Abstract
Purpose
To compare the effectiveness and safety of excimer laser trabeculotomy (ELT) ab interno vs selective laser trabeculoplasty (SLT) over 24 months of follow-up in patients with primary open-angle glaucoma (POAG) refractory to medical therapy.
Patients and methods
This prospective, randomized study included 30 consecutive eyes assigned randomly to either ELT or SLT group. ELT was carried out using a XeCl Excimer Laser with an emission wavelength of 308 nm. Eight spots were equally distributed at a distance of 500 μm from one another over the anterior trabeculum. The SLT patients were treated with a frequency-doubled q-switched neodymium : yytrium–aluminum–garnet laser (wavelength 532 nm). Approximately 50 adjacent, but not overlapping, laser spots were distributed over 180° of the trabecular meshwork, using an energy level ranging from 0.7 to 1.0 mJ per pulse. The main outcome measure was intraocular pressure (IOP) lowering after ELT and SLT. Success was defined as ⩾20% reduction in IOP without further glaucoma intervention.
Results
At 24 months, complete success rates were 53.3% for the ELT group and 40% for the SLT group (P=0.35, Fisher's exact test); qualified success rates were 33.3% for the ELT and 26.6% for the SLT group (P=0.5, Fisher's exact test).Mean IOP decreased from 25.0±1.9 to 17.6±2.2 mmHg (−29.6%; P<0.0001) in the ELT group and from 23.9±0.9 to 19.1±1.8 mmHg (−21%;P<0.0001) in the SLT group.
Conclusions
Both ELT and SLT proved to be effective techniques in the treatment of POAG refractory to medical therapy.
Similar content being viewed by others
Introduction
High intraocular pressure (IOP) often associated with open-angle glaucoma, can be ameliorated by laser treatment.1, 2 Recently, two new modalities of laser therapy, which have been developed to improve the aqueous outflow, are available in the market.3, 4, 5 The first one is the Excimer Laser Trabeculotomy (ELT) ab interno using a XeCl Excimer Laser AIDA (Glautec AG, Nürnberg, Germany) with an emission wavelength of 308 nm. ELT was developed to enhance the outflow facility by creating 0.5-mm holes through the anterior meshwork in the inner wall of Schlemm's canal with minimal thermal effects or necrosis of the trabecular meshwork (TM) tissue because of the evaporation associated with the denaturalization of organic structures and lack of coagulative damage to the TM.6, 7 Using this new technique, effective trabeculotomy has been produced in rabbit and in human eyes.8, 9, 10
The second one is the Selective Laser Trabeculoplasty (SLT), which uses the 532-nm frequency-doubled q-switched neodymium : yyttrium–aluminium–garnet laser (Trabeculas A.R.C. Laser GmbH, Germany), with a pulse duration in nanosecond range. Owing to specific characteristics such as wavelength of the light, as well as the power, and duration of the exposure, SLT delivers a short pulse duration of 3 ns that limits the conversion of energy to heat inducing a selective photoablation of cells with pigment in trabeculum.11, 12, 13 Ultrastructural analysis of the TM in human eyes after SLT showed no alteration of the collagen structure and central core regions of the trabecular beams with no evidence of coagulative damage of the trabecular structure.14, 15
To date, several reports comparing 180° SLT vs 180° ALT13, 16, 17, 18 and studies evaluating the efficacy and safety of ELT ab interno over one-half of the TM9, 19, 20 have been published.
To the best of our knowledge no randomized clinical trials comparing ELT ab interno and SLT have been reported. The aim of this prospective, randomized study is to compare the 2-year term efficacy and safety of ELT ab interno vs 180° SLT in the treatment of primary open-angle glaucoma (POAG) refractory to medical therapy.
Patients and methods
Between February, 2006 and September, 2006, 30 consecutive patients (12 men, 18 woman), aged from 58 to 73 years (mean age: 65.5±4.2), affected from POAG uncontrolled by maximum tolerated medical therapy, were recruited in this study. The enrolment was carried out at the Glaucoma Center of the Eye Department at S. Antonio Hospital in Padova, Italy. Only one eye in each patient was treated. The POAG diagnosis was formulated in the presence of an IOP ⩾22 mmHg, glaucomatous optic disc abnormalities (stereo photographs)21 associated with glaucomatous retinal nerve-fiber layer defects (StratusOCT, software version 3.0, 3.4 mm scanning circle protocol, Carl Zeiss Ophthalmic System Inc., Dublin, CA, USA)22 and/or glaucomatous visual field (VF) alterations (30-2 threshold program, statpac 2 software, single field analysis, Humphrey–Zeiss, San Leandro, CA, USA).23
The indications for ELT or SLT treatment were an increased IOP under maximum tolerated medical therapy, and non-compliance with medical therapy. The exclusion criteria were the following: narrow anterior chamber angle (Shaffer I-II); neovascularization of the iris; corneal diseases precluding an adequate view of the TM; advanced VF defects with scotoma within 10° of fixation; and split fixation. Patients in systemic steroid therapy were also excluded.
The randomization schedule and sequential numbering was generated using SAS version 8.2 (SAS Institute, Cary, NC, USA) program and stored in a locked cabinet. No previous ocular surgery or laser treatment was carried out in any patient. All ELT and SLT procedures were carried out by the same operator (SB).
Informed consent after a full explanation about the potential risks, benefits, and alternatives to the procedures, was obtained from all the patients. The study was approved by the local ethical committee and was conducted in accordance with the principles laid down in the 1964 Declaration of Helsinki.
One day before (baseline) and at all other scheduled visits (1 day, 1 week, and 1, 3, 6, 9, 12, 18, and 24 months after the treatment), the patients underwent Snellen's visual acuity assessment, Goldmann's applanation tonometry after topical anesthesia with 0.4% benoxinate in a single-dose solution, slit lamp evaluation, and gonioscopy by Goldmann's three-mirror lens. The baseline IOP was determined by the mean value of three consecutive measurements carried out by the same operator using the same tonometer and masked to the type of treatment. Visual acuity alteration was considered significant when a change of ⩾2 Snellen's lines was observed. Visual field was carried out before and every 6 months after the treatment.
At each follow-up visit, the number of medications prescribed was recorded, and any complication was noted and treated appropriately. Authors evaluating the patients at each follow-up were blinded to whether the patient had undergone ELT or SLT. ELT and SLT laser parameters are illustrated in Table 1.
The ELT treatment was carried out in the surgical room. The following procedure was carried out. Preservative free lidocaine 4% (lidocaine 4%, Alfa Intes, Napoli, Italy) was administered by touching the perilimbar area for few seconds with a cellulose sponge tip. A 1.2 mm incision was made either temporally or nasally at the superior limbus. Cohesive viscoelastic substance was injected in the anterior chamber to enlarge the intraocular spaces and to protect the ocular structures. Next, under microscope control the laser probe was gently inserted in the eye with the tip up to 2 mm from the trabecular meshwork and the indirect-view goniolens was placed on the cornea. Then the laser tip was brought into contact with the TM to apply the laser energy. Directing the aiming beam almost perpendicularly to the eye wall, eight laser spots, equally distributed at a distance of 500 μm from one another, were delivered to the anterior trabeculum. At the end of the procedure, the probe was withdrawn, the viscoelastic was removed and the anterior chamber was thoroughly washed-out.
Selective laser trabeculoplasty treatment was carried out after the administration of topical anesthesia with 0.4% benoxinate in a single-dose solution and application of Goldmann's three-mirror goniolens on the cornea with 1% methylcellulose. The Trabeculas A.R.C. laser, a frequency-doubled q-switched neodymium : yytrium–aluminum–garnet laser (wave length 532 nm) was applied according to the parameters listed in Table 1. Approximately 50 adjacent, but not overlapping, laser spots were distributed over 180° of the TM. The energy level for treatment was initially set at 0.7 mJ and ranged from 0.7 to 1.0 mJ. If the energy level was too high (demonstrated by cavitation bubbles), the pulse energy was decreased by increments of 0.1 mJ until minimal bubble formation was visualized. The total number of pulses delivered at each energy level and the total amount of energy delivered was indicated on the laser control panel.
Post-treatment management of both groups was similar. A topical steroid-antibiotic association with tobramicin and dexamethasone eyedrops (Tobradex, Alcon labs, Inc. Fort Worth, TX, USA) was prescribed four times daily for 14 days. Glaucoma therapy was gradually tapered off based on reduction in IOP.
Statistical analysis
The sample size was chosen to assure a power of 80% in detecting statistically significant difference between groups from the baseline. Data were reported as means±SD or as percentages. Results were analysed using unpaired t-test, χ2 test, Mann–Whitney U-test and analysis of variance (ANOVA) to test the differences between groups. Differences were considered significant when the P-value was ⩽0.05.
A treatment was defined to be successful if (1) IOP was lowered by ⩾20% with no additional glaucoma medical, laser, or surgical therapy (‘complete success’), and if (2) IOP was lowered by ⩾20% with or without additional glaucoma medical, laser, or surgical therapy (‘qualified success’). Patients considered to have failed treatment were those with an IOP drop <20% compared with baseline values or needing to increase the number of glaucoma medications from pretreatment levels.
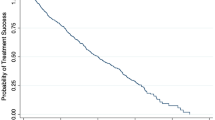
Adopting these criteria, we carried out Kaplan–Meier survival analyses and Fisher's exact test to compare outcomes between groups.
For randomization we adopted the intent-to-treat analysis, which also includes the patients who dropped out.
Results
The baseline characteristics of the two groups are summarized in Table 2. The ELT and SLT patients were similar in terms of age, sex, preoperative IOP, visual field parameters, and number of glaucoma medications. The mean follow-up time was 24.6±1.3 months for the ELT group and 24±1.6 months for the SLT group (ELT vs SLT: P=0.26; range: 22–26 months).
Figure 1 illustrates the mean IOP values at different time intervals after ELT or SLT. As compared with baseline value, in the eyes treated with ELT an IOP-lowering effect from 25.0±1.9 to 17.6±2.2 mmHg was observed at the last follow-up. The mean reduction of 7.4 mmHg, corresponding to −29.6% of the baseline value, resulted statistically significant (P<0.0001). Also in the eyes submitted to SLT, a significant decrease in mean IOP, from 23.9±0.9 to 19.1±1.8 mmHg, corresponding to −21% of the baseline value, was detected at the last follow-up (P<0.0001).
The Kaplan–Meier cumulative probabilities of success in the two groups are plotted in Figures 2 and 3. At 24 months, the cumulative probability of complete success was 53.33% for ELT (95% CI: 28,09—78,57%) vs 40% for SLT (95% CI:15,21—64,79%). Comparison of the survival curves for the complete success did not reveal any significant difference between the groups (P=0.35, Fisher's exact test). About qualified success, at 24 months it was 33,33% for ELT (95% CI: 9,6—57,06%) vs 26,67% for SLT (95% CI: 4,29—49,05%) (P=0.5, Fisher's exact test).
Before both laser treatments all patients received antiglaucoma therapy including topical β-blockers, α2 agonists, prostaglandin analogues, and carbonic anhydrase inhibitors. Table 2 shows the distribution of hypotensive drugs between the groups. In particular, 12 of 15 patients (80%) of ELT group and 8 of 15 patients (53.4%) of SLT group received β-blockers, whereas prostaglandins were used in 10 of 15 patients (66.7%) of ELT and 14 of 15 patients (93.4%) of SLT group, respectively. The distribution of the remaining antiglaucoma medications did not show a marked difference between the groups. At final examination, the mean number of IOP-lowering drugs significantly decreased from 2.27±0.6 to 0.73±0.8 in the ELT group and from 2.20±0.7 to 0.87±0.8 in the SLT group (ELT: P=0.005; SLT: P<0.0001).
Statistically significant differences in visual acuity were not found in any of the two groups at any time during the follow-up period. Consequent to the overall lack of significance, data are not shown.
The VF testing remained stable without significant progression in both groups over the follow-up period. The averaged MD changed from 9.5±2.3 to 9.4±2.4 decibels in the ELT group, and from 8.9±1.3 to 8.8±1.1 decibels in the SLT group. The averaged baseline CPSD of 5.6±2.5 db for ELT and 4.5±2.3 db for SLT, at the last follow-up was 5.4±3.6 db for ELT and respectively 4.4±2.8 db for SLT.
In the eyes treated by ELT, postoperative gonioscopy at 1 month showed rounded or ovoid holes with hyperpigmentation around the edge of the hole, stable throughout the follow up. No goniosynechias were detected.
In the SLT group no changes in the pigmentation of the meshwork or any peripheral anterior synechia was observed after the treatment.
Intra- and postoperative complications are summarized in Table 3.
In the ELT group, during the procedure a slight bleeding after each laser impact occurred in 12 of 15 eyes (80%). The bleeding was spontaneously adsorbed within the following 5 days without functional consequences. In 3 of these 15 patients (20%), a transient IOP increase no >5 mmHg and resolved within 48 h, was observed.
In the SLT group, 2 of 15 eyes (13.3%) had an IOP increase associated with a mild flare in the anterior chamber was recorded the first day postoperatively; in these 2 cases the IOP did not exceed 8 mmHg and normalized within 24 h.
Discussion
Although endowed with a different mechanism of action, both ELT ab interno and SLT induced a statistically significant IOP-lowering effect and improvement in mean antiglaucoma drug scores over 24 months' duration. In our series, there was no selection for laser treatment based on severity of glaucoma. This is supported by the statistically similar pretreatment IOP and medications.
Regarding the hypotensive efficacy of ELT ab interno, our results do not differ appreciably from those reported by other authors as Neuhann et al9 and Vogel and Lauritzen6 showing results similar to ours at 6 and 7 months, respectively, whereas recent studies involving eyes affected from POAG with cataract and submitted to combined ELT and cataract surgery, report success rates much better than ELT carried out alone.20, 24
Regarding the efficacy of SLT, previous studies report success rates varying from 64 to 89%.12, 13, 15, 16
In this study, at the end of the follow-up, the success rate was not significantly different between the ELT and SLT groups. However, considering the degree of IOP-lowering compared with the baseline, ELT seems to give better results than SLT and this could be ascribed to the following reasons.
First, the baseline IOP in the SLT group was lower than in the ELT group; this finding agrees with previous reports showing that eyes with higher baseline IOP benefit more from the laser treatment.16, 25
Second reason concerns the preoperative antiglaucoma therapy. A previous report by Melamed et al13 showed that after 18 months of follow-up, SLT induced a 30% reduction of IOP as a primary treatment in patients with POAG. In that study, the authors treated the nasal 180° of the TM using the same laser parameters we used in our SLT group. As reported by the authors, the high rate of success was because of the fact that their patients were newly diagnosed with untreated glaucoma or had a history of a single topical medication only. In this study the mean number of IOP-lowering drugs before SLT was 2.20±0.7 and in many cases the drugs were prostaglandin (93.4%). Both laser trabeculoplasty and prostaglandins act by increasing the uveoscleral outflow by regulating the secretion of metalloproteinases and stimulating TM tissue.26, 27 The biochemical theory, supports the hypothesis that the action of the SLT associated with previous prostaglandin use induce a supersaturation and subsequent depletion of the metalloproteinases, yielding a decreased ability of the conventional outflow system to respond to the laser treatment. More recently, studies by Nagar et al28 and McItraith et al5 comparing SLT vs latanoprost as initial therapy, have suggested comparable efficacy in IOP reduction of about 30% below baseline levels.
In our study, both the techniques were carried out over one-half of the TM and were never repeated. The technical aspects, the difficulties encountered by the surgeon to exactly position the probe on the trabeculum just posterior to Schwalbe's line and to correctly localize the laser impact during the ELT procedure, have already been reported in detail.19
Selective laser trabeculoplasty is repeatable. During the SLT procedure, the laser impact cannot be clearly visualized with the risk of an over- or underdosage without a therapeutic effect. On the contrary, an evidence of successful perforation by ELT is the occurrence of microbleedings during laser spot applications. In fact, blood can be present in Schlemm's canal in some physiological conditions, and can also reach the anterior chamber through the holes made by ELT. This haemorrhagic reflux from Schlemm's canal is the proof that the holes created by the excimer laser in the inner wall of the Schlemm's canal are open. However, ELT needs for a sterile surgical procedure and is not repeatable if compared with SLT.
Recently, the first case of hyphema occurring during SLT in an eye without neovascularization was described. The hyphema resolved spontaneously without any sequel and with a good IOP control. This fact confirms the possibility of complications occurring after ELT or SLT, as with any operative procedure. Therefore, careful monitoring of the IOP and the anterior chamber reaction are advisable.29
In our study, at the end of the follow-up period, visual acuity and visual field had not changed and gonioscopy did not detect any scarring or development of peripheral anterior sinechiae. This confirms the strong safety profile of both ELT ab interno and SLT.
In conclusion, the results of our study appear to confirm that both ELT and SLT are effective and safe laser treatments of refractory POAG, proving to be viable alternative to current, much more traumatic surgical procedures. However, prospective randomized studies involving a larger group of patients affected from medically uncontrolled POAG, are required to support the findings of this study.
Conflict of interest
The authors declare no conflict of interest.
References
Van Buskirk EM . Pathophysiology of laser trabeculoplasty. Surv Ophthalmol 1989; 33: 264–272.
Wilensky JT . Laser trabeculoplasty. In: Podos SM, Yanoff M, Kaufman PL, Mittag TW (eds). Textbook of Ophthalmology. CV Mosby: St Louis, MO, USA, 1994; 7: 9.31–9.42.
Johnson PB, Katz LJ, Rhee DJ . Selective laser trabeculoplasty: predictive value of early intraocular pressure measurements for success at three months. Br J Ophthalmol 2006; 90: 741–743.
Kano K, Kuwayama Y, Mizoue S . Clinical results of selective laser trabeculoplasty. Nippon Ganka Gakkai Zasshi 1999; 103: 612–616.
McIlraith I, Strasfeld M, Colev G, Hutnik CM . Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma 2006; 15: 124–130.
Vogel M, Lauritzen K . Selective excimer laser ablation of the trabecular meshwork. Clinical results. Ophthalmologe 1997; 94: 665–667.
Walker R, Specht H . Theoretical and physical aspects of excimer laser trabeculotomy (ELT) ab interno with the AIDA laser with a wave length of 308 nm. Biomed Tech 2002; 47: 106–110.
Huang S, Yu M, Feng G, Zhang P, Qiu C . Histopathological study of trabeculum after excimer laser trabeculectomy ab interno. Yan Ke Xue Bao 2001; 17: 11–15.
Neuhann Th, Scharrer A, Haefliger E . Excimer laser trabecular ablation ab interno (ELT) in the treatment of chronic open-angle glaucoma. A pilot study. Ophthalmo-Chirurgie 2001; 13: 3–7.
Vogel M, Lauritzen K, Quentin CD . Targetted ablation of the trabecular meshwork with excimer laser in primary open-angle glaucoma. Ophthalmologe 1996; 94: 565–568.
Latina MA, Park C . Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res 1995; 60: 359–372.
Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G . Q-switched 532-nm Nd:YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter, pilot, clinical study. Ophthalmology 1998; 105: 2082–2088, discussion 2089-90.
Melamed S, Simon GJB, Levkovitch-Verbin H . Selective laser trabeculoplasty as primary treatment for open-angle glaucoma. Arch Ophthalmol 2003; 121: 957–960.
Cvenkel B, Hvala A, Drnovsek-Olup B, Gale N . Acute ultrastructural changes of the trabecular meshwork after selective laser trabeculoplasty and low power argon laser trabeculoplasty. Lasers Surg Med 2003; 33: 204–208.
Kramer TR, Noecker RJ . Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology 2001; 108: 773–779.
Damji KF, Shah KC, Rock WJ, Bains HS, Hodge WG . Selective laser trabeculoplasty v argon laser trabeculoplasty: a prospective randomized clinical trial. Br J Ophthalmol 1999; 83: 718–722.
Juzych MS, Chopra V, Banitt MR, Hughes BA, Kim C, Goulas MT et al. Comparison of long-term outcomes of selective laser trabeculoplasty vs argon laser trabeculoplasty in open-angle glaucoma. Ophthalmology 2004; 111: 1853–1859.
Martinez-de-la-Casa J, Garcia-Feijoo J, Castillo A, Matilla M, Macias JM, Benitez-del-Castillo JM et al. Selective vs argon laser trabeculoplasty: hypotensive efficacy, anterior chamber inflammation, and postoperative pain. Eye 2004; 18: 498–502.
Babighian S, Rapizzi E, Galan A . Efficacy and safety of ab interno excimer laser trabeculotomy in primary open-angle glaucoma: two years of follow-up. Ophthalmologica 2006; 220: 285–290.
Wilmsmeyer S, Philippin H, Funk J . Excimer laser trabeculotomy: a new, minimally invasive procedure for patients with glaucoma. Graefe's Arch Clin Exp Ophthalmol 2005; 19: 1–7.
Jonas JB, Gusek GC, Naumann GOH . Optic disc morphometry in chronic open-angle glaucoma. I. Morphometric intrapapillary characteristic. Graefe's Arch Clin Exp Ophthalmol 1988; 226: 522–530.
Guedes V, Schuman JS, Hertzmark E, Wollstein G, Correnti A, Mancini R et al. Optical coherence tomography measurement of macular and nerve fiber layer thickness in normal and glaucomatous human eyes. Ophthalmology 2003; 110: 177–189.
Hodapp E, Parrish IIRH, Anderson DR . Clinical Decisions in Glaucoma. The CV Mosby: St Louis, MO, USA, 1993; 84–126.
Sourdille P . Study shows ab interno excimer trabeculotomy lowers, controls IOP. Ocular Surgery News, Europe/Asia-Pacific edition 2001; 12: 28.
Rubin MP, Lafayette SR, Albanis CV et al. Pre-operative Pressure as a Significant Determinant of SLT Efficacy—The University of Chicago SLT study. ARVO. Fort Lauderdale, FL, USA, Invest opthalmol Vis Sci 2004; 45: E-abstract 4462.
Birkedal-Hansen H, Moore WG, Bodden MK,, Windsor LJ, Birkedal-Hansen B, Decarlo A et al. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med 1993; 4: 197–250.
Weinreb RN, Lindsey JD, Kashiwagi F, Sagara T, Gaton DD . Prostaglandin effects on the uveoscleral outflow pathway. In Krieglstein GK (eds) Glaucoma Update. Sprinter Verlag: Berlin, Germany, 1999; 197–202.
Nagar M, Ogunyomade A, O'Brart DP, Howes F, Marshall J . A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol 2005; 89: 1413–1417.
Shihadeh WA, Ritch R, Liebmann JM . Hyphema occuring during selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging 2006; 37: 432–433.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Babighian, S., Caretti, L., Tavolato, M. et al. Excimer laser trabeculotomy vs 180° selective laser trabeculoplasty in primary open-angle glaucoma. A 2-year randomized, controlled trial. Eye 24, 632–638 (2010). https://doi.org/10.1038/eye.2009.172
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.172
Keywords
This article is cited by
-
Systematic review of the method and quality of reporting of complications from studies evaluating innovative glaucoma surgical procedures
Eye (2023)
-
The AIDA and the extra laser systems for excimer laser trabeculotomy proved comparable IOP lowering efficacy—12-month results
International Ophthalmology (2022)
-
Long-term treatment success and safety of combined phacoemulsification plus excimer laser trabeculostomy: an 8-year follow-up study
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Long-term follow-up of intraocular pressure and pressure-lowering medication in patients following Excimer laser trabeculotomy
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Selective Laser Trabeculoplasty Versus MIGS: Forgotten Art or First-Step Procedure in Selected Patients with Open-Angle Glaucoma
Ophthalmology and Therapy (2021)