Abstract
Purpose
To compare the in vitroantimicrobial susceptibilities of Gram-positive cocci isolated from the ocular infections to the second and fourth generation fluoroquinolones at a tertiary eye care centre in south India.
Methods
A retrospective review of microbiology records at LV Prasad eye institute, Hyderabad, India, identified 787 Gram-positive cocci isolated from different ocular infections between January 2005 to May 2008.The isolates were identified using culture characteristics and biochemical tests. In vitroantibiotic susceptibility of the isolates was determined by using Kirby–Bauer disc diffusion method. We analysed the susceptibility data of ciprofloxacin, ofloxacin, gatifloxacin, and moxifloxacin.
Results
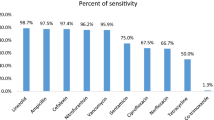
Out of 787 isolates, 147 (18.7%) were Staphylococcus aureus, 279 (35.2%) were coagulase-negative Staphylococci, 357 (45.4%) were Streptococcus pneumoniae,and 4 (0.4%) were other Streptococcus species. Of the four quinolones, susceptibility to gatifloxacin was highest (85.6%) followed by ofloxacin (65.6%), moxifloxacin (63.9%), and ciprofloxacin (60.5%). In all, 33 (4.2%) of 787 isolates were resistant to all the four fluoroquinoles. S. aureusand coagulase-negative Staphylococcus isolates that were resistant to ciprofloxacin and ofloxacin were most susceptible to gatifloxacin. S. pneumoniaewere more susceptible to gatifloxacin, ofloxacin, and ciprofloxacin than moxifloxacin.
Conclusions
In our institute, we observed that gatifloxacin is more potent than moxifloxacin against Gram-positive cocci isolated from ocular infections.
Similar content being viewed by others
Introduction
In 1962, the first quinolone, nalidixic acid was introduced. Nalidixic acid has moderate Gram-positive coverage and minimal systemic distribution.1 The structural modifications of quinolones have resulted in the development of the second, third, and fourth generation quinoles.2 The second generation quinolones (ciprofloxacin and ofloxacin) have expanded Gram-negative coverage, but limited Gram-positive coverage.1 Ciprofloxacin was approved for use as topical therapy for bacterial corneal ulcers in 1990.1 Ofloxacin, another second generation quinolone, was approved for treatment of corneal ulcers in 1996.1 In the late 1990s, several studies showed excellent efficacy of the second generation fluoroquinolones in treating bacterial keratitis and conjunctivitis.3, 4, 5, 6 This resulted in widespread use of these molecules as monotherapy in treatment of various ocular infections. Development of the third generation quinolones (levofloxacin) improved Gram-positive coverage while retaining Gram-negative activity. Levofloxacin solution was approved for ophthalmic use in the year 2000.1
Around the beginning of the 20th century, a number of studies reported emerging resistance to the second and third generation quinolones, primarily among Gram-positive ocular isolates.7, 8, 9 The fourth generation quinolones have been introduced to ophthalmology to counteract this resistance. The fourth generation quinolones (gatifloxacin and moxifloxacin) have improved Gram-positive coverage and retained Gram-negative activity.1 Minimum inhibitory concentrations of the fourth generation fluoroquinolones suggests that the fourth generation fluoroquinolones are more effective than the second and third generation quinolones against Gram-positive bacteria, including the second and third generation fluoroquinolone resistant Staphylococcus species isolated from endophthalmitis and keratitis cases.10, 11 Mather et al11 suggested that among the fourth generation quinolones, moxifloxacin is more potent than gatifloxacin for Gram-positive bacteria, and both are equally potent towards Gram-negative bacteria.
In this in vitro study, the susceptibility of Gram-positive cocci isolated from various ocular infections were tested against the fourth generation fluoroquinolones, and the results were compared with the second generation fluoroquinolones.
Materials and methods
A retrospective review of microbiology records at LV Prasad Eye Institute, Hyderabad, India, identified 787 Gram-positive cocci isolated from different ocular infections between January 2005 and May 2008. The organisms were identified by conventional biochemical tests and by using Mini API (bioMérieux, France).
Antibiotic susceptibility of the isolates was determined by using Kirby–Bauer disc diffusion method. Antibiotic discs were obtained from Hi media, Mumbai, India, and always tested for their potency once in 15 days and also as and when a new batch of disc is introduced in to the laboratory using standard ATCC (American Type Culture Collection) bacteria (S. aureus-25923, P. aeruginosa-27853, and Escherichia coli-25922) as a general quality control laboratory procedure.
Antibiotic susceptibility of Staphylococcus species was performed on Cation-adjusted Mueller Hinton agar, and that of the Streptococcus species was performed on Mueller Hinton agar with 5% sheep blood. Plates were incubated at 35°C for 16–18 h in non-CO2 incubator. The results were interpreted as per the guidelines of the Clinical Laboratory Standards Institute.
The bacterial groups when applicable were designated as fluoroquinolone resistant or susceptible based on disc diffusion susceptibility testing to ciprofloxacin and ofloxacin. Selection of resistance to ciprofloxacin and ofloxacin was desired to test any possible advantage for moxifloxacin and gatifloxacin.
Statistical analysis
Statistical analysis was performed by using Fishers’ exact test or χ2-test as appropriate.
Results
Out of 787 isolates, 147 (18.7%) were Staphylococcus aureus, 279 (35.2%) were coagulase-negative Staphylocci, 357 (45.4%) were Streptococcus pneumoniae, and 4 (0.4%) were other Streptococcus species. Antibiotic susceptibility of 787 gram-positive cocci is shown in Table 1. Of all the four quinolones tested, Organisms showed the highest susceptibility to gatifloxacin (85.6%) followed by ofloxacin (65.6%), moxifloxacin (63.9%), and ciprofloxacin (60.5%). Out of 787 isolates tested, 33 (4.2%) were resistant to all the four fluoroquinoles. The number of isolates that were intermediately sensitive to ciprofloxacin (11.1%) was more when compared with other quinolones.
Comparison of susceptibilities of Gram-positive cocci isolated from keratitis, endophthalmitis, and other specimens (conjunctival swabs, swabs from orbital abscess, and lachrymal abscess) to quinolones is shown in Table 2. Susceptibilities of quinolones against Gram-positive cocci isolated from keratitis, endophthalmitis, and other specimens (conjunctival swabs, swabs from orbital abscess, and lachrymal abscess) were similar to over all susceptibility data; that is, gatifloxacin has increased susceptibility to all Gram-positive cocci isolated from keratitis, endophthalmitis, and other specimens.
Table 3 details the comparisons of antibacterial susceptibilities to the second and fourth generation fluoroquinolones. Out of 39 ciprofloxacin- and ofloxacin-sensitive S. aureus isolates, all the 39 isolates were sensitive to gatifloxacin and only 37 (94.9%) were sensitive to moxifloxacin (P=0.494). Out of 97 ciprofloxacin and ofloxacin resistant S. aureus isolates, 40 (41%) were sensitive to gatifloxacin and only 7 (7.2%) were sensitive to moxifloxacin (P<0.0001). Of 120 ciprofloxacin- and ofloxacin-sensitive coagulase-negative staphylococci, 119 (99%) were susceptible to gatifloxacin and 103 (85%) were sensitive to moxifloxacin (P<0.0001). Of 111 ciprofloxacin- and ofloxacin-resistant coagulase-negative staphylococci, 84 (75.7%) were susceptible to gatifloxacin and 28 (25.2%) were sensitive to moxifloxacin (P<0.0001). Of 301 ciprofloxacin and ofloxacin sensitive S. pneumoniae, 294 (97%) were susceptible to gatifloxacin and 251 (83%) were sensitive to moxifloxacin (P<0.0001). Of five ciprofloxacin- and Ofloxacin-resistant S. pneumoniae, two (40%) were susceptible to gatifloxacin and one (20%) was sensitive to moxifloxacin. Streptococcus species other than S. pneumoniae were in small numbers and were not included in the table for comparison.
Comparison of fourth generation fluoroquinolones showed that the organisms were highly susceptible to gatifloxacin when compared to moxifloxacin.
Discussion
The fluoroquinolone antibiotics are unique class of antibacterial agents with a broad spectrum of antimicrobial activity against most aerobic Gram-negative and Gram-positive bacteria. They have low toxicity, safety, good ocular surface penetration, prolonged tear film concentration, stability at room temperature, and easy availability.12, 13, 14 The emergence of resistance among Gram-positive organisms to the second generation fluoroquinolones was first noticed in 1990 in patients with community-acquired pneumonia caused by S. pneumoniae.15 A number of recent studies have reported resistance to the second and third generation fluoroquinolones among Gram-positive ocular isolates.7, 8, 9 Goldstein et al7 found increased resistance of S. aureus, coagulase-negative staphylococci, and Streptococcus species to the second and third generation fluoroquinolones. Alexandrakis et al16 found that there was increasing laboratory resistance of S. aureus keratitis isolates to quinolones from 11% in 1990 to 28% in 1998.
The fourth generation fluoroquinolones moxifloxacin and gatifloxacin were introduced in 2003, and offer improved spectrum of activity, increased penetration into ocular tissues, and delayed propensity to the development of bacterial antibiotic resistance.17 A retrospective in vitro study by Mather et al11 compared the potencies and antibiotic susceptibilities of ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin against 93 bacterial isolates of endophthalmitis. The second generation fluoroquinolone-resistant S. aureus was statistically more susceptible to moxifloxacin than the other fluoroquinolones. Coagulase-negative Staphylococcus were statistically more susceptible to gatifloxacin and moxifloxacin than levofloxacin, ciprofloxacin, and ofloxacin. They concluded that the fourth generation fluoroquinolones are more potent than the second and third generation quinolones for Gram-positive bacteria, and the fourth generation fluoroquinolones appear to cover the second and third generation fluoroquinolones resistance among Staphylococcus species. Among the gatifloxacin and moxifloxacin, they found moxifloxacin to be more potent than gatifloxacin for Gram-positive bacteria. Stroman et al18 presented similar data showing a high potency of moxifloxacin against fluoroquinolones-resistant isolates of S. aureus and Staphylococcus epidermidis collected from patients with bacterial conjunctivitis and blepharitis. Kowalski et al10 compared the in vitro activity of gatifloxacin, moxifloxacin, levofloxacin, ofloxacin, and ciprofloxacin against 177 bacterial keratitis isolates. They found that the fourth generation fluoroquinolones provide greater antibacterial activity against the Gram-positive keratitis isolates and appear to cover many second generation fluoroquinolone-resistant Staphylococcus isolates. Moxifloxacin showed greater susceptibility for the second generation fluoroquinolone-resistant S. aureus.
Our results are contrary to these earlier reports. We found that, Gram-positive cocci were more susceptible to gatifloxacin (85.6%) when compared with other quinolones. Though moxifloxacin is a fourth generation fluoroquinolone, it showed activity comparable to that of (63.9%) ofloxacin (65.6%) and ciprofloxacin (60.1%). S. aureus isolates susceptible to ciprofloxacin and oflaxacin were also susceptible to gatifloxacin, but only 94% of these isolates were susceptible to moxifloxacin. Among S. aureus isolates that were resistant to ciprofloxacin and oflaxacin, only 7% of were sensitive to moxifloxacin, whereas 40% were sensitive to gatifloxacin.
We noticed similar trends for coagulase-negative Staphylococcus and Streptococcus pneumoniae. One must be careful in interpretation of these results and its applications in clinical practice because (1) the in vitro test is based on the blood concentrations achieved on systemic administration; (2) concentration achieved in ocular tissues after topical administration are much higher; (3) determination of minimum inhibitory concentration gives better approximation of the degree of resistance; (4) the concentration achieved in the ocular tissue depends on the concentration of the drug, and moxifloxacin is marketed as 0.5% solution, whereas gatifloxacin is marketed as 0.3%.The study results are from a single tertiary eye care centre, not representative of the whole region, and susceptibility of bacteria varies from region to region.
Conclusion
On the basis of in vitro antibiotic susceptibility test, using Kirby–Bauer disc diffusion test, gatifloxacin was found to have better acitivity against all Gram-positive cocci, including those resistant to the second generation quinolones at our institute.
References
Thompson NF, Penida R . Antibiotic advances in Ophthalmology. Int Ophthalmol Clin 2004; 44: 91–102.
Yagsi R, Oflu Y, Dincel A, Kaya E, Yarq̆ci S, Bayar B et al. Penetration of second, third and fourth generation topical fluoroquinolones in to aqueous and vitreous humour in a rabbit endophthalmitis model. Eye 2007; 21: 990–994.
Leibowitz HM . Antibacterial effectiveness of ciprofloxacin 0.3% ophthalmic solution in treatment of bacterial conjunctivitis. Am J Opthalmol 1991; 112: 29s–233s.
Hyndiuk RA, Eiferman RA, Caldwel DR, Rosenwasser GO, Santos CI, Katz HR et al. Comparison of ciprofloxacin ophthalmic solution 0.3% to fortified tobramycin–cefazolin in treating bacterial corneal ulcers. Ophthalmology 1996; 103: 1854–1863.
O’ Brien TP, Maguire MG, Fink NE, Alfonso E, McDonnell P . Efficacy of ofloxacin vs cefazolin and tobramycin in the therapy of bacterial keratitis. Arch Opthalmol 1995; 113: 1257–1265.
The Ofloxacin study group. Ofloxacin monotherapy for the primary treatment of microbial keratitis: a double masked, randomized controlled trail with conventional dual therapy. Ophthalmology 1997; 104: 1902–1909.
Goldstein MH, Kowlaski RP, Gordon J . Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology 1999; 106: 1313–1318.
Kunimoto DY, Sharma S, Garg P, Rao GN . In vitro susceptibility of bacterial keratitis pathogens to ciprofloxacin. Ophthalmology 1999; 106: 80–85.
Sharma V, Sharma S, Garg P, Rao GN . Clinical resistance of Staphylococcus keratitis to ciprofloxacin monotherapy. Indian J Ophthalmol 2004; 52: 287–292.
Kowalski RP, Dhaliwal DK, Karenchak LM, Romanowski EG, Mah FS, Ritterband DC et al. Gatifloxacin and moxifloxacin: an in vitro susceptibility comparison to levofloxacin, ciprofloxacin, and ofloxacin using bacterial keratitis isolates. Am J Ophthalmol 2003; 136: 500–505.
Mather R, Karenchak LM, Romanowski EG, Kowalski RP . Fourth generation fluoroquinolones: New weapons in the arsenal of ophthalmic antibiotics. Am J Ophthalmol 2002; 133: 463–466.
Neu HC . Microbiologic aspects of fluoroquinolones. Am J Ophthalmol 1991; 112: 15s–124s.
McDermott ML, Tran TD, Cowden JW, Bugge CJ . Corneal stromal penetration of topical ciprofloxacin in humans. Ophthalmology 1993; 100: 197–200.
Diamond JP, White L, Leeming JP, Bing Hoh H, Easty DL . Topical 0.3% ciprofloxacin, norfloxacin, and ofloxacin in the treatment of bacterial keratitis: a new method for comparative evaluation of ocular drug penetration. Br J Ophthalmol 1995; 79: 606–609.
Borek AP, Dressel DC, Hussong J, Peterson LR . Evolving clinical problems with Streptococcus pneumoniae: increasing resistance to antimicrobial resistance, and failure of traditional optochin identification in Chicago, Illionois, between 1993–1996. Diagn Microbiol Infect Dis 1997; 29: 209–214.
Alexandrakis G, Afonso EC, Miller D . Shifting trends in bacterial keratitis in South Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000; 107: 1497–1502.
Mah FS . Fourth generation fluoroquinolones: new topical agents in the war on ocular bacterial infections. Curr Opin Ophthalmol 2004; 15: 316–320.
Stroman DW, Clark L, Macke L, Mendoza B, Schlech BA, O’Brien TP . Moxifloxacin activity against quinolone resistant Staphylococcal ocular isolates. Invest Ophthalmol Vis Sci 2001; 42 (suppl 4): 1377.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented orally in the 42 annual meeting of Ocular Microbiology and Immunology Group, held on 7th November 2008 at Atlanta, USA
Rights and permissions
About this article
Cite this article
Reddy, A., Garg, P., Alam, M. et al. Comparison of in vitro susceptibilities of Gram-positive cocci isolated from ocular infections against the second and fourth generation quinolones at a tertiary eye care centre in South India. Eye 24, 170–174 (2010). https://doi.org/10.1038/eye.2009.29
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.29
Keywords
This article is cited by
-
Bacterial profile of ocular infections: a systematic review
BMC Ophthalmology (2017)