Abstract
Purpose
To assess the safety and effectiveness of treating corneal endothelial rejection with a subconjunctival injection of 20 mg triamcinolone acetonide in combination with topical application of 1% prednisolone acetate, as compared to treatment with an intravenous pulse of 500 mg methylprednisolone in combination with topical application of 1% prednisolone acetate.
Methods
A case–controlled study including a literature review was performed. Patients who presented with an initial episode of corneal endothelial rejection were treated with subconjunctival injection of 20 mg triamcinolone in combination with topically applied 1% prednisolone and were retrospectively matched for age and diagnosis to patients who received a single intravenous injection of 500 mg methylprednisolone in combination with topical 1% prednisolone. Patients were analysed regarding reversion of the rejection episode, intraocular pressure, and visual acuity after 1 year.
Results
Overall, the triamcinolone group had a better outcome regarding reversion of corneal transplant rejection (P=0.025), with 15 of 16 patients in the triamcinolone group having clear grafts, compared to only 10 of 16 patients in the methylprednisolone group. Intraocular pressure (IOP) was increased in both groups at day 30 (P=0.002), although there was no statistically significant difference in IOP between the groups (P=0.433). Visual acuity improved in both groups after 1 year (P=0.049), although slightly more improvement was observed in the triamcinolone group (P=0.002).
Conclusions
The results observed in this case–controlled study suggest that the use of subconjunctival triamcinolone acetonide may benefit patients with corneal transplant rejection.
Similar content being viewed by others
Introduction
Immunological rejection of donor grafts is one of the major causes of corneal transplant failure.1, 2, 3, 4 Currently, the rate of corneal failure following penetrating keratoplasty is roughly 25–35% at the end of 5 years,4, 5 and the main cause of graft failure is acute corneal rejection. Williams et al4 reported that 30.9% of corneal failures in a large patient cohort were due to immunological rejection. The rate of reversibility after an acute corneal rejection is quite variable, ranging from 50 to 94%,1, 6, 7, 8, 9, 10, 11, 12 and this depends on numerous factors, including previous rejection episodes, amount of time between symptom onset and treatment, graft size, preoperative diagnosis, graft thickness at the time when rejection is diagnosed, recipient age, lens status, concomitant vitrectomy, deep stromal vascularization, and peripheral anterior synechiae, among others.2, 5, 12, 13, 14
The primary treatment of corneal allograft rejection is corticosteroids, which can be administered through topical, periocular, oral, and intravenous routes. The optimal route of administration remains unknown,15 and many diverse approaches are currently employed.6, 7, 16, 17, 18, 19, 20
Prednisolone acetate is the most widely used topical corticosteroid for treating corneal transplant rejection.18 Topical corticosteroids are used to treat all corneal rejection episodes, and about 60% of ophthalmologists used only topical corticosteroids, even in patients with severe rejection with an obvious rejection line and corneal oedema, in a survey of members of the Cornea Society performed by Randleman et al.18 The advantages of using topical application include fewer side effects and facility of use, along with an acceptable success rate. The most commonly used regimen is topical 1% prednisolone acetate, which is used at hourly intervals throughout the day and night for the first few days after the onset of corneal rejection, followed by the tapering of the dose. The disadvantages of the topical route include reduced adherence, as the high frequency of instillation decreases outpatient compliance. However, Hudde et al9 reported a 92% success rate with topical and subconjunctival treatment in an inpatient setting.
Systemic medication to treat corneal rejection is also widely used. The two major systemic therapeutic options are oral prednisone and an intravenous pulse of methylprednisolone.14 In a study, Hill et al6 found a high success rate (92.3%) using intravenous methylprednisolone when treatment was given within 8 days of the onset of symptoms.
Oral corticosteroids can be used alone or in combination with an intravenous pulse of methylprednisolone. The most commonly used is prednisone, usually given daily at a dose greater than 60–80 mg for the first several days, with subsequent tapering of the dose as the graft begins to recover.14
Some immunosuppressants also have a role in the treatment and prevention of corneal rejections. Cyclosporine, used both topically and systemically, has been the most commonly used drug in this group.8, 21, 22 Newer drugs are being investigated for this same purpose, such as FK-506 (tacrolimus), rapamycin, and 15-deoxyspergualin.14
Subconjunctival corticosteroids may be used in cases of diffuse, recurrent, or hard-to-control rejections. The most commonly used drugs for this purpose are dexamethasone, which may require multiple applications,23 and bethamethasone.24 Interestingly, Randleman and Stulting18 recently reported that the use of subconjunctival corticosteroids to treat corneal transplant rejection decreased during the period between 1989 and 2004.
Triamcinolone is a depot corticosteroid that has been used with some success to treat inflammatory conditions, such as uveitis, diabetic macular oedema, and age-related macular degeneration. A variety of administration routes exist for triamcinolone, including subconjunctival, intravitreal, and sub-Tenon.25, 26, 27, 28
The purpose of this study was to assess the safety and efficacy of treating corneal endothelial allograft rejection with a subconjunctival injection of 20 mg triamcinolone acetonide and topical 1% prednisolone acetate, when compared to treatment with an intravenous pulse of 500 mg methylprednisolone and topical 1% prednisolone acetate.
Materials and methods
All patients seen at the State University of Campinas Hospital Cornea Service, Brazil, from November 2005 to October 2006, who presented with their first episode of corneal transplant endothelial rejection and met the study criteria (listed later in this section) were included in this case–controlled study. These patients composed the experimental group and were treated with subconjunctival injection of 20 mg triamcinolone acetonide, along with topical 1% prednisolone acetate administered once every hour for the first week, with subsequent tapering of treatment frequency. All patients in this group signed an informed consent form, and the University Medical Ethics Committee approved the study, according to the tenets of the Declaration of Helsinki.
To select the control group, we analysed 10 years of archived corneal service charts from the State University of Campinas Hospital (November 1995 to October 2005) to identify all patients who also experienced an initial episode of corneal transplant rejection and met the study criteria. During this period, 67 patients had their first episode of corneal transplant rejection treated with an intravenous pulse of 500 mg methylprednisolone plus 1% prednisolone acetate.
The optimal sample size was calculated for an unmatched case–control study with a confidence level (1−α) of 95%, a power (1−β) of 80%, a rate of 60% of success for the control group and an expected rate of success of 80% for the experimental group. The sample size needed was 91 patients for each study group, totalling 182 patients. As enroling such a large number would be unfeasible, we opted to perform a matched case–controlled study as it was a more appropriate design for rare outcomes. Over the typical period 1 year, we recruited patients for the experimental treatment and then performed the matching of participants in the control group. Patients in the control group were matched by age (within 5 years) and diagnosis. Surgical parameters did not differ significantly during the study period.
Corneal graft rejection was defined as the appearance of one or more of the following: an endothelial rejection line, new keratic precipitates, anterior chamber cells, and/or corneal oedema in the donor graft not previously noted.
The inclusion criteria were (a) first episode of corneal transplant rejection and (b) referral to Cornea Service within 15 days following the symptom onset. Patients diagnosed with herpetic infections that led to keratoplasty, pregnant women, and patients who refused to sign the informed consent form were excluded from the study. Patients with a primary diagnosis of herpes simplex keratitis were excluded mainly because triamcinolone is known to cause recurrent herpetic keratitis,29, 30 and because of the difficulties to properly differentiate between corneal graft rejection and recurrent viral keratitis.
On the day that the rejection was diagnosed, subconjunctival injection of 20 mg triamcinolone acetonide was performed, after which 1% prednisolone acetate was administered once every hour for 1 week, with subsequent tapering of frequency. Patients in the control group had been treated with a single intravenous pulse of 500 mg methylprednisolone given on the same day that rejection was diagnosed. Similar to the experimental group, the control group received topical 1% prednisolone acetate once every hour for 1 week with subsequent tapering.
All patients were assessed on days 1, 7, 15, 30, 90, 180, and 365 following corticosteroid administration. Examinations included review of patient medical history, assessment of best-corrected visual acuity, biomicroscopy, funduscopy, and Goldmann applanation tonometry.
Successful treatment of corneal transplant rejection was determined by slit-lamp examination and was defined by both the return of the donor cornea to a transparent state and the absence of associated oedema and aqueous humour cells, if initially present.
Any patient who had an additional episode of corneal rejection during the 1-year follow-up period received a second intervention with corticosteroids, consisting of either 20 mg subconjunctival triamcinolone or 500 mg intravenous methylprednisolone. If the cornea returned to transparency after the second administration of corticosteroids, these patients were classified as achieving qualified success.
All side effects were monitored, and patients received topical treatment as needed for any increased intraocular pressure (IOP).
The variables examined in this study included successful resolution of corneal rejection 1 year following the first episode of rejection, visual acuity (VA) after 1 year of treatment, and IOP after 30 days of corticosteroid administration. Repeated measures analysis of variance was used to compare the VA and the IOP between both groups during follow-up, as more than one measurement was taken in each patient. To compare the variable success of both groups following treatment of corneal rejection, the marginal homogeneity test was used. P-values <0.05 were considered statistically significant. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
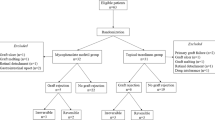
Sixteen patients met the study criteria and received subconjunctival injections of 20 mg triamcinolone acetonide combined with topical 1% prednisolone acetate during the 12-month recruitment period. The patients in the control group who received 500 mg methylprednisolone combined with topical 1% prednisolone acetate were compared with the patients who received subconjunctival triamcinolone; only one patient in the control group could be properly matched to each experimental patient. Patient 6 of the triamcinolone group was diagnosed with postradial keratotomy ectasia, and no exact match could be found in the historical series. Therefore, this patient was matched with a patient with leukoma secondary to bacterial keratitis, who had the most similar prognosis among those in the control group. All patients in the study were followed up for at least 1 year after the first episode of corneal rejection.
In the triamcinolone group, the initial episode of corneal rejection reverted in all patients except patient 4. Three patients experienced new corneal endothelial rejections after the initial reversion within the 1-year follow-up period and needed a second administration of subconjunctival corticosteroid.
In the methylprednisolone group, four of 16 patients had corneal rejection episodes that did not respond to treatment. Another four patients experienced new episodes of corneal endothelial rejection and needed a second administration of intravenous corticosteroid. Of the four patients who were given two administrations, two experienced reversion of the second episode of corneal rejection, whereas the other two suffered corneal failure. Figure 1 demonstrates the treatment progression for both patient groups.
After 1 year, patients treated with triamcinolone had a higher rate of transplant survival (15/16), as determined by optically clear corneas, compared with patients treated with methylprednisolone (10/16; P=0.025). Table 1 shows the results of transplant rejection treatment for both study groups.
IOP increased in both groups, peaking on the 30th day. Baseline IOP was 13.38±3.24 and 13.75±3.06 mmHg in the subconjunctival triamcinolone and intravenous methylprednisolone groups, respectively, and reached 18.31±6.53 mmHg after 1 month in the triamcinolone group and 15.69±4.3 mmHg in the intravenous methylprednisolone group. VA improved in both groups. Baseline VA was 1.27±0.54 log MAR for the patients in the experimental group and 1.74±0.53 log MAR for the patients in the control group. At the end of 1 year, VA improved to 0.74±0.67 log MAR and 1.54±0.94 log MAR in the experimental and control groups, respectively. Individual results for IOP, VA, and reversion success of endothelial corneal rejection are shown in Table 2.
Table 3 shows repeated measures analysis of variance for IOP and VA. These results confirm that the two groups did not differ, on average, with respect to the IOP measures taken during follow-up (P=0.433). However, both groups showed a statistically significant increase in IOP at day 30 (P=0.002). VA improvement was observed between the baseline measures and the measures taken at the end of 1 year for both treatment groups (P=0.049), although a greater improvement was observed in the triamcinolone group (P=0.002).
Complications were observed in some patients following treatment. Secondary glaucoma was seen in four patients in the triamcinolone group (patients 4, 8, 14, and 15); these patients received topical treatment to lower their IOP. Patients 4 and 15 needed only topical β-blocker treatment to achieve adequate IOP control, whereas patients 8 and 14 needed additional medication. Patient 8 had all medication discontinued at the end of the ninth month as the IOP returned to normal levels. In addition, patient 2 developed a posterior subcapsular cataract (P3—LOCS III—Lens Opacity Classification System III). In the methylprednisolone group, only one patient developed glaucoma (patient 12), which was properly controlled with a topical β-blocker.
Discussion
As a depot corticosteroid, triamcinolone acetonide may persist in the aqueous humour longer than other corticosteroids that are commonly utilized to treat corneal transplant endothelial rejection.31 Aqueous humour levels of triamcinolone were detectable up to 18 months following the injection of 20–25 mg intravitreal triamcinolone.32 However, Thomas et al33 emphasized that the intraocular concentration of triamcinolone may vary following sub-Tenon's administration.
We hypothesized that the use of subconjunctival triamcinolone would maintain therapeutic corticosteroid levels in the aqueous humour for a sufficient amount of time to inhibit the rejection process and, thus, would both minimize possible failures during topical corticosteroid treatment and increase the likelihood of successful corneal transplant rejection treatment.
Patients with corneal endothelial rejection usually undergo an intense topical corticosteroid therapy, which often requires hourly applications of steroid eye drops. Application frequency is cited as a cause of irregular compliance that may compromise results. Hudde et al9 reported no statistically significant differences between two groups that received either topical corticosteroids alone or topical corticosteroids in combination with a single pulse of 500 mg methylprednisolone. The authors attributed their results to in-patient treatment that ensured hourly application of steroid drops. In this study, 15/16 patients (93.75%) exhibited clear grafts at the end of follow-up after treatment with a single triamcinolone subconjunctival injection plus topical prednisolone. Hudde et al9 reported a similar, though slightly lower, percentage of clear grafts (16/19, 84.2%) at a comparable follow-up with an in-patient treatment regimen that also included one subconjunctival 2 mg bethamethasone injection.
Hill et al6 reported an overall graft survival of 79.2% (19/24) with a single intravenous injection of 500 mg methylprednisolone combined with topical treatment but found only 63.6% (7/11) graft survival when patients presented more than 8 days after symptom onset. In our study, we found 62.5% (10/16) graft survival with intravenous methylprednisolone treatment in patients that presented up to 15 days after the onset of rejection. This is very similar to the results reported by Hill et al6 for late presenting patients. We found, however, that subconjunctival triamcinolone yielded 93.75% (15/16) graft survival in our patients, which is quite similar to both the 92.3% (12/13) that Hill et al6 found in early rejection patients who received intravenous methylprednisolone and the 94% (32/34) graft survival that Young et al8 reported using a combination of intravenous pulse methylprednisolone, oral cyclosporine, and 1% prednisolone eye drops. Therefore, subconjunctival injection of 20 mg triamcinolone yielded high numbers of clear grafts 1 year after corneal rejection, similar to the best results currently reported in literature.
In our study, we opted to analyse all patients who began treatment within 15 days of symptom onset because most of our patients who experience corneal rejection after a penetrating keratoplasty do not come to our service within 1 week of the graft rejection episode, even though they have extensive counselling about the symptoms of corneal rejection. This could be attributed to the low socioeconomic status of this population and their difficulty in reaching the State University of Campinas Hospital. We believe that the inclusion criteria adopted in this study enhance its clinical applicability. In a tertiary care eye hospital in the United States of America, Epstein et al34 reported that about 70% of patients who experienced corneal graft rejection after penetrating keratoplasty had no symptoms and had graft rejection diagnosis at a routine follow-up visit.
A whitish deposit in the superior conjunctiva was noted in all patients treated with triamcinolone; however, this was not a significant aesthetic problem. Subconjunctival haemorrhage, ptosis, eyelid oedema, and other complications related to subconjunctival drug injection may also be expected.
The disadvantages of subconjunctival triamcinolone use include those associated with corticosteroid treatment, such as the possibility of posterior subcapsular cataracts, secondary infections, and a rise in IOP.
Triamcinolone acetonide elevates IOP, especially when administered through periocular and intravitreal pathways.35, 36 This effect was not detected in this study, as the average IOP did not differ between the experimental and control groups. However, the triamcinolone-treated group had more individuals with secondary glaucoma (4/16) as compared with the control group (1/16). Three out of the four individuals who developed glaucoma in the experimental group had only transient IOP elevations, which may correspond to a temporary response to the subconjunctival triamcinolone. Because of the small number of patients in our study, the IOP data analysis could potentially have been affected by type-II statistical error; we may have come to alternative conclusions if a larger number of patients had been included in the study. Nonetheless, we believe that the benefits associated with subconjunctival triamcinolone treatment outweigh the inconvenience of using IOP lowering medications.
We acknowledge that this study has some limitations, such as the relatively small number of patients and the fact that the study groups were non-contemporaneous, with the control group being based on chart reviews. However, these limitations are common to a number of studies that deal with corneal graft rejection.
The results observed in this case–controlled study suggest that the use of subconjunctival triamcinolone acetonide may benefit patients with corneal transplant rejection. Further studies are needed to assess the safety and effectiveness of this treatment regimen in larger populations.
References
Williams KA, Muehlberg SM, Lewis RF, Coster DJ . Long-term outcome in corneal allotransplantation. The Australian Corneal Graft Registry. Transplant Proc 1997; 29 (1–2): 983.
Price MO, Thompson Jr RW, Price Jr FW . Risk factors for various causes of failure in initial corneal grafts. Arch Ophthalmol 2003; 121 (8): 1087–1092.
Thompson Jr RW, Price MO, Bowers PJ, Price Jr FW . Long-term graft survival after penetrating keratoplasty. Ophthalmology 2003; 110 (7): 1396–1402.
Williams KA, Esterman AJ, Bartlett C, Holland H, Hornsby NB, Coster DJ . How effective is penetrating corneal transplantation? Factors influencing long-term outcome in multivariate analysis. Transplantation 2006; 81 (6): 896–901.
Sit M, Weisbrod DJ, Naor J, Slomovic AR . Corneal graft outcome study. Cornea 2001; 20 (2): 129–133.
Hill JC, Maske R, Watson P . Corticosteroids in corneal graft rejection. Oral vs single pulse therapy. Ophthalmology 1991; 98 (3): 329–333.
Hill JC, Ivey A . Corticosteroids in corneal graft rejection: double vs single pulse therapy. Cornea 1994; 13 (5): 383–388.
Young AL, Rao SK, Cheng LL, Wong AK, Leung AT, Lam DS . Combined intravenous pulse methylprednisolone and oral cyclosporine A in the treatment of corneal graft rejection: 5-year experience. Eye 2002; 16 (3): 304–308.
Hudde T, Minassian DC, Larkin DF . Randomised controlled trial of corticosteroid regimens in endothelial corneal allograft rejection. Br J Ophthalmol 1999; 83 (12): 1348–1352.
Alldredge OC, Krachmer JH . Clinical types of corneal transplant rejection. Their manifestations, frequency, preoperative correlates, and treatment. Arch Ophthalmol 1981; 99 (4): 599–604.
The collaborative corneal transplantation studies (CCTS). Effectiveness of histocompatibility matching in high-risk corneal transplantation. The Collaborative Corneal Transplantation Studies Research Group. Arch Ophthalmol 1992; 110 (10): 1392–1403.
Naacke HG, Borderie VM, Bourcier T, Touzeau O, Moldovan M, Laroche L . Outcome of Corneal transplantation rejection. Cornea 2001; 20 (4): 350–353.
Boisjoly HM, Tourigny R, Bazin R, Laughrea PA, Dubé I, Chamberland G et al. Risk factors of corneal graft failure. Ophthalmology 1993; 100 (11): 1728–1735.
Panda A, Vanathi M, Kumar A, Dash Y, Priya S . Corneal graft rejection. Surv Ophthalmol 2007; 52 (4): 375–396.
Coster DJ, Williams KA . The impact of corneal allograft rejection on the long-term outcome of corneal transplantation. Am J Ophthalmol 2005; 140 (6): 1112–1122.
Barker NH, Henderson TR, Ross CA, Coster DJ, Williams KA . Current Australian practice in the prevention and management of corneal allograft rejection. Clin Experiment Ophthalmol 2000; 28 (5): 357–360.
Koay PY, Lee WH, Figueiredo FC . Opinions on risk factors and management of corneal graft rejection in the United Kingdom. Cornea 2005; 24 (3): 292–296.
Randleman JB, Stulting RD . Prevention and treatment of corneal graft rejection: current practice patterns (2004). Cornea 2006; 25 (3): 286–290.
Rinne JR, Stulting RD . Current practices in the prevention and treatment of corneal graft rejection. Cornea 1992; 11 (4): 326–328.
Thiel MA, Ross CA, Coster DJ . Corneal allograft rejection: has the time come for intravenous pulsed methylprednisolone? A debate. Clin Experiment Ophthalmol 2000; 28 (6): 398–404.
Inoue K, Amano S, Kimura C, Sato T, Fujita N, Kagaya F et al. Long-term effects of topical cyclosporine A treatment after penetrating keratoplasty. Jpn J Ophthalmol 2000; 44 (3): 302–305.
Lam DS, Wong AK, Tham CC, Leung AT . The use of combined intravenous pulse methylprednisolone and oral cyclosporin A in the treatment of corneal graft rejection: a preliminary study. Eye 1998; 12 ( Pt 4): 615–618.
Moro F, Cvintal T . Tratamento Padrão da Rejeição. In: Cvintal T (ed). Complicações do Transplante de Córnea. Livraria Santos Editora Ltda.: São Paulo, 2004, pp 241–245.
Ehlers JP, Shah CP, Fenton GL, Hoskins EN, Shelsta HN . The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease, 5th edn. Lippincott Williams & Wilkins: Philadelphia, 2008, pp 97–98.
Bandello F, Pognuz R, Polito A, Pirracchio A, Menchini F, Ambesi M . Diabetic macular edema: classification, medical and laser therapy. Semin Ophthalmol 2003; 18 (4): 251–258.
Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE . Macular edema. Surv Ophthalmol 2004; 49 (5): 470–490.
Ip MS . Intravitreal injection of triamcinolone: an emerging treatment for diabetic macular edema. Diabetes Care 2004; 27 (7): 1794–1797.
Jonas JB . Intravitreal triamcinolone acetonide for diabetic retinopathy. Dev Ophthalmol 2007; 39: 96–110.
Gulkilik G, Demirci G, Ozdamar AM, Muftuoglu GI . A case of herpetic keratitis after intravitreal triamcinolone injection. Cornea 2007; 26 (8): 1000–1001.
Shtein RM, Stahl RM, Saxe SJ, Mian SI . Herpes simplex keratitis after intravitreal triamcinolone acetonide. Cornea 2007; 26 (5): 641–642.
Weijtens O, Feron EJ, Schoemaker RC, Cohen AF, Lentjes EG, Romijn FP et al. High concentration of dexamethasone in aqueous and vitreous after subconjunctival injection. Am J Ophthalmol 1999; 128 (2): 192–197.
Jonas JB . Intraocular availability of triamcinolone acetonide after intravitreal injection. Am J Ophthalmol 2004; 137 (3): 560–562.
Thomas ER, Wang J, Ege E, Madsen R, Hainsworth DP . Intravitreal triamcinolone acetonide concentration after subtenon injection. Am J Ophthalmol 2006; 142 (5): 860–861.
Epstein AJ, de Castro TN, Laibson PR, Cohen EJ, Rapuano CJ . Risk factors for the first episode of corneal graft rejection in keratoconus. Cornea 2006; 25 (9): 1005–1011.
Roth DB, Realini T, Feuer WJ, Radhakrishnan R, Gloth J, Heimmel MR et al. Short-term complications of intravitreal injection of triamcinolone acetonide. Retina 2008; 28 (1): 66–70.
Yamamoto Y, Komatsu T, Koura Y, Nishino K, Fukushima A, Ueno H . Intraocular pressure elevation after intravitreal or posterior sub-Tenon triamcinolone acetonide injection. Can J Ophthalmol 2008; 43 (1): 42–47.
Author information
Authors and Affiliations
Corresponding author
Additional information
Accepted for presentation at ARVO 2008 annual meeting
Rights and permissions
About this article
Cite this article
Costa, D., de Castro, R. & Kara-Jose, N. Case–control study of subconjunctival triamcinolone acetonide injection vs intravenous methylprednisolone pulse in the treatment of endothelial corneal allograft rejection. Eye 23, 708–714 (2009). https://doi.org/10.1038/eye.2008.289
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.289
Keywords
This article is cited by
-
Methylprednisolone/prednisolone acetate/triamcinolone
Reactions Weekly (2018)
-
Reply to: Costa DC et al
Eye (2009)