Abstract
Falls are an important health issue. They cause significant morbidity and mortality particularly in older people, and also have marked psychological effects on the individual. The literature focuses particularly on older adults, an age group in which both visual impairment and falls are more prevalent, as is the associated morbidity. In this review, we summarise the current literature and point to further studies which need to be undertaken. The consequences of falls are well recognised, and there has been considerable work into identifying risk factors. Changes in visual components such as visual field, acuity, contrast sensitivity and stereopsis all have a part and the co-existence of other sensory impairments certainly increases the risk of falls. However there remain considerable gaps in our knowledge of the relationship between visual loss and falls, for example in patients with diabetic eye disease. Furthermore, there is also conflicting data as to the importance of different visual components. Various interventions, such as programmed inter-disciplinary involvement, have shown promise, however these need further confirmation of their efficacy and cost effectiveness. An added confounder may be that an intervention (eg, cataract extraction) paradoxically affects an individual's future activity level and behaviour, thereby increasing the risk of falling. With an ageing population the importance of this topic is likely to increase, as will the potential benefits of optimising our assessment and management of these patients.
Similar content being viewed by others
Introduction
Falls account for approximately half of all accident-related deaths1 In 1999 there were 204 424 admissions to hospital for fall-related injuries in the United Kingdom for adults aged 60 years and older. The cost to the NHS was previously estimated at £981 million,2 but a more recent report suggests that the NHS spends £1.7 billion per annum solely treating hip fractures resulting from falls.3 The major financial implications at the population level,2 has made the issue important politically, a fact acknowledged in the National Service Framework (2006).4
The impact experienced by younger individuals is less clear;5 however, it has been argued that falls are just as much a problem in the young due to greater knock on effects on work and economic activity. A descriptive study based on questionnaire results found 18% of individuals below 40 and 21% of middle aged individuals reported a fall in the previous year.6 The pattern of injuries was slightly different, with the young injuring their hands, knees and ankles while the older group injured their heads and knees. The authors suggested that further investigation is warranted in younger age groups. This is certainly true; nevertheless this review concentrates on the effects in older individuals; the group in which both falls and visual impairment are more common and the consequences more severe.
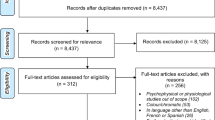
Search strategy
A search of the Medline, Pubmed, and Cochrane databases was performed in February 2010 using the terms ‘vision’ or ‘visual loss’ and ‘falls’ to identify suitable studies. A background search on falls was performed using the terms ‘falls’, ‘review’ and ‘elderly’ and relevant references were sourced. Relevant studies were reviewed and are discussed as appropriate in the review.
Where do falls occur?
Falls might be expected to occur most commonly with more active pursuits; however, in all age groups studies have shown that most falls occur while walking or doing routine tasks.6, 7 In older individuals over 50% of falls happen in the home,8, 9 possibly related to the fact that nearly 20% of people over the age of 75 years are house bound. In one study 60% falls occurred at home, 30% in public places and 10% in healthcare institutions.10
Risk factors
The main risk factors for falls are listed in Table 1 . The increased risk of falls in the elderly is thought to be multifactorial. Decreased vestibular reflexes, decreased muscle strength, increasing postural sway and concurrent medical issues are the main contributors.11 Visual input is thought to be important in allowing individuals to co-ordinate and plan movement, as well as helping in maintaining balance.12
Consequences of a fall
The consequences of a fall can be far reaching; causing serious injury, physical deterioration and institutionalisation.26, 27 The risk of injury after a fall is higher in the elderly because of greater bone fragility and poorer protective reflexes. In a community-based study28 active older people had more serious injuries than frail participants after a fall (22% compared with 6%). Frail participants were defined by combining demographic, physical and psychological characteristics. The incidence of falling in 1 year of follow-up was highest in the frail group (52%) and lowest in the more active group (17%). However 22% (5 of 23) of falls by more active subjects, but only 6% (5 of 89) of falls by frail subjects, resulted in serious injury requiring hospital treatment. It is likely that the forces involved in falls in more active individuals are greater leading to worse injuries.
Hip fracture is the most serious injury secondary to a fall,27 the incidence varying from 6–10%.29 This rate is higher in older individuals; 15–20% in over 85 years old. The majority of patients with a hip fracture do not return to the level of activity of daily living, which they showed before the fracture.1 Twelve months after a hip fracture, 21.8% who had previously lived at home had moved to a nursing home and only 24% were as mobile as they were before the fracture.30 The high mortality rate for individuals in the first year after a hip fracture is also well described, with rates of 20–35%.31
In addition to the purely physical effects of a fall, many older people experience psychological difficulties. This may result in activity avoidance and loss of self-confidence.32 Fear of falling can lead to self-imposed restrictions on activities, which in themselves cause isolation and a loss of independence. Fear of falling has gained acceptance as a medical issue and has been found to be present in individuals who have never fallen as well as those who have. A recent review found the main risk factors for fear of falling to be increasing age, being female and having had at least one previous fall.33 The main consequences were identified as a decline in physical and mental performance, an increased risk of falling and progressive loss of health-related quality of life. Furthermore, a recent study investigating health-related quality of life measures found that fear of falling had the greatest impact in elderly women.34
Prevalence of visual loss in the elderly
Visual impairment affected approximately 10% of people aged 65–75 years and 20% of those aged 75 and older in one study.35 In all, 90% of the blind and partially sight-registered individuals in the United Kingdom are over 60 years of age. In addition, 98% of people aged 65 years and above wear glasses as a result of the loss of accommodation and lenticular changes that develop with increasing age.35 Other data also confirm the increasing prevalence of visual impairment with age, with 3.1% of 65 to 74 year old, 11.6% of 75 to 84-year-old and 35.5% of 85+ year old individuals having visual impairment.1
Vision loss and falls
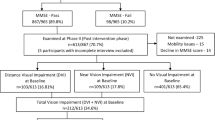
Older adults with impaired vision have been shown to be more likely to fall than their sighted peers. Hip fractures have been linked to visual impairment and to individual measures of vision such as reduced visual acuity, contrast sensitivity and visual field.21A study by Squirrel et al36 examined the prevalence of visual impairment in adults suffering a hip fracture. They found that 33% were classified as visually impaired (6/18 or worse in both eyes) and 58% had a distance visual acuity of 6/18 or worse in at least one eye.
There is considerable epidemiological evidence that older individuals with visual impairment are more likely to fall than those without. The Beaver Dam Study showed impaired visual acuity to be associated with an increased risk of falls; odds ratios for two or more falls in the past year for the poorest category of visual function (⩽20/40) were 2.02 (95% confidence interval (CI), 1.13–3.63) for current binocular acuity and 1.85 (95% CI, 1.10–3.12) for visual sensitivity.37 It was also shown that poor vision was associated with increased frailty in the elderly; the odds ratios of nursing home placement were 3.20 (95% CI, 1.85–5.56) for current binocular vision ⩽20/40, and 5.00 (95% CI, 2.28, 10.94) for near vision of ⩽20/40 Snellen equivalent. Other measures of frailty in this study included use of walking aids, and time taken for a measured walk. This study found visual acuity to be more strongly linked to falls and measures of frailty than contrast sensitivity. However, other studies have found contrast sensitivity and stereopsis to have a more significant effect.18
The results of the Blue Mountains Eye Study also showed significant associations between visual impairment and an increased risk of falls and hip fractures. Two or more falls in individuals with visual acuity worse than 20/40 were 1.9 times more common than controls, after correcting for confounders.19
Recent publications have understandably emphasized the importance of visual assessment in patients who have fallen,38, 39 despite this a recent Royal College of Physicians audit showed 50% (151/302) of sites did not employ a proforma to prompt standardised visual acuity assessment.40
Types of visual loss
Visual loss is a broad term encompassing a range of visual impairments. Vision comprises of many elements and is not merely a measure of visual acuity and visual field; other components of vision such as contrast sensitivity and depth perception undoubtedly affect the risk of falling and of hip fractures. As the epidemiological data above suggest it is still unclear, which measure is most important. Different ophthalmic conditions such as glaucoma and age-related macular degeneration cause quite different patterns of visual loss, thus having data relating to different measures of vision is useful (Table 2 ).
Age-related macular degeneration and falls
Age-related macular degeneration (ARMD) primarily affects central and reading vision, with symptoms such as distortion and difficulty recognising faces being prominent. However, peripheral vision is unaffected, and this is probably more important for navigation. Two thirds of patients with age-related macular degeneration were found to have visuomotor and balance deficits resulting in clumsiness and an increased risk of falls.48 Older women with ARMD have been shown to have impaired balance, slower visual reaction times, and poorer vision, compared with age-matched controls. These combined to cause a greater risk of falls; a measure of fall-risk in the AMD cohort (3.20) was significantly greater than that of the non-AMD cohort (OR 1.21; P<0.001).46
A recent investigation of patients with age-related maculopathy assessed postural stability and gait to try to identify the visual factors responsible for any deficits.49 The results suggested that all visual factors but particularly reduced contrast sensitivity were associated with postural instability and changes in gait after adjustment for age, sex, self-reported physical function and cataract severity.
Studies including balance training in a more general population have shown promising results. Pooled data from three studies, with a total of 566 participants, using a programme of progressive muscle strengthening, balance retraining exercises and a walking plan, showed a reduction of the number of individuals falling over a 1-year period (pooled RR 0.80, 95% CI 0.66–0.98). The number of people sustaining an injury from a fall was also significantly reduced (pooled RR 0.67, 95% CI 0.51–0.89).50 Radvay et al48 investigated whether balance training may help patients with ARMD. A total of 16 ARMD individuals and 14 controls received balance training sessions on a postural platform, (during which there was selective inhibition or disturbance of either visual, vestibular, or somatosensory input). The impact of balance training on several visuomotor functions and reading speed were investigated, showing a significant improvement for some measures (vestibular input and fixation stability), but no effect for others (pointing accuracy and reading speed). This preliminary study is encouraging as the improvement of visuomotor and balance skills in AMD patients should reduce their risk of subsequent falls.
Glaucoma and falls
The association between visual field loss and falls is confirmed in the literature. The Salisbury Eye Evaluation assessed the role of various components of vision and the risk of falls.43 Visual acuity, contrast sensitivity, visual field, and stereoacuity were tested and visual field loss was found to be the primary vision component increasing the risk of falls, (for a 10-point loss in Humphrey visual field testing, OR 1.08; 95% CI 1.03–1.13). Recent prospective results from the Los Angeles Latino Eye study confirm an independent association with central and peripheral visual impairment and an increased risk of falls (OR 2.36; 95% CI 1.02–5.45 and OR 1.42; 95% CI 1.06–1.91, respectively).47
In a study of 54 adults, aged 65 years and older with primary open angle glaucoma, participants with greater binocular visual field loss had increased postural sway, both on firm and foam surfaces, independent of age, gender, body mass index, and physical performance levels.51 Furthermore, participants with the majority of their visual field loss in the inferior field, showed increased postural sway on the foam surface. This would be expected as the inferior field provides visual input regarding the floor surface.
The effect of binocular visual field loss on increasing the risk of falls has also been confirmed by other investigators. A multi-centre, prospective, cohort study confirmed the association between visual field loss and falls.41 Severe binocular visual field loss was significantly associated with frequent falls when adjusting for age, study site, and cognitive function (OR 1.50, 95% CI 1.11–2.02). The data also showed a trend for increasing odds of two or more falls with greater binocular visual field loss (P<0.001).
In a case–control study, patients with glaucoma and relatively mild field defects were shown to be over three times more likely to have fallen in the previous year, and over six times more likely to have been involved in one or more motor vehicle collisions in the previous 5 years;52 however, no explanation was given for this association.
The inference of these studies is that visual field loss deprives individuals of adequate visual input, decreasing postural stability as well as the risk of bumping into objects around them or misjudging surfaces, causing them to fall.
Cataracts and falls
Cataracts are the most common reversible cause of visual impairment in the elderly after refractive error. The benefit of first eye cataract surgery in reducing the risk of falls was confirmed by a randomised control trial, which compared expedited cataract surgery versus routine surgery. The median time from randomisation to expedited surgery was 27 days (1–212), and time to routine surgery was 337 days (133–485) in this study. The numbers of individuals who suffered a fall were relatively low at 4 in the expedited surgery group versus 12 in the routine group, nevertheless the results were statistically significant; rate of falling was reduced by 34% in the expedited surgery group (OR 0.66, 95% CI 0.45–0.96, P=0.03).53
The same group showed second eye cataract surgery improved vision and general status. Surgery reduced the rate of falling by 32% compared with controls, but this was not statistically significant (OR 0.68, 95% CI 0.39–1.19, P=0.18)54 The number of individuals who fell was again low in this study, and this may be a factor in the lack of statistical significance. However, it is possible that patients' activity level and behaviour may alter after surgery, thus affecting the fall-risk.
A meta-analysis suggested that patients who wait more than 6 months for cataract surgery may experience a reduced quality of life and increased rate of falls during the waiting period.55 Fewer patients who received expedited surgery fell two or more times compared with the group still awaiting surgery (18% (28/154) vs 25% (38/152), P=0.04).
Diabetes mellitus and falls
There is surprisingly little evidence relating the effects of diabetic retinopathy to falls. Patients with diabetic retinopathy have been included in various studies of falls and visual loss as part of larger groups with visual impairment;19, 41 however, this important group have not been studied separately.
Nevertheless diabetics are at increased risk of falls through several possible mechanisms. The systemic manifestations of diabetes, the effects of lower limb neuropathy and any concurrent vascular disease may affect walking, gait and the risk of falls.56 Glycaemic control itself can also affect the risk of falls.57
As well as the visual disability caused by diabetes, pan-retinal photocoagulation does affect an individual's visual field and hence increase the risk of falls, however this has not been independently investigated.
Other visual factors and falls
Various other visual components have also been linked with falls. Lord et al18 found reduced edge contrast sensitivity to be more strongly associated with falls than visual acuity and suggested that it may be more important than visual acuity in assessing the risk of falls. One hypothesis is that this measure may reflect the ability of individuals to see ground-level obstacles more accurately. Their group also found increased postural sway in older individuals with worse distance contrast sensitivity.58
Depth perception or stereopsis has also been investigated by several groups. Impaired stereopsis has been shown to be a risk factor for falls and hip fractures. A case–control study investigating hip fracture found having no depth perception was strongly associated with increased risk (OR=6.0 95% CI 3.2–11.1), as were categories of decreasing stereopsis (trend P=0.0001).29 In another study, lack of stereopsis was the strongest risk factor for multiple falls out of nine visual measures.42
Vale et al59 investigated the effect of inducing monocular blur on 11 elderly subjects, and showed gait alterations when negotiating a raised object with even small amounts of monocular blur. Monocular blur also impaired stereopsis (P<0.01), with more minor effects on high and low contrast acuity.
The role of spectacles is also important. Incorrect spectacle correction may be a reversible cause of visual loss and one that is easily fixed. The prismatic effects of the near portion of bifocal glasses may also have a role in increasing falls risk in the elderly. Elderly individuals using a single vision lens had improved precision when negotiating a raised surface than when using their regular multifocal glasses. Multifocal glasses have also been shown to affect toe clearance and risk of tripping.60 It may be that impaired distance contrast sensitivity and depth perception through the near portion of multifocal glasses is a mechanism for this effect.44
Balance relies on the co-ordination of stimuli from the visual and vestibular system, with proprioception, muscle strength and reaction time also contributing. However, with increasing age there is deterioration in function in all these inputs.11 Several studies have focused on the effect of vision on balance in trying to explain the link between vision and falls. Peripheral visual field occlusion, has been shown to worsen postural stability significantly in older adults.61 In a sample of 183 older adults, good contrast sensitivity assisted in maintaining balance and stability.62
The effect of vision on the interaction of muscle activity and movement of the lower limbs during episodes of perturbed balance has also been investigated.63 The study was in young healthy individuals, so the results may not be directly applicable to the elderly, but it showed proof of principle of the role of vision in coordination with the vestibular system. Volunteers standing on a platform with their eyes open and closed were subjected to calf muscle vibration and the muscle responses showed greater activity with their eyes closed. Thus muscle responses may be more important to maintain the balance in individuals with poor vision.
Visual loss and other sensory impairments
If visual impairment is present with other sensory impairments, such as hearing or balance problems, the relative risk of falls has been shown to be even higher. A twin study in older women with vision impairment (logMAR VA of <1.0) but no other sensory impairments had a higher, but non-significant, risk for falls compared with persons with normal vision (RR 1.5, 95% CI 0.6–4.2).45 Co-existing vision impairment and impaired balance increased the risk (RR 2.7, 95% CI 0.9–8.0), as did co-existing vision and hearing impairment (RR 4.2, 95% CI 1.5–11.3) Among persons with all three impairments, the relative risk for falls increased substantially to 29.4 (95% CI 5.8–148.3) compared with participants with good vision.
Preventive work to reduce falls
There has been considerable published work investigating methods of trying to prevent falls. The Cochrane reviews in 2005 comprehensively covered population and individual strategies for this.50 Studies relating to vision can be split into methods of risk assessment and stratification and those assessing methods of prevention. The assessment and recognition of visual problems is essential as without this, steps cannot be taken to try and rectify reversible causes of visual impairment (Table 3 ).
Previous studies have confirmed that systems in identifying visual impairment in patients suffering falls were inadequate.68 Suggestions for improvements have been made by several organisations. In 2003, the College of Optometrists and the British Geriatrics Society released an evidence-based report recommending that all people undergoing a falls assessment should be screened for visual impairment and those identified as suffering from a visual impairment should have a full eye examination.69
Surprisingly, a randomised controlled trial by Cumming et al67 in Australia found no benefit in reducing falls following a comprehensive vision and eye assessment by a study optometrist in elderly individuals (average age 80 years). Individuals had their glasses updated or were referred for further intervention, such as occupational therapy or cataract surgery. A possible explanation for the lack of reduction in falls was that, paradoxically, those individuals who received interventions to improve their vision may have increased their activity level and thus put themselves at higher risk of falling.
Another randomised controlled trial, the PROFET study, however, found a structured interdisciplinary assessment with detailed medical and occupational therapy assessment with referral to relevant services had a highly significant effect.70 At 12 months the risk of falling was significantly reduced in the intervention group (odds ratio 0.39 (95% CI 0.23–0.66)) as was the risk of recurrent falls (OR 0.33 (95% CI 0.16–0.68)) This study did not, however, include any direct intervention to improve vision.
Day et al66 compared three interventions; group-based exercise, home hazard management and vision improvement on individuals aged over 70 years and living at home. Only the group-based exercise, which consisted of weekly exercises over a 15-week period, had a significant effect in reducing the annual fall rate, though combinations of the interventions did have a greater effect. The visual intervention consisted of testing vision and referring the participant to their usual eye care provider if their vision fell below a threshold. However, the numbers receiving an intervention were very low; of 547 participants receiving the vision intervention, 287 were recommended for referral, of whom 186 had either recently visited or were about to visit their optometrist or ophthalmologist. Of the remaining 101 participants, only 26 had some form of treatment glasses (20) or surgery (6). With such a low number having treatment, it is unsurprising that the results for visual intervention were not significant.
Environmental or extrinsic factors are also important in contributing to falls risk.71 Poor lighting and objects around the home, such as loose rugs may increase the risk of falls. These factors would be of more concern in individuals with visual impairment. Contrast sensitivity diminishes in the elderly, and may be further compromised by concurrent ocular disease. Thus assessment of the home circumstances of patients including the lighting would be another avenue for intervention in reducing falls risk.
The benefit of home interventions and assessments have been proven in three studies that confirmed that home hazard assessment and modification resulted in fewer falls.50 However, further investigation of its clinical benefit, economic viability and effectiveness is awaited, as well as trials between those with and without visual problems.
Optimising public spaces may be a way of reducing falls risk. The metro in Washington DC have tried to optimise lighting to some degree, and also added visual contrast and tactile contrast to help delineate surfaces and drop-offs.72 Effective use of luminance and colour contrast should be used to help visually impaired individuals interact with the environment.73
The effectiveness of a programme of muscle strengthening and balance retraining, individually prescribed at home by a trained health professional has been confirmed;74 however, the interaction with the visual system remains unclear. Further results from studies investigating strategies aiming to improve balance and the co-ordination of the visual and vestibular systems, will be helpful in clarifying whether they may have a greater role in the future.
Conclusion
The association between visual loss and falls would seem to be intuitive. However, it has remained a relatively understudied phenomenon until the last two decades, over which time the number of studies addressing this topic has rapidly increased.
Visual impairment encompasses a range of defects in different components of vision which may increase the risk of falls. Falls have significant implications at the population level and at an individual level due to the physical effects of injury, effects on the mental health of the patient and future mobility as well as mortality. Assessment to identify patients at risk and subsequently managing risk factors are essential in trying to lessen the impact of this problem. This is particularly important as many causes of visual impairment in older people are reversible.
Great strides have been taken in improving the assessment and management of risk factors regarding falls and visual impairment; however, there are still many areas that require further study. The relative contribution of different visual parameters has been studied but there is still much to be clarified. Knowing which visual parameter most accurately reflects falls risk in a given population will help optimise the assessment of individuals for primary or secondary prevention of falls. The effects in different ocular conditions needs further clarification, as they affect vision in different ways. Furthermore, investigations are required in various populations with different baseline mobility, social situation, ethnicity and co-morbidity. Better understanding of the risk factors will help improve targeting of possible interventions.
The end point of research into falls would be to develop an efficacious and cost-effective intervention. Even an intervention that is in widespread use, such as multi-disciplinary team assessment has been shown to be effective in some studies,66 but not in others.65, 67 As discussed earlier, interventions may affect subsequent behaviour or activity level in an individual, possibly confounding the results, and ideally this needs to be controlled for.
Regarding vision and falls, cataract surgery is one of the best studied interventions. A cost analysis showed an incremental cost–utility ratio of £35 704 for cataract surgery, above the generally accepted UK threshold per Quality Associated Life Year (QALY) of £30 000. However, in the same study the cost per QALY was calculated to be £13 172, when calculated for lifetime savings as opposed to over the time of the study.75 Similar analyses of other promising interventions will aid assessment of their potential efficacy.
References
Adelhafiz AH, Austin CA . Visual factors should be assessed in older people presenting with falls or hip fracture. Age Ageing 2003; 32: 26–30.
Scuffham P, Chaplin S, Legood R . Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health 2003; 57: 740–744.
Lawrence TM, White CT, Wrenn R, Moran CG . The current hospital costs of treating hip fractures. Injury 2005; 36: 88–91; discussion 92.
Department of Health. National Service Framework for Older People. DoH: London, 2001.
Moorin RE, Hendrie D . The epidemiology and cost of falls requiring hospitalisation in children in Western Australia: a study using linked administrative data. Accid Anal Prev 2008; 40: 216–222.
Talbot LA, Musiol RJ, Witham EK, Metter EJ . Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005; 5: 86.
Tideiksaar R . Reducing the risk of falls and injury in older persons: contribution of a falls and immobility clinic. In: LaFont C et al., (eds). Falls, Gait and Balance Disorders in the Elderly: From Successful Aging to Frailty. Springer Publishing Company: New York, 1996, pp 163–182.
Rubenstein LZ . Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006; 35 (Suppl 2): ii37–ii41.
Evans JR, Fletcher AE, Wormald RP, Ng ES, Stirling S, Smeeth L, Breeze E et al. Prevalence of visual impairment in people aged 75 years and older in Britain: results from the MRC trial of assessment and management of older people in the community. Br J Ophthalmol 2002; 86: 795–800.
Scott JC . Osteoporosis and hip fractures. Rheum Dis Clin North Am 1990; 16: 717–740.
Sturnieks DL, St George R, Lord SR . Balance disorders in the elderly. Neurophysiol Clin 2008; 38: 467–478.
Manchester D . Visual, vestibular and somatosensory contributions to balance control in the older adult. J Gerontology 1989; 44: 118–127.
Bueno-Cavanillas A, Padilla-Ruiz F, Jiménez-Moleón JJ, Peinado-Alonso CA, Gálvez-Vargas R . Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol 2000; 16: 849–859.
Masud T, Morris RO . Epidemiology of falls. Age Ageing 2001; 30 (Suppl 4): 3–7.
Campbell AJ, Borrie MJ, Spears GF . Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol 1989; 44: M112–M117.
Tinetti ME, Speechley M, Ginter SF . Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701–1707.
Chu LW, Chi I, Chiu AY . Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore 2005; 34: 60–72.
Lord SR . Visual risk factors for falls in older people. Age Ageing 2006; 35 (Suppl 2): ii42–ii45.
Ivers RQ, Cumming RG, Mitchell P, Attebo K . Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc 1998; 46: 58–64.
Coleman AL, Stone K, Ewing SK, Nevitt M, Cummings S, Cauley JA et al. Higher risk of multiple falls among elderly women who lose visual acuity. Ophthalmology 2004; 111: 857–862.
De Boer MR, Pluijm SM, Lips P, Moll AC, Völker-Dieben HJ, Deeg DJ et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res 2004; 19: 1539–1547.
Yu PL, Qin ZH, Shi J, Zhang J, Xin MZ, Wu ZL et al. Prevalence and related factors of falls in an urban community of Beijing. Biomed Environ Sci 2009; 22 (3): 179–187.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Ann Intern Med 2009; 169 (21): 1952–1960.
Nevitt M, Cummings S, Kidd S, Black D . Risk factors for recurrent non-syncopal falls. JAMA 1989; 261: 2663–2668.
Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF . A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol 2002; 55: 1088–1094.
Iglesias CP, Manca A, Torgerson DJ . The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int 2008; 20 (6): 869–878.
Keene GS, Parker MJ, Pryor GA . Mortality and morbidity after hip fractures. BMJ 1993; 307: 1248.
Speechley M, Tinetti M . Falls and injuries in frail and vigorous community elderly persons. J Am Geriatr Soc 1991; 39: 46–52.
Ivers RQ, Norton R, Cumming RG, Butler M, Campbell AJ . Visual impairment and hip fracture. Am J Epidemiol 2000; 152: 663–669.
March LM, Chamberlain AC, Cameron ID, Cumming RG, Brnabic AJ, Finnegan TP . et al. How best to fix a broken hip. Fractured Neck of Femur Health Outcomes Project Team. Med J Aust 1999; 170: 489–494.
Goldacre MJ, Roberts SE, Yeates D . Mortality after admission to hospital with fractured neck of femur: database study. BMJ 2002; 325 (7369): 868–869.
Evitt CP, Quigley PA . Fear of falling in older adults: a guide to its prevalence, risk factors, and consequences. Rehabil Nurs 2004; 29: 207–210.
Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE . Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008; 37: 19–24.
Iglesias CP, Manca A, Torgerson DJ . The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int 2009; 20: 869–878.
Wormald RP, Wright LA, Courtney P, Beaumont B, Haines AP . Visual Problems in the elderly population and implications for services. BMJ 1992; 2304 (6836): 1226–1229.
Squirrell DM, Kenny J, Mawer N, Gupta M, West J, Currie ZI et al. Screening for visual impairment in elderly patients with hip fracture: validating a simple bedside test. Eye 2005; 19: 55–59.
Klein BE, Moss SE, Klein R, Lee KE, Cruickshanks KJ . Associations of visual function with physical outcomes and limitations 5 years later in an older population: the Beaver Dam eye study. Ophthalmology 2003; 11: 644–650.
National Institute for Health and Clinical Excellence. Falls: the Assessment and Prevention of Falls in Older People. Clinical guideline 21, NICE, 2004.
British Geriatric Society. Falls. Best Practice Guide 4.5, BGS 2007.
Royal College of Physicians. National Audit of the Organisation of Services for Falls and Bone Health of Older People. National Falls and Bone Health Audit Report, RCP, March 2009.
Coleman AL, Cummings SR, Yu F, Kodjebacheva G, Ensrud KE, Gutierrez P, et al., Study Group of Osteoporotic Fractures. Binocular visual-field loss increases the risk of future falls in older white women. J Am Geriatr Soc 2007; 55: 357–364.
Lord SR, Dayhew J . Visual risk factors for falls in older people. J Am Geriatr Soc 2001; 49: 508–515.
Freeman EE, Muñoz B, Rubin G, West SK . Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci 2007; 48: 4445–4450.
Lord SR, Dayhew J, Howland A . Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc 2002; 50: 1760–1766.
Kulmala J, Viljanen A, Sipilä S, Pajala S, Pärssinen O, Kauppinen M et al. Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing 2009; 38 (2): 162–167.
Szabo SM, Janssen PA, Khan K, Potter MJ, Lord SR . Older women with age-related macular degeneration have a greater risk of falls: a physiological profile assessment study. J Am Geriatr Soc 2008; 56: 800–807.
Patino CM, McKean-Cowdin R, Azen SP, Allison JC, Choudhury F, Varma R et al. Central and peripheral visual impairment and the risk of falls and falls with injury. Ophthalmology 2010; 117: 199–206.
Radvay X, Duhoux S, Koenig-Supiot F, Vital-Durand F . Balance training and visual rehabilitation of age-related macular degeneration patients. J Vestib Res 2007; 17: 183–193.
Wood JM, Lacherez PF, Black AA, Cole MH, Boon MY, Kerr GK . Postural stability and gait among older adults with age-related maculopathy. Invest Ophthalmol Vis Sci 2009; 50: 482–487.
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH . Interventions for preventing falls in elderly people. Cochrane Database Syst Rev 2003 Issue no. 4. Article no. CD000340.
Black AA, Wood JM, Lovie-Kitchin JE, Newman BM . Visual impairment and postural sway among older adults with glaucoma. Optom Vis Sci 2008; 85: 489–497.
Haymes SA, Leblanc RP, Nicolela MT, Chiasson LA, Chauhan BC . Risk of falls and motor vehicle collisions in glaucoma. Invest Ophthalmol Vis Sci 2007; 48: 1149–1155.
Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T . Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol 2005; 89: 53–59.
Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T . Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing 2006; 35: 66–71.
Hodge W, Horsley T, Albiani D, Baryla J, Belliveau M, Buhrmann R et al. The consequences of waiting for cataract surgery: a systematic review. CMAJ 2007; 176: 1285–1290.
Paul L, Ellis BM, Leese GP, McFadyen AK, McMurray B . The effect of a cognitive or motor task on gait parameters of diabetic patients, with and without neuropathy. Diabet Med 2009; 26: 234–239.
Nelson JM, Dufraux K, Cook PF . The relationship between glycemic control and falls in older adults. Tighter control increases falls. J Am Geriatr Soc 2007; 55: 2041–2044.
Lord SR, Menz HB . Visual contributions to postural stability in older adults. Gerontology 2000; 46: 306–310.
Vale A, Buckley JG, Elliott DB . Gait alterations negotiating a raised surface induced by monocular blur. Optom Vis Sci 2008; 85: 1128–1134.
Johnson L, Buckley JG, Scally AJ, Elliott DB . Multifocal spectacles increase variability in toe clearance and risk of tripping in the elderly. Invest Ophthalmol Vis Sci 2007; 48: 1466–1471.
Lichtenstein MJ, Shields SL, Shiavi RG, Burger MC . Clinical determinants of biomechanics platform measure of balance in aged women. J Am Geriatr Soc 1998; 36: 996–1002.
Turano K, Rubin GS, Herdman SJ . Visual stabilisation of posture in the elderly: fallers vs. nonfallers. Visual Science 1994; 71: 761–769.
Patel M, Gomez S, Lush D, Fransson PA . Adaptation and vision change the relationship between muscle activity of the lower limbs and body movement during human balance perturbations. Clin Neurophysiol 2009; 120: 601–609.
Brannan S, Dewar C, Sen J, Clarke D, Marshall T, Murray PI . A prospective study of the rate of falls before and after cataract surgery. Br J Ophthal 2003; 57: 860–862.
Lord SR, Tiedemann A, Chapman K, Munro B, Murray SM, Gerontology M et al. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. J Am Geriatr Soc 2005; 53: 1296–1304.
Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S . Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002; 325 (7356): 128–131.
Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 2007; 55: 175–181.
Wormald RPL, Wright LA, Courtney P, Beaumont B, Haines AP . Visual problems in the elderly population and implications for services. BMJ 1992; 304: 1226–1229.
College of Optometrists and British Geriatric Society. The importance of vision in preventing falls. Best Practice Guide 4.7, BGS, 2003.
Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C . Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999; 353 (9147): 93–97.
Feldman F, Chaudhury H . Falls and the physical environment: a review and a new multifactorial falls-risk conceptual framework. Can J Occup Ther 2008; 75: 82–95.
Freeman PB . Steady as she goes. Editorial perspective. J Optometry 2009; 80: 161–162.
Project Rainbow. Colour selection and the visually impaired: a design guide for building refurbishment. Second Advisory Paper, University of Reading, 1996.
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM . Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing 1999; 28: 513–518.
Sach TH, Foss AJ, Gregson RM, Zaman A, Osborn F, Masud T et al. Falls and health status in elderly women following first eye cataract surgery: an economic evaluation conducted alongside a randomised controlled trial. Br J Ophthalmol 2007; 91: 1675–1679.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dhital, A., Pey, T. & Stanford, M. Visual loss and falls: a review. Eye 24, 1437–1446 (2010). https://doi.org/10.1038/eye.2010.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.60
Keywords
This article is cited by
-
Typologies of dependency, household characteristics, and disparity in formal and informal care use: analysis of community-dwelling long-term care insurance claimants in an urban municipality of China
International Journal for Equity in Health (2023)
-
Effect of home-based exercise on falls in community-dwelling older adults: an umbrella review
Sport Sciences for Health (2023)
-
Quality of life in people with visual impairment compared with the general population
Journal of Public Health (2023)
-
Visual impairment and ten-year mortality: the Liwan Eye Study
Eye (2021)
-
Smoking, urinary cotinine levels and incidence of visual impairment
Scientific Reports (2021)