Abstract
Purpose
To investigate whether the tickling inside the nose before a light-induced sneeze in susceptible individuals is correlated to a recordable local activity or not.
Methods
Seven healthy volunteers, three with a history of light-induced sneezing, were stimulated with stroboscopic light or a strong halogen lamp. Recording was done with an evoked potential averaging technique via intranasal electrodes placed in such a way that they substantially reduced the strong electrical response from the retina.
Results
Despite an adequate light stimulus, no reproducible electrical activity could be recorded from any of the members in any experiment.
Conclusion
Light-induced sneezing is presumably a central phenomenon. The electrical activity travels through the optic pathways straight to the trigeminal nucleus and the tickling is a referred sensation. A genetic variation in the distance between the optic pathways (colliculus superior) and the mesencephalic part of the trigeminal nucleus may explain why light-induced sneezing is more common in certain families and races.
Similar content being viewed by others
Introduction
Light-induced sneezing (=The photic sneeze reflex=Photo-sternutatory reflex=ACHOO-reflex/Autosomal dominant Compelling HelioOphtalmic Outburst/) in humans, with or without a positive heredity, is well-known to ophthalmologists. To most of affected people it is just a nuisance, but it may be hazardous for pilots and car-drivers.1, 2 In an American Study on medical students, 28% of white males reported light-induced sneezing compared with 16% of white females.3 The prevalence was higher among those with a family-history. Only 2% of black males and females had a history of light-induced sneezing. According to a Swedish study 24% of blood donors experienced sneezing on visual exposure to strong light.4 The family data in this study suggested an autosomal dominant mode of inheritance.
What is the cause to this odd sneeze without obvious function? Why does it vary in frequency among families and races?
Everett (1964)3 seems to be alone in trying to approach the cause of light-induced sneezing by establishing two theories. His first theory is that light provokes a parasympathetic stimulation through the ganglion sphenopalatinum, causing congestion and secretion inside the nose. This in turn irritates the trigeminal nerve endings with a resulting sneeze. His second theory is that stimulation of the optic nerve in some way affects the trigeminal nucleus by central pathways with a subsequent sneeze, and that the tickling that is felt before the sneeze is a referred sensation.3
Despite the fact that this is a common phenomenon, knowledge about its neurophysiological background is still lacking. To test one theory, we have carried out an experiment in ‘light-sneezers’ that addresses the question whether their reported tickling inside the nose before a light-induced sneeze correlates to a local electrical activity that can be recorded. If so, this would speak in favour of Everett's first theory that a local stimulation of nerve-endings inside the nose triggers the sneeze. If not, a central cause is more probable, where the tickling is a referred sensation.
Material and methods
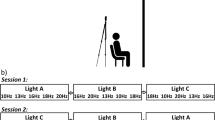
In all seven healthy members of our research team were tested. Three had light-induced sneezing. They were all highly motivated to participate and well informed of the nature of the research including the minimal risks involved. As stimulus we used either a stroboscopic light (Brüel and Kjaer) with a frequency of 5–10/s with the lamp held about 30 cm from the member's eyes or a halogen lamp (12V, 20W, and luminous intensity 2300cd) placed about 10 cm from the member's eyes. Recording was done with two gold electrodes (Grass) placed in the left nasal cavity, one reference Ag/AgCl-electrode on each cheek, and with one ground electrode in the forehead. To substantially reduce the strong electric response from the retina in the time domain from 15 to 250 ms by light-stimulation, one electrode was placed on the medial side of the nasal septum and another on the lateral side 3–4 cm from the orifice and with a silicone sheet in between. In that way both electrodes picked up nearly the same electric signal from the retina. Recording of electric activity was done with the evoked potential averaging technique with a sweep-duration of 50 or 100 ms and with a 5–10/s repetition rate.
Results
At several occasions both tickling and sneezing were provoked by the applied light in the ACHOO-members, indicating that the stimulus was adequate. These members reported that the tickling appeared immediately after the stimulus was switched on. However, no reproducible electrical activity evoked by light stimulation could be recorded in the nose from any of the members in any of the experiments.
Discussion
The tickling that precedes a normal sneeze should correlate to a neural response in the trigeminal nerve. As such, it ought to be possible by a sensitive technique to measure an electrical response in the distribution area of that nerve. Practically, a reliable experimental setup inside the narrow nasal space, with for instance a controlled pressure on the actual sensory area to verify that the tickling is synonymous with a neural response, is not possible in man. Introducing a strong odour or chemical inside the nose would be a way to stimulate the nerve endings and simultaneously measure any response. However, such a procedure will first of all stimulate the organ of smell giving rise to a response in the first cranial nerve. The trigeminal nerve endings inside the nose are not primarily aimed at responding to smells. To reach such a level from a smell or a chemical, concentrations have surely to be used making the experiment intolerable. Our experimental set-up with a controlled light-stimulus far away from the recording site in the nose allows a reliable experimental situation if the strong electrical retinal response during light-stimulation is minimized, as we have tried to do.
As light stimulation did not cause a simultaneous electric response inside the nose, neither in ACHOO-members nor in members who lack light-induced sneezing, Everett's theory of a local, inside the nose, triggered response seems less probable. The phenomenon is presumably a central one.
Where inside the brain can light stimulate the individual to feel a tickling in the nose that is followed by a sneeze? Why does this light-induced sneezing occur more commonly in some families and races? To try answering these questions we have to consider what is known about the neural pathways in sneezing in general.
Sneezing is normally triggered by stimulation from infectious agents, mechanically by nose-picking, or during rhinological examination of the anterior part of the internal nose. Experimentally, sneezing can be elicited by electric stimulation directly applied to the foremost part of the trigeminal nerve (the anterior ethmoidal nerve) or to the cutaneous membrane area controlled by the same nerve both in cats and humans.5, 6 From the nose, the signal travels to the brainstem area. According to experiments on cats a sneeze-evoking area has been found situated bilaterally along the ventromedial spinal trigeminal nuclei and in the adjacent pontomedullary lateral reticular formation.7 In humans there are no experimental data. The observation that some patients with Wallenberg's syndrome lack the ability to sneeze, indicates that there is a sneeze-centre in the corresponding area in humans.8 The loss of the sneeze-reflex in these patients with a unilateral damage suggests that in man both right and left centres must be intact for a sneeze to occur. One patient with systemic lupus erythematosus (SLE) reported inability to sneeze. An MRI showed a brainstem demyelination in the dorsolateral medulla.9
The only experimental data on light-induced sneezing comes from a study by Morris, who in a woman with an ACHOO-positive history found the latency between a flash-light stimulation of 15 Hz to a sneeze-response, noted as an EMG-artefact on an EEG-curve, to be about 10 s. From this finding Morris concluded that the reflex must have a polysynaptic pathway.10 However, as the tickling comes instantly after switching on the light, there must be a much more direct connection than indicated by the delay between light and sneeze as shown by Morris. Along which pathway does the signal travel from the eyes to reach the sneeze-centre in the brainstem?
We presume that the electrical signal follows the optic pathways posteriorly to the superior colliculus, which is in the vicinity of the mesencephalic part of the nucleus of the fifth nerve. From there the signal travels inside the trigeminal nucleus to the pontomedullary located sneeze-centre. The tickling is a referred sensation due to the optico-trigeminal stimulation. A genetic variation in distance between the superior colliculus and the nucleus of the fifth nerve may explain why this phenomenon is more common in certain families and races.
Our expectation is that this early scientific approach to a scientifically unknown but very common phenomenon in man will inspire others to further investigations.
References
Benbow EW . Practical hazards of photic sneezing. Br J Ophtalmol 1991; 75: 447.
Breitenbach RA, Swisher PK, Kim MK, Patel BS . The photic sneeze reflex as a risk factor to combat pilots. Mil Med 1993; 158: 806–809.
Everett HC . Sneezing in response to light. Neurology (Minneap) 1964; 14: 483–490.
Beckman L, Nordenson I . Individual differences with respect to the sneezing reflex: an inherited physiological trait in man? Hum Hered 1983; 33: 390–391.
Batsel HL, Lines J . Neural mechanisms of sneeze. Am J Physiol 1975; 229: 770–776.
Hydén D, Arlinger S . On the sneeze-reflex and its control. Rhinology 2007; 45: 218–219.
Nonaka S, Unno T, Ohta Y, Mori S . Sneeze-evoking region within the brainstem. Brain Res 1990; 511: 265–270.
Hersch M . Loss of ability to sneeze in lateral medullary syndrome. Neurology 2000; 54: 520–521.
Fink J . Localization of the ‘sneeze center’. Neurology 2001; 56: 138.
Morris HH . ACHOO syndrome: laboratory findings. Cleve Clin J Med 1989; 56: 743–744.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hydén, D., Arlinger, S. On light-induced sneezing. Eye 23, 2112–2114 (2009). https://doi.org/10.1038/eye.2009.165
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.165
Keywords
This article is cited by
-
Practical experience on emergency ophthalmic surgery during the prevalence of COVID-19
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)