Abstract
Purpose
To evaluate results of 23-gauge transconjunctival sutureless vitrectomy in various indications of vitreoretinal diseases.
Design
Prospective, non-comparative study.
Materials and methods
Fifty-seven consecutive eyes of 57 patients underwent vitreoretinal surgery by one surgeon using the 23-gauge, two-step instrumentation developed by Dutch Ophthalmic Research Center Inc., for epiretinal membranes (n=24), macular holes (n=10), diabetic retinopathy (n=4), rhegmatogenous retinal detachment (n=3), silicone oil removal (n=10), and other procedures (n=4). Mean operative time and intraoperative and postoperative complications were recorded. At 1 month, postoperative visual acuity, anatomical results, and induced astigmatism measured by Orbscan (BAUSCH and LOMB laboratories Inc., Rochester, NY, USA) were analysed.
Results
Mean operative time was 32.6±21.5 min. At 1 month, mean visual acuity improved from 1.09±0.82 to 0.80±0.79 logMar. Transient postoperative hypotony was the most common complication (21.1%), resolving without treatment. There was no choroidal effusion; and no postoperative endophthalmitis was observed. There were no significant changes in mean keratometry (P=0.957), mean axis (P=0.818), and power of astigmatism (P=0.860) at 1 month.
Conclusions
A 23-gauge vitrectomy seems to be safe and effective for a wide range of indications for vitreoretinal surgery. Further studies are needed to compare it with 25-gauge and 20-gauge vitrectomy in larger series.
Similar content being viewed by others
Introduction
Pars plana transconjunctival sutureless vitrectomy is becoming more and more popular. This surgical procedure has been developed to be less invasive and to improve the postoperative recovery of patients.
The first system described was the 25-gauge transconjunctival sutureless vitrectomy by Fujii et al1, 2 in 2002. They showed the suitability and safety of this procedure for surgical vitreoretinal diseases with no specific complications. However, the 23-gauge vitrectomy system has since been developed because the relative flexibility of the 25-gauge instruments allowed less practical surgery than the conventional 20-gauge vitrectomy.3
We evaluate the safety of this technique and its surgical use for different indications of vitreoretinal diseases and analyse the induced astigmatism.
Materials and methods
We present a consecutive case series (non-comparative prospective) study done at the University Hospital of Bordeaux (France) from October 2006 to March 2007. Fifty-seven consecutive eyes of 57 patients underwent 23-gauge vitrectomy by one trained surgeon (JF Korobelnik) for various indications of vitreoretinal diseases. Indications included idiopathic epiretinal membrane (n=26), macular hole (n=10, three cases of stage 3, seven cases of stage 4), diabetic retinopathy with vitreous haemorrhage, proliferative retinopathy, or other vitreoretinal tractions (n=4, one case was combined with a cataract extraction), rhegmatogenous retinal detachment (n=3, two cases with a macular detachment, one complex case with a vitreoretinal proliferation classified C4), silicone oil removal (n=10, four cases associated with a peeling of a macular pucker, one case combined with a cataract extraction), and four other indications (one case of neovascular glaucoma after a central retinal vein occlusion; one case of Terson syndrome with a retro-hyaloidal haemorrhage; one case of vitreoretinal traction consecutive to a congenital toxoplasmosis, this case was combined with a cataract extraction; one case of retinal detachment consecutive to an acute endophtalmitis). At the beginning of the study, the inclusion of patients was limited because the endolaser probe was not available. Occurrences of foreign intraocular bodies and lens luxation in the vitreous body were excluded from the study.
For all cases, we used the three-port 23-gauge vitrectomy system and instrumentation developed by Eckardt and DORC® (Dutch Ophthalmic Research Center Inc., Zuidland, The Netherlands) with its two-step incision, as initially described in a previous study.3 The vitrectomy system for all surgeries was the Accurus surgical system (ALCON Laboratories Inc., Fort Worth, Texas, USA) calibrated at 400 mm Hg of vacuum and with a cut rate of 1500 per minute. For the cases of macular puckers and macular holes, we performed the epiretinal membrane and internal limiting membrane peels with triamcinolone as a vital dye. Phacoemulsification was applied for cataract surgery, when necessary, before the 23-gauge procedure in three eyes. When a retinal dehiscence occurred or was discovered during peripheral vitrectomy, we performed an internal retinopexy by endolaser or an external procedure by cryotherapy. For all cases of macular hole, we used a tamponade by gas with the head in a face-down postoperative position for 1 week. The gas tamponade was also applied for two cases of retinal detachment and one case of diabetic retinopathy. One of the retinal detachment cases required a tamponade by silicone oil (1000 cs). See Table 1 for the details of each procedure.
We evaluated the visual acuity of each eye preoperatively with the Monoyer scale. For analysis, these results were converted into the logarithm of the Minimum Angle of Resolution (logMAR). A clinical exam was performed and optical coherence tomography (OCT) was done for idiopathic epiretinal membrane, macular holes, and other vitreoretinal tractions. The day after surgery, we evaluated the conjunctiva and the incisions with and without fluorescein adjunction, inflammation state, intraocular pressure (IOP), and anatomic result by ocular fundus examination.
One month postoperatively, we carried out a clinical exam using the same criteria as the preoperative exam. We evaluated visual acuity by Monoyer scale converted to a logarithmic scale; we recorded anatomic clinical results; and we performed an evaluation by OCT for those cases that had received OCT preoperatively.
We evaluated the astigmatism induced by the 23-gauge procedure with a corneal exam by Orbscan® (Bausch and Lomb Laboratories Inc., Rochester, NY, USA) preoperatively and at 1 month postoperatively in 20 eyes operated for idiopathic epiretinal membranes or macular holes. Eyes operated for retinal detachment, diabetic retinopathy, silicone oil extraction, combined procedures, corneal diseases, and scars were excluded. The mean keratometry, keratometry of the two main axes (K1, K2), and degree of astigmatism and its power were analysed and compared with the statistical method of Wilcoxon. Differences between preoperative and postoperative values were considered as statistically significant with P<0.05.
At 1 month, two patients in the idiopathic epiretinal membrane group returned for follow-up because of general diseases independent of the ophthalmologic management.
Results
The mean operating time was 32.6 min with times varying across the indications. The shortest operating times were 21.92±9.17 min for idiopathic epiretinal membranes and 29±6.99 min for macular holes; for retinal detachments the operating time was 71.67±27.54 min. The other mean operating times were 67±34.7 min for diabetic retinopathy, 28.88±7.82 min for silicone oil extraction, and 51.25±10.31 min for other indications (Figure 1).
At 1 month, we had an improvement of the mean visual acuity for each indication (Figure 2), and above all for idiopathic epiretinal membranes, from 0.53±0.27 to 0.33±0.25 logMar.
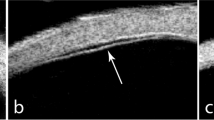
We successfully peeled the idiopathic epiretinal membranes without any complications during the procedure or follow-up. For all cases of membrane peeling there was an improvement in the OCT profile, reduction of macular oedema with a mean foveolar thickness of 321.4±70.9 μm at 1 month (mean preoperative foveolar thickness 395.3±89.8 μm), and a better foveolar morphology.
Macular holes were successfully sealed at 1 month in 80% of our cases without any residual vitreomacular traction on the OCT profile. One case had a recurrence of its macular hole because of a lack of internal limiting membrane peeling and above all a lack of compliance with positioning. The other case was highly myopic and developed retinal detachment from the macular hole, requiring repeated surgery.
In eyes with diabetic retinopathy, we observed no complications during the peeling of neovascular and fibrous tissues or during peripheral endolaser. We had no vitreoretinal traction or bleeding at 1 month.
In the three cases of rhegmatogenous retinal detachment, two retinas were reattached, with an improvement of the visual acuity at 1 month. These retinas were reattached, for the first case, with endolaser around the breaks and silicone oil tamponade, and for the second case with cryotherapy and a gas tamponade. The third eye presented a recurrence of retinal detachment at 1 month. The retina had been reapplied 8 days postoperatively, using a retinotomy of the vitreoretinal proliferation by the vitreous cutter and a retinopexy by endolaser with a gas tamponade. This was due to a recurrence of the vitreoretinal proliferation on the edge of the retinotomy and a lack of gas tamponade in the first postoperative days (postoperative IOP was less than 5 mm Hg with no gas under the conjunctiva). After removal of the cannulae, there was probably a gas leakage by the sclerotomies.
Silicone oil removal was achieved without any complications. In four eyes, we achieved peeling of the macular pucker, but in one the membrane was too adherent to the retina and could not be released. We observed two cases of recurrence of retinal detachment apparently not related to the 23-gauge surgical procedure. One was the fourth recurrence despite extensive endophotocoagulation, and the other was due to ocular trauma 8 days after the surgery.
The retrohyaloidal haemorrhage of the Terson syndrome was successfully removed with an improvement of the visual acuity from 1.6 to 0 logMar at 1 month. In the case of congenital toxoplasmosis, the vitreoretinal traction and the cataract were successfully released with an improvement of the visual acuity from 0.5 to 0.4 logMar at 1 month. Vitrectomy and endolaser were successfully performed in the case of neovascular glaucoma. We could not reapply the retina in the case of acute endophtalmitis because the tissue was too necrotic (Table 1).
During all the procedures, we observed three complications, all treated perioperatively, without any consequences for the anatomic result. In two cases, retinal breaks were made, one during peripheral vitrectomy. The other was the consequence of a sclerotomy located more than 4 mm from the limbus with the pressure plate too low. There was one conjunctival break at the entry site of a cannula needing a suture. None of the cases treated with 23-gauge procedures needed a scleral suture and none needed to be converted to a 20-gauge procedure.
Postoperative hypotony was the most common complication observed on day 1 after surgery. Twelve eyes (21.1%) had an IOP under 9 mm Hg, six of these were under 5 mm Hg (10.5%) without choroidal effusion at the ocular fundus and no flat anterior chamber. No treatment was performed and the hypotony resolved in a few days, for all the eyes, without any ocular consequences. Eleven of these eyes had no gas at the end of the procedure. Hypotony most frequently occurred (5 cases of 12) in eyes receiving peeling of the epiretinal membrane. Gas at the end of the procedure seemed to protect against hypotony: there was one case (7.7%) of hypotony for the 13 procedures with a gas tamponade (10 macular holes, two retinal detachments, one diabetic retinopathy for a retinal tear) and 11 cases (25%) for the other 44 procedures without gas. There were no silicone bubbles under the conjunctiva for the case of retinal detachment treated by silicone oil tamponade.
We observed three cases of minor inflammation (Tyndall+) and three cases of moderate inflammation (Tyndall++) of the anterior chamber, resolved with steroid drops. Three eyes had a minor conjunctival haemorrhage.
At 1 month, three retinal detachments recurred, two after silicone oil removal and one related to vitreoretinal proliferation on the edge of the initial retinal break. One case of macular hole surgery was complicated by a central retinal detachment. All the cases were considered not to be specific to the 23-gauge procedure.
We had two eyes with posterior lens opacification at 1 month, one related to gas tamponade and one induced by a crystalline lens touch during the introduction of the vitreous cutter through a cannula. There was no case of endophthalmitis in our series.
One month postoperatively, there was no significant statistical change in the corneal keratometry measured by Orbscan®. The preoperative mean keratometry power was 43.94±1.20 D and postoperative keratometry was 43.87±1.37 D (P=0.957). Mean induced astigmatism was 0.01 D at 6°. The mean power and angle of axis changes were not statistically significant (P=0.860; P=0.818) (Figure 3).
Discussion
Since the introduction of pars plana vitrectomy in 1971,4 one of the most important challenges has been to determine the best type of incision: which is the least invasive and with the best instrumentation function during the procedure. In the last decade, different types of self-sealing sclerotomies have been described to shorten the operating time, decrease IOP variation during instrumentation removal, and reduce conjunctival irritation induced by sclerotomy sutures.5, 6, 7, 8, 9 In 2002, the development of a transconjunctival sutureless pars plana vitrectomy with a 25-gauge system was another important step.1, 2 The incision was small enough to be self-sealing without any sutures, and above all with an oblique scleral tunnel,10, 11 allowing less invasive surgery with a decrease in the operating time and a faster postoperative recovery. The healing of sclerotomies was significantly faster with fewer inflammatory cells for a 25-gauge transconjunctival sutureless incision than for a 20-gauge incision.12, 13
The 23-gauge transconjunctival sutureless vitrectomy developed by Eckardt3 uses the same technique of an oblique scleral tunnel made by a stiletto blade but with insertion of the microcannulae in a second step. The oblique scleral incision and the decrease of its diameter from 20-gauge to 23-gauge allow a self-sealing and sutureless surgery. The use of microcannulae preserves the edge of the incision during the instrumentation procedure and the incarceration of a residual vitreous in the sclerotomies can also act as a plug.
In our study, the 23-gauge transconjunctival sutureless vitrectomy developed by Eckardt and DORC appeared safe, without any major complications related to the system. We observed a retinal tear after the insertion of the cannula in only one case. This was induced by a posterior position of the pressure plate, and treated perioperatively.
Transient postoperative hypotony was the most common complication and resolved in a few days. It was probably due to a fluid leakage of the sclerotomies in the hours following surgery (a fluorescein test was negative on the first postoperative day in all eyes). We had no severe complication related to hypotony, such as choroidal effusion, and no eyes needed any treatment. The hypotony concerned 12 eyes (21.1%) of our series, and gas tamponade seemed to protect the eye against hypotony at day 1. The rate of transient hypotony is higher for transconjunctival sutureless vitrectomy than for the conventional 20-gauge sutured vitrectomy and higher for the 23-gauge system than for the 25-gauge system.14 O’Reilly et al reported 25.6% of hypotony that spontaneously resolved without any complications, such as choroidal detachment or endophthalmitis, whereas Fine et al had a rate of 2.5% and used a gas tamponade for 52.9% of the procedures.15, 16 In our study, we have a high rate of transient hypotony linked to the low incidence of gas tamponade use in the procedures (22.8%). It confirms the protective role of gas tamponade against hypotony.
We had no cases of choroidal effusion and the incidence, in published studies, seems to be low between 0 and 1.8%.17 In an analysis of the wound closure of the sclerotomies by anterior segment OCT, Taban et al18 report a shallow choroidal effusion, not seen clinically, in the case of hypotony. Choroidal effusion is transitory, peripheral, and linked to hypotony; it resolves without any treatment.17, 18
The construction of the transconjunctival incision and of the sclerotomies (sufficiently oblique and long) is important to keep the sclerotomies self-sealed. The sclerotomy wounds seem closed on postoperative days 1 and 8,18 but some contamination of the entire length of the incision by the ocular surface fluid could occur.19
We observed no cases of endophthalmitis, but this complication has previously been described with a higher incidence for 25-gauge transconjunctival surgeries than the conventional 20-gauge sutured pars plana vitrectomy.20, 21, 22, 23 This rate of endophthalmitis ranges from 0.23 to 1.6% according to previous studies,22, 23 and most often appeared in 3 days immediately following surgery. Kunimoto et al noted that all eyes had a fluid-filled vitreous cavity at the end of surgery with no documented hypotony at day 1 of examination. Diabetes seems to be another risk factor.20, 21, 22 The presence of hypotony or of a bacterial proliferation from a residual vitreous incarceration in the sclerotomy sites has to be determined to decrease the risk of endophthalmitis in transconjunctival surgery.
The 25-gauge transconjunctival sutureless vitrectomy could induce some peripheral retinal break due to the type of incision. Vitreous incarceration in the sclerotomies could be responsible for anterior vitreoretinal traction.24, 25 We did not observe such complications in our series. The 23-gauge system permitted us to perform a more complete peripheral vitrectomy, with the help of better endo-illumination.
In our series, recurrences after retinal detachment surgery were not related to the 23-gauge system. Recurrences after silicone oil removal were due to traction on retinal tears previously treated in two eyes. They were related to limited gas tamponade associated with vitreoretinal proliferation on the edge of the tear in the final case. A recent and large retrospective study found a similar rate of retinal tears and detachments between the conventional 20-gauge and the 25-gauge transconjunctival sutureless vitrectomy.23
The use of microcannulae allows the easiest introduction and removal of the 23-gauge instrumentation through the sclerotomies. However, we had one case of posterior lens opacification induced by a crystalline lens touch during the introduction of the vitreous cutter. The cannulae are not always vertical enough because of the oblique sclerotomy and the instruments have to be introduced carefully, above all in phakic eyes.
In our series, macular hole and epiretinal membranes were treated without any problem during the procedure. The size of the cannulae permits the extraction of silicone oil, and the instruments are larger and more rigid3 to allow the treatment of extensive or severe retinal detachment with vitreoretinal proliferation and the treatment of proliferative diabetic retinopathy. Peripheral vitrectomy seems to be easier and more complete than with a 25-gauge system. No procedure needed a switch to a conventional 20-gauge sclerotomy. However, pars plana fragmentation of the lens cannot be done in cases of posterior luxation of the crystalline lens, because there is no 23-gauge fragmatome available at this moment and the extraction of intraocular foreign bodies (IOFBs) will always require an enlargement of one sclerotomy to the size of the IOFB.
In our study, we observed a very weak inflammatory response to the surgery. The 23-gauge system decreased the operating time, and the conjunctiva, rich in inflammatory mediator, is less affected by surgical trauma. There is no irritation induced by sutures and the incision is transconjunctival and protected by microcannulae. This minimally invasive surgery improves the patient's comfort, care, and management, as was shown in the past for the 25-gauge transconjunctival system.1, 2
The 23-gauge vitrectomy induced no corneal astigmatism. There is very significant stability for all the measured parameters between the preoperative and the postoperative conditions, as was shown for the 25-gauge transconjunctival sutureless vitrectomy in previous studies.26, 27 The self-sealing sclerotomies and the sutureless scleral and conjunctival incisions explain the corneal curvature stability after the procedure. By contrast, the conventional 20-gauge vitrectomy is responsible for significant corneal topographic changes in the first preoperative days or weeks.27, 28, 29
The 23-gauge system appears to be less invasive than the conventional 20-gauge sutured vitrectomy with less postoperative inflammation and a decrease in the operating time linked, above all, to the type of incision. It allows a faster recovery time for the patient. The 25-gauge transconjunctival vitrectomy described by Fujii et al1, 2 was an important development in the surgical management of vitreoretinal diseases, but this technique is characterised by a lower aspiration rate and power of the vitreous cutter. Furthermore, the instruments are too flexible and a complete peripheral vitrectomy or complex manoeuvres are less easy to manage than with the 23-gauge vitrectomy, limiting the indications to isolated vitreous haemorrhage, epiretinal membrane peeling, macular hole, and some uncomplicated retinal detachment.1, 30, 31, 32, 33 The 23-gauge transconjunctival system has the advantages of the 25-gauge vitrectomy with an expansion of the range of indications to complex retinal detachment, diabetic retinopathy, and other vitreoretinal tractions requiring a complete peripheral vitrectomy with scleral depression, as was described in a previous study.3, 15 The rate of vacuum and the level of cut of the vitrector can be adapted to a 23-gauge system as well as the conventional 20-gauge system. The instruments are less flexible than for the 25-gauge system and allow similar movements in the eye as with the 20-gauge system.
The 23-gauge transconjunctival sutureless vitrectomy in the surgical management of vitreoretinal diseases is associated with a low rate of complications specific to the procedure; with transient hypotony resolving without any damage to the eye. It conserves the advantages of the minimally invasive 25-gauge procedure in improving patient recovery, comfort, care, and management, with respect to the conjunctival tissue and a very low inflammatory response. Because of the transconjunctival and sutureless incision there were no corneal topographic changes after the procedure. The 23-gauge system allows an expansion of the 25-gauge system indications to diabetic retinopathy, complex retinal detachment, and other vitreoretinal tractions with an easier surgical practice close to that of the conventional 20-gauge pars plana vitrectomy.
New technological developments are expected to broaden the spectrum of the instrumentation available and the construction of the incision with the introduction of cannulae in one step.
Further studies are required for comparison with the conventional 20-gauge vitrectomy and to determine the incidence of endophthalmitis or complications linked to hypotony.
References
Fujii GY, De Juan Jr E, Humayun MS, Pieramici DJ, Chang TS, Awh C et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology 2002; 109: 1807–1812.
Fujii GY, De Juan Jr E, Humayun MS, Chang TS, Pieramici DJ, Barnes A et al. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology 2002; 109: 1814–1820.
Eckardt C . Transconjunctival sutureless 23-gauge vitrectomy. Retina 2005; 25: 208–211.
Machemer R, Buettner H, Norton EW, Parel JM . Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol 1971; 75: 813–820.
Chen JC . Sutureless pars plana vitrectomy through self-sealing sclerotomies. Arch Ophthalmol 1996; 114: 1273–1275.
Kwok AK, Tham CC, Lam DS, Li M, Chen JC . Modified sutureless sclerotomies in pars plana vitrectomy. Am J Ophthalmol 1999; 127: 731–733.
Jackson T . Modified sutureless sclerotomies in pars plana vitrectomy. Am J Ophthalmol 2000; 129: 116–117.
Theelen T, Verbeek AM, Tilanus MA, Van den Biesen PR . A novel technique for self-sealing, wedge-shaped pars plana sclerotomies and its features in ultrasound biomicroscopy and clinical outcome. Am J Ophthalmol 2003; 136: 1085–1092.
Schmidt J, Nietgen GW, Brieden S . Self-sealing, sutureless sclerotomy in pars plana vitrectomy. Klin Monatsbl Augenheilkd 1999; 215: 247–251.
Lopez-Guajardo L, Pareja-Esteban J, Teus-Guezala MA . Oblique sclerotomy technique for prevention of incompetent wound closure in transconjunctival 25-gauge vitrectomy. Am J Ophthalmol 2006; 141: 1154–1156.
Shimada H, Nakashizuka H, Mori R, Mizutani Y, Hattori T . 25-gauge scleral tunnel transconjunctival vitrectomy. Am J Ophthalmol 2006; 142: 871–873.
Keshavamurthy R, Venkatesh P, Garg S . Ultrasound biomicroscopy findings of 25G transconjuctival sutureless (TSV) and conventional (20G) pars plana sclerotomy in the same patient. BMC Ophthalmol 2006; 6: 7.
Wan T, Hu J, Luo Y, Xu Z, Lin S, Ma P et al. Experimental study of the healing condition of sclerotomy sites after 25-gauge transconjunctival sutureless sclerotomy and 20-gauge vitrectomy. Yan Ke Xue Bao 2007; 23: 37–42.
Warrier SK, Jain R, Gilhotra JS, Newland HS . Sutureless vitrectomy. Indian J Ophthalmol 2008; 56: 453–458.
Fine HF, Iranmanesh R, Iturralde D, Spaide RF . Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology 2007; 114: 1197–1200.
O’Reilly P, Beatty S . Transconjunctival sutureless vitrectomy: initial experience and surgical tips. Eye 2007; 21: 518–521.
Ooto S, Kimura D, Itoi K, Mukuno H, Kusuhara S, Miyamoto N et al. Suprachoroidal fluid as a complication of 23-gauge sutureless vitreous surgery. Br J Ophthalmol 2008; 92: 1433–1434.
Taban M, Sharma S, Ventura AA, Kaiser PK . Evaluation of wound closure in oblique 23-gauge sutureless sclerotomies with visante optical coherence tomography. Am J Ophthalmol 2008; 147: 101–107.
Gupta OP, Maguire JI, Eagle Jr RC, Garg SJ, Gonye GE . The competence of pars plana vitrectomy incisions: a comparative histologic and spectrophotometric analysis. Am J Ophthalmol 2008, available online 23 October 2008.
Taban M, Ufret-vincenty RL, Sears JE . Endophthalmitis after 25-gauge transconjunctival sutureless vitrectomy. Retina 2006; 26: 830–831.
Acar N, Unver YB, Altan T, Kapran Z . Acute endophthalmitis after 25-gauge sutureless vitrectomy. Int Ophthalmol 2007; 27: 361–363.
Kunimoto DY, Kaiser RS . Wills eye retina service. Incidence of endophthalmitis after 20- and 25-gauge vitrectomy. Ophthalmology 2007; 114: 2133–2137.
Shaikh S, Ho S, Richmond PP, Olson JC, Barnes CD . Untoward outcomes in 25-gauge versus 20-gauge vitreoretinal surgery. Retina 2007; 27: 1048–1053.
Okuda T, Nishimura A, Kobayashi A, Sugiyama K . Postoperative retinal break after 25-gauge transconjunctival sutureless vitrectomy: report of four cases. Graefes Arch Clin Exp Ophthalmol 2007; 245: 155–157.
Lam DS, Yuen CY, Tam BS, Cheung BT, Chan WM . Sutureless vitrectomy surgery. Ophthalmology 2003; 110: 2428–2429.
Yanyali A, Celik E, Horozoglu F, Nohutcu AF . Corneal topographic changes after transconjunctival (25-gauge) sutureless vitrectomy. Am J Ophthalmol 2005; 140: 939–941.
Okamoto F, Okamoto C, Sakata N, Hiratsuka K, Yamane N, Hiraoka T et al. Changes in corneal topography after 25-gauge transconjunctival sutureless vitrectomy versus after 20-gauge standard vitrectomy. Ophthalmology 2007; 114: 2138–2141.
Weinberger D, Lichter H, Loya N, Axer-Siegel R, Muzmacher L, Gabbay U et al. Corneal topographic changes after retinal and vitreous surgery. Ophthalmology 1999; 106: 1521–1524.
Domniz YY, Cahana M, Ayni I . Corneal surface changes after pars plana vitrectomy and scleral buckling surgery. J Cataract Refract Surg 2001; 27: 868–872.
Yoon YH, Kim DS, Kim JG, Hwang JU . Sutureless vitreoretinal surgery using a new 25-gauge transconjunctival system. Ophthalmic Surg Lasers Imaging 2006; 37: 12–19.
Lakhanpal RR, Humayun MS, De Juan Jr E, Lim JI, Chong LP, Chang TS et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology 2005; 112: 817–824.
Romero P, Salvat M, Almena M, Baget M, Méndez I . Experience with 25-gauge transconjunctival vitrectomy compared to a 20-gauge system. Analysis of 132 cases. J Fr Ophtalmol 2006; 29: 1025–1032.
Ibarra MS, Hermel M, Prenner JL, Hassan TS . Longer-term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol 2005; 139: 831–836.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the congress of the French Society of Ophthalmology (SFO): 6 May 2007.
Proprietary/financial interests: None.
Rights and permissions
About this article
Cite this article
Schweitzer, C., Delyfer, MN., Colin, J. et al. 23-Gauge transconjunctival sutureless pars plana vitrectomy: results of a prospective study. Eye 23, 2206–2214 (2009). https://doi.org/10.1038/eye.2008.431
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.431
Keywords
This article is cited by
-
Intraoperative choroidal detachment during small-gauge vitrectomy: analysis of causes, anatomic, and visual outcomes
Eye (2022)
-
Intraocular pressure outcomes after 23-G vitreoretinal surgery with two different transconjunctival sutureless sclerotomy techniques: vertical versus tunnel entry
International Ophthalmology (2022)
-
Long-Term Reproducibility of Axial Length after Combined Phacovitrectomy in Macula-sparing Rhegmatogenous Retinal Detachment
Scientific Reports (2018)
-
Response to Park et al
Eye (2012)
-
Conjunctival nevus-like lesions originating from a sclerotomy site after 23-gauge transconjunctival sutureless vitrectomy
Japanese Journal of Ophthalmology (2010)