Abstract
Purpose
Allergic keratoconjunctivitis coexists regularly with allergic rhinitis. However, little is known about the relationship between these conditions. The purpose of this study was to investigate the possible involvement of nasal allergy in keratoconjunctivitis by means of nasal challenge with allergen (NPT), in combination with recording of the ocular symptoms.
Methods
In 26 patients suffering from atopic (n=15) or vernal (n=11) keratoconjunctivitis showing positive history and skin tests, but responding insufficiently to the local ophthalmologic therapy, 71 NPTs with inhalant allergens were performed and combined with the recording of the ocular response. In 11 control subjects with allergic rhinitis, but without ocular disease history, 11 positive NPTs were repeated and supplemented with the registration of the ocular features.
Results
Of the 26 patients, 24 developed 51 positive nasal responses (NRs; P<0.01), 43 of which were accompanied by significant ocular response (P<0.01). No ocular responses were measured during the 26 PBS control challenges (P>0.05) or during 11 repeated NPTs in control subjects (P>0.2).
Conclusions
These results give evidence for possible involvement of nasal allergy in some cases of keratoconjunctivitis. They also show diagnostic value of nasal challenges with allergen in combination with registration of the ocular symptoms in such patients, allowing then consideration of additional therapeutic measures concerning the nasal allergy.
Similar content being viewed by others
Introduction
Keratoconjunctivitis (KC) represents a more serious subtype of allergic conjunctivitis, as cornea, besides the conjunctiva, is also affected in this disorder.1, 2, 3 KC has previously been supposed to be attributed predominantly to the mechanism of IgE-mediated hypersensitivity, caused by direct exposure of conjunctiva with inhalant allergens.1, 2, 3, 4, 5, 6, 7
However, the data gathered during last decade have revealed the multifactorial background of this disorder, where various mechanisms and hypersensitivity types may be involved.1, 2, 3, 8
The possible relationship of the eye and especially of the conjunctiva with the nose has repeatedly been suggested and discussed in the literature.9 The coexistence of allergic rhinitis and allergic conjunctivitis, especially those of the seasonal subforms, has regularly been referred to and has led some investigators to use the term ‘rhinoconjunctivitis’.9
However, there is a dearth of information concerning the possible mutual influences and interaction between the nasal mucosa and conjunctiva, especially with respect to the allergy.1, 2, 9, 10, 11 Moreover, little data are available to show the possible role and involvement of an allergic reaction occurring initially in the nasal mucosa in the conjunctiva, and especially in the possible induction of the secondary conjunctival and corneal response.10, 11, 12, 13, 14
The purpose of this study, being a continuation of our earlier work,10, 11, 12, 13, 14 was to investigate (1) the possible role of nasal allergy in the KC of patients with an insufficient compliance to the current topical ophthalmologic treatment; (2) the possible existence of an ocular response (OR) induced by the primary allergic reaction in the nasal mucosa, its clinical features and types; and (3) the diagnostic value of nasal challenge with allergen for the patients with allergic KC.
Material and methods
Patients
Twenty-six patients, 10 males and 16 females, 20–47 years of age, suffering from KC for more than 4 years, showing insufficient compliance to the topical ophthalmologic therapy, having been referred to our Department of Allergology and Immunology (Institute of Medical Science ‘De Klokkenberg’, Breda, The Netherlands), volunteered to participate in this study. Fifteen patients suffered from atopic KC (AKC) and 11 from vernal KC (VKC). Six of the fifteen AKC patients suffered also from atopic dermatitis, being in a non-acute stage at the time of this study. All these patients showed subjective symptoms as well as objective signs of KC and positive skin tests with various inhalant allergens. Nine of these patients also showed positive specific IgE in serum (RAST) to Dermatophagoides pteronyssinus and/or grasspollen and in 12 of them an increased eosinophil count in the conjunctival scraping specimens had been found previously. All these patients had normal intraocular pressure. None of them suffered from other eye disorders, systemic disease, or immunodeficiency. They had previously been treated with topical and oral H1-receptor antagonists, topical cromolyn and glucocorticosteroids, decongestants, topical vasoconstrictors, some of them with NSAID drugs, but without substantial improvement of their complaints. None of them received nasal cromolyn, nasal or systemic glucocorticosteroids, immunosuppressive drugs, or immunotherapy. The six AKC patients with atopic dermatitis have been treated with topical glucocorticosteroids in the past. All patients underwent a routine diagnostic procedure consisting of detailed history, general examination, ophthalmologic examination including slit-lamp evaluation and vital staining with fluorescein, supplementary skin tests with various inhalant and food allergens, otolaryngologic examination including nasoscopy, cytologic examination of the nasal secretions and X-ray of paranasal sinuses in Water's projection, basic laboratory tests, and bacteriological screening of the conjunctiva. The diagnostic procedure revealed positive history for nasal allergy, violaceous and oedematous nasal mucosa, increased eosinophil and neutrophil count in nasal secretions, and distinctly positive skin tests to a number of inhalant allergens. In seven patients, a significant blood eosinophilia was also found. No other abnormalities or pathologic findings have been detected. In these 26 patients, 71 nasal challenges (nasal provocation test; NPT) with various inhalant allergens were performed by means of rhinomanometry and combined with recording of ocular signs and symptoms. Topical glucocorticosteroids, long-acting H1-receptor antagonists, and NSAID drugs were withdrawn 4 weeks, whereas the topical as well as oral short-acting H1-receptor antagonists, topical decongestants, and other treatments 24 h before this study. The study protocol was approved by the local ethical committee and informed consent was obtained from all participants.
Allergens
Dialysed and lyophilized allergen extracts (Allergopharma, Germany) were diluted in phosphate-buffered saline (PBS), and used for skin tests in concentrations of 100–500 BU/ml and for NPTs in concentrations of 1000–5000 BU/ml (Table 1). If indicated, higher dilutions of the allergen extracts were used both for the skin tests and for the NPTs.
Skin tests
The intracutaneous tests were evaluated 20 min, 6, 12, 24, 36, 48, 72, and 96 h after intradermal allergen injection. A skin wheal reaction (>7.0 mm in diameter) appearing within 20 min after the injection was considered to be a positive immediate skin response, an infiltration occurring 6–12 h later to be a late skin response, and the skin induration appearing later than 24 h, usually between 36–72 h, after the allergen injection, to be a delayed skin response.10, 11, 12, 13, 14, 15, 16, 17
Nasal provocation tests
Nasal challenges with allergens were performed by means of rhinomanometry, as it has already been described in our earlier studies.10, 11, 15, 16 The nasal mucosa response (nasal obstruction) was evaluated by means of nasopharynx–nostril pressure gradients (NPGs), which are the pressure differences (ΔP) between the nasopharyngeal cavity and the outside air, expressed in cm H2O. NPTs were performed according to the following schedule: (1) baseline values recorded at 0, 5, and 10 min before the challenge; (2) PBS control values recorded at 0, 5, and 10 min after a 3-min application of PBS to the nasal mucosa of the non-intubated nasal cavity by means of a saturated wad of cotton wool on a nasal probe inserted under the middle turbinate; (3) postchallenge values recorded after a 3-min challenge with allergen, carried out in the same manner as the challenge with PBS, at 0, 5, 10, 20, 30, 45, 60, 90, and 120 min, and subsequently every hour up to the 12 h, and then every second hour during the time periods between 24–36 and 48–56 h. The allergens used for the NPTs were chosen with respect to the disease history and positive skin tests (Table 1). The nasal response (NR) was considered to be positive when the postchallenge mean NPG values increased by at least 2.0 cm H2O (1.2±0.3, mean±SE) with respect to the mean baseline values, recorded at least at three consecutive time intervals.10, 11, 15, 16 The NPG changes recorded within 60–120 min after the allergen challenge were considered to be an immediate NR, those recorded within 4–12 h to be a late NR, and the changes measured later than 24 h to be a delayed NR.10, 11, 16
Control tests with PBS
The control nasal challenge with PBS was performed in each of these patients by the same schedule as that used for the NPTs with allergen 2, days later.
Ocular response
The objective conjunctival and corneal signs as well as the relevant subjective symptoms were registered before and repeatedly during all NPTs with allergens and PBS at the same time points as the nasal NPG values. The condition of conjunctiva and cornea was assessed by ophthalmoscopy including the slit-lamp evaluation and vital staining with fluorescein. The following parameters were registered: (1) conjunctival signs: hyperaemia (injection), chemosis, hyperlacrimation, papillary hypertrophy, and palpebral oedema; (2) corneal signs: diminished corneal sheen, transparency and reflection; scars (cicatrices); appearance of Horner–Trantas dots; cobblestoning, and appearance of epithelial defects; (3) subjective symptoms: itching (burning), blurred or disturbed vision, foreign body sensation, ocular pain, and photophobia. These parameters were evaluated by means of the modified scale of Abelson et al.7, 18, 19 The following grading scale was applied: 0=absent, 1=mild (present to a slight degree or intermittently), 2=moderate, 3=pronounced (moderately severe), and 4=severe. The statistically significant difference (P<0.05) of the total score was considered to be six points (5±1, mean±SE),recorded at least at three consecutive time intervals.
Control group
Eleven young adults with allergic rhinitis but without history of any ocular disease and with normal ophthalmologic findings volunteered to participate as control subjects. In these patients, 11 positive NPTs (five isolated immediate NRs and six isolated late NRs) with inhalant allergens were repeated and supplemented with registration of the ocular features.
Statistical analysis
NRs and total mean ocular scores were statistically evaluated by means of generalized multivariate analysis of variance (MANOVA) model.20, 21 The polynomials were fitted and the hypotheses were tested by the Pothoff and Roy MANOVA computerized system,20 modified by Timm.21 Statistical evaluation of OR was performed separately for each of the eyes, and then the mean from both the P-values was calculated. A P-value of <0.05 was considered to be statistically significant. Additionally, the total mean score values recorded after the allergen challenge in every individual patient were compared with mean values measured after the PBS control challenge at each time interval and evaluated by Wilcoxon matched-pair signed-rank test. A P-value of <0.05 was considered to be statistically significant.
Results
Nasal responses
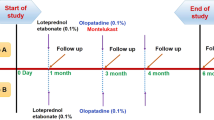
In the 26 patients, 71 NPTs were performed. Twenty-four patients developed 51 positive NRs (P<0.01):11 isolated immediate (IINR; P<0.01), 27 isolated late (ILNR; P<0.01), 3 dual late (DLNR=immediate+late; P<0.05 and P<0.01, respectively), 8 isolated delayed (IDYNR; P<0.05), 2 dual delayed (DDYNR=immediate+delayed; P<0.05 and P<0.01, respectively), and 12 negative responses (NNR; P>0.05; Table 2; Figures 1d, 2d, and 3d). The remaining 2 patients showed eight negative (NRs P>0.05). No statistically significant differences in the NPG values were detected during 26 PBS control tests (P>0.1).
The conjunctival and corneal responses accompanying the isolated immediate nasal responses (IINR; n=8) I=initial (baseline) value; All=Allergen challenge. (a) The mean score of conjunctival signs during IINR (□=hyperemia; ▵=chemosis; ⌖=hyperlacrimation;  =palpebral oedema; ◊=itching;
=palpebral oedema; ◊=itching;  =papillary hypertrophy). (b) The mean score of corneal signs during IINR (▪=epithelial defects; ▴=Horner–Trantas dots;
=papillary hypertrophy). (b) The mean score of corneal signs during IINR (▪=epithelial defects; ▴=Horner–Trantas dots;  =decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=foreign body sensation). (c) The total mean score of conjunctival and corneal response during IINR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during IINR (○) and PBS ( × ).
=decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=foreign body sensation). (c) The total mean score of conjunctival and corneal response during IINR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during IINR (○) and PBS ( × ).
The conjunctival and corneal responses accompanying the isolated late nasal responses (ILNR; n=25) I=initial (baseline) value; All=Allergen challenge. (a) The mean score of conjunctival signs during ILNR (□=hyperemia; ▵=chemosis; ⌖=hyperlacrimation;  =palpebral oedema; ◊=itching;
=palpebral oedema; ◊=itching;  =papillary hypertrophy). (b) The mean score of corneal signs during ILNR (▪=epithelial defects; ▴=Horner–Trantas dots;
=papillary hypertrophy). (b) The mean score of corneal signs during ILNR (▪=epithelial defects; ▴=Horner–Trantas dots;  =decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=foreign body sensation). (c) The total mean score of conjunctival and corneal response during ILNR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during ILNR (○) and PBS ( × ).
=decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=foreign body sensation). (c) The total mean score of conjunctival and corneal response during ILNR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during ILNR (○) and PBS ( × ).
The conjunctival and corneal responses accompanying the isolated delayed nasal responses (IDYNR; n=7) I=initial (baseline) value; All=Allergen challenge. (a) The mean score of conjunctival signs during IDYNR (□=hyperemia; ▵=chemosis; ⌖=hyperlacrimation;  =palpebral oedema; ◊=itching;
=palpebral oedema; ◊=itching;  =papillary hypertrophy). (b) The mean score of corneal signs during IDYNR (▪=epithelial defects; ▴=Horner-Trantas dots;
=papillary hypertrophy). (b) The mean score of corneal signs during IDYNR (▪=epithelial defects; ▴=Horner-Trantas dots;  =decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=ocular pain). (c) The total mean score of conjunctival and corneal response during IDYNR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during IDYNR (○) and PBS ( × ).
=decreased corneal transparency; ◆=diminished corneal sheen/reflection; *=photophobia; +=ocular pain). (c) The total mean score of conjunctival and corneal response during IDYNR (•) and PBS ( × ). (d) The mean rhinomanometric values (NPG) recorded during IDYNR (○) and PBS ( × ).
The differences between the positive and negative NRs were distinctly significant (P<0.001). No differences in NRs were found regarding the particular allergens (Table 1).
Ocular responses
Forty-three of the fifty-one positive NRs and three of the negative NRs, recorded in 24 patients, and three of the negative NRs measured in two patients were associated with significant ocular (conjunctivocorneal) response (P<0.01; Tables 1 and 2). The significant changes in conjunctival and corneal signs were recorded during 8 of 11 isolated immediate NRs (P<0.01), 25 of 27 isolated late NRs (P<0.01), 2 of 3 dual late NRs (P<0.05), 7 of 8 isolated delayed NRs (P<0.05), 1 of 2 dual delayed NRs (P<0.05; Table 2). Of the 20 negative NRs, 6 NRs were accompanied by significant ORs (P<0.05), 2 of which were of an immediate, and 4 were of a late type. The positive ORs were represented by significant changes in the objective conjunctival and corneal signs (P<0.01) as well as in the subjective symptoms (P<0.05; Figures 1a–c, 2a–c and 3a–c). The immediate ORs appeared 10–20 min later than the corresponding INRs, whereas the course of the late and delayed ORs ran parallel to the corresponding NRs.
The immediate OR was characterized by transient functional changes (conjunctival hyperaemia, hyperlacrimation, itching, palpebral oedema, diminished corneal transparency and reflection, and sporadic punctate epithelial erosions), the late OR by persisting functional changes and transient morphologic changes to a slight degree (pronounced conjunctival injection, chemosis, palpebral oedema, papillary hypertrophy of superior tarsus, decreased corneal transparency, limbal Horner–Trantas dots, punctate epithelial erosions, photophobia, and foreign body sensation), whereas the delayed OR was characterized predominantly by morphologic changes (pronounced papillary hypertrophy, decreased corneal transparency, limbal oedema, numerous Horner–Trantas dots, and corneal epithelial defects), accompanied by photophobia, vision disturbance, and moderate ocular pain, lasting for hours to days.
No significant changes in the conjunctival or corneal signs or subjective symptoms were found during the 26 PBS control tests (P>0.1). No significant differences in the ocular changes were measured between both the eyes (P>0.05).
Control subjects
No significant differences were recorded between the first and repeated NRs in 11 control subjects developing five isolated immediate and six isolated late NRs (P>0.05). No significant conjunctival, corneal, or subjective symptoms were detected during the 11 repeated NRs (P>0.05).
Discussion
The relationship between the eye, especially conjunctiva and lacrimal passage, and the nasal mucosa may be implemented on the anatomical as well as the functional level.1, 2, 10, 13, 14, 22, 23, 24, 25 These aspects may include the connection of the conjunctival–lacrimal system with the nasal cavity by means of the nasolacrimal duct and through its opening into nasal cavity facilitating the drainage of tears, blood vessel network, lymphatic tissue and system, and nerve networks, all of them belonging partly to one local network and expressing some links and common properties. In this way, both the organs can influence each other.1, 2, 10, 13, 14, 22, 23, 24, 25
Hypersensitivity reactions developed primarily in the nasal mucosa as a consequence of the intranasal exposure to external (inhalant) allergens may affect the conjunctiva and lacrimal ways and subsequently affect the cornea in various ways and upon involving of various mechanisms.1, 2, 3, 9, 10, 11, 12, 13, 14, 19, 22, 23, 24, 25, 26, 27 (1) The mediators, cytokines, chemokines, chemotactic, and other factors released during allergic reaction in the nasal mucosa could reach conjunctiva either directly by the retrograde penetration through the nasolacrimal duct and lacrimal system, or indirectly by their transport through the blood streamof the related blood vessel system;1, 2, 3, 10, 11, 23, 26 (2) allergic reaction in the nasal mucosa can activate and/or inhibit a number of cell types, such as mast cells, basophils, eosinophils, neutrophils, macrophages, and dendritic cells, and stimulate their migration through the blood stream into the ocular tissues;1, 2, 3, 10, 12, 13, 14, 19, 22, 26, 27, 28, 29, 30 (3) this reaction occurring in the nasal mucosa by stimulating the neurogenic network (sensory nerves, sympathetic as well as parasympathetic fibres) can result in release of various neuropeptides (neurotransmitters), which may reach conjunctivae through the appropriate neurogenic links (nerves);25 (4) the eye, especially conjunctiva and lacrimal system, are rich on the lymphatic tissue, such as ‘eye-associated lymphatic tissue’ (EALT), ‘conjunctiva-associated lymphatic tissue’ (CALT), ‘tear-associated lymphatic tissue’(TALT), and ‘lacrimal drainage-associated lymphatic tissue’ (LDALT), whereas a very prominent ‘nose-associated lymphatic tissue’(NALT) is located in the nasal mucosa.10, 22, 23, 24, 31, 32 Both the local lymphatic structures, belonging to the general ‘mucosa-associated lymphatic system’ (MALT),32 can express manifold mutual communication.22, 32 This communication may include not only transmission of various signals but also the exchange and traffic of certain cell kinds, such as T-lymphocytes (subsets ‘natural killers’, cytotoxic, helper Th1 and Th2), B-lymphocytes (plasma cells) producing immunoglobulins of various classes, macrophages, and other cell types.1, 2, 3, 10, 19, 22, 26, 27, 28, 29, 31, 33, 34 The cell traffic (migration) can be realized not only by means of attraction mechanisms, governed by attraction and/or chemotactic factors and adhesion molecules, but also through the so-called ‘homing’ mechanism of the B-and T-lymphocytes, being controlled by a number of homing factors.1, 10, 22, 26, 27, 31, 32, 35, 36, 37, 38 The disturbed homing mechanisms can then lead to the migration of the particular cell types to different localities.
The diagnostic confirmation of the involvement of hypersensitivity mechanisms in the patient's complaints can be performed by various diagnostic methods, skin tests, and RAST, being the most frequently used of them.1, 2, 5, 6 However, these tests provide only general evidence for the possible existence of hypersensitivity mechanism(s) elsewhere in the body, without further specification of their localization. Moreover, these tests are unable to show the existence and possible involvement of local antibodies in the particular organ or tissue. Finally, they provide only static data related to a certain time interval without any further information on the dynamic aspects of the particular hypersensitivity.10, 11
The PTs with allergens are the only method, which meets the above mentioned criteria.10, 11, 15, 16 PTs are able (1) to confirm the existence of an allergic component in the particular or related organ, (2) to show the causal role of the particular allergen in the patient's complaints, (3) to measure quantitatively the individual types of the organ response in their dynamic course, (4)) to discriminate the participation of allergic component and non-specific hyperreactivity, (5) to show the causal role of an allergic reaction occurring in one organ in the induced response of another.10, 11, 12, 13, 14, 15, 16, 17
The conjunctival PTs (CPT) with allergen are well established techniques, although they are not performed routinely in every relevant patient.1, 2, 3, 4, 5, 6, 7, 9, 18, 26 These tests performed directly on the conjunctiva are able to show different types of the primary conjunctival response (CR), such as immediate (ICR) and late responses (LCR), resulting from the direct exposure of an allergen on the conjunctiva and subsequently on the cornea.30, 39 However, the immunologic mechanisms underlying the individual CR types may differ.1, 3, 10, 19, 26, 27 Although the primary form of delayed CR to allergen challenge has not been reported yet, there is growing evidence for the existence of such mechanism in conjunctiva and cornea disorders as well.22, 27, 29, 30, 33, 34, 38, 39, 40 Nevertheless, CPTs are unable to detect CRs induced secondarily by an allergic reaction occurring initially in an other organ, for example, nasal mucosa. Such CR form can only be shown by nasal challenge with allergen (NPT) combined with registration of the ocular symptoms.10, 12, 13, 14
Our results revealed a number of interesting aspects of allergic KC. The observation of three types of OR, comparable with the three types of NR, suggest involvement of different mechanisms underlying the primary nasal as well as the secondarily induced ORs.10, 12, 13, 14, 15, 17 The immediate OR was associated mainly with transient functional changes, the late OR was represented by persisting functional and partly transient morphologic changes, most of them lasting for several (12–36 h) hours, whereas the delayed OR was associated with a transient tissue damage, predominantly of the corneal epithelium usually persist for hours to days. The observed changes, especially those accompanying the delayed OR, may be comparable with histological changes found by us in the nasal mucosa during the delayed NR.10, 11, 12, 13, 14, 15, 16, 17
The appearance of OR induced by nasal challenge with allergen, even in the absence of the preceding NR, observed in some patients gives evidence for the direct link between the nasal mucosa and conjunctiva.10, 12, 14
It can be concluded that NPTs with allergen performed by means of rhinomanometry in combination with registration of the OR may be an advantageous supplement to the diagnostic procedure in patients with KC, especially in those who respond unsatisfactorily to the topical ophthalmologic therapy. The confirmation of a nasal allergy involvement in KC of some patients may then reveal the need for an additional treatment of nasal allergy.12, 13 Such a combination can improve the total therapeutical effects and achieve better control of the ocular complaints.
References
Mc Gill JI, Holgate ST, Church MK, Anderson DF, Bacon A . Allergic eye disease mechanisms. Br J Ophthalmol 1998; 82: 1203–1214.
Bielory L . Allergic and immunologic disorders of the eye. Part II: Ocular allergy. J Allergy Clin Immunol 2000; 106: 1019–1032.
Leonardi A, De Dominicis C, Motterle L . Immunopathogenesis of ocular allergy: a schematic approach to different clinical entities. Curr Opin Allergy Clin Immunol 2007; 7: 429–435.
Friedlaender MH . Corneal findings in ocular allergy. Int Ophthalmol Clin 1998; 38: 39–46.
Leonardi A . In-vivo diagnostic measurements of ocular inflammation. Curr Opin Allergy Clin Immunol 2005; 5: 464–472.
Radcliffe MJ, Lewith GT, Prescott P, Church MK, Holgate ST . Do skin prick and conjunctival provocation tests predict symptom severity in seasonal allergic rhinoconjunctivitis? Clin Exp Allergy 2006; 36: 1488–1493.
Friedlaender MH . Conjunctival provocative tests: A model of human ocular allergy. Tr Am Ophth Soc 1989; 87: 577–597.
Majmudar PA . Allergic conjunctivitis. June, 30, 2008. www.emedicine.com/oph/topic85.htm.
Baroody FM, Foster K, Markarian A, deTineo M, Naclerio R . Nasal ocular reflexes occur after nasal challenge with allergen. J Allergy Clin Immunol 2007; 119 (Suppl to No 1): S162.
Pelikan Z . The Late Nasal Response. Thesis. The Free University of Amsterdam: Amsterdam, 1996, pp 15–174.
Melillo G, Bonini S, Cocco G, Davies RJ, De Monchy JGR, Frølund L et al. Provocation tests with allergens. Allergy 1997; 52 (Suppl 35): 5–36.
Pelikan M, Pelikan Z . The role of the nasal mucosa in some cases of allergic conjunctivitis and the effects of Disodium cromoglycate (DSCG). J Allergy Clin Immunol 1985; 75 (Suppl to No 1): 186.
Pelikan Z . Allergic conjunctivitis: primary and secondary role of the allergy reaction in the nose. Dutch J Med (Ned Tijdschr Geneesk) 1988; 132: 561–563.
Pelikan Z . The causal role of the nasal allergy in some patients with allergic conjunctivitis. Allergy 2002; 57 (Suppl 73): 230.
Pelikan Z . Late and delayed response of the nasal mucosa to allergen challenge. Ann Allergy 1978; 41: 37–47.
Pelikan Z, Feenstra L, Barree GOF . Response of the nasal mucosa to allergen challenge measured by two different methods of rhinomanometry. Ann Allergy 1977; 38: 263–267.
Pelikan Z . Histologic changes in the nasal mucosa during the immediate (INR), late (LNR) and delayed (DNR) nasal response to allergen challenge. Allergy Clin Immunol News 1991; (Suppl 1): 132 (abstract 158).
Abelson MB, Loeffler O . Conjunctival allergen challenge: models in the investigation of ocular allergy. Curr Allergy Asthma Rep 2003; 3: 363–368.
Bonini S, Bonini S, Berruto A, Tomassini M, Carlesimo S, Bucci MG et al. Conjunctival provocation test as a model for the study of allergy and inflammation in humans. Int Arch Allergy Appl Immunol 1989; 88: 144–148.
Potthoff RF, Roy SN . A generalized multivariate analysis of variance model, useful especially for growth curve problems. Biometrica 1964; 51: 313–326.
Timm NH . Multivariate Analysis with Application in Educations and Psychology. Brooks Cole: Monteray (USA), 1975; 490–510.
O'Sullivan NL, Montgomery PC, Sullivan DA . Ocular mucosal immunity. In: Mestecky J, Binnenstock J, Lamm M, Strober W, McGhee J, Mayer L (eds). Mucosal immunology, 3rd ed. Elsevier- Academic Press: Burlington (MA, USA), San Diego (CA, USA), London, 2005; 1477–1496.
Knop E, Knop N . Lacrimal drainage-associated lymphoid tissue (LDALT): a part of the human mucosal immune system. Invest Ophthalmol Vis Sci 2001; 42: 566–574.
Paulsen F . The human nasolacrimal ducts. Adv Anat Embryol Cell Biol 2003; 170: 1–106.
Motterle L, Diebold Y, De Salamanca AE, Saez V, Garcia-Vazquez C, Stern ME et al. Altered expression of neurotransmitter receptors and neuromediators in vernal keratoconjunctivitis. Arch Ophthalmol 2006; 124: 462–468.
Bacon AS, Ahluwalia P, Irani AM, Schwartz LB, Holgate ST, Church MK et al. Tear and conjunctical changes during the allergen-induced early- and late-phase responses. J Allergy Clin Immunol 2000; 106: 948–954.
Metz DP, Hingorani M, Calder VL, Buckley RJ, Lightman SL . T-cell cytokines in chronic allergic eye disease. J Allergy Clin Immunol 1997; 100: 817–824.
Takano Y, Fukagawa K, Dogru M, Asano-Kato N, Tsubota K, Fujishima H . Inflammatory cells in brush cytology samples correlate with severity of corneal lesions in atopic keratoconjunctivitis. Br J Ophthalmol 2004; 88: 1504–1505.
Abu El-Asrar AM, Struyf S, Al-Kharashi SA, Missotten L, Van Damme J, Geboes K . Expression of T lymphocyte chemoattractants and activation markers in vernal keratoconjunctivitis. Br J Ophthalmol 2002; 86: 1175–1180.
Metz DP, Bacon AS, Holgate ST, Lightman SL . Phenotypic characterization of T cells infiltrating the conjunctiva in chronic allerguc eye disease. J Allergy Clin Immunol 1996; 98: 686–696.
Dua HS, Gomes JA, Jindal VK, Appa SN, Schwarting R, Eagle RC et al. Mucosa specific lymphocytes in the human conjunctiva, corneoscleral limbus and lacrimal gland. Curr Eye Res 1994; 13: 87–93.
Wotherspoon AC, Hardman-Lea S, Isaacson PG . Mucosa-associated lymphoid tissue (MALT) in the human conjunctiva. J Pathol 1994; 174: 33–37.
Stern ME, Siemasko KF, Niederkorn JY . The Th1/Th2 paradigm in ocular allergy. Curr Opin Allergy Clin Immunol 2005; 5: 446–450.
Baudouin Ch, Liang H, Bremond-Gignac D, Hamard P, Hreiche R, Creuzot-Garcher C et al. CCR4 and CCR5 expression in conjunctival specimens as differential markers of Th1/Th2 in ocular surface disorders. J Allergy Clin Immunol 2005; 116: 614–619.
Youngman KR, Lazarus NH, Butcher EC . Lymphocyte homing: Chemokines and adhesion molecules in T cell and IgA plasma cell localization in the mucosal immune system. In: Mestecky J, Binnenstock J, Lamm M, Strober W, McGhee J, Mayer L (eds). Mucosal immunology, 3rd ed. Elsevier-Academic Press: Burlington (MA, USA), San Diego (CA, USA), London, 2005; 667–680.
Alcaide P, King SL, Dimitroff CJ, Lim YC, Fuhlbrigge RC, Luscinskas FW . The 130-kDa glycoform of CD43 functions as an E-selectin ligand for activated Th1 cells in vitro and in delayed-type hypersensitivity reactions in vivo. J Invest Dermatol 2007; 127: 1964–1972.
Warnock RA, Askari S, Butcher EC . Molecular mechanisms of lymphocyte homing to peripheral lymph nodes. J Exp Med 1998; 187: 205–216.
Shoji J, Inada N, Sawa M . Antibody array-generated cytokine profiles of tears of patients with vernal keratoconjunctivitis or giant papillary conjunctivitis. Jpn J Ophthalmol 2006; 50: 195–204.
Calder VL, Jolly G, Hingorani M, Adamson P, Leonardi A, Secchi AG et al. Cytokine production and mRNA expression by conjunctival T-cell lines in chronic allergic eye disease. Clin Exp Allergy 1999; 29: 1214–1222.
Leonardi A, Fregona IA, Plebani M, Secchi AG, Calder VL . Th1- and Th2-type cytokines in chronic ocular allergy. Graefe's Arch Clin Exp Ophthalmol 2006; 244: 1240–1245.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial or conflict of interest: None
Rights and permissions
About this article
Cite this article
Pelikan, Z. The possible involvement of nasal allergy in allergic keratoconjunctivitis. Eye 23, 1653–1660 (2009). https://doi.org/10.1038/eye.2008.341
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.341
Keywords
This article is cited by
-
Cellular changes in tears associated with keratoconjunctival responses induced by nasal allergy
Eye (2014)
-
Allergic Conjunctivitis and Nasal Allergy
Current Allergy and Asthma Reports (2010)