Abstract
Background
Congenital cataract significantly impairs visual development. Although treatable, a good visual outcome is difficult to achieve, requiring prompt lensectomy and prolonged visual rehabilitation.
Purpose
The aim of this study was to investigate whether useable visual acuity (VA) is a realistic goal in these patients.
Methods
A retrospective case review from a tertiary referral centre was performed. This study included children with unilateral congenital cataract who underwent cataract surgery with posterior capsulectomy and anterior vitrectomy.
Results
A total of 62 patients were identified. Of them, 32% of aphakic eyes had a final VA of 0.6 LogMAR or better (average 0.34±0.17). The average age at the time of surgery was 5.0±4.1 weeks. The remaining 68% had vision that was less than 0.6, with 27% having vision of <1.00. The group with vision less than 0.6 (68%) had an average age of 9.7±6.5 weeks at the time of surgery. One case (1.6%) achieved a VA of 0.0 and also had demonstrable stereoacuity (110 arc s). Manifest strabismus was present in 85% of cases. Glaucoma developed in 19% of patients and 31% discontinued the occlusion regime before the age of 4 years. In most of these cases, occlusion was ceased by the age of 2 years when testing revealed dense amblyopia in the aphakic eye even if good compliance had previously been achieved. In many cases, this coincided with the child becoming noncompliant with occlusion.
Conclusions
More than two-thirds of children in our cohort did not develop acuity better than 0.6 LogMAR in their aphakic eye.
Similar content being viewed by others
Introduction
Cataract in the infant eye significantly impairs visual development by reducing the clarity of the retinal image. Although treatable with prompt surgical removal of the lens and prolonged visual rehabilitation, a good visual outcome is still difficult to achieve.
Almost 3 in every 10 000 children born in the United Kingdom each year have congenital or infantile cataract diagnosed in their first year, with one-third of them having unilateral cataract.1 This equates to approximately 72 patients per year in the United Kingdom having unilateral congenital cataract.2
Overall, 92% of patients with unilateral congenital cataract do not have any associated systemic pathology.3 However, 51% of unilateral cataracts are associated with ocular abnormalities compared with 12% of bilateral congenital cataracts.3
IOL implantation in an infant's eye is controversial.4, 5, 6, 7, 8, 9, 10 Monocular aphakes are usually corrected using contact lens, as spectacles are associated with a high degree of aniseikonia and are poorly tolerated cosmetically.
Once the refractive error has been corrected, occlusion therapy must be initiated to stimulate visual development in the aphakic eye.11 Occlusion therapy may need to be continued for at least 6 years, which can be difficult for the whole family. Realistic expectations need to be provided at the onset, and occlusion therapy should be ceased in patients with poor acuity levels, who do not respond to patching.12
Many studies have addressed the issue of occlusion therapy in unilateral aphakes, and suggested probable outcomes with varying results.10, 13, 14, 15, 16, 17, 18, 19, 20
Small-scale studies have reported good visual results, suggesting that a visual acuity (VA) of 0.5 or better is achievable; Pratt-Johnson and Tillson19 reported on four selected cases, all of whom achieved a VA of 0.3 or better. Gregg and Parks21 reported one patient who achieved a VA of 20/25 and 50 s of arc stereopsis in a patient who was operated upon at 1 day of age Wright et al22 reported that 23% of their 13 patients showed sensory fusion.
Dewsberry's group of 24 patients, all of whom had lensectomy after 3 weeks of age, reported 46% with a vision of 0.6 or better.15 Those patients who were operated on at less than 8 weeks of age had poorer visual outcomes, which conflicts with the results of Birch and co-workers13 who found that treatment before 6 weeks of age maximizes the opportunity for normal development of the aphakic eye,13 and that 36.8% of children had a vision better than 0.60.16 However, Dewsberry's group did not differentiate between infantile and congenital cataracts, which confuses the outcomes.
The findings of previous studies give conflicting evidence for final VA prognosis for any patient with a unilateral cataract.
This study aims to improve the quality of information available to clinicians and to patients and their families. Although we do not dismiss the achievement of a good field of vision, as well as that of improved appreciation of blur, colour, and motion, all of which may also be of benefit, VA is measurable and easily communicated. However, the risks of aphakic glaucoma, reported to be 32% of cases,23 and costs in terms of quality of early life during prolonged patching treatment need to be considered, as does the risk of reduced recognition acuity (iatrogenic amblyopia) of the fellow eye, which may be caused by prolonged occlusion therapy,24 although a slightly reduced VA in the fellow eye has also been recorded irrespective of patching duration.25
Materials and Methods
A retrospective review of case records from a tertiary referral centre was carried out for patients who had undergone surgery for unilateral congenital cataract or PFV since 1990. These patients had all worn contact lens for all or part of their follow-up. No eye had secondary IOL implantation. A total of 130 patients were identified.
Patients were excluded if they had bilateral cataract, traumatic cataract, retinal abnormality, cortical blindness, or were uniocular. Patients were also excluded if there was less than 3 years of follow-up or when the cataract diagnosis or lensectomy was carried when the patient was more than 1 year of age. Patients whose primary indication for lens removal was to reduce the risk of pupil-block glaucoma were not excluded if they opted to explore potential vision even if dense amblyopia was predicted.
Visual acuity was recorded using a standard LogMAR chart at 4 m, with the patient wearing optimal refractive correction. Orthoptic, optometric, and ophthalmic examinations were performed at every clinic visit. Follow-up schedule was decided on an individually tailored basis.
Visual rehabilitation was achieved through the use of daily-wear contact lens; if use of contact lens was not possible, spectacles were used. Soft high-water-content lens (72%) was the lens of first choice, although this was changed to rigid gas permeable or silicone rubber contact lens if fitting problems occurred. The initial contact lens fitting was carried out as soon as possible after surgery, usually within 5–14 days of cataract extraction, and spectacles were issued earlier on a temporary basis in many instances or permanently if contact lens correction could not be commenced within 14 days.
Refractive error was determined by retinoscopy at each appointment, at least four times a year over the follow-up period.
The contact lens power was overcorrected by +2.00 to +3.00 DS for the first 2–3 years to provide a focusing distance of 1/2 to 1/3 m. This was altered to distance correction, and a reading or bifocal spectacle lens was prescribed for near vision once the child reached school-going age.
Occlusion therapy was initiated as soon as the aphakic eye received a refractive correction. This was prescribed at a rate of 1 h per day per month until the age of 6 months; thereafter, a maintenance level of 50% of waking hours was prescribed.11 The maintenance level was then adjusted according to VA measurements,11 but the majority of patients received patching for 50% of their waking hours after 6 months of age.
Data were collected with regard to primary diagnosis, age at cataract removal, compliance with occlusion regime, final VA in aphakic eye (best corrected), final VA in phakic eye, presence of stereopsis/binocularity, need for any further operations, and need for any further medical attention.
Analysis of data was performed, assessing the proportion of patients with useable vision (which was set at a LogMAR acuity of 0.6 or better16) compared with those with a vision of less than 0.6, to give a prognosis of outcome. Birch et al16 consider a ‘spare’ eye with a VA of at least 0.6 to be a worthwhile aim; we will take this as our marker of successful outcome in this study. The final acuity achieved was related to the age of cataract extraction.
Results
A total of 73 patients were identified within the inclusion criteria, 7 sets of data were unobtainable and 4 patients were lost to follow-up, leaving 62 eyes included. Of these, 13 had PFV and 7 were recorded as microcornea (horizontal corneal diameter of less than 10 mm). The age at the time of recording the final VA was 7.99±2.96 years.
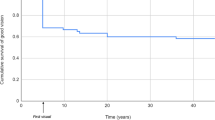
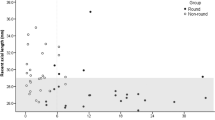
In all, 32% (20/62) of eyes had a final VA of 0.6 LogMAR or better (average 0.34±0.17). The average age at surgery was 5.0±4.1 weeks. The remaining 68% had a VA of less than 0.6; the average age at surgery was 9.7±6.5 weeks.
Of the 62 eyes, 36 had surgery at less than 8 weeks of age and 15 (42%) of these eyes achieved a final VA of 0.6 LogMAR or better. Of these 62 eyes, 46 underwent surgery at the age of 12 weeks or less, and 16 (35%) achieved a final VA of 0.6 LogMAR or better. A total of 27% (17/62) had a vision of less than 1.00 LogMAR, with an average age of 9.9±7.0 weeks at the time of surgery (see Table 1 for comparison of age of lensectomy with final VA achieved).
Four eyes (6.3%) had a vision of 0.2 or better. One eye (1.6%) achieved a VA of 0.0 and the child showed 110 arc s of stereoacuity. This patient had surgery at the age of 2 weeks. Three eyes had surgery before 1 week; two eyes had a VA of 0.22 and one eye had a VA of 0.36.
The 49 cases with cataract alone (no PFV) had an average VA of 1.24 (SD±0.72), with an average age at the time of surgery of 8.70 (±6.56) weeks.
Of the 13 eyes with PFV, the final VA was 1.16 (±0.77) and the average age of lensectomy was 5.9 (±4.4) weeks.
Seven eyes were reported to be microcornea, these achieved a final VA of 1.60±0.43. The average age at the time of surgery was 9.8 (±3.3) weeks.
There were three eyes that had microcornea and PFV. They achieved an average final VA of 1.41 (±0.68). The average age at the time of surgery in these eyes was 8.7 (±3.1) weeks.
Strabismus was reported in 85% (53/62) of cases. Glaucoma occurred in 19% (12/62) of eyes, with 4 requiring surgery and the remainder receiving topical treatment.
Occlusion therapy was abandoned in 31% (19/62) before the age of 4 as it was deemed too distressing for the child, or the amblyopia was deemed to be too dense to be recoverable. The average age of these children at the time of lensectomy was 8.08 (±4.48) weeks. The average VA of the 62 phakic eyes was 0.02±0.14.
Discussion
Previous studies16, 25, 26, 27, 28, 29 have assessed visual outcome in children after congenital cataract extraction (see Tables 2 and 3 for comparison of outcomes with results from this study).
This study found that an earlier age of surgery correlated with a better chance of good visual outcome, which is in agreement with most previous studies. Birch and Stager13 reported on 38 patients and found a VA of 0.60 or better in 53% of cases, with the best outcomes in those operated before 2 months of age. Birch et al17 found that VA development was within normal range for the first year of life, but then lagged behind normal development during years 2–4.17 Lambert et al10 reported a mean grating VA of 0.87±0.31 in the affected eye in 13 subjects who had had unilateral cataract extraction before 7 months of age.10
In 1996, Birch and Stager30 performed statistical analysis of 45 cases and identified that surgical intervention before 6 weeks of age maximized the potential for good visual outcome.
Although operating at an early age does increase the chance of achieving a good vision, the results varied. The potential for achieving 0.0 LogMAR acuity in the aphakic eye is less (1.6%). Being operated upon at a young age does involve a risk of complications. The risk of glaucoma is highest with cataract extraction in the first 4 weeks,31 with about 50% developing glaucoma (19% of all cases in this study). There is also the risk of developing secondary membrane formation (10%)32 and retinal detachment (1%).32
In approximately a third of patients, occlusion therapy was abandoned before the age of 4 years because of a poor visual outcome. It is important to consider this fact, as there is often a significant amount of stress and upset for the child, parents, and other family members while attempting to comply with an occlusion regime.
The high incidence of strabismus is similar to that observed in most other studies, including the study by Lambert et al,10 who recorded manifest strabismus in 92% of patients.10, 15, 16, 33, 34, 35
This can have further issues, as the child may require further surgery to improve cosmesis. However, there is also a significant risk of strabismus without lensectomy. Approximately 20% of eyes develop glaucoma and require life-long medical therapy or surgical intervention. Postoperative care of unilateral cataract patients also involves other significant issues; Maurer et al18 found a reduced threshold of sensitivity in the nasal visual field when compared with the temporal visual field.
The risk of loss of vision in the phakic eye should also be considered when considering treatment for unilateral cataract. Rahi et al36 found that the projected risk of loss of vision in the non-amblyopic eye was 1.2%, with 65% of people of working age being affected.
Possible bias in this study includes a high proportion of children with complicated cataract and PFV. This may be because of the specialist nature of the study centre. Other studies may not reflect the full extent of visual loss, as more complicated cases are often transferred to tertiary referral centres for treatment and ongoing care. This may be a source of difference and may counteract any bias from a smaller centre that may have simpler cases and that may report better prognosis. This fact should be borne in mind when viewing other studies, and all reports should be viewed together to reflect the national outcome in the context of a small population.
Cost implications of cataract surgery for congenital cataract must also be considered, as well as the social costs to families. Further investigation of this cohort would be beneficial to assess the cost/benefit ratio. This would be beneficial to the health service provider, as treatment for eyes with a poor predicted outcome needs to be critically evaluated.
Conclusion
Two-thirds of children operated for unilateral congenital cataract do not develop acuity better than 0.6 LogMAR in their aphakic eye. Very early surgery improves the chance of good vision but the majority will have a poor VA outcome. The majority will be strabismic, and there is a high risk of glaucoma.

References
Rahi J, Dezateaux C . Measuring and interpreting the incidence of congential ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci 2001; 42: 1444–1448.
http://www.statistics.gov.uk/cci/nugget.asp?id=951 accessed: 27 September 2006.
Rahi J, Dezateaux C . Congenital and infantile cataract in the United Kingdom: underlying or associated factors. Invest Ophthalmol Vis Sci 2000; 41: 2108–2114.
Greenwald MJ, Glaser SR . Visual outcomes after surgery for unilateral cataract in children more than two years old: posterior chamber implantation versus contact lens correction of aphakia. J AAPOS 1998; 2,3: 168–176.
Lambert SR, Buckley EG, Plager DA, Medow NB, Wilson ME . Unilateral intraocular lens implantation during the first six months of life. J AAPOS 1999; 3 (6): 344–349.
Wright KW . Paediatric cataracts. Curr Opin Ophthalmol 1997; 8 (1): 50–55.
Asrani S, Freedman S, Hasselblad V, Buckley EG, Egbert J, Dahan E et al. Does primary intraocular lens implantation prevent ‘aphakic’ glaucoma in children? J AAPOS 2000; 4 (1): 33–39.
O’Keefe M, Fenton S, Lanigan B . Visual outcomes and complications of posterior chamber intraocular lens implantation in the first year of life. J Cataract Refr Surg 2001; 27 (12): 2006–2011.
Moore BD . Changes in the aphakic refraction of children with unilateral congenital cataracts. J Pediat Ophth Strab 1989; 26 (6): 290–295.
Lambert SR, Lynn M, Drews-Botsch C, Loupe D, Plager D, Medow NB et al. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. J AAPOS 2001; 5 (2): 70–75.
Lloyd IC, Dowler JG, Kriss A, Speedwell L, Thompson DA, Russell-Eggitt I et al. Modulation of amblyopia therapy following early surgery for unilateral congenital cataracts. Br J Ophthalmol 1995; 79 (9): 802–806.
Dixon-Woods M, Awan M, Gottlob I . Why is compliance with occlusion therapy for amblyopia so hard? A qualitative study. Arch Dis Child 2006; 91: 491–494.
Birch EE, Stager DR . Prevalence of good visual acuity following surgery for congenital unilateral cataract. Arch Ophthalmol 1988; 106: 40–43.
Yamamoto M, Dogru M, Nakamura M, Shirabe H, Tsukahahra Y, Sekiya Y . Visual function following congenital cataract surgery. Jpn J Ophthalmol 1998; 42: 411–416.
Dewsberry C . Factors that influence the outcome in cases of infantile unilateral cataract. Br Ir Orthopt J 2005; 2: 32–39.
Birch EE, Swanson WH, Stager DR, Woody M, Everett M . Outcome after very early treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci 1993; 34: 3687–3699.
Birch EE, Stager DR, Wright WW . Grating acuity development after early surgery for congenital unilateral cataract. Arch Ophthalmol 1986; 104: 1783–1787.
Maurer D, Lewis TL, Brent HP . Peripheral vision and optokinetic nystagmus in children with unilateral congenital cataract. Behav Brain Res 1983; 10: 151–161.
Pratt-Johnson JA, Tillson G . Unilateral congenital cataract: binocular status after treatment. J Pediatr Ophth Strab 1989; 26 (2): 72–75.
Beller R, Hoyt CS, Marg E, Odom JV . Good visual function after neonatal surgery for congenital monocular cataracts. Am J Ophthalmol 1981; 91 (5): 559–565.
Gregg FM, Parks MM . Stereopsis after congenital monocular cataract extraction. Am J Ophthalmol 1992; 114 (3): 314–317.
Wright KW, Matsumoto E, Edelman PM . Binocular fusion and stereopsis associated with early surgery for monocular congenital cataracts. Arch Ophthalmol 1992; 110 (11): 1607–1609.
Johnson CP, Keech RV . Prevalence of glaucoma after surgery for PHPV and infantile cataracts. J Pediatr Ophth Strab 1996; 33 (1): 14–17.
Thompson DA, Møller H, Russell-Eggitt I, Kriss A . Visual acuity in unilateral cataract. Br J Ophthalmol 1996; 80: 794–798.
Lewis TL, Maurer D, Tytla ME, Bowering ER, Brent HP . Vision in the good eye of children treated for unilateral congenital cataract. Ophthalmology 1992; 7: 1013–1017.
Robb RM, Mayer JD, Moore BD . Results of early treatment of unilateral congenital cataracts. J Pediatr Ophth Strab 1987; 24 (4): 178–181.
Birch EE, Stager D, Leffler J, Weakley D . Early treatment of congenital unilateral cataract minimizes unequal competition. Invest Ophthalmol Vis Sci 1998; 39 (9): 1560–1566.
Lundvall A, Kugelberg U . Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scan 2002; 80: 588–592.
Drummond GT, Scott WE, Keech RV . Management of monocular congenital cataracts. Arch Ophthalmol 1989; 107 (1): 45–51.
Birch EE, Stager DR . The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci 1996; 37 (8): 1532–1538.
Vishwanath M, Cheong-Leen R, Taylor D, Russell-Eggitt I, Rahi J . Is early surgery for congenital cataract a risk factor for glaucoma? Br J Ophthalmol. 2004; 88 (7): 905–910.
Keech RV, Tongue AC, Scott WE . Complications after surgery for congenital and infantile cataracts. Am J Ophthalmol 1989; 108 (2): 136–141.
Lesueur LC, Arné JL, Chapotot EC, Thouvenin D, Malecaze F . Visual outcomes after paediatric cataract surgery: is age a major factor? Br J Ophthalmol 1998; 82: 1022–1025.
Parks MM, Johnson DA, Reed GW . Long term visual results and complications in children with aphakia. Ophthalmology 1993; 100 (6): 826–840.
Cheng KP, Hiles DA, Biglan AW, Pettepiece MC . Visual results after early surgical treatment of unilateral congenital cataracts. Ophthalmology 1991; 98 (6): 903–910.
Rahi J, Logan S, Timms C, Russell-Eggitt I, Taylor D . Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population based study. Lancet 2002; 360 (9333): 597–602.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Allen, R., Speedwell, L. & Russell-Eggitt, I. Long-term visual outcome after extraction of unilateral congenital cataracts. Eye 24, 1263–1267 (2010). https://doi.org/10.1038/eye.2009.295
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.295
Keywords
This article is cited by
-
Outcomes of the infantile cataract surgery: case series with a 5-year follow-up
International Ophthalmology (2022)
-
Cataract management in children: a review of the literature and current practice across five large UK centres
Eye (2020)
-
Advances in the management of the surgical complications for congenital cataract
Frontiers of Medicine (2012)