD) and median spherical equivalent refraction was +1.75 D (range −3.75 to +5.75 D).
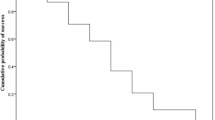
In total, 18 children (35.3%) required patching preoperatively to treat fixation preference. The median age at the time of surgery was 11.8 months (range 5.1 months to 3.6 years; Figure 2). Median overall follow-up after surgery was 3.1 years (range 1.6 months to 13.4 years).
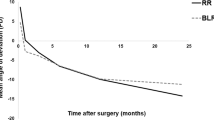
Figure 3a demonstrates the change from preoperative alignment to postoperative alignment after one surgery. Surgical success to orthotropia (±10 PD) after one surgery was 100% at 2 months, 95.7% at 6 months, 91.3% at 12 months, 77.8% at 4 years, and 73.6% at 8 years (Figure 3b).
Postoperative failure requiring further horizontal surgery by 8 years occurred in 17.6% (residual esotropia 4, consecutive exotropia 5). The mean age at the time of surgery in this group was 16.9 months and mean preoperative deviation was 70.6 PD. Mean time to failure overall was 21.3 months (range, 2.5–47.2 months). Mean time to failure for residual esotropia was 23.3 months (range, 2.8–40.5 months, mean age at surgery 17.4 months, mean preoperative deviation 68.8 PD) and for consecutive exotropia was 19.7 months (range, 2.5–47.2 months, mean age at surgery 16.6 months, mean preoperative deviation 72 PD).
Only one patient required more than two horizontal surgeries. Overall 23.5% (n=12) patients required further surgery for either postoperative failure (n=9), dissociated horizontal deviation (n=2), or subsequent oblique overaction that was not apparent preoperatively (n=8). The mean number of total surgeries required was 1.27 (range 1–4). The rate of dissociated strabismus complex was 37.3% (n=19): dissociated vertical deviation 16 and dissociated horizontal deviation 5. The rate of inferior oblique overaction was 52.9% (n=27), but the majority of these patients (n=20) underwent inferior oblique surgery at the time of the initial three horizontal muscle surgery.
Surgical success to orthotropia (±10 PD) after subsequent surgery was 100% at 2 months, 97.9% at 6 months, 97.9% at 12 months, 97.9% at 4 years, and 85% at 8 years (Figure 3c).
In our series, 35% (n=18) patients required preoperative patching vs 33% (n=17) postoperatively. At study conclusion, there were seven patients with amblyopia, all of whom had amblyopia treated preoperatively. Five patients required patching postoperatively, who did not have preoperative patching and were successfully treated (ie, no amblyopia at last follow-up).
Discussion
The purpose of this study was to validate a table of amounts of surgery previously reported for large-angle infantile esotropia (≥60 PD). There are few studies recommending table of amounts of surgery, but none have been validated in follow-up studies.4
Since the late 1970s the success rates of large bilateral medial rectus recession for infantile esotropia >50 PD has been reported between 60 and 91%.5, 11, 14, 16, 17, 26, 27 Ing and Okino5 reported only a 30% success rate for bilateral medial rectus recessions of 5 mm for esotropia greater than 50 PD. In 1979, Hess and Calhoun11 reported 60% success to orthotropia with 7 mm bilateral medial rectus recession. Stager et al14 and Weakley et al26 had surgical success of 60% and 75–77%, respectively, using 6–7 mm recessions.14, 26 Symzd et al16 reported 91% success rates at 6 weeks postoperatively using 6–7 mm bilateral medial rectus recession in 45 patients with esotropia >50 PD. Damanakis et al27 performed 8 mm recession in 16 patients (70–80 PD), and although successful in 75%, the rate of undercorrection was still 25%. In 1999, Tolun et al17 reported results of bilateral medial rectus recessions of 8 mm in a group of 54 patients with mean preoperative deviation of 70 PD and had success in 67% of cases up to 7 years follow-up. In these studies, the medial rectus recession amounts were measured from the muscle insertion and not the limbus as in our study. Kushner et al28 performed large bilateral medial rectus recessions of 10.5 mm measured from the limbus and demonstrated success in 84% of cases in a group with mean preoperative deviation of 53 PD. In the same study, graded recessions up to 6 mm from the insertion had poorer results (success 63%), which formed part of the basis for our recommendation to measure the recession amount from the limbus.
Three horizontal muscle surgeries for large-angle infantile esotropia have had a similar spread of success rates (61–82%; Figure 4).1, 18, 19, 20 In our previous study of 49 patients with mean 69 PD (range 60–85), surgical success to orthotropia was 77.6% when formulating the proposed table of numbers.20
Scott compared the results of 107 patients with >50 PD infantile esotropia who underwent either two muscle surgery (5–6.5 mm recession from insertion, but no further than 11.5 mm from the limbus) vs three/four muscle surgery (11 mm bilateral medial rectus recession in conjunction with a 6 or 7 mm lateral rectus resection) in a retrospective comparison study.1 A table similar to our recommended surgery amounts was reported.1 Surgical success with three or four horizontal muscle surgery was twice that of bilateral medial rectus recession alone (65% vs 29%). The rate of undercorrection after three/four muscle surgery was 21% (vs 58% in two muscle surgery) and the rate of overcorrection in the early postoperative period was 17% (vs 5% in two muscle surgery), but in most cases patients became orthotropic over time.1 In this series, three and four muscle surgery reduced the need for reoperation almost fivefold (6% vs 29%).1 The authors also argued that three/four horizontal muscle surgery as the initial surgical treatment reduced the anaesthetic risk to the child through lower reoperation rates.1 Although this showed promising results in support of a more directed selective surgery, there are some limitations of the study making the application of these results to clinical practice difficult. The two groups compared were not similar preoperatively and the study also included patients up to 11 years old, which is beyond the critical period for visual development.
In 2005, Minkoff and Donohue29 reported their poor results because of late consecutive exotropia in a small cohort of 10 children (mean age 13 months, mean preoperative deviation 62.5 PD (50–85 PD). Their reasoning for the low success rate (30%) was attributed to adult surgery dosages and ‘preoperative measurement error’ causing overestimation of the esotropia.29 Another proposed reason for their high overcorrection correction rate was either due to the placement of the medial rectus more than 1.5 mm posterior to the equator or posterior migration of the new insertion with axial length growth.29 The patients in this study who had preoperative angles >60 PD and required subsequent surgery for consecutive exotropia received larger amounts of recessions/resection at the initial surgery than our table would suggest.
The reasons why some patients develop late-onset consecutive exotropia are poorly understood. A number of authors have suggested multiple reasons for late-onset consecutive exotropia (amblyopia and lack of postoperative binocularity, mechanical limitation of postoperative adduction, high hypermetropia, nystagmus, A/V patterns, family history of strabismus, and vertical deviations).30, 31 Ludwig and Chow32 have demonstrated the presence of scar remodeling with lengthening of the scar between the previously recessed muscle and the sclera in 50% of patients with later onset of consecutive exotropia. In our small group of patients who developed overcorrection (n=5), they had one or more of the following previously reported features that may be associated with a risk of late consecutive exotropia: amblyopia, hyperopia >4 D, need for secondary surgery for oblique overaction, and/or the presence of dissociated strabismus complex. However, with such small numbers these were not statistically meaningful. No patient in this cohort exhibited signs of scar remodelling at reoperation.
Our recommended table of amounts of surgery has been validated in this second cohort by reproducing the success rate of the previously published cohort (77.8% vs 77.1% at 4 years). If the published table of surgical amounts is used, three horizontal muscle surgery in large-angle infantile esotropia (≥60PD) appeared to have a good long-term success rate, and did not lead to the high rates of either residual esotropia or consecutive exotropia reported by others in the literature.

References
Scott W, Reese PD, Hirsch CR, Flabetich CA . Surgery for large angle congenital esotropia: two vs three and four horizontal muscles. Arch Ophthalmol 1986; 104: 374–377.
Polling JR, Eijkemans MJ, Esser J, Gilles U, Kolling GH, Schultz E et al. A randomised comparison of bilateral recession vs unilateral recession–resection as surgery for infantile esotropia. Br J Ophthalmol 2009; 93: 954–957.
Kushner BJ, Morton GV . A randomized comparison of surgical procedures for infantile esotropia. Am J Ophthalmol 1984; 98: 50–61.
Elliott S, Shafiq A . Interventions for infantile esotropia. Cochrane Database Syst Rev 2005; 25 (1): CD004917.
Ing MR, Okino LM . Outcome study of stereopsis in relation to duration of misalignment in congenital esotropia. J AAPOS 2002; 6: 3–8.
Birch EE, Stager DR . Monocular acuity and stereopsis in infantile esotropia. Invest Ophthalmol Vis Sci 1985; 26: 1624–1630.
Wong A . Timing of surgery for infantile esotropia: sensory and motor outcomes. Can J Ophthalmol 2008; 43: 643–651.
Nelson LB, Wagner RS, Simon JW, Harley RD . Congenital esotropia. Surv Ophthalmol 1987; 31: 363–383.
Assaf AA . Early vs late alignment of infantile esotropia. Strabismus 1995; 3 (2): 61–69.
Costenbader FS . Infantile esotropia. Trans Am Ophthalmol 1961; 59: 397–429.
Hess JB, Calhoun JH . A new rationale for the management of large angle esotropia. J AAPOS 1979; 16: 345–348.
Prieto-Diaz J, Prieto-Diaz I . Long term outcome of treated congenital/infantile esotropia: does early surgical binocular alignment restoring (subnormal) binocular vision guarantee stability? Binocul Vis Strabismus 1998; 13: 249–254.
Louwagie CR, Diehl NN, Greenberg AE, Mohney BG . Long-term follow-up of congenital esotropia in a population-based cohort. J AAPOS 2009; 13 (1): 8–12.
Stager DR, Wagner Jr DR, Everett ME, Birch EE . Delayed consecutive exotropia following 7-millimetre bilateral medial rectus recession for congenital esotropia. J AAPOS 1994; 31: 147–150.
Nelson LB, Calhoun JH, Simon JW, Wilson T, Harley RD . Surgical management of large angle infantile esotropia. Br J Ophthalmol 1987; 71: 380–383.
Szmyd SM, Nelson LB, Calhoun JH, Spratt C . Large bimedial rectus recessions in infantile esotropia. Br J Ophthalmol 1985; 69: 271–274.
Tolun H, Dikici K, Ozkiris A . Long term results of bimedial rectus recessions in infantile esotropia. J AAPOS 1999; 36: 201–205.
Lee DA, Dyer JA . Bilateral medial rectus recession and lateral rectus muscle resection in the treatment of congenital esotropia. Am J Ophthalmol 1983; 95: 528–535.
Foster RS, Paul TO, Jampolsky A . Management of infantile esotropia. Am J Ophthalmol 1976; 82: 291–292.
Forrest MP, Finnigan S, Finnigan S, Gole GA . Three horizontal muscle squint surgery for large angle infantile esotropia. Clin Experiment Ophthalmol 2003; 31: 509–516.
Helveston EM . Surgical Management of Strabismus: An Atlas of Strabismus Surgery, 5th edn. Wayenborgh Publishing: Belgium, 2005, pp 109–110.
O'Flynn EA . Strabismus documentation: an alternative approach. Br Orthopt J 1994; 51: 10–14.
Thompson JT, Guyton DL . Ophthalmic prisms: measurement errors and how to minimize them. Ophthalmology 1983; 90: 204–210.
White JE, Gole GA . Combining the Bruckner reflex and the Krimsky test for measuring the angle of strabismus. Clin Experiment Ophthalmol 2009; 37 (6): 633–634.
Wright KW, Farzavandi S, Thompson L . Colour Atlas of Ophthalmic Surgery: Strabismus. Lippincott: Philadelphia, 1991.
Weakley Jr DR, Stager DR, Everett ME . Seven millimeter bilateral medial rectus recessions in infantile esotropia. J AAPOS 1991; 28: 113–115.
Damanakis AG, Arvanitis PG, Ladas ID, Theodossiadis GP . 8 mm bimedial rectus recession in infantile esotropia of 80–90 prism dioptres. Br J Ophthalmol 1994; 78: 842–844.
Kushner BJ, Fisher MR, Lucchese NJ, Morton GV . Factors influencing response to strabismus surgery. Arch Ophthalmol 1993; 111: 75–79.
Minkoff OV, Donahue SP . Three-muscle surgery for infantile esotropia in children younger than age 2 years. J AAPOS 2005; 42: 144–148.
Windsor CE . Surgically overcorrected esotropia: a study of its causes, sensory anomalies, fusional results, and management. Am Orthopt J 1966; 16: 8–15.
Bradbury JA, Doran RML . Secondary exotropia: a retrospective analysis of matched cases. J Pediatric Ophthalmol Strabismus 1993; 30: 163–166.
Ludwig IH, Chow AY . Scar remodeling after strabismus surgery. J AAPOS 2000; 4: 326–333.
Acknowledgements
MJ Walsh was supported by National Health and Medical Research Council Grant No. 496602.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented as part of the Claud Worth Oration at the Annual Scientific Meeting of the British Isles Paediatric Ophthalmology and Strabismus Association, Glasgow, 23 September 2009.
Rights and permissions
About this article
Cite this article
Camuglia, J., Walsh, M. & Gole, G. Three horizontal muscle surgery for large-angle infantile esotropia: validation of a table of amounts of surgery. Eye 25, 1435–1441 (2011). https://doi.org/10.1038/eye.2011.185
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.185
Keywords
This article is cited by
-
Dreimuskelchirurgie bei großwinkliger Esotropie
Der Ophthalmologe (2022)
-
Why bilateral medial rectus recession fails? Factors associated with early repeated surgery
International Ophthalmology (2020)
-
Essential infantile esotropia: postoperative motor outcomes and inferential analysis of strabismus surgery
BMC Ophthalmology (2014)