Abstract
Purpose
To evaluate the learning effect of frequency doubling technology (FDT) perimetry using the Humphrey Matrix perimeter in healthy subjects with no perimetric experience.
Methods
One eye of 28 healthy adults who had no history of visual field testing underwent three Matrix tests using 24-2 programme with full-threshold strategy. The results of the first session were compared with those of the second, and the third sessions. Learning effect was defined as an improvement at results for duration, perimetric indices, and the number of points with a P<5 and <1% in the total and pattern deviation maps. Anderson's criteria were applied to define abnormal examinations.
Results
The mean in the mean deviation global index was −7.40±1.49 dB in the first session, −4.64±0.97 dB in the second session, and −3.29±0.93 dB in the third session. Pattern standard deviations were decreased as the tests were repeated (P<0.01). Test duration, fixation losses, false negative, and the number of points with a P<5 and <1% in the total and pattern deviation maps rate were also changed significantly (P<0.05). Among the criteria suggested by Anderson, the Glaucoma Hemifield Test performed better in all session tests. The false-positive rates ranged from 50% (95% confidence intervals [CI] 30.6–69.4%) to 64% (95% CI 44.1–81.4%) for the first session, 29% (95% CI 13.2–48.7%) to 54% (95% CI 33.9–72.5%) for the second session, and from 18% (95% CI 6.1–36.9%) to 32% (95% CI 15.9–52.4%) for the third session.
Conclusions
The results of this study show that the learning effect for Humphrey Matrix FDT perimetry must be considered in normal individuals with no perimetric experience.
Similar content being viewed by others
Introduction
Glaucoma is a major cause of preventable blindness worldwide and an increasingly significant global health problem. It is estimated that 60.5 million people will have primary glaucoma by the year 2010, with 8.4 million suffering from bilateral blindness.1 Automated perimetry has become an essential component in the successful diagnosis and follow-up of glaucoma for the past three decades.2 Currently, standard automated perimetry (SAP) is the clinical test most often used for evaluating the visual field (VF) in these patients, however, many newer instruments are continuously being developed to improve the diagnostic yield and shorten the test duration, to help reduce the fatigue induced by the test and increase patient acceptability.3, 4, 5, 6, 7
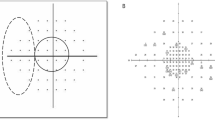
Frequency doubling technology (FDT) is based on a phenomenon called the ‘frequency doubling illusion’, which occurs when low spatial frequency (<1 cycle/degree) grating undergoes high temporal frequency (>15 Hz) counterphase flicker.3, 4 This type of illusion is thought to be mediated by the magnocellular retinal ganglion cells, whose loss, probably because of reduced redundancy, may be detectable in early glaucoma. Thus, this method of perimetry is useful to detect early glaucomatous VF.7 The first available version of the FDT perimeter has been reported to be a good predictor of future glaucomatous damage that is not yet detectable by SAP.6 However, it is difficult to compare original FDT findings to those obtained by SAP directly.
Humphrey Matrix perimetry (HMP) is a new device for perimetry using FDT.8 The FDT Matrix perimeter uses smaller stimuli and more tests locations than those of the original FDT device for better characterization of the defect. All the parameters, such as the mean deviation (MD), pattern standard deviation (PSD), Glaucoma Hemifield Test (GHT), total deviation plots, and pattern deviation plots are shown in the printout, which is similar to that of the SAP. Reliability checks include 10 fixation checks using Heijl and Krakau9 method, 10 false-positive and 6 false-negative trials, in which the final results are given as both as a ratio and as a percentage. Theoretically, HMP could be used like FDT perimetry to detect early glaucomatous VF abnormalities with the benefit of having a direct correlation with SAP in terms of testing locations.10, 11
The improvement in perimetric results occurring over repetitions in inexperienced subjects is a well-known phenomenon called ‘learning effect’. It is an important issue in many psychophysical tests.12 A learning effect would tend to increase the false-positive rates for inexperienced examinees, influencing the specificity, and therefore be detrimental to the implementation of any technology used as a screening device.13
The learning effect for SAP was extensively studied showing an increase in the absolute mean sensitivity with subsequent examinations.14, 15, 16 This effect was also shown in short wavelength automated perimetry,17, 18 flicker perimetry,19 and frequency doubling perimetry.20, 21, 22, 23 The aim of this study was to evaluate the learning effect across multiple tests in HMP using the full-threshold 24-2 strategy in healthy patients without perimetric experience.
Materials and methods
This study was approved by the ethics in research committee of the University Vale of Acaraú and conducted according to the tenets of Declaration of Helsinki. Written informed consent was obtained from the participants. All subjects underwent a comprehensive ophthalmic examination, including medical and family history, manifest refraction, visual acuity (VA) measurement, slit lamp examination, Goldmann applanation tonometry, gonioscopy, pachimetry, and dilated fundus examination using a 78-diopter (D) lens. To be included in the study, subjects were required to be 18 years or older, had not previously undergone automated perimetry, had corrected VA of 20/30 or better, clear ocular media, a cup-to-disc ratio ⩽0.4, an open-angle, no known family history of glaucoma in first-degree relatives, spherical refraction within plus or minus 5.0 D, and cylinder correction within plus or minus 3.0 D. These were excluded if they had an intraocular pressure of more than 21 mm Hg in either eye, suspicious appearing optic disc (ie, localized rim loss, optic disc haemorrhage, cup disc asymmetry >0.2), history of any ocular disease, surgery or trauma, abnormal pupillary examination or history of miotic use, or other medications use that might affect pupil size, history of systemic medication use that might affect the VF, history of cerebrovascular event, or diabetes mellitus.
Subjects were recruited from the general population, including hospital staff and their family members, spouses, or friends of patients. One eye was chosen at random for each volunteer, and only that eye was tested throughout the study. The subjects were not informed about the purpose of the study to avoid any bias. Each subject received a brief explanation about testing, the device, and the examination procedure, including a short demonstration of frequency doubling phenomenom. All subjects were examined three times, with the necessary corrective lenses or their own spectacles, using the 24-2 full-threshold programme of the commercially available Humphrey Matrix FDT perimeter (Welch Allyn, Skaneateles Falls, NY, USA and Carl Zeiss Meditec, Dublin, CA, USA) under normal room illumination. They were merely and repeatedly asked to do their best at each and every examination. Patients were required to take at least a 30 min rest between each test, in an attempt to diminish the fatigue effect.
The Humphrey Matrix 24-2 full threshold uses 55 stimuli (square 5° × 5° target with 6° grid spacing), arranged in a 24-2-like pattern, with spatial frequency of 0.50 cycles/degree and temporal frequency of 18 Hz. Stimuli are presented for 500 ms, including ramped onsets and offsets of 100 ms. The full-threshold strategies use a maximum likelihood threshold strategy known as zippy estimation by sequential testing, to provide accurate threshold results as quick as possible. This strategy determines the likely distribution of sensitivities according to the patient's responses to four stimuli presentations at each location. When all sensitivities are estimated, its algorithm checks for any points that differ by more than 4 dB from four neighbouring points, then determines sensitivity again for these points.8, 24
The results of each test were classified as normal or abnormal to establish the false-positive rate of each session. Anderson's criteria were use to define abnormality: GHT outside normal limits (GHT definition), PSD probability <5% (PSD definition), or a cluster of three or more adjacent non-edge points in typically glaucomatous locations, all of which were depressed on the pattern deviation plot at a P<5% level and one of which was depressed at a P<1% level (cluster definition).25 Tests were performed with the same machine, and each subject had the same VF technician for all tests. As there are no common values of normality for FDT reliability indexes, we included all the FDT examinations carried out in the analysis, without any subjective exclusion criteria. We subsequently considered the results according to the reliability indexes of normality used for conventional perimetry (fixation losses <20%, false-positive and false-negative responses <33%).
To assess for learning effects, we compared the results of test duration (excluding instruction time), global indexes (MD and PSD), reliability indexes (fixation errors, false-positive, and false-negatives responses), and a number of locations with P<5 and <1% in both total and pattern deviation maps across all the three tests using Friedman's test or Wilcoxon test as appropriate. In addition, we calculated the false-positive rate of each criterion suggested by Anderson. The false-positive rates were compared by the McNemar's test. Statistical analyses were performed with SAS version 8.20 (SAS Institute Inc., Cary, NC, USA). A P-value <0.05 was considered statistically significant. Data are reported as mean±SD where applicable, uncertainty quantified as 95% confidence intervals (CI).
Results
Twenty-eight subjects were recruited and completed the protocol. The mean age was 43.5±1.5 years (range, 26–61 years). Nine (32.1%) were men and 19 (67.9%) women. Regarding race distribution, 13 (46.4%) were White, 6 (21.4%) were Black, and 9 (32.2%) were mixed. Regarding educational level, 10 (35.7%) had incomplete primary education, 11 (39.3%) had complete primary education, 5 (17.9%) had secondary education, and 2 (7.1%) had complete tertiary education. Ten eyes were emmetropic and the remaining 18 had a mean refractive error of −1.05 D (range, +0.75 to −3.0 D). The mean central corneal thickness was 550.89±5.64 μ (range, 500–640 μ).
The average results for each repetition are summarized in Table 1. The false-positive rate did not significantly fluctuate. A statistically significant difference was found in test duration, MD, PSD, fixation errors, false negatives, and a number of depressed points deviating at P<5 and <1% on the total and pattern deviation maps. The average duration of examination (expressed in seconds) decreased progressively when the tests were repeated. On average, each examination was performed faster than the preceding one. As far as test duration is concerned, we found a clear, but mild learning effect throughout the study (from 329.36±3.81 s (95% CI 327.95–330.77) for the first examination to 320.82±2.87 s (95% CI 319.76–321.88) for the third examination; P=0.001) (Table 1). There was an obvious improvement in MD when repeating the examination. MD progressively improved from −7.40±1.49 dB at the first examination to −3.29±0.93 dB at the third examination (P<0.05). PSD progressively decreased from 4.13±0.24 dB at the first examination to 3.34±0.21 dB at the third examination (P<0.05) (Table 1).
The results of GHT appeared different between the first and both second and third examinations, with an increase of normal results when the examination was repeated.
When we analysed the average number of depressed locations with P<5 and <1% in both total and pattern deviation plots, we found a progressively reduction in all values when repeating the examination. The improvement seen among the examinations reached statistical significance (P<0.05).
When considering the reliability indexes with the same criteria of normality used for conventional perimetry (fixation losses <20%, false-positive and false-negative responses <33%), there were more unreliable results in the first session (nine cases) than both second (two cases; P=0.019) and third sessions (one case; P=0.005).
Table 2 shows the false-positive rate of each criterion for each session test. Among the criteria suggested by Anderson, the GHT performed better in all session tests. The false-positive rates varied from 50% (95% CI 30.6–69.4%) to 64% (95% CI 44.1–81.4%) for the first session, 29% (95% CI 13.2–48.7%) to 54% (95% CI 33.9–72.5%) for the second session, and from 18% (95% CI 6.1–36.9%) to 32% (95% CI 15.9–52.4%) for the third session. There was no statistically significant difference between the false-positive rates when comparing the first and second session for all criteria studied (P>0.05). However, a statistically significant difference was found when comparing the false-positive rates between the first and third session tests for all criteria (P<0.05).
Discussion
FDT perimetry has shown several advantages over SAP, including the following:26 low cost; transportability; tolerance to blur, pupil size, and refractive errors; shorter test time; and lower test–retest variability. Furthermore, it is suggested that FDT may detect VF loss before SAP.7
Humphrey Matrix provides new programmes with smaller targets at narrower intervals, which may prove to detect subtle VF deficits and monitor VF progression more accurately than original FDT. Most reports that compare the results of Humphrey Matrix with those of the Humphrey Field Analyser indicate that the two VF techniques produce similar results.27 Additionally, HMP has been reported to have reasonably uniform variability properties for all levels of glaucomatous VF loss,24 and some studies have suggested that FDT testing may be useful for determining glaucomatous visual progression.7, 28
In SAP, a learning effect can influence the results of the VF test in both healthy and glaucomatous patients.12, 13, 14 Patients with ocular hypertension and experienced with SAP showed mild learning effect at Matrix, significantly affecting only the first test.22 In this study, we evaluated the learning effect for the Matrix perimetry using the full-threshold 24-2 strategy over three test repetitions in healthy individuals who never underwent automated perimetry. The data presented strongly suggest a learning effect. The improvement in MD was shown to be statistically significant when comparing the first session with subsequent sessions; PSD, test duration, fixation losses, false negative, and the number of depressed locations with a P<5 and <1% on the total and pattern deviation maps rate were largest at the first test and decreased as the test was repeated. Our results confirm earlier findings suggesting presence of learning for FDT, regardless of the version of the device, of the adopted strategy10, 13, 20, 23 (screening and full-threshold procedures), and of the features of the study population21 (normal subjects vs glaucomatous patients).
Iester et al29 observed a mild learning effect with the first-generation FDT programme C-20 full threshold in a group of 20 healthy subjects. The authors used a normal SAP as an inclusion criterion. This might have biased the results. The earlier exposure to SAP might diminish learning effect with FDT perimetry, because the same principles of static perimetry test administration are used with both types of tests. Another report30 with FDT evaluating the learning effect of a group of glaucoma patients showed that a learning effect was present between the first and second, but not between the second and third, tests. Again, these patients had experience with conventional automated perimetry.
The learning effect of FDT Matrix was assessed on a group of 37 healthy subjects, inexperienced to perimetry.23 This study, using the 30-2 full-threshold programme, confirmed the presence of a learning effect at the first test, but its design was limited by the absence of eye randomization: both eyes of each patient were tested twice over two sessions and learning effect was esteemed as the improvement in results for left eyes. This method does not control the possible interference of phenomena such as the cortical adaptation to FDT stimulus and the fatigue effect occurring at the end of each session. Moreover, owing to the limited number of tests, this study did not show stability in perimetric performances, as it did in our study from the second to the third test.
Our results are consistent with those of an earlier study,21 which showed a learning effect of the MD and PSD in both normal and glaucoma patients using HMP with a full-threshold 30-2 strategy. However, in contrast with our findings, the study did not show a statistically significant difference in test duration, fixation losses, and false-negative responses (P>0.05), and did not evaluate the number of points with a P<5 and <1% in the total and pattern deviation maps.
Some authors recommend administration of a demonstration of the frequency doubling phenomenon,31, 32 or a training session,29 to reduce learning effects. In this study, subject instruction before the first FDT Matrix test included such a short demonstration; however, this did not eliminate learning effects or unreliability. With regard to reliability, the manufacturer's criteria for abnormality are not explicitly known. As FDT is a psychophysical test, explanations for differences in reliability reported by other studies may be because of differences in the patient population, culture, language, education background, and technician ability and training. The majority of the patient population of this study had a low educational level and limited experience with electronics or buttons. This factor also may be a possible influence factor to the relatively high rate of unreliable and/or abnormal fields in our patient population even after the third test. Indeed, as found in another study32 with FDT perimetry, there was a progressive increase in the number of reliable VF tests when repeating the examination.
We assumed that results based on a single test of subjects inexperienced in perimetry might result in high false-positive rates because of undetected learning effect. Although the Anderson's criteria may not be so applicable for assessing abnormal Matrix VF, we wanted to avoid using any other perimetric technique in these subjects. Of the criteria examined, usage of the GHT has a lower false-positive rate for all session tests. These findings suggest that a single examination with FDT Matrix would not be appropriate during mass screening for glaucoma.
In summary, our study shows that healthy subjects without experience with SAP showed a learning effect at Matrix, significantly affecting the first three sessions, and the results of the GHT appeared improved. In the presence of low MD and high PSD values at the first Matrix, caution in analysis is needed and retest could be advisable to exclude the possibility of a false-positive result owing to learning artefacts. Although our findings may also be limited by the small sample size of the study, resulting in wide CIs, by the lack of a control group, and because we only examined changes between the first three field examinations, it is probably necessary to obtain at least three repetitions to rule out the presence of a learning effect in the majority of such patients before providing useful results. These above all should be taken into account when considering the clinical use of this test to avoid erroneous diagnostic conclusions.
References
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90 (3): 262–267.
Medeiros FA, Zangwill LM, Bowd C, Weinreb RN . Comparison of the GDx CCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomography for the detection of glaucoma. Arch Ophthalmol 2004; 122 (6): 827–837.
Kelly DH . Frequency doubling in visual responses. J Opt Soc Am 1966; 56: 1628–1633.
Kelly DH . Nonlinear visual responses to flickering sinusoidal gratings. J Opt Soc Am 1981; 71 (9): 1051–1055.
Hong S, Ahn H, Ha SJ, Yeom HY, Seong GJ, Hong YJ . Early glaucoma detection using the Humphrey matrix Perimeter, GDx VCC, Stratus OCT, and retinal nerve fiber layer photography. Ophthalmology 2007; 114 (2): 210–215.
Wu LL, Suzuki Y, Kunimatsu S, Araie M, Iwase A, Tomita G . Frequency doubling technology and confocal scanning ophthalmoscopic optic disc analysis in open-angle glaucoma with hemifield defects. J Glaucoma 2001; 10 (4): 256–260.
Medeiros FA, Sample PA, Weinreb RN . Frequency-doubling technology perimetry abnormalities as predictors of visual field loss. Am J Ophthalmol 2004; 137 (5): 863–871.
Turpin A, McKendrick AM, Johnson CA, Vingrys AJ . Properties of perimetric threshold estimates from full threshold, ZEST, and SITA-like strategies, as determined by computer simulation. Invest Ophthalmol Vis Sci 2003; 44 (11): 4787–4795.
Heijl A, Krakau CE . An automatic static perimeter, design and pilot study. Acta Ophthalmol 1975; 53 (3): 293–310.
Spry PG, Johnson CA . Within-test variability of frequency-doubling perimetry using 24-2 test pattern. J Glaucoma 2002; 11 (4): 315–320.
Anderson AJ, Johnson CA, Fingeret M, Keltner JL, Spry PG, Wall M et al. Characteristics of the normative database for the Humphrey matrix perimeter. Invest Ophthalmol Vis Sci 2005; 46 (4): 1540–1548.
Heijl A, Lindgren G, Olsson J . The effect of perimetric experience in normal subjects. Arch Ophthalmol 1989; 107 (1): 81–86.
Pierre-Filho PT, Schimiti RB, Vasconcellos JP, Costa VP . Sensitivity and specificity of frequency-doubling technology, tendency-oriented perimetry, SITA Standard and SITA Fast perimetry in perimetrically inexperienced individuals. Acta Ophthalmol Scand 2006; 84 (3): 345–350.
Heijl A, Bengtsson B . The effect of perimetric experience in patients with glaucoma. Arch Ophthalmol 1996; 114 (1): 19–22.
Werner EB, Krupin T, Adelson A, Feitl ME . Effect of patient experience on the results of automated perimetry in glaucoma suspect patients. Ophthalmology 1990; 97 (1): 44–48.
Schimiti RB, Avelino RR, Kara-José N, Costa VP . Full-threshold vs Swedish Interactive Threshold Algorithm (SITA) in normal individuals undergoing automated perimetry for the first time. Ophthalmology 2002; 109 (11): 2084–2092; discussion 2092.
Wild JM, Moss ID . Baseline alterations in blue-on-yellow normal perimetric sensitivity. Graefes Arch Clin Exp Ophthalmol 1996; 234 (3): 141–149.
Rosseti L, Fogagnolo P, Miglior S, Centofanti M, Vetrugno M, Orzalesi N . Learning effect of short-wavelength automated perimetry in patients with ocular hypertension. J Glaucoma 2006; 15 (5): 399–404.
Bernardi L, Costa VP, Shiroma LO . Flicker perimetry in healthy subjects: influence of age and gender, learning effect and short term fluctuation. Arq Bras Oftalmol 2007; 70 (1): 91–99.
Horani A, Frenkel S, Yahalom C, Farber MD, Ticho U, Blumenthal EZ . The learning effect in visual field testing of healthy subjects using frequency doubling technology. J Glaucoma 2002; 11 (6): 511–516.
Hong S, Na K, Kim CY, Seong GJ . Learning effect of Humphrey matrix perimetry. Can J Ophthalmol 2007; 42 (5): 707–711.
Centofanti M, Fogagnolo P, Oddone F, Orzalesi N, Vetrugno M, Manni G et al. Learning effect of humphrey matrix frequency doubling technology perimetry in patients with ocular hypertension. J Glaucoma 2008; 17 (6): 436–441.
Contestabile MT, Perdicchi A, Amodeo S, Recupero V, Recupero SM . The influence of learning effect on frequency doubling technology perimetry (Matrix). J Glaucoma 2007; 16 (3): 297–301.
Artes PH, Hutchinson DM, Nicolela MT, LeBlanc RP, Chauhan BC . Threshold and variability properties of matrix frequency doubling technology and standard automated perimetry in glaucoma. Invest Ophthalmol Vis Sci 2005; 46 (7): 2451–2457.
Anderson DR, Patella VM . Automated Static Perimetry. Mosby: St Louis, MO, 1992, pp 10–35.
Anderson AJ, Johnson CA . Frequency-doubling technology perimetry. Ophthalmol Clin North Am 2003; 16 (2): 213–225.
Spry PG, Hussin HM, Sparrow JM . Clinical evaluation of frequency doubling technology perimetry using the Humphrey Matrix 24-2 threshold strategy. Br J Ophthalmol 2005; 89 (8): 1031–1035.
Burganski-Eliash Z, Wollstein G, Patel A, Bilonick RA, Ishikawa H, Kagemann L et al. Glaucoma detection with matrix and standard achromatic perimetry. Br J Ophthalmol 2007; 91 (7): 933–938.
Iester M, Capris P, Pandolfo A, Zingirian M, Traverso CE . Learning effect, short-term fluctuation, and long-term fluctuation in frequency doubling technique. Am J Ophthalmol 2000; 130 (2): 160–164.
Fujimoto N, Minowa K, Miyauchi O, Hanawa T, Adachi-Usami E . Learning effect for frequency doubling perimetry in patients with glaucoma. Am J Ophthalmol 2002; 133 (2): 69–270.
Johnson CA, Cioffi GA, Van Buskirk EM . Frequency doubling technology perimetry using a 24-2 stimulus presentation pattern. Optom Vis Sci 1999; 76 (8): 571–581.
Joson PJ, Kamantigue ME, Chen PP . Learning effects among perimetric novices in frequency doubling technology perimetry. Ophthalmology 2002; 109 (4): 757–760.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pierre-Filho, P., Gomes, P., Pierre, E. et al. Learning effect in visual field testing of healthy subjects using Humphrey Matrix frequency doubling technology perimetry. Eye 24, 851–856 (2010). https://doi.org/10.1038/eye.2009.210
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.210