Abstract
Purpose
Basal laminar drusen (BLD) is a rare retinal disorder that may be complicated with choroidal neovascularisation (CNV). Here we describe four patients treated with verteporfin photodynamic therapy (PDT) for CNV secondary to BLD.
Methods
Four consecutive patients presented with subfoveal CNV secondary to BLD. Mean visual acuity was 20/50. CNV was treated with one single PDT session.
Results
Exsudative features of CNV were resolved after one session for all patients. After 6 months, mean visual acuity was 20/25 and remained stable.
Conclusion
In this series, PDT was an effective treatment for CNV secondary to BLD.
Similar content being viewed by others
Introduction
Basal laminar drusen (BLD) is a rare condition, described in 1977 by Gass as small yellow lesions on the posterior pole and the periphery of the retina.1 Commonly appearing in early adulthood, the drusen are usually 25–75 μm in size and are discretely round, slightly raised, subretinal nodules. Later, they often become more numerous and are grouped in clusters. They are more easily visualised angiographically than biomicroscopically, harbouring a ‘star in the sky’ pattern. Vitelliform macular detachment can also be observed.
Gass hypothesised that BLD are caused by nodular thickening of the retinal pigment epithelium (RPE) basement membrane. Recent studies have shown that BLD are located between the basal lamina of the RPE and the inner collagenous layer of Bruch's membrane, just as they are in age-related macular degeneration (AMD).2 This rare condition can be associated with membranoproliferative glomerulonephritis type II (MPGN II).3 Occasionally, BLD may be complicated with choroidal neovascularisation (CNV), resulting in a visual loss.
Photodynamic therapy (PDT) with verteporfin is a recognised method for the treatment of subfoveal CNV in AMD.4 PDT has been also used for the treatment of CNV in pathological myopia or in macular diseases, such as malattia leventinese5 or vitelliform dystrophy.6, 7, 8, 9 To the best of our knowledge, treatment with PDT has not yet been described in this condition.
Here we report four patients with CNV secondary to BLD who underwent treatment with PDT.
Case reports
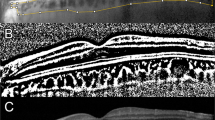
A 40-year-old man, a 59-year-old woman, a 54-year-old woman, and a 38-year-old man presented consecutively at our clinic with subfoveal CNV secondary to BLD. All described metamorphopsia and visual loss on one eye for less than 3 days at presentation. All eyes were treatment naive. At presentation, mean visual acuity was 20/60. (Table 1) One patient (case no. 1) was affected by a MPGN II. Mean age at presentation was 51 years and mean age at diagnosis of BLD was 43 years. Fundus examination showed a little subfoveal haemorrhage in one patient (case no. 1, Figure 1). In all eyes, a grey subfoveal lesion was observed, associated with BLD. In all cases, fluorescein angiography revealed numerous early and intense hyperfluorescent dots like ‘stars in the sky’ corresponding to BLD. Furthermore, we observed a hyperfluorescence of the lesion on early phases, with leakage on late phases corresponding to subfoveal classic CNV. Vitelliform macular detachment was observed in one patient (case no. 2). Optical coherence tomography (OCT-3, Humphrey-Zeiss, San Leandro, CA, USA) confirmed the presence of a subfoveal CNV, showing a moderately hypereflective mass above the RPE with the neurosensory retina elevation and little macular thickening (Figure 1).
Patient no. 1 affected with basal laminar drusen (BLD) and choroidal neovascularisation (CNV). At presentation, visual acuity is 20/64. (a) Colour fundus photograph shows a grey subfoveal lesion with a little haemorrhage. (b) Early phases of fluorescein angiography (FA) reveal a hyperfluorescence of the lesion associated with innumerable hyperfluorescent BLD harbouring a ‘stars in the sky’ pattern. (c) On the late phases of FA, a leakage of the lesion is observed corresponding to a subfoveal classic CNV. (d) On the late phases of indocyanine green angiography (ICGA), we observe a heterogeneous hyperfluorescence corresponding to the neovascularisation. (e) Optical coherence tomography (OCT) scan (arrow) shows a hypereflective mass above the retinal pigment epithelium corresponding to a subfoveal CNV with macular thickening. Central macular thickness is 298 μm.
One single PDT session was performed, in accordance with the standard protocol used for treating CNV secondary to AMD,4 after obtaining a written informed consent, in agreement with the French legislation and our local ethics committee.
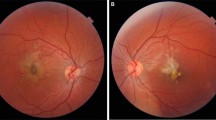
Three months later, the four patients reported improvement of their visual symptoms. Mean visual acuity improved to 20/32 (Table 1). Fundus examination revealed regression of the grey lesion (Figure 2). On late phases of fluorescein angiography, no more leakage was observed. OCT showed the absence of macular fluid in all cases. No recurrence occurred and no re-treatment was needed. After 6 months, mean visual acuity was 20/25 and remained stable throughout the follow-up (2 years for two patients, 4 years for one, and 9 years for one).
Patient no. 1 affected with BLD and CNV. At 4 years after treatment with PDT, visual acuity is 20/20. (a) Colour fundus photograph shows regression of the grey lesion. (b) Early phases of FA show a hyperfluorescent atrophic area. (c) Late phases of FA also show the hyperfluorescent atrophic area without any leakage. (d) The lesion is strictly hypofluorescent on the late phases of ICGA. (e) On OCT scan (arrow), there is no retinal fluid or macular thickening. Central macular thickness is 171 μm.
Discussion
Choroidal neovascularisation is the main complication of BLD occurring in 10–31% of cases.10, 11 We describe here for the first time four patients with CNV complicating BLD who were successfully treated by one single session of PDT. Visual acuity improved in all patients without metamorphopsia at the end of the follow-up (2 years at least).
It could be hypothesised that vascular endothelial growth factor (VEGF) is probably implicated in the occurrence of CNV in BLD patients. To our knowledge, anti-VEGF antibodies have not been reported yet for treatment of CNV secondary to BLD.
In conclusion, in our small series, PDT was an effective treatment for CNV secondary to BLD. However, additional data are needed to establish the visual benefit of PDT in this condition. Furthermore, intravitreal anti-VEGF treatment should also be evaluated.

Conflict of interest
The authors declare no conflict of interest.
References
Gass JD . Stereoscopic Atlas of Macular Diseases. The CV Mosby Co: St Louis, 1977.
Russell SR, Mullins RF, Schneider BL, Hageman GS . Location, substructure, and composition of basal laminar drusen compared with drusen associated with aging and age-related macular degeneration. Am J Ophthalmol 2000; 129: 205–214.
Leys A, Vanrenterghem Y, Van Damme B, Snyers B, Pirson Y, Leys M . Fundus changes in membranoproliferative glomerulonephritis type II. A fluorescein angiographic study of 23 patients. Graefes Arch Clin Exp Ophthalmol 1991; 229: 406–410.
Bressler NM . Treatment of Age-Related Macular Degeneration with Photodynamic therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials-tap report 2. Arch Ophthalmol 2001; 119: 198–207.
Dantas MA, Slakter JS, Negrao S, Fonseca RA, Kaga T, Yannuzzi LA . Photodynamic therapy with verteporfin in mallatia leventinese. Ophthalmology 2002; 109: 296–301.
Verteporfin in Photodynamic Therapy Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin. 1-year results of a randomized clinical trial—VIP report no. 1. Ophthalmology 2001; 108: 841–852.
Verteporfin Roundtable 2000 and 2001 Participants. Treatment of age-related macular degeneration with photodynamic therapy (TAP) study group principal investigators; Verteporfin in photodynamic therapy (VIP) study group principal investigators. Guidelines for using verteporfin (visudyne) in photodynamic therapy to treat choroidal neovascularization due to age-related macular degeneration and other causes. Retina 2002; 22: 6–18.
Menchini U, Giacomelli G, Cappelli S, Giansanti F, Romani A, Virgili G . Photodynamic therapy in adult-onset vitelliform macular dystrophy misdiagnosed as choroidal neovascularization. Arch Ophthalmol 2002; 120: 1761–1763.
Ergun E, Costa D, Slakter J, Yannuzzi LA, Stur M . Photodynamic therapy and vitelliform lesions. Retina 2004; 24: 399–406.
Gass JD, Jallow S, Davis B . Adult vitelliform macular detachment occurring in patients with basal laminar drusen. Am J Ophthalmol 1985; 99: 445–459.
Cohen SY, Meunier I, Soubrane G, Glacet-Bernard A, Coscas GJ . Visual function and course of basal laminar drusen combined with vitelliform macular detachment. Br J Ophthalmol 1994; 78: 437–440.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guigui, B., Martinet, V., Leveziel, N. et al. Photodynamic therapy for choroidal neovascularisation secondary to basal laminar drusen. Eye 23, 2115–2118 (2009). https://doi.org/10.1038/eye.2009.239
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.239