Abstract
Objective
In a recent study, we found high levels of erythropoietin (EPO) in patients with diabetic macular oedema (DME), suggesting a role of EPO in the pathogenesis of this condition. To investigate a possible relationship between EPO and other diseases causing macular oedema, we determined vitreous levels of this peptide in patients with macular oedema secondary to retinal vein occlusion (RVO) and compared them with levels in patients with DME and control patients.
Methods
Vitreous and serum samples were obtained from patients with macular oedema secondary to RVO, DME, epiretinal membrane, and macular hole (controls). EPO was measured by radioimmunoassay.
Results
No differences were found in median vitreous EPO levels between patients with RVO and controls: RVO, 76 mU/ml (30–806) vs controls, 25 mU/ml (10–75) (P=0.105). Median EPO concentration was higher in DME patients than in patients with RVO or controls: DME, 430 mU/ml (41–3000) vs RVO, 76 mU/ml (30–806) (P<0.0001) vs controls, 25 mU/ml (10–75) (P<0.0001).
Conclusions
EPO levels are not elevated in patients with macular oedema secondary to RVO. Patients with DME have high levels of EPO. These results suggest that EPO could be involved in the pathogenesis of diabetic retinopathy, but not in macular oedema secondary to RVO.
Similar content being viewed by others
Introduction
Over the last years, several studies have shown that vitreous factors play an important role in the pathophysiology of macular oedema.1, 2, 3, 4, 5, 6, 7 Vascular endothelial growth factor (VEGF), which is also a proangiogenic factor, is the best known of these factors. High concentrations of this peptide have been found in the vitreous of patients with macular oedema secondary to several diseases. Other vitreous factors, also related to angiogenesis, are thought to have a role in oedema formation. We found lower concentrations of somatostatin (SST), an antiangiogenic factor, in the vitreous fluid of patients with proliferative diabetic retinopathy as compared with controls, suggesting that SST deficit can contribute to neovascularization in this disease.8, 9 In addition, SST levels are decreased in the vitreous fluid of patients with diabetic macular oedema (DME), which suggests a relationship between vascular permeability and SST deficit.10 Erythropoietin (EPO) is a glycoprotein with a well recognized erythropoietic function. High concentrations of this factor have been found in the vitreous fluid of patients with proliferative diabetic retinopathy; hence, EPO could act as an angiogenic factor in this disease.11 Recently, we found high levels of intravitreal EPO in patients with DME, suggesting a link between this factor and the pathogenesis of this condition.12 The aim of this study was to evaluate vitreous levels of EPO in patients with retinal vein occlusion (RVO), a condition in which macular oedema also develops, as compared to patients with DME and control patients.
Materials and methods
Patients
The study included non-diabetic patients with central RVO (CRVO) or branch RVO (BRVO) and patients with DME, who had undergone vitrectomy or vitreous tapping. The control group consisted of non-diabetic patients with other conditions requiring vitrectomy, but who were not affected by macular oedema or neovascularization. The exclusion criteria were proliferative diabetic retinopathy, other ischaemic retinal diseases, previous ocular surgery, uveitis, vitreal haemorrhage, and haemoglobin detection in the vitreous sample. Informed consent was obtained from each patient following an explanation of the purpose and potential adverse effects of the procedures. This study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of our hospital.
Ophthalmologic examinations
Preoperative examinations included visual acuity using Snellen charts, complete biomicroscopic evaluation, measurement of intraocular pressure by Goldmann tonometer, and fundus examination using a quadraspheric fundus contact lens (Volk). Macular oedema was confirmed by fluorescein angiography (FAG) and optical coherence tomography (OCT), which was also used to measure retinal thickness at the central fovea. Idiopathic epiretinal membrane and macular hole were diagnosed both clinically and by OCT.
Vitreous samples
Vitreous was obtained from taps or vitrectomies. Vitrectomy plus radial optic neurotomy, vitrectomy plus arteriovenous decompression, and vitrectomy plus posterior hyaloid and internal limiting membrane dissection were performed to treat CRVO, BRVO, and DME, respectively. Undiluted vitreous samples (0.5–1 ml) were obtained at the start of vitrectomy by aspiration into a 1-ml syringe attached to the vitreous cutter (Alcon Model, Accurus 800 × S4; Irvine, California, USA) before initiating intravitreal infusion of balanced salt solution. Vitreous taps were performed in cases in which intravitreal injection of triamcinolone acetonide was administered to treat macular oedema; 0.5–1 ml of vitreous was obtained with a portable vitreous cutter just before the injection. The vitreous samples were transferred to a sterile tube, placed immediately on ice, and centrifuged at 16 000 × g for 5 min at 4°C. Supernatants were frozen at −80°C until assayed. For serum determinations, blood samples were collected at the same time as vitrectomy or vitreous tap and centrifuged at 3000 × g for 10 min at 4°C. The serum obtained was aliquoted and stored at −80°C until assayed.
EPO assessment
Erythropoietin was measured by an RIA method (Phoenix Pharmaceutical, Belmont, USA) with a limit of detection of 4.4 mU/ml.
Intravitreous haemoglobin
Vitreous haemoglobin level was measured by spectrophotometry (Uvikon 860, Kontron Instruments, Zurich), which permits haemoglobin measurement in micromolar concentrations. The limit of detection of the method was 0.03 mg/ml.
Protein assay
Vitreal proteins were measured by a previously validated microturbidimetric method with an autoanalyzer (Hitachi 917; Boehringer, Manheim, Germany). This method, based on the benzetonium chloride reaction, is highly specific for the detection of proteins and has higher sensitivity and reproducibility than the classic method of Lowry. The lowest level of proteins detected was 0.02 mg/ml. Intra- and interassay coefficients of variation were 2.9 and 3.7%, respectively.
Vitreous fluid analysis as a surrogate of retinal physiology
In this study we applied a method developed by our group that allows rationalized use of vitreous fluid as a tool for in vivo assessment of the events taking place in the retina. First, we reject samples containing haemoglobin. Vitreous haemorrhage can produce an influx of serum proteins into the vitreous fluid, thus precluding its usefulness for the study of intraocular production of a particular protein. Second, we perform case–control studies, matching patients and control patients for plasma levels of the peptide under study, as plasma protein levels can influence the vitreal concentrations. Third, we corrected the intravitreal concentration of the peptide under study for total vitreal protein levels. The presence of elevated intravitreal levels of any protein does not necessarily mean that intraocular production is responsible for the elevation. It may simply be a reflection of a nonspecific increase in total vitreal proteins due to disruption of the blood–retinal barrier (BRB).
This methodology has been used in previous publications and has been used by other groups investigating diabetic retinopathy.
Statistical analysis
The Kolmogorov–Smirnov test was used to confirm the assumption of normality of the variables. Student's t-test and ANOVA were used to compare continuous variables, and the χ2 test for categorical variables. Because of their skewed distribution, EPO concentrations are expressed as the median and range, and statistical comparisons were performed using a nonparametric test (Mann–Whitney U-test). Statistical significance was set at P<0.05.
Results
The study included 12 consecutive patients with DME, 12 consecutive patients with RVO, 9 with CRVO, and 3 with BRVO. The level of retinopathy of the patients with DME was mild nonproliferative diabetic retinopathy in every case according to the international clinical diabetic retinopathy and DME disease severity scales.13 FAG did not show peripheral ischaemia in patients with DME. Patients with RVO presented with profuse haemorrhages, so areas of nonperfusion could not be assessed by FAG. Twenty age-matched patients (10 with idiopathic epiretinal membrane and 10 with macular hole) served as the control group. Demographic characteristics and treatments performed in patients with RVO and DME are summarized in Table 1.
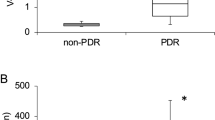
There were no significant differences in serum EPO concentration between the groups: RVO, 8.9 mU/ml (7–20.8) vs DME, 12.4 mU/ml (7.8–46.7), P=0.573; RVO, 8.9 mU/ml (7–20.8) vs controls, 8.6 mU/ml (4.1–19), P=0.075; DME, 12.4 mU/ml (7.8–46.7) vs controls, 8.6 mU/ml (4.1–19), P=0.488, (Figure 1). Vitreous EPO concentration was significantly higher in patients with DME than in patients with RVO and controls in absolute terms: DME, 430 mU/ml (41–3000) vs RVO, 76 mU/ml (30–806) (P<0.0001); DME, 430 mU/ml (41–3000) vs controls, 25 mU/ml (10–75) (P<0.0001); and after adjusting for intravitreal proteins: DME, 105 mU/mg (13–967) vs RVO, 69 mU/mg (27–800), P=0.02 and DME, 105 mU/mg (13–967) vs controls, 50 mU/mg (13–107) (P=0.02) (Figure 2). No differences in vitreous EPO concentration were found in patients with RVO as compared to the control patients (76 mU/ml (30–806) vs 25 mU/ml (10–75), P=0.105) After adjusting the results by intravitreous protein concentration, there were again no differences between these groups (RVO: 69 mU/mg (27–800) vs 50 mU/mg (13–107); P=0.095) (Figure 2).
No differences in vitreous EPO concentration were found in patients with CRVO as compared to patientss with BRVO: CRVO, 91.3 mU/ml (30–417) vs BRVO, 101 mU/ml (100–806) (P=0.081); Patients with CRVO were compared with patients with DME and there was still a difference between them in absolute terms: CRVO, 91.3 mU/ml (30–417) vs DME, 430 mU/ml (41–3000), P<0.0001; and after adjusting for intravitreal proteins: CRVO, 53 mU/mg (27–190) vs DME, 105 mU/mg (13–967) (P=0.02). Moreover, there were no differences between patients with CRVO and controls in absolute terms: CRVO, 91.3 mU/ml (30–417) vs controls, 25 mU/ml (10–75) (P=0.1) and after adjusting for intravitreal proteins: 53 mU/mg (27–190) vs 50 mU/mg (13–107) (P=0.096).
Discussion
Macular oedema is responsible for vision loss in many patients with RVO and diabetic retinopathy. Several factors are involved in the pathophysiology of these conditions. In patients with RVO, thrombosis at the level of the lamina cribosa and the arteriovenous crossing increases distal intraluminal capillary pressure, which induces hypoxic damage to endothelial cells; this, in turn, leads to elevated vascular permeability.14, 15 In patients with DME, chronic metabolism alterations, such as the polyol and hexosamine pathways, de novo synthesis of diacylglycerol -proteincinase C, and production of free radicals and advanced glycosylation end products, damage endothelial cell function and ultimately lead to capillary hyperpermeability.16, 17 Many investigators have suggested that growth factors and cytokines play an important role in the pathogenesis of macular oedema in both diseases.
In two different studies, Noma et al18, 19 determined aqueous and vitreal levels of VEGF and IL-6 in patients with BRVO. Concentrations of these factors were elevated as compared to controls and correlated with the severity of macular oedema. A great deal of information is available on the role of VEGF in the pathogenesis of DME.3, 4, 20, 21, 22 EPO is a glycoprotein with a neuroprotective effect in the retina.23 Watanabe et al11 determined vitreous levels of EPO in patients with proliferative diabetic retinopathy. They found strikingly elevated levels of this peptide when compared to controls, suggesting a role for this factor in neovascularization secondary to diabetic retinopathy. Recently, we found that patients with DME and no significant ischaemia have elevated levels of intravitreal EPO and that intraocular production is responsible for these elevated levels.12 It is possible that EPO enhancement might be related to hyperpermeability in patients with DME. However, in vitro and experimental studies have shown that EPO decreases permeability of the blood–brain barrier (BBB), an anatomical structure similar to the BRB. Martinez-Estrada et al24 using an in vitro model of bovine BBB provided evidence that EPO protects against VEGF-induced permeability of the BBB and restores the tight junction proteins. EPO treatment also prevented an increase of BBB permeability in a rat model of induced seizures.25 As the BBB is structurally and functionally similar to the BRB, it is possible that EPO could act as an antipermeability factor in the retina. In this regard, a substantial improvement in DME has been reported after treating azotemia-induced anaemia with EPO.26
Is it possible that this increase might be related to a self-regulated physiological neuroprotective mechanism to prevent chronic retinal metabolic damage, rather than a pathogenic contribution to vascular permeability? In an attempt to answer this question, we have investigated a possible relationship between EPO and macular oedema secondary to another disease. In this study, we determined vitreous concentrations of EPO in patients with macular oedema due to RVO. Our results showed no differences in vitreous EPO concentrations between these patients and the controls, both in absolute terms and after adjusting for intravitreal proteins. Moreover, vitreous EPO concentrations in patients with DME were higher than in patients with RVO and the controls. Taken together, these results suggest that EPO might not be related to vascular permeability, and support the idea that EPO enhancement in patients with DME may be related to its neuroprotective properties. Furthermore, our results show that diabetic retinal chronic metabolic alteration may be a more powerful stimulus for EPO enhancement than retinal ischaemia. Even the patients with CRVO (who theoretically have more ischaemia than patients with BRVO) and controls had similar levels of EPO.
This study has several limitations. First, the small number of patients in each group and the large range of EPO concentration in both the DME and RVO patients. Nonetheless, statistically significant differences between diabetic patients and patients with RVO and controls were observed. Second, the duration of macular oedema was not recorded. It is possible that in patients with RVO, macular oedema had lasted for a shorter period of time due to the acute nature of the disease, which prompts patients to consult early. Hence, it is possible that hyperproduction of EPO occurred later in the evolution of the disease. Finally, although vitreous fluid obtained from patients undergoing vitreoretinal surgery is currently used to explore the synthesis of factors by the retina, it is an indirect measure. A direct method, quantification of EPO RNA expression, with which we demonstrated EPO RNA expression in the adult human retina and showed that this expression is higher in diabetic patients, cannot be performed in patients with RVO for obvious reasons. Finally, we can only suggest that EPO is not related to vascular permeability. Further studies must be performed to investigate the precise relationship between EPO and the BRB. In this regard, Western immunoblot studies on the tight junctions in endothelial cell cultures exposed to EPO would provide data to determine whether or not EPO has an effect on BRB homoeostasis.
In conclusion, vitreous EPO levels are elevated in patients with DME. In patients with macular oedema secondary to RVO, EPO levels are similar to those of control patients. Although it seems that EPO enhancement in patients with DME is related to its neurotrophic properties, further studies are needed to clarify the precise role of EPO in the pathogenesis of this condition.
References
Pe'er J, Folberg R, Itin A, Gnessin H, Hemo I, Keshet E . Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology 1998; 105: 412–416.
Boyd SR, Zachary I, Chakravarthy U, Allen GJ, Wisdom GB, Cree IA et al. Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion. Arch Ophthalmol 2002; 120: 1644–1650.
Funatsu H, Yamashita H, Ikeda T, Mimura T, Eguchi S, Hori S . Vitreous levels of interleukin-6 and vascular endothelial growth factor are related to diabetic macular edema. Ophthalmology 2003; 110: 1690–1696.
Funatsu H, Yamashita H, Nakamura S, Mimura T, Eguchi S, Noma H et al. Vitreous levels of pigment epithelium-derived factor and vascular endothelial growth factor are related to diabetic macular edema. Ophthalmology 2006; 113: 294–301.
Patel JL, Tombran-Tink J, Hykin PG, Gregor ZJ, Cree IA . Vitreous and aqueous concentrations of proangiogenic, antiangiogenic factors and other cytokines in diabetic retinopathy patients with macular edema: implications for structural differences in macular profiles. Exp Eye Res 2006; 82: 798–806.
Ouchi M, West K, Crabb JW, Kinoshita S, Kamei M . Proteomic analysis of vitreous from diabetic macular edema. Exp Eye Res 2005; 81: 176–182.
Peters S, Cree IA, Alexander R, Turowski P, Ockrim Z, Patel J et al. Angiopoietin modulation of vascular endothelial growth factor: Effects on retinal endothelial cell permeability. Cytokine 2007; 40: 144–150.
Simo R, Lecube A, Sararols L, García-Arumí J, Segura RM, Casamitjana R et al. Deficit of somatostatin-like immunoreactivity in the vitreous fluid of diabetic patients. Diabetes Care 2002; 25: 2282–2286.
Hernandez C, Carrasco E, Casamitjana R, Deulofeu R, García-Arumí J, Simó R . Somatostatin molecular variants in the vitreous fluid: comparative study between diabetic patients with proliferative diabetic retinopathy and nondiabetic control subjects. Diabetes Care 2005; 28: 1941–1947.
Simo R, Carrasco E, Fonollosa A, García-Arumí J, Casamitjana R, Hernández C . Deficit of somatostatin in the vitreous fluid of patients with diabetic macular edema. Diabetes Care 2007; 30: 725–727.
Watanabe D, Suzuma K, Matsui S . Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. N Engl J Med 2005; 353: 782–789.
Hernandez C, Fonollosa A, Garcia-Ramirez M, Higuera M, Catalán R, Miralles A et al. Erythropoietin is expressed in the human retina and it is highly elevated in the vitreous fluid of patients with diabetic macular edema. Diabetes Care 2006; 29: 2028–2033.
Wilkinson CP, Ferris III FL, Klein RE, Lee PP, Agardh CD, Davis M et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003; 110: 1677–1682.
Ciardella AP, Clarkson JG, Guyer DR, Renno RZ, Yannuzzi LA . Central retinal vein occlusion: a primer and review. In: Yannuzzi LA (ed). Retina-Vitreous-Macular. W.B. Saunders: New York, 1999.
Hayreh SS . Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res 2005; 24: 493–519.
Giardino I, Brownlee M . The biochemical basis of microvascular disease. In: Pickup JC, Williams G (eds). Textbook of diabetes. Blackwell Science: Oxford, 1997; 42.1–42.16.
Brownlee M . Biochemistry and molecular cell biology of diabetic complications. Nature 2001; 414: 813–820.
Noma H, Funatsu H, Yamasaki M, Tsukamoto H, Mimura T, Sone T et al. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and IL-6. Am J Ophthalmol 2005; 140: 256–261.
Noma H, Minamoto A, Funatsu H, Tsukamoto H, Nakano K, Yamashita H et al. Intravitreal levels of vascular endothelial growth factor and interleukin-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2006; 244: 309–315.
Antonetti D, Barber AJ, Khin S, Lieth E, Tarbell JM, Gardner TW et al. Vascular permeability in experimental diabetes is associated with reduced endothelial occluding content: vascular endothelial growth factor decreases occludin in retinal endothelial cells. Diabetes 1998; 47: 1953–1959.
Antonetti DA, Lieth E, Barber AJ, Gardner TW . Molecular mechanisms of vascular permeability in diabetic retinopathy. Semin Ophthalmol 1999; 14: 240–248.
Antcliff RJ, Marshall J . The pathogenesis of edema in diabetic maculopathy. Semin Ophthalmol 1999; 14: 223–232.
Junk AK, Mammis A, Savitz SI, Singh M, Roth S, Malhotra S et al. Erythropoietin administration protects retinal neurons from acute ischemia reperfusion injury. Proc Natl Acad Sci USA 2002; 99: 10659–10664.
Martínez-Estrada OM, Rodríguez-Millán E, González-De Vicente E, Reina M, Vilaró S, Fabre M . Erythropoietin protects the in vitro blood-brain barrier against VEGF-induced permeability. Eur J Neurosci 2003; 18: 2538–2544.
Uzum G, Sarper Diler A, Bahcekapili N, Ziya Ziylan Y . Erythropoietin prevents the increase in blood brain barrier permeability during pentylenetetrazol-induced seizures. Life Sci 2006; 78: 2571–2576.
Friedman EA, L'Esperance FA, Brown CD, Berman DH . Treating azotemia induced anemia with erythropoietin improves diabetic eye disease. Kidney Int 2003; (Suppl 64): S57–S63.
Acknowledgements
Jose Garcia-Arumi had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcí-Arumí, J., Fonollosa, A., Macià, C. et al. Vitreous levels of erythropoietin in patients with macular oedema secondary to retinal vein occlusions: a comparative study with diabetic macular oedema. Eye 23, 1066–1071 (2009). https://doi.org/10.1038/eye.2008.230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.230
This article is cited by
-
Systemic and vitreous biomarkers — new insights in diabetic retinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Erythropoietin produced by the retina: its role in physiology and diabetic retinopathy
Endocrine (2012)
-
Neuroprotection in Diabetic Retinopathy
Current Diabetes Reports (2012)
-
Retinal vein occlusions: The potential impact of a dysregulation of the retinal veins
EPMA Journal (2010)
-
Diabetic macular oedema and erythropoietin
Eye (2009)