Abstract
Diabetic eye disease confers substantial burden on the patient quality of life. Current therapeutic strategies indicate an unmet clinical need for preventive therapy. Tight control of blood pressure and glycaemia are mandatory components of primary prevention strategies, but are insufficient to eliminate risk in all patients. A body of evidence supports a role for lipid-modifying therapy in reducing the diabetic retinopathy endpoints. Although inconclusive for statin therapy, results from the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study show beneficial effects of fenofibrate in reducing the requirement for laser therapy, and particularly in preventing disease progression in patients with pre-existing diabetic retinopathy. However, there is a need for confirmation of these findings in large prospective studies with progression of retinopathy as the primary endpoint, such as the ACCORD-EYE (Action to Control Cardiovascular Risk in Diabetes-EYE) study, and in a clinical trial specifically conducted for diabetic maculopathy. In addition, elucidation of the mechanism(s) of effect of fenofibrate is indicated.
Similar content being viewed by others
Introduction
Diabetic eye disease affects up to 50 million people worldwide, and its prevalence is projected to double by 2025 in the absence of improvement in therapeutic preventive strategies.1 In developed countries, diabetic retinopathy is the leading cause of vision loss in adults of working age (20–65 years),1 and substantially impacts on the patient quality of life.2 In the United Kingdom, retinopathy affects about 40% of people with diabetes; of those with type II diabetes, nearly 20% have significant impairment at the time of diagnosis of diabetes.3 Prevalence and severity of diabetic retinopathy appear to be higher in some ethnic groups, specifically in those of Hispanic, Afro-Caribbean,4, 5, 6, 7 or Indo-Asian origin.7 These data suggest that the burden of diabetic eye disease may be even greater in rapidly developing regions.
Pathogenesis of diabetic eye disease
Impaired autoregulation in the microvasculature, arising from high intracellular glucose concentration, is a key initiating factor in diabetic retinopathy.8 A number of biochemical pathways modulate the disease process through effects on cellular metabolism, signalling, and growth factors.9 Increased aldose reductase activity leads to higher intracellular sorbitol concentrations, in turn increasing oxidative stress. High intracellular glucose levels promote the formation of advanced glycation end products, which are implicated in microaneurysm formation. Activation of protein kinase C isoforms mediates a number of effects, including increased vascular permeability, angiogenesis, capillary and vascular occlusion, and pro-inflammatory gene expression, as well as increased production of reactive oxygen species, all of which have deleterious effects on the cell. In particular, an increase in vascular endothelial growth factor (VEGF) is a key angiogenic factor implicated in the pathogenesis of diabetic retinopathy.10, 11 Additionally, increased flux via the hexosamine pathway results in modulation of transcription factors leading to pathological changes in gene expression. Hyperglycaemia-induced overproduction of superoxide by the mitochondria has been proposed as the key unifying mechanism that activates all four pathways. Understanding the metabolic pathways involved in the development of diabetic retinopathy offers clues to future therapeutic possibilities.12, 13
Microangiopathy and capillary occlusion underlie the pathogenesis of diabetic retinopathy.12, 13 Microaneurysms are a hallmark of retinal microvascular disease due to capillary wall abnormalities. Retinal haemorrhages are also observed in the early stages of retinopathy. Breakdown of the blood-retinal barrier, caused by endothelial cell damage and apoptosis, plays a central role in the development of diabetic macular oedema. Increasing closure of capillaries is linked with the appearance of cotton-wool spots, intraretinal haemorrhages, and with intraretinal microvascular abnormalities, which contain large numbers of endothelial-like cells. With further retinal ischaemia, proliferative retinopathy develops, which is characterised by the growth of new blood vessels on the surface of the retina and/or on the optic disc. Visual acuity may be compromised owing to maculopathy, or preretinal, subhyaloid, and vitreous haemorrhage, and subsequent traction from glial tissue formation.
Current management strategies
The management strategies focus on early identification and treatment to reduce the morbidity of diabetic eye disease. In patients with established eye disease, laser therapy is currently regarded as the mainstay of treatment, supported by an extensive body of clinical trial evidence.14 However, laser treatment is usually indicated for more severe disease (proliferative or maculopathy), is not completely effective in all patients,14, 15, 16 and has a number of limitations, which may impact substantially on the patient quality of life, and a reported possibility of visual loss in the short-term following treatment. In one study, vision loss was reported in 10–23% of patients within 6 weeks of treatment.17
The alternatives to laser therapy include surgical and medical treatments (Table 1). However, these are not indicated for all patients, and some have limited data to support their use in routine clinical practice.14, 18, 19 Vitrectomy has a role in the treatment of more severe diabetic eye diseases, including proliferative retinopathy that does not resolve with extensive laser photocoagulation with consequent repeated vitreous haemorrhage, or traction from gliosis. Clinical trials have shown that intravitreal corticosteroids, such as triamcinolone, may improve macular oedema and visual acuity, although raised intraocular pressure, and cataract formation were also frequently reported, as well as rare endophthalmitis.14 As such, this treatment is generally reserved for use in laser resistant cases. Finally, intravitreal injection of VEGF inhibitors (currently indicated for age-related macular degeneration) represents a potential therapeutic alternative.20 Although initial results of trials investigating intravitreal pegaptanib, ranibizumab, and bevacizumab have shown promising results,21, 22, 23 larger studies with longer follow-up are needed. There is a risk of the serious potentially devastating complication of endophthalmitis with all intravitreal injection treatments.
Screening and preventive strategies
Screening, which is integral to the early identification and initiation of preventive strategies, may substantially reduce the morbidity of diabetic eye disease.24 Clinical evidence shows that retinal lesions develop early in the disease process and may be evident in 20% of patients presenting with a new diagnosis of type II diabetes mellitus.3 Early identification of diabetic retinopathy therefore allows earlier intervention and treatment.
Glycaemic and blood pressure control are essential for prevention of diabetic retinopathy, which is supported by evidence from large prospective studies. The United Kingdom Prospective Diabetes Study (UKPDS) in 3867 newly diagnosed patients with type II diabetes, showed that intensive glycaemic control (reducing glycosylated haemoglobin (HbA1c) from 7.9% with conventional control to 7.0% with tight control) reduced all microvascular endpoints by 25% (95% CI 7–40%, P=0.0099). Of note, there was a 29% reduction in the need for laser photocoagulation.25 Data from a subgroup of patients with retinal photographs at diagnosis and follow-up 6 years later showed a similar association, emphasising the need for good glycaemic control.26 Furthermore, the UKPDS showed that tight control of blood pressure was also crucial for preventing deterioration in diabetic retinopathy. Tight control led to a 34% reduction in the risk for deterioration of retinopathy by two steps and a 47% reduced risk of deterioration of visual acuity by three lines of the Early Treatment Diabetic Retinopathy Study (ETDRS) scale.27 The risk of diabetic complications was shown to be associated independently and additively with these two risk factors.28 Whether further improvement provides greater benefit is controversial. The ADVANCE (Action in Diabetes and Vascular Disease: preter Ax and diamicronN-MR Controlled Evaluation) trial showed that better blood pressure control (with combination blood-pressure lowering treatment) failed to significantly impact on the rate of worsening of retinopathy or need for laser treatment compared with conventional control.29 Furthermore, in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial, intensive glycaemic control (reducing median HbA1c from 7.5% with conventional control to 6.4% with tight control) was associated with an excess mortality, leading to termination of this arm of the trial.30
Consensus based on the available evidence is that achievement of recommended targets for HbA1c and blood pressure does not eliminate the risk of diabetic retinopathy, which suggests the need to target other potential risk factors that may be implicated in diabetic retinopathy pathogenesis.
Do lipids have a role?
Patients with combined dyslipidemia (although not familial hypercholesterolaemia) have been shown to have an increased incidence of retinal abnormalities, suggesting that elevated lipids (cholesterol and triglycerides) may be implicated in the development of retinovascular lesions that may occur in diabetic retinopathy (for example, haemorrhage and cotton-wool spots).31 Evidence from observational studies has also supported a link between serum lipids and diabetic eye disease. Elevated total and low-density lipoprotein (LDL) cholesterol levels, and triglycerides were associated with progression of retinopathy, proliferative retinopathy,32, 33, 34, 35 and the development of macular oedema.34, 36 Besides, a high total to high-density lipoprotein (HDL) cholesterol ratio and elevated LDL cholesterol were each associated with the development of clinically significant macular oedema.37 Furthermore, measurement of lipoprotein subclass using nuclear magnetic resonance showed positive associations between the severity of retinopathy and triglyceride levels, and LDL particle concentration and apolipoprotein B levels (a constituent lipoprotein of very low-density, intermediate-density lipoproteins, and LDL), and a negative association with HDL cholesterol.38
Statins and fibrates
Early clinical studies did show a benefit with fibrates in patients with hard retinal exudates.39, 40, 41 However, there was no evidence of improvement in visual acuity, which was not surprising as patients had severe retinopathy and poor vision at baseline. A number of subsequent studies showed improvement in macular oedema and regression of hard exudates with statin therapy,42, 43, 44, 45 as well as significant improvement in worsening of visual acuity.44 However, these studies were in small numbers of patients, and in most cases, involved limited treatment duration.
Exploratory analyses of the microvascular endpoints in the Collaborative Atorvastatin Diabetes Study (CARDS),46 a primary prevention trial including 2838 patients with type II diabetes randomised to treatment with atorvastatin 10 mg or placebo for 4 years, have recently been presented. There was evidence of a trend for reduction in laser therapy with atorvastatin compared with placebo (odds ratio 0.79, P=0.14), although no impact was seen on the progression of diabetic retinopathy.47 Results from other prospective studies, such as the ASPEN (Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in Non-Insulin-Dependent Diabetes Mellitus) study and the ACCORD-EYE study48 are awaited. However, it is not clear on the possible effects of the more usual higher dose of statins commonly used in clinical practice on retinopathy, as data are not available.
Although the exact benefit of statins on diabetic retinopathy remains controversial, the STENO-2 study showed that intensive multifactorial intervention, aimed at management of glycaemia, blood pressure, and lipids (with a statin in 85% of patients), adjunctive to lifestyle modification, produced sustained benefit over conventional treatment in reducing the risk of diabetes-related microvascular complications.49 At the end of the 13.3-year study period (mean of 7.8 years of treatment and 5.5 years of follow-up), intensive treatment led to a 43% reduction in the risk of progression of diabetic retinopathy compared with conventional treatment (P=0.01), as well as 55% reduction in laser treatment for proliferative retinopathy or macular oedema. Intensive treatment, however, was insufficient to prevent the progression of retinopathy in all patients. These data highlight an unmet clinical need for additional preventive therapy in diabetes patients receiving intensive multifactorial treatment, in accordance with current standards of care.
The FIELD microvascular studies
The new findings reported by the FIELD study are promising with regards to potential medical therapy of microvascular disease.50 Briefly, the FIELD study was primarily designed to evaluate the efficacy and tolerability of fenofibrate treatment for prevention of cardiovascular disease in 9795 patients with well-controlled (HbA1c 6.9%) type II diabetes, the majority of whom (about 80%) did not have pre-existing macrovascular or microvascular disease at entry to the trial. The FIELD study failed to show significant reduction in the primary endpoint (nonfatal myocardial infarction and coronary heart disease death, reduction by 11%, P=0.16), but there was significant benefit for the secondary endpoint (total cardiovascular events, reduction by 11%, P=0.035). In part, the lack of significance for the primary endpoint may have been due to a smaller number of events, although there was also the added potential confounder of disproportionate prescription of non-study lipid-modifying therapy (mainly statins) in the placebo group (17 vs 8% in the fenofibrate group, averaged over the study).50
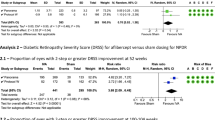
The FIELD study also investigated the effect of fenofibrate on diabetes-related microvascular complications on the basis of a number of pre-specified tertiary endpoints (requirement for laser therapy, progression of albuminuria, and non-traumatic lower-extremity amputation). Importantly, fenofibrate treatment led to a significant 30% reduction (P=0.0003) in the requirement for one or more laser treatments for retinopathy.50 Subsequent intention-to-treat analysis, in which the reasons for laser treatment were independently verified by clinical personnel, who remained masked to treatment allocation, showed significant treatment benefits in reducing first laser therapy in separate analysis of both macular laser and pan retinal photocoagulation for proliferative retinopathy (Table 2).51
In addition, a cohort of 1012 patients also participated in the FIELD Ophthalmology Substudy, which involved serial retinal photography to investigate whether treatment with fenofibrate impacted on the progression of diabetic eye disease. Disease severity was assessed using the ETDRS scale. Although the effect of fenofibrate on the primary endpoint (two-step progression of the ETDRS scale) was not significant for the entire substudy cohort, it was significant among patients with pre-existing retinopathy (absolute event rates of 3.1% vs 14.6% on placebo, P=0.004) with a low number of patients needed to treat (NNT) to prevent a first laser treatment (at 17), and 16 fewer multiple laser events per 100 patients treated with fenofibrate over a 5-year period.51 There was also reduction in a composite endpoint (two-step progression of ETDRS retinopathy grade, macular oedema or laser treatment) (Table 2).51 Although there was a trend to fewer cases of macular oedema in the fenofibrate treatment group (absolute event rates 0.8 vs 2.2% on placebo, P=0.09), the drug did not influence the occurrence of new retinopathy, the occurrence or progression of hard exudates, or the worsening in visual acuity.51 Importantly, there were no major safety concerns of fenofibrate treatment compared with placebo in the main study, and this was also the case in patients on both statin and fibrate combination treatment.
A number of limitations associated with these studies need to be taken into account.47, 52 First, the baseline retinal photographs were not available in all patients in the main study to verify pre-existing retinopathy. Second, the absolute event rates were small, particularly in the substudy. Third, the FIELD study suffered from a number of confounding effects, most notably an excess of non-study lipid-modifying therapy (predominantly statins) in the placebo group.50 Despite these caveats, the results of the FIELD study do point to a beneficial effect of fenofibrate, especially in patients with established diabetic retinopathy. Further data are needed to confirm these findings. In this context, results from the combination treatment group (simvastatin plus fenofibrate) of the ACCORD-EYE study,48 may provide further insight.
Interestingly, the mechanism of benefit of fenofibrate may not be related to its lipid-modifying effects. There was no clinically relevant difference in HDL cholesterol levels between fenofibrate and placebo groups at end of the study.50 Moreover, baseline lipid levels did not differ between patients who did and did not undergo laser treatment.51 Fenofibrate also did not significantly lower the markers of glycaemic control.50 Furthermore, reduction in systolic blood pressure with fenofibrate was less than that reported in the ADVANCE trial with the combination of perindopril and indapamide (decrease of 5.6 mm Hg), which did not report any significant change in eye events.29, 50 Besides, the benefits of fenofibrate were achieved despite excess use of antihypertensive therapy and lipid-modifying therapy (mainly statins) in the placebo group.
Taking these points into consideration, the mechanisms responsible for these effects of fenofibrate are unclear. The FIELD investigators did suggest a number of possibilities based on in vitro findings and experimental studies. These include inhibition of the VEGF pathway,53 and sustained activation of the AMP-activated protein kinase pathway, which suggests a rationale for protection of endothelial cells in the retina against apoptosis.54 Fenofibrate has also been shown to reduce the levels of pro-inflammatory cytokines, such as tumour necrosis factor-α, and interleukins,55 which are elevated in patients with proliferative diabetic retinopathy,56 to improve endothelium-dependent vascular reactivity57 and reduce oxidative stress,58 which have all been implicated in the progression of diabetic retinopathy.9 Although the findings of the FIELD study are clearly of potential clinical interest, these need to be confirmed in other large prospective studies (such as ACCORD-EYE), and in an intention-to-treat study comparing fenofibrate with placebo with the primary endpoints of diabetic retinopathy.48 The elucidation of the postulated mechanism(s) implicated in these effects is indicated as well.
Clinical implications
There is a clear unmet need for medical treatments for diabetic retinopathy, in addition to management of glycaemia and blood pressure as components of diabetes care (Table 3).
It is clear from the FIELD study that there is potential benefit to be gained with fenofibrate in patients with established diabetic retinopathy (that is, secondary prevention), and that this is likely to be in combination with a statin. The FIELD study supports an early benefit after only eight months, and a relatively small and clinically worthwhile number of patients needed to treat (NNT) to prevent a laser endpoint (at 17) over the 5-year study period; in contrast, this figure was large (at 90) for primary prevention. These observations point to the benefit of fenofibrate in those patients following development of diabetic retinopathy, and this is likely to be the case in clinical practice in patients already on statins or in those patients who are statin intolerant. For fenofibrate to gain a specific licence for treatment of diabetic retinopathy, further trials will be required with diabetic retinopathy as the primary endpoint. Although the ACCORD-EYE study should further answer the possible benefits of both statins and fenofibrate in combination, the study is based on a photographic subset of patients, and the primary endpoint is cardiovascular disease.48 Thus, a fenofibrate treatment trial powered and designed with diabetic retinopathy as the primary endpoint is still required to widely establish this therapy in all diabetic patients with diabetic retinopathy. Our own clinical practice is to use this approach, particularly in patients with exudative maculopathy; however, this could be widened to include all patients with diabetic retinopathy if subsequent positive trial data with diabetic retinopathy as primary endpoint are concluded.
Methodology
The following terms were used to search the PUBMED database on 1 September 2008: diabetic retinopathy; diabetic eye disease; macular oedema; treatment; lipid; fibrate; statin; prevention of diabetic eye disease.
References
International Diabetes Federation. Available from www.idf.org. Accessed 15 May 2008.
Candrilli SD, Davis KL, Kan HJ, Lucero MA, Rousculp MD . Prevalence and the associated burden of illness of symptoms of diabetic peripheral neuropathy and diabetic retinopathy. J Diabetes Complications 2007; 21: 306–314.
Diabetes UK . Diabetes and blindness: a focus on action. A report from Diabetes UK. June 2005 Available from www.diabetes.org.uk. Accessed 15 May, 2008.
Emanuele N, Sacks J, Klein R, Reda D, Anderson R, Duckworth W et al. Ethnicity, race and baseline retinopathy correlates in the Veterans Affairs Diabetes Trial. Diabetes Care 2005; 28: 1954–1958.
Harris PD, Klein R, Cowie CC, Rowland M, Byrd-Holt DD . Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? Diabetes Care 1998; 21: 1230–1235.
The Eye Disease Prevalence Research Group. The prevalence of diabetic retinopathy among adults of the United States. Arch Ophthalmol 2004; 122: 552–563.
Day C . The rising tide of type 2 diabetes. Br J Diabetes Vasc Dis 2001; 414: 813–820.
Alder VA, Su EN, Yu DY, Cringle S, Yu P . Overview of studies on metabolic and vascular regulatory changes in early diabetic retinopathy. Aust NZ J Ophthalmol 1998; 26: 141–148.
Brownlee M . Banting Lecture 2004. The pathobiology of diabetic complications. A unifying mechanism. Diabetes 2005; 54: 1615–1625.
Caldwell RB, Bartoli M, Behzadian M, El-Remessy AE, Al-Shabrawey M, Platt DH et al. Vascular endothelial growth factor and diabetic retinopathy: role of oxidative stress. Curr Drug Targets 2005; 6: 511–524.
Nguyen QD, Tatlipinar S, Shah SM, Haller JA, Quinlan E, Sung J et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol 2006; 142: 961–969.
Fong DS, Ferris FL, Aiello LP, Klein R . Diabetic retinopathy. Diabetes Care 2004; 27: 2540–2553.
Joussen A, Smyth N, Niessen C . Pathophysiology of diabetic macular edema. Dev Ophthalmol 2007; 39: 1–12.
Mohamed Q, Gillies MC, Wong TY . Management of diabetic retinopathy: a systematic review. JAMA 2007; 298: 902–916.
Fong DS, Girach A, Boney A . Visual side effects of successful scatter laser photocoagulation surgery for proliferative diabetic retinopathy: a literature review. Retina 2007; 27: 816–824.
Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology 1991; 98: 766–785.
Early Treatment Diabetic Retinopathy Study Research Group. Focal photocoagulation treatment of diabetic macular edema; relationship of treatment effect to fluoroscein angiographic and other retinal characteristics at baseline: ETDRS report no 19. Arch Ophthalmol 1995; 113: 1144–1155.
Sorbinil Retinopathy Trial Research Group. A randomized trial of sorbinil, an aldose reductase inhibitor, in diabetic retinopathy. Arch Ophthalmol 1990; 108: 1234–1244.
Kirkegaard C, Nordgaard K, Snorgaard O, Bek T, Larsen M, Lund-Andersen H . Effect of a one year continuous subcutaneous infusion of a somatostatin analogue, octreotide, on early retinopathy, metabolic control and thyroid function in type 1 (insulin-dependent) diabetes mellitus. Acta Endocrinol 1990; 122: 766–772.
Furlani BA, Meyer CH, Rodrigues EB, Maia M, Farah ME, Penha FM et al. Emerging pharmacotherapies for diabetic macular edema. Expert Opin Emerg Drugs 2007; 12: 591–603.
Cunningham Jr ET, Adamis AP, Altaweel AP, Aiello LP, Bressler NM, D’Amico DJ et al., Macugen Diabetic Retinopathy Study Group. A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Opthalmology 2005; 112: 1747–1757.
Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, Sanchez JG, Wu L, Maia M et al., Pan-American Collaborative Retina Study Group. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema: results from the Pan-American Collaborative Retina Study Group at a 6-month follow-up. Opthalmology 2007; 114: 743–750.
Jorge R, Costa RA, Calucci D, Cintra LP, Scott IU . Intravitreal bevacizumab (Avastin) for persistent new vessels in diabetic retinopathy (IBEPE study). Retina 2006; 26: 1006–1013.
Rohan TE, Frost CD, Wald NJ . Prevention of blindness by screening for diabetic retinopathy: a quantitative assessment. BMJ 1989; 299: 1198–1201.
The UKPDS Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. UKPDS 33. Lancet 1998; 352: 837–853.
Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia 2001; 44: 156–163.
UKPDS. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS report No 38. BMJ 1998; 703–713.
Stratton IM, Cull CA, Adler AI, Turner RC, Holman RR, Manley SE et al. Additive effects of glycaemia and blood pressure exposure on risk of complications in type 2 diabetes: a prospective observational study (UKPDS 75). Diabetologia 2006; 49: 1761–1769.
Patel A, MacMahon S, Chalmers J, Neal B, Woodward M, Billot L et al., ADVANCE Collaborative Group. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 2007; 370: 829–840.
The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008; 358: 2545–2559.
Dodson PM, Galton DJ, Winder AF . Retinal vascular abnormalities in the hyperlipidemias. Trans Ophthalmol Soc UK 1981; 101: 17–21.
Orchard TJ, Dorman JS, Maser RE, Becker DJ, Ellis D, LaPorte RE et al. Factors associated with avoidance of severe complications after 25 yr of IDDMC. Pittsburgh Epidemiology of Diabetes Complications Study I. Diabetes Care 1990; 13: 741–747.
Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss. Early Treatment Diabetic Retinopathy Study Report 18. Invest Ophthalmol Vis Sci 1998; 39: 233–252.
Ucgun NI, Yildirim Z, Kilic N, Gursel E . The importance of serum lipids in exudative diabetic macular edema in type 2 diabetic patients. Ann NY Acad Sci 2007; 1100: 213–217.
Hadjadj S, Duly-Bouhanick B, Bekherraz A, BrIdoux F, Gallois Y, Mauco G et al. Serum triglycerides are a predictive factor for the development and the progression of renal and retinal complications in patients with type 1 diabetes. Diabetes Metab 2004; 30: 43–51.
Ferris III FL, Chew EY, Hoogwerf BJ . Serum lipids and diabetic retinopathy. Early Treatment Diabetic Retinopathy Study Research Group. Diabetes Care 1996; 19: 1291–1293.
Miljanovic B, Glynn RJ, Nathan DM, Manson JE, Schaumberg DA . A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes. Diabetes 2004; 53: 2883–2892.
Lyons TJ, Jenkins AJ, Zheng D, Lackland DT, McGee D, Garvey WT et al. Diabetic retinopathy and serum lipoprotein subclasses in the DCCT/EDIC cohort. Invest Ophthalmol Vis Sci 2004; 45: 910–918.
Duncan LJ, Cullen JF, Ireland JT, Nolan J, Clarke BF, Oliver MF . A three-year trial of atromid therapy in exudative diabetic retinopathy. Diabetes 1968; 17: 458–467.
Harrold BP, Marmion VJ, Gough KR . A double-blind controlled trial of clofibrate in the treatment of diabetic retinopathy. Diabetes 1969; 18: 285–291.
Cullen JF, Town SM, Campbell CJ . Double-blind trial of Atromid-S in exudative diabetic retinopathy. Trans Ophthalmol Soc UK 1974; 94: 554–562.
Chowdhury TA, Hopkins D, Dodson PM, Vafidis GC . The role of serum lipids in exudative diabetic maculopathy: is there a place for lipid-lowering therapy? Eye 2002; 16: 689–693.
Gordon B, Chang S, Kavanagh M, Berrocal M, Yannuzzi L, Robertson C et al. The effects of lipid lowering on diabetic retinopathy. Am J Ophthalmol 1991; 112: 385–391.
Sen K, Misra A, Kumar A, Pandey RM . Simvastatin retards progression of retinopathy in diabetic patients with hypercholesterolemia. Diabetes Res Clin Pract 2002; 56: 1–11.
Gupta A, Gupta V, Thapar S, Bhansali A . Lipid-lowering drug atorvastatin as an adjunct in the management of diabetic macular edema. Am J Ophthalmol 2004; 137: 675–682.
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ et al. CARDS investigators. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004; 364: 685–696.
Dodson PM . Medical treatment for diabetic retinopathy: do the FIELD microvascular study results support a role for lipid lowering? Prac Diabetes 2008; 25: 76–79.
Chew EY, Ambrosius WT, Howard LT, Greven CM, Johnson S, Danis RP et al. Rationale, design and methods of the Action to Control Cardiovascular Risk in Diabetes Eye Study (ACCORD-EYE). Am J Cardiol 2007; 99 (12A): 103i–111i.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O . Effect of a multifactorial intervention in mortality in type 2 diabetes. N Engl J Med 2008; 358: 580–591.
Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR et al. The FIELD study investigators. Effect of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005; 366: 1849–1861.
Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TM, Moffitt MS et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 2007; 370: 1687–1697.
Simó R, Hernández C . Fenofibrate for diabetic retinopathy. Lancet 2007; 370: 1667–1668.
Ferrara N . Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am J Physiol 2001; 280: C1358–C1366.
Kim J, Ahn JH, Yu YS, Yu YS, Kim HS, Ha J et al. Fenofibrate regulates retinal endothelial cell survival through the AMPK signal transduction pathway. Exp Eye Res 2007; 84: 886–893.
Ryan KE, McCance DR, Powell L, McMahon R, Trimble ER . Fenofibrate and pioglitazone improve endothelial function and reduce arterial stiffness in obese glucose tolerant men. Atherosclerosis 2007; 194: e123–e130.
Demircan N, Safran BG, Soylu M, Ozcan AA, Sizmaz S . Determination of vitreous interleukin-1 (IL-1) and tumour necrosis factor (TNF) levels in proliferative diabetic retinopathy. Eye 2006; 20: 1366–1369.
Malik J, Melenovsky V, Wichterle D, Haas T, Simek J, Ceska R et al. Both fenofibrate and atorvastatin improve vascular reactivity in combined hyperlipidemia (fenofibrate versus atorvastatin trial – FAT). Cardiovasc Res 2001; 52: 290–298.
Rosenson RS, Wolff DA, Huskin AL, Helenowski IB, Rademaker AW . Fenofibrate therapy ameliorates fasting and postprandial lipoproteinemia, oxidative stress, and the inflammatory response in subjects with hypertrigyceridemia and the metabolic syndrome. Diabetes Care 2007; 30: 1945–1951.
Author information
Authors and Affiliations
Corresponding author
Additional information
Professor PM Dodson has received honoraria for advisory board membership from Pfizer, AstraZeneca, Takeda and Solvay, and research grants from Eli Lilly. The author is on advisory boards concerning the DIRECT, CARDS, and FIELD studies and principal investigator for the Ruboxistaurin trials in the UK.
Rights and permissions
About this article
Cite this article
Dodson, P. Management of diabetic retinopathy: could lipid-lowering be a worthwhile treatment modality?. Eye 23, 997–1003 (2009). https://doi.org/10.1038/eye.2008.428
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.428
Keywords
This article is cited by
-
Emerging insights into the relationship between hyperlipidemia and the risk of diabetic retinopathy
Lipids in Health and Disease (2020)
-
Medical management of diabetic retinopathy: fenofibrate and ACCORD Eye studies
Eye (2011)
-
Long-term visual and retinopathy outcomes in a predominately type 2 diabetic patient population undergoing early vitrectomy and endolaser for severe vitreous haemorrhage
Eye (2011)
-
Diabetic retinopathy and blockade of the renin–angiotensin system: new data from the DIRECT study programme
Eye (2010)