Abstract
Purpose
To identify the predictive factors for overcorrection and depression impairment after recession of the inferior rectus muscle (IRM) in patients with Graves’ orbitopathy.
Design
Retrospective cohort study, single institution.
Methods
The charts of 124 consecutive patients who underwent recession of the IRM were retrospectively examined, as well as all literature with regard to the subject until January 2008. Ductions measurements, computed tomography (CT) appearance, proptosis, NOSPECS-scores, duration of thyroid disease, duration of orbitopathy, previous treatment of Graves’ thyroid disease and orbitopathy, extent of recession, age, gender, diabetes, smoking, and use of immunosuppressants were all evaluated for prognostic significance.
Results
Duration and severity of orbitopathy and impaired contralateral elevation were significant prognostic factors for overcorrection. Increase of volume of the ipsilateral superior rectus muscle was an independent risk factor for both overcorrection and limitation of depression.
Conclusion
An increase in volume of the ipsilateral superior rectus muscle should be considered when determining the extent of recession of the IRM.
Similar content being viewed by others
Introduction
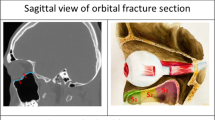
Oculomotor dysfunction in Graves’ disease commonly leads to disabling diplopia, because of extraocular muscle infiltration by inflammatory cells, deposition of mucopolisaccharides, and consequently restrictive myopathy.1 With diplopia in primary gaze or troubling head tilt, extraocular muscle surgery is the treatment of choice, provided the thyroid disease is dealt with and is stable.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
Hypotropia because of restriction of the most frequently affected inferior rectus muscle (IRM) can be corrected by recession of this muscle. However, postoperative depression impairment and overcorrection of the operated eye are sometimes noticed after this particular operation. This phenomenon requires reoperation in 17 to 45% of cases.11
Very little has been published on possible prognostic factors predictive for postoperative depression impairment and overcorrection.
This study aims at identifying preoperative predictors of overcorrection or depression impairment among all patients who underwent recession of the IRM between January 1997 and January 2008 in the Utrecht University Medical Centre, The Netherlands. Ductions measurements, prism cover test, computed tomography (CT) appearance, proptosis, NOSPECS-scores, duration of thyroid disease, duration of orbitopathy, previous treatment of Graves’ thyroid disease and orbitopathy, extent of recession, age, gender, diabetes, smoking, and use of immunosuppressants were all evaluated for prognostic significance.
Patients and methods
Patients
The charts of all patients with Graves’ orbitopathy who had undergone inferior rectus recession from January 1997 to January 2008 were reviewed.
The male/female ratio was 1 : 4 (23 men, 18.5%; 101 women, 81.5%) in this study. The mean age at operation was 55.7 years (range age 33–86 years).
Patients were excluded if previous eye muscle surgery had been performed. When operated simultaneously on the ipsilateral superior rectus muscle, patients were also excluded. Bilateral recession of the IRMs occurred in 24 patients, which were thus analysed for depression impairment, but not for overcorrection. Twenty-eight patients were simultaneously operated upon on the ipsilateral horizontal rectus muscles, which was not an exclusion criterion. Patients with any other kind of strabismus, neuromuscular diseases, amblyopia, or retinal problems were excluded. Seven patients were excluded because of deep amblyopia, a pre-existing form of strabismus, orbital cellulitis, or myasthenia gravis. A total of 124 patients were included in our study.
Methods
In these 124 patients, Graves’ orbitopathy was confirmed by clinical symptoms, orthoptic findings and, in most cases, by CT.
Preoperatively, all patients had undergone a full orthoptic and ophthalmic examination. Thyroid status and orthoptic status were stable before surgery in all patients, for at least 6 months. The indication for surgery was diplopia in primary position of gaze.
In 90% of all eyes, a recession of 3 mm was performed. In severe unilateral cases of impaired elevation (a difference in elevation of ⩾16°) and a large angle of hypotropia (⩾25 prism dioptres), a recession of 4 mm was performed. In case of a unilateral small angle hypotropia (⩽8 prism dioptres) and reasonable elevation (a difference in elevation of 8° between the two eyes), a recession of 2 mm was performed.
In case of bilateral recession, a symmetrical 3 mm recession was performed, unless there was an angle of >5 prism dioptres. In these cases, when elevation was >5°, recessions of 2 and 3 mm were performed. In case of severe elevation impairment, combined with an angle of >5 prism dioptres, 3 and 4 mm recessions were performed.
Patients were evaluated 2 weeks, 3 months, and 6 months postoperatively. Surgical success was defined as the absence of vertical diplopia in primary position and downgaze. Severity of postoperative diplopia was stratified in no diplopia (none), diplopia on extreme gaze (mild), diplopia on down gaze (moderate), and diplopia in primairy position (severe).
Hypertropia of the operated globe of more than five prism dioptres in primary position was considered to be an overcorrection. Limitation of depression was defined as a loss of ⩾5° of downward motility, combined with a total depression of ⩽55°. Duction measurements were performed using the motility meter by Mourits et al (1994).12
Severity of orbitopathy was based on the NOSPECS scoring system, items 2 (soft tissue involvement), 3 (degree of proptosis), 4 (extraocular muscle involvement), and 6 (sight loss). In each of these categories, the signs were scored as mild (a), moderate (b), and severe (c). Patients were stratified according to their worst score on each of these descriptives (Table 2). Mild and moderate sight loss, however, placed patients directly in the ‘moderate’ and ‘severe’ category, respectively.
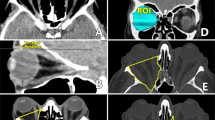
On CT-imaging, an increase in volume was subdivided into three groups, that is, no mild and severe swelling, and was applied to all four rectus muscles. The lateral rectus muscle was used as a reference. When the extraocular muscle was swollen to an extent of 2 times the volume of the lateral rectus muscle, swelling was scored as ‘mild’. Greater swelling was scored as ‘severe’.
Fixed sutures were applied in all cases to avoid late overcorrection by slippage of recessed muscles, which has been described by Hudson and Feldon in 1991.13
Forced duction testing was performed intraoperatively, before placement of a traction suture.
Results
Success according to orthoptic examination
In all, 53 patients (43%) were free of diplopia after the operation, 22 (18%) still had diplopia on extreme gaze (mild), 24 (19%) had diplopia on down gaze (moderate), and 25 (20%) had diplopia in primary position (severe) (Table 1).
Of the 124 patients, 29 (24%) had an overcorrection, whereas 46 (37%) suffered from limitation of depression. There was an overlap of 24 patients. In 43 cases reoperation was required. The remaining eight patients chose not to be reoperated upon after sufficient prismatic correction.
Overcorrection and limitation of depression were not significantly different in patients receiving 2, 3, or 4 mm recessions.
Univariate analysis overcorrection
The univariate analysis of baseline characteristics is shown in Table 2.
The median duration of orbitopathy was significantly shorter in the group with overcorrection (P=0.037).
No patients in the NOSPECS ‘mild’ category suffered from overcorrection, whereas 26 patients did in the higher categories (P=0.018).
None of the general risk factors for impaired tissue repair (smoking, diabetes, and immunosuppressants) showed any prognostic significance.
Univariate analysis limitation depression
None of the factors indicative for overcorrection proved prognostic significance for depression impairment.
Univariate analysis computed tomography appearance
For all 124 patients, only 61% CT-scans were available before operation, most likely because of irretrievable CT-scans performed elsewhere. There was no significant difference in outcome between the group that did and the group that did not have CT-imaging. The results comparing CT appearance to outcome of inferior rectus recession are shown in Table 3.
Increased volume of the ipsilateral superior rectus muscle was a significant predictor for overcorrection and for limited depression postoperatively (P=0.025 and 0.046, respectively). Increase in volume of the other ipsilateral rectus muscles was not associated with our end points, nor was swelling of the contralateral extraocular muscles.
Univariate analysis ductions
Preoperative and postoperative ductions (motility in degrees) were available for 89 patients in the analysis of overcorrection and for 78 patients in the analysis of limited depression. The results are shown in Table 4. Preoperative impairment of elevation of the contralateral eye proved to be of prognostic significance in predicting overcorrection (P=0.017), but not in predicting postoperative limitation of depression (P=0.154). Neither ipsilateral depression nor the contralateral vertical ductions showed any prognostic value for the end points.
Multivariate analysis
In a multivariate analysis of the prognostic factors, none of the other variables showed any interference with significant factors, and P-values remained as they were in univariate analysis.
Intraoperative forced duction testing
All patients underwent intraoperative forced duction testing, which was invariably positive on forced elevation.
Discussion
Very few studies have been performed determining the prognostic factors for motility disorders after recession of the IRM in Graves’ orbitopathy. The few studies that have been performed studied small numbers of patients, and had controversial outcomes.
This study represents the largest series in literature examining the prognostic factors for overcorrection and depression impairment after recession of the IRM in patients with Graves’ orbitopathy so far.
The male/female ratio of 1 : 4 in this study is consistent with the predominance of Graves’ disease in female patients.14
Hudson and Feldon (1991)13 retrospectively studied the charts of 12 consecutive patients who underwent a first operation for vertical muscle imbalance in patients with Graves’ orbitopathy. Five patients developed late hypertropia after recession of the IRM; the seven orthotropic patients served as a reference group. They found the degree of proptosis in both eyes, the volume of the ipsilateral superior rectus muscle, and postoperative limitation of depression in the originally hypotropic eye to be independent prognostic factors for developing late overcorrection. However, they used adjustable sutures for their recessions.
Sprunger and Helveston (1993)15 found, in a review of 67 patients, adjustable sutures to cause progressive overcorrection after inferior rectus recession. However, in this study, patients with thyroid-related orbitopathy were but a mere subgroup of 18 patients. The severity of duction limitation was equal in all groups and the severity of thyroid-related orbitopathy was equally distributed over the two different suture groups.
In a prospective, non-comparative case series of 31 patients with Graves’ orbitopathy, Prendiville et al (2000)11 found, in an attempt to identify predictive factors for operative success for vertical muscle surgery, restriction of the contralateral opposing rectus muscles to be the only significant predictor for overcorrection. The degree of proptosis and preoperative hypotropia were not significantly predictive of surgical success (Table 5).
More recently, Nassar et al (2009)16 retrospectively described the outcomes of strabismus surgery in 50 patients with Graves’ orbitopathy. They found symmetry of orbitopathy at onset and earlier timing of surgery to be associated with good postoperative outcome. The latter being in contrast to our finding that a shorter duration of orbitopathy is related to overcorrection. This study included all surgical procedures that do not focus on the IRM. Their follow-up was 5 weeks, after which overcorrection might still occur. They also performed their surgeries with adjustable sutures, when possible.
This study was performed using non-adjustable sutures only and therefore the results from Sprunger and Helveston (1993)15 could not be compared. The results from Hudson and Feldon (1991)13 have nearly all been reproduced. We found severity of orbitopathy deduced from the NOSPECS scoring system (including proptosis) to be a prognostic factor for overcorrection, and swelling of the ipsilateral superior rectus muscle to be an independent risk factor for overcorrection and impaired postoperative depression. We also found a substantial and significant overlap between the two groups, which they also described. Remarkably, in our study, no patients with mild orbitopathy suffered from postoperative overcorrection.
Our study found shorter duration of orbitopathy to be predictive of overcorrection. A possible explanation could be that the severe cases are generally operated on at an earlier stage, provided that the disease is stable for at least 6 months. However, the exact mechanism remains unclear.
None of the baseline characteristics indicative for overcorrection proved prognostic significance for depression impairment. Finally, impaired elevation preoperatively on the contralateral side was a risk factor for overcorrection, which can be understood with Herings’ law of motor correspondence (equal innervation yoke muscles). Bilateral (asymmetric) recession of the IRM should be considered in such cases.
Conclusion
An increase in volume of the ipsilateral superior rectus muscle can be assumed to be an independent prognostic factor for both postoperative overcorrection and depression impairment, and should be considered when determining the extent of recession of the IRM. Preoperative contralateral elevation impairment was a predictive factor for overcorrection, which advocates bilateral recession of the IRM or a smaller ipsilateral recession. A combination of short duration of Graves’ orbitopathy and contralateral elevation impairment could be considered preoperatively to predict overcorrection, but to evaluate and reproduce the clinical value of these factors, a larger prospective study is to be performed.

References
Kroll AJ, Kuwabara T . Dysthyroid ocular myopathy: anatomy, histology, and electron microscopy. Arch Ophthalmol 1966; 76: 244–257.
Miller JE, Van Heuven W, Ward R . Surgical correction of hypotropias associated with thyroid dysfunction. Arch Ophthalmol 1965; 74: 509–515.
Pratt-Johnson JA, Drance SM . Surgical treatment of dysthyroid restriction syndromes. Can J Ophthalmol 1972; 7: 405–412.
Dyer JA . The oculorotary muscles in Graves’ disease. Trans Am Ophthalmol Soc 1977; 74: 425–456.
Ellis FD . Strabismus surgery for endocrine ophthalmopathy. Ophthalmology 1979; 86: 2059–2063.
Sugar HS . Management of eye movement restriction (particularly vertical) in dysthyroid myopathy. Ann Ophthalmol 1979; 11: 1305–1318.
Scott WE, Thalacker JA . Diagnosis and treatment of thyroid myopathy. Ophthalmology 1981; 88: 493–498.
Evans D, Kennerdell JS . Extraocular muscle surgery for dysthyroid myopathy. Am J Ophthalmol 1983; 95: 767–771.
Mourits MP, Koorneef L, van Mourik-Noordenbos AM, van der Meulen-Schot HM, Prummel MF, Wiersinga WM et al. Extraocular muscle surgery for Graves’ ophthalmopathy: does prior treatment influence surgical outcome? Br J Ophthalmol 1990; 74: 481–483.
Rosenbaum AL, Metz HS, Carlson M, Jampolsky AJ . Adjustable rectus muscle recession surgery: a follow-up study. Arch Ophthalmol 1977; 95: 817–820.
Prendiville P, Chopra M, Gauderman J, Feldon SE . The role of restricted motility in determining outcomes for vertical strabismus surgery in Graves’ ophthalmopathy. Ophthalmology 2000; 107: 545–550.
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L . Measuring eye movements in Graves ophthalmopathy. Ophthalmol 1994; 101 (8): 1341–1346.
Hudson HL, Feldon SE . Late overcorrection of hypotropia in Graves ophthalmopathy. Ophthalmology 1991; 99: 356–361.
Wiersinga WM, Bartalena L . Epidemiology and prevention of Graves’ ophthalmopathy. Thyroid 2002; 10: 855–860.
Sprunger DT, Helveston EM . Progressive overcorrection after inferior rectus recession. J Pediatr Ophthalmol Strabismus 1993; 30: 145–148.
Nassar MM, Dickinson AJ, Neoh C, Powell C, Buck D, Galal E et al. Parameters predicting outcome of strabismus surgery in the management of Graves’ ophthalmopathy. J AAPOS 2009; 13: 236–240.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
De Hoog, J., Stravers, S. & Kalmann, R. Recession of the inferior rectus muscle in Graves’ orbitopathy. Eye 24, 1011–1017 (2010). https://doi.org/10.1038/eye.2009.267
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.267
Keywords
This article is cited by
-
Elongation of the inferior rectus tendon with fascia lata graft for large vertical squint angles in patients with Graves’ orbitopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Predictability of horizontal versus vertical muscle surgery outcomes in thyroid eye disease
International Ophthalmology (2016)