Abstract
Purpose
To examine the early changes of retinal sensitivity by fundus-related microperimetry after subthreshold micropulse diode laser photocoagulation (SMDLP) for diabetic macular oedema (DMO).
Methods
Twenty-eight eyes of 28 patients with diffuse DMO were treated with SMDLP. The mean retinal sensitivity within the central 10 degrees measured with a fundus-related microperimeter, MP1, best corrected visual acuity (BCVA) in logarithm of minimum angle of resolution units, and optical coherence tomography-determined foveal thickness (FT) were examined before and 3 months after SMDLP. The pretreatment values of the retinal sensitivity, FT, BCVA, and funduscopic findings were compared with the corresponding values at 3 months after SMDLP.
Results
At 3 months, the BCVA was significantly improved (P=0.03), and the FT was significantly reduced (P=0.0043). The mean retinal sensitivity within the central 10 degree, however, did not change significantly (P=0.70). The correlation between the changes in the retinal sensitivities and the decrease in the FT was not significant. The correlation between the changes in the retinal sensitivities and the BCVA was also not significant.
Conclusions
Significant improvements in retinal sensitivities within the central 10 degrees were not observed even though the decrease in FT and the improvement of BCVA were significant. On account of this difference of changes in retinal sensitivity and BCVA, the combination of retinal sensitivity by MP1 and BCVA may be beneficial in assessing the visual function from various angles after SMDLP for eyes with DMO.
Similar content being viewed by others
Introduction
Macular oedema is a major cause of visual decrease, and the decrease can reduce the quality of life markedly in patients with diabetic retinopathy. The results of the Early Treatment of Diabetic Retinopathy Study (ETDRS) indicated that visible end-point laser photocoagulation reduced the risk of vision loss in patients with clinically significant diabetic macular oedema (DMO).1 However, photocoagulation with conventional continuous wave laser systems can damage the microstructures of the neural retina by the spread of heat from the retinal pigment epithelium (RPE).2, 3
The damage created by laser photocoagulation can be reduced by reducing the laser exposure time and the laser power to the subvisible level.4, 5, 6 It was recently reported that subthreshold micropulse diode laser photocoagulation (SMDLP) could minimize the chorioretinal damage in eyes with clinically significant DMO.7, 8 An improvement of the visual acuity (VA) and resolution of the macular oedema were also shown.
The visual function of patients with DMO is usually assessed by the conventional VA even though it is well known that fundus-related perimetry is clinically useful in assessing the effects of macular oedema. We have reported that the retinal sensitivity of the macular area determined by fundus-related microperimetry, MP1 (Nidek, Japan), was significantly correlated with the VA and foveal retinal thickness, and suggested that this may provide another method to assess the effects of DMO.9 Similar findings were also reported,10 and it was suggested that microperimetry may be of value in predicting the outcome of DMO.10
The purpose of this study was to determine the retinal sensitivity of the macula area with the MP1 in patients with DMO treated with SMDLP, and to compare the retinal sensitivity with the best corrected visual acuity (BCVA) and the foveal thickness (FT) measured by optical coherence tomography (OCT).
Materials and methods
The procedures used in this study conformed to the tenets of the Declaration of Helsinki, and an informed consent was obtained from all subjects after the nature and possible consequences of the study were explained. Twenty-eight consecutive patients who had diffuse DMO based on the criteria of the ETDRS or with cystoid macular oedema and had undergone SMDLP at the Chiba University Hospital were recruited. As a result, one eye of each patient was treated with SMDLP and included in the study. Unintentionally, none of the patients underwent SMDLP bilaterally. All patients completed 3 months of follow-up. Patients that had undergone pars plana vitrectomy, direct photocoagulation of microaneurysms, and panretinal photocoagulation (PRP) 6 months before the SMDLP were excluded. Among the 28 patients, 3 patients had undergone pars plana vitrectomy for DMO and 13 patients had undergone PRP. These procedures were performed more than 6 months earlier. The ages of the patients ranged from 39 to 89 years (60.2±11.5 years; mean±SD).
SMDLP was performed with an 810 nm infrared diode laser (Iris Medical OcuLight SLx, Iridex Corporation, Mountain View, CA, USA). The parameters of the laser used were 200μm spot diameter, 0.2s exposure, and 15% duty cycle. Initially, the power necessary to cause a barely visible burn by a continuous wave was determined, and the power was then set to twice that value for the treatment. The area of macular oedema was treated in a standard grid pattern as described by the ETDRS except for the area of the papillomacular nerve bundle.
Before and 3 months after SMDLP, each patient had an MP1 examination and a comprehensive ophthalmic examinations including measurements of the BCVA, OCT, fluorescein angiography, and indirect ophthalmoscopy.
Fundus-related microperimetry was performed with the MP1 using the software available with the 2006 model (Version: MP1 SW 1.4.1.SP1) with automated correction for eye movements. The follow-up examination was performed exactly over the earlier tested retinal points and was performed 3 months after the SMDLP. The auto-tracking system calculates the x and y coordinates and rotational shifts relative to a reference frame obtained by an infrared camera at the beginning of the examination, which returns a map of the patient’s eye movements during the examination. Goldmann III stimuli and a 4-2 staircase strategy were used, and a rectangular 3 × 3 degrees test grid with 24 stimulus locations covering an area of 10 degrees was applied. The stimuli were projected on a white background with white background illumination set at 1.27 cd/m2, and the stimulus duration was 100 ms. The differential luminance, defined as the difference between stimulus luminance and background luminance, was 127 cd/m2 at 0 dB stimulation, and the maximum stimulus attenuation was 20 dB. The mean retinal sensitivity within the central 10 degrees was determined.
The BCVA was measured with a Japanese Landolt chart and converted into the logarithm of the minimum angle of resolution (logMAR) units for statistical analyses. The FT was defined as the distance between the vitreoretinal interface and the RPE in the centre of the fovea, that is the foveola, using the OCT3000 (Carl Zeiss Meditec, Dublin, CA, USA).
The numerical data were analysed with the Student's t-test and Pearson's correlation tests. A P-value of <0.05 was considered statistically significant. The change in retinal sensitivity was defined as the retinal sensitivity (dB) at baseline subtracted from the retinal sensitivity (dB) obtained at the post-treatment examination. A change in FT was defined by a ratio of the decrease value from the baseline divided by the FT at the baseline. Changes in VA were defined as the logMAR VA obtained at the post-treatment examination subtracted from the logMAR VA at baseline.
Results
The changes in BCVA (in logMAR units), FT, and mean retinal sensitivity at baseline and at 3 months after SMDLP are presented in Table 1. Although the BCVA improved significantly (P=0.03) and the OCT-determined FT decreased significantly (P=0.0043) after SMDLP, the mean retinal sensitivities within the central 10 degrees did not improve significantly (P=0.70).
Among the 28 patients treated with SMDLP, 7 patients (25%) had an improvement of BCVA of >0.2 logMAR units and 21 patients (75%) remained unchanged at 3 months after SMDLP. Eleven patients (39%) had an improvement of mean retinal sensitivity in the central 10 degrees of >2 dB, 7 patients (25%) remained the same, and 10 patients (36%) had a reduction 3 months after SMDLP.
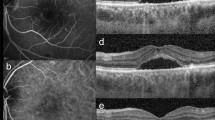
The OCT images and microperimetric results obtained from a 56-year-old woman before and 3 months after SMDLP are shown in Figure 1. Her VA improved slightly from 20/30 to 20/25 at 3 months after SMDLP, and the mean retinal sensitivity within the central 10 degree improved from 14.6 dB at baseline to 17.0 dB at 3 months after SMDLP.
OCT images and microperimetric images from a 56-year-old woman whose VA was reduced to 20/60 because of DMO in her right eye. (Top left) OCT image before SMDLP shows cystoid macular oedema and hard exudates. (Top right) OCT image 3 months after SMDLP shows a reduction of the macular oedema. (Bottom left) Microperimeter 1 (MP1) image before treatment. Mean retinal sensitivity within the central 10 degree is 14.6 dB before SMDLP. (Bottom right) Mean retinal sensitivity improved to 17.0 dB at 3 months after SMDLP.
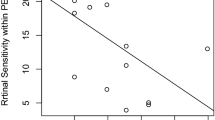
The relationship between the changes in retinal sensitivity from the baseline after SMDLP and changes from the baseline in the BCVA or FT after SMDLP are plotted in Figure 2a–c, respectively. The changes in the BCVA was not significantly correlated with the changes in FT (r=0.33, P=0.10) at 3 months after SMDLP (Figure 2a). The changes in retinal sensitivities within the central 10 degrees were also not significantly correlated with the changes in FT (r=−0.29, P=0.15) at 3 months after SMDLP (Figure 2b). The correlation between the changes in retinal sensitivity and the BCVA was not significant (r=0.29, P=0.16) at 3 months after SMDLP (Figure 2c).
(a) Relationship between changes in BCVA and changes in FT. The correlation between these two parameters is not significant (r=0.33, P=0.10). (b) Relationship between changes in retinal sensitivity and changes in FT. The correlation between these two parameters is not significant (r=−0.29, P=0.15). (c) Relationship between changes in BCVA and changes in retinal sensitivity. The correlation between these two parameters is not significant (r=0.29, P=0.16).
The correlations between changes in retinal sensitivity and the preoperative FT (r=0.29, P=0.15) and between changes in BCVA and the preoperative FT (r=0.12, P=0.56) were also not significant.
Before SMDLP, a serous retinal detachment was detected at the fovea by OCT in 6 patients, and cystoid macular oedema without retinal detachment was observed in 22 patients. There was no significant difference in the improvement of BCVA, FT, and retinal sensitivity between patients with and without a serous retinal detachment (Table 2).
Ophthalmoscopic examinations at the baseline showed an accumulation of hard exudates within the foveal avascular zone in 10 patients. Comparisons of the mean change in BCVA, FT, and retinal sensitivity did not show any significant difference between patients with an accumulation of hard exudates and those without (Table 3).
Postoperative fundus photographs and fluorescein angiograms did not show any evidence of laser treatment in all patients. No complication related to SMDLP was observed postoperatively.
Discussion
A significant improvement in the BCVA and a significant reduction in the FT were found at 3 months after SMDLP for DMO. However, the mean retinal sensitivity within the central 10 degrees did not improve significantly. These findings indicate that there is a difference in the changes of the resolution at the fovea and those of the retinal sensitivity around the macular area.
We have reported that a significant correlation existed between the retinal sensitivity measured by fundus-related microperimetry and the BCVA or FT in normal eyes and eyes with DMO.9 Similar results were also reported by Vujosevic et al.10 We had concluded that the retinal sensitivity may be another measure that can be used to assess the effects of DMO. In both studies, the patients with DMO had not undergone any treatment for their macular oedema; however, in this study, the results of SMDLP on the VA and retinal sensitivity were different. Although the BCVA improved significantly along with the reduction of FT, the retinal sensitivity from a larger area around macula did not change significantly.
Similar findings were observed in two other studies on DMO patients who had undergone vitrectomy with the creation of a posterior vitreous detachment.11, 12 We assessed the macular function by multifocal electroretinography (mfERG) and found that the electrical responses obtained from the macular area were also significantly correlated with the FT.11 In that electrophysiological study, we examined the macular mfERG from the central 10 degrees along with the VA and OCT-determined FT. Although the VA improved significantly and the FT was reduced significantly at 6 months postoperatively, the amplitude of the mfERGs did not show any significant change, and only the peak latency of the macular response decreased significantly.12 It was concluded that the recovery of the macular electrical response might be limited to the shortening of the implicit time because of the severely depressed macular function due to the chronic oedema.
In this study, there was no significant correlation between the preoperative FT and the postoperative improvement of the VA and retinal sensitivity. There was also no significant difference in the changes of VA and retinal sensitivity between eyes with serous macular detachment and those without, or between eyes with hard exudates and those without. These results indicated that such preoperative morphological changes did not alter the effects of SMDLP. The preoperative duration of the DMO may be a more important factor, which determines the permanence of the macular visual dysfunction, and it might affect the results of the treatments. However, it is not possible to determine the duration because most of the DMO patients were referred from other ophthalmologists. There was no significant difference in the efficacy of the SMDLP between eyes with macular detachment and those without, or between eyes with an accumulation of hard exudates within the foveal avascular zone and those without. Thus, our results indicate that the SMDLP had a therapeutic efficacy even in eyes severely damaged by macular oedema.
In patients with DMO after grid laser photocoagulation, Striph et al.13 examined the retinal sensitivity using the Humphrey field analyser. They concluded that VA and foveal sensitivity were preserved at the expense of generalized loss of retinal sensitivity across the central 10 degrees of visual field. Using fundus-related microperimetry, loss of retinal sensitivity in the grid laser spots might be proved. In this study, significant improvement of VA and preservation of retinal sensitivity within the central 10 degrees were observed after SMDLP. Thus, SMDLP may be more effective than grid laser photocoagulation for the treatment of eyes with DMO.
In conclusion, although our results showed that the SMDLP is effective in the reduction of macular oedema, the functional improvement was limited to the improvement of VA, and there was no improvement in the retinal sensitivity in the macular area. The combination of retinal sensitivity and VA may be beneficial in assessing the visual function in eyes with DMO.
References
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol 1985; 103: 1796–1806.
Schatz H, Maderia D, McDonald HR, Johnson RN . Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Arch Ophthalmol 1991; 109: 1549–1551.
Rutledge BK, Wallow IHL, Poulsen GL . Sub-pigment epithelial membranes after photocoagulation for diabetic macular edema. Arch Ophthalmol 1993; 111: 608–613.
Friberg TR, Karatza EC . The treatment of macular disease using a micropulsed wave 810-nm diode laser. Ophthalmology 1997; 104: 2030–2038.
Pollack JS, Kim JE, Pulido JS, Burke JM . Tissue effects of subclinical diode laser treatment of the retina. Arch Ophthalmol 1998; 116: 1633–1639.
Laursen ML, Moeller F, Sander B, Sjoelie AK . Subthreshold micropulse diode laser treatment in diabetic macular oedema. Br J Ophthalmol 2004; 88: 1173–1179.
Luttrull JK, Musch DC, Mainster MA . Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular oedema. Br J Ophthalmol 2005; 89: 74–80.
Luttrull JK, Spink CJ . Serial optical coherence tomography of subthreshold diode laser micropulse photocoagulation for diabetic macular edema. Ophthalmic Surg Lasers Imaging 2006; 37: 370–377.
Okada K, Yamamoto S, Mizunoya S, Hoshino A, Arai M, Takatsuna Y . Correlation of retinal sensitivity measured with fundus-related microperimetry to visual acuity and retinal thickness in eyes with diabetic macular edema. Eye 2006; 20: 805–809.
Vujosevic S, Midena E, Pilotto E, Radin PP, Chiesa L, Cavarzeran F . Diabetic macular edema: correlation between microperimetry and optical coherence tomography findings. Invest Ophthalmol Vis Sci 2006; 47: 3044–3050.
Yamamoto S, Yamamoto T, Hayashi M, Takeuchi S . Morphological and functional analyses of diabetic macular edema by optical coherence tomography and multifocal electroretinograms. Graefes Arch Clin Exp Ophthalmol 2001; 239: 96–101.
Yamamoto S, Yamamoto T, Ogata K, Hoshino A, Sato E, Mizunoya S . Morphological and functional changes of the macular after vitrectomy and creation of posterior vitreous detachment in eyes with diabetic macular edema. Doc Ophthalmol 2004; 109: 249–253.
Striph GG, Hart Jr WM, Olk RJ . Modified grid laser photocoagulation for diabetic macular edema. The effect on the central visual field. Ophthalmology 1988; 95: 1673–1679.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest: None.
Rights and permissions
About this article
Cite this article
Nakamura, Y., Mitamura, Y., Ogata, K. et al. Functional and morphological changes of macula after subthreshold micropulse diode laser photocoagulation for diabetic macular oedema. Eye 24, 784–788 (2010). https://doi.org/10.1038/eye.2009.207
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.207
Keywords
This article is cited by
-
Pascal short-pulse plus subthreshold endpoint management laser therapy for diabetic macular edema: the “sandwich technique”
International Journal of Retina and Vitreous (2022)
-
Real-life outcomes of subthreshold laser therapy for diabetic macular edema
International Journal of Retina and Vitreous (2021)
-
A Review of Subthreshold Micropulse Laser for Treatment of Macular Disorders
Advances in Therapy (2017)
-
Randomised clinical trial evaluating best-corrected visual acuity and central macular thickness after 532-nm subthreshold laser grid photocoagulation treatment in diabetic macular oedema
Eye (2015)
-
Relationship between vision-related quality of life and microperimetry-determined macular sensitivity in patients with retinitis pigmentosa
Japanese Journal of Ophthalmology (2011)